A Systematic Review of Evidence-Based Family Interventions for Trauma-Affected Refugees
Abstract
:1. Introduction
1.1. Working with Displaced and Minoritized Refugee Families
1.2. Family Interventions Implemented with Trauma-Affected Refugees
2. Materials and Methods
2.1. Search Strategy
2.2. Criteria for Inclusion and Exclusion
3. Results
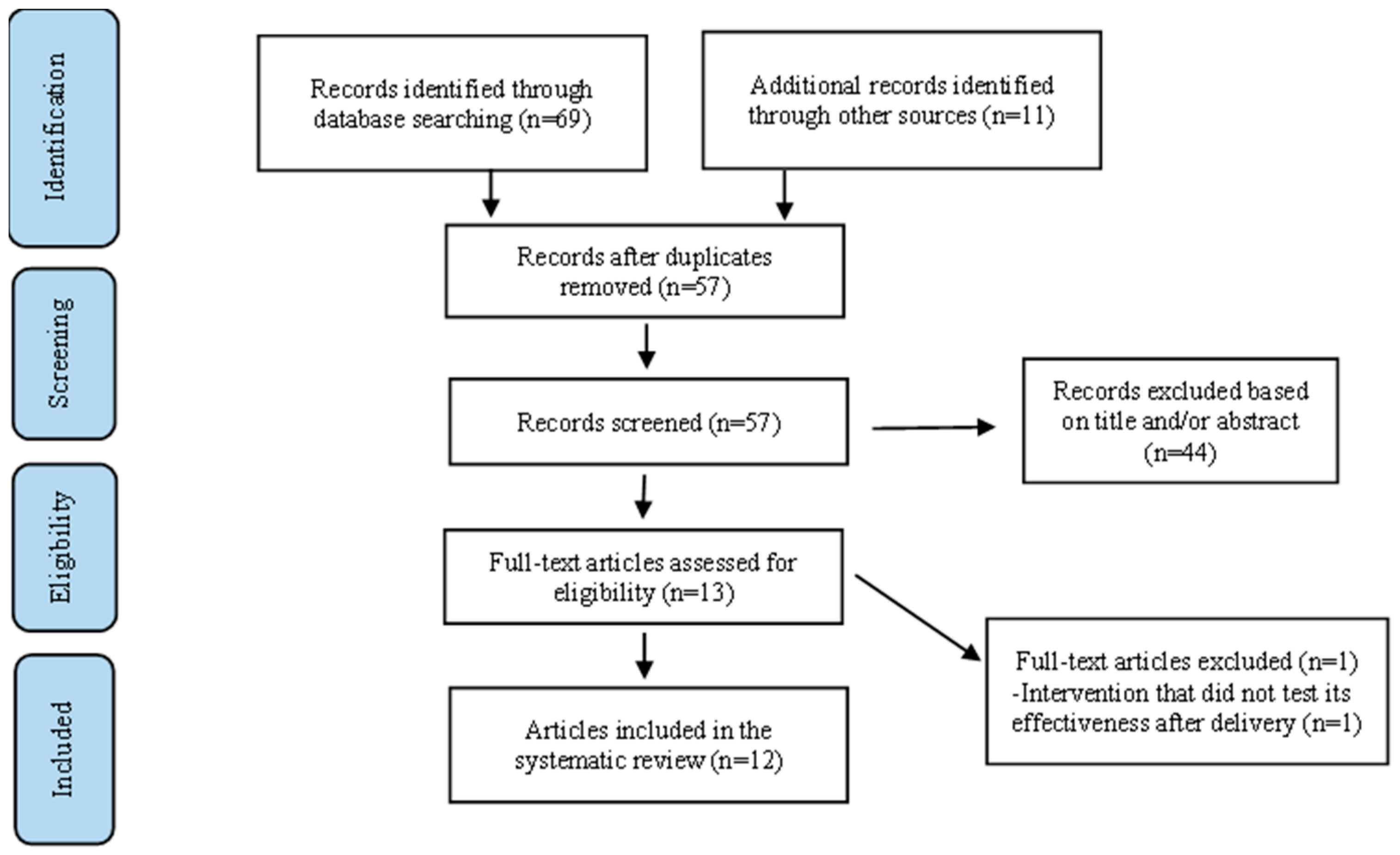
3.1. Study Selection
3.2. Study Designs
3.3. Types of Interventions
3.3.1. Parenting Interventions
3.3.2. Multifamily Interventions
3.3.3. School-Based Interventions
3.4. Effectiveness of the Interventions/Results of the Studies
3.5. Cultural Adaptation Processes
3.6. Implementation and Dissemination Strategies
4. Discussion
Known Barriers to Advancing Mental Health and Systemic Treatments
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Study | Design | Intervention | Aims of the Intervention | Were the Aims Achieved? | Culturally Adaptation Process | Implementation and Dissemination Strategies |
|---|---|---|---|---|---|---|
| Nonexperimental | School-based | Reduce PTSD symptoms Improve social functioning | Yes | Not specified | Refugee staff |
| Nonexperimental | School-based | Improve social functioning | Yes | Not specified | Scale developer/therapist/psychiatrist/graduate students |
| RCT | School-based | Reduce PTSD symptoms | Yes | Not specified | School clinicians/ educators/psychologist |
| Quasi- experimental | School-based | Reduce PTSD symptoms Improve social functioning | Yes | Use of native translator | Psychiatrist/Medical student/translator |
| Nonexperimental | School-based | Reduce PTSD symptoms Improve social functioning | Yes | Including drumming | Not specified |
| RCT | Multifamily group | Increase mental health seeking Improve family functioning | Yes | Use of native facilitators | Refugee staff |
| Feasibility | Multifamily group | Increase mental health seeking Improve family functioning | Yes | Use of native facilitators | Refugee staff |
| Feasibility | Multifamily group | Reduce PTSD symptoms Improve family functioning | Yes | Community participatory research approach (CBPR) | Refugee staff/social workers |
| Nonexperimental | Multifamily group | Reduce PTSD symptoms | Yes | Not specified | EBTS leaders/interpreter |
| Feasibility | Parenting | Improve parent–child relationships and family functioning | Yes | Ecological validity model | Trained therapists/Intervention Coaches |
| RCT | Parenting | Improve parent–child relationships and family functioning | Yes | Not specified | Trained lay facilitators |
| Feasibility | Parenting | Improve child behaviors, family functioning | Yes | Not specified | Trained research assistants/translators |
References
- UNHCR. Refugee Data Finder. Available online: https://www.unhcr.org/refugee-statistics/ (accessed on 20 July 2022).
- Wilmsen, B.; Webber, M. What can we learn from the practice of development-forced displacement and resettlement for organised resettlements in response to climate change? Geoforum 2015, 58, 76–85. [Google Scholar] [CrossRef]
- UNHCR. Global Trends. Available online: https://www.unhcr.org/flagship-reports/globaltrends/ (accessed on 2 May 2022).
- Slobodin, O.; De Jong, J.T.V.M. Family interventions in traumatized immigrants and refugees: A systematic review. Transcult. Psychiatry 2015, 52, 723–742. [Google Scholar] [CrossRef] [PubMed]
- Birman, D.; Tran, N. Psychological distress and adjustment of Vietnamese refugees in the United States: Association with pre- and postmigration factors. Am. J. Orthopsychiatry 2008, 78, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Mollica, R.F.; McInnes, K.; Pool, C.; Tor, S. Dose-effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. Br. J. Psychiatry 1998, 173, 482–488. [Google Scholar] [CrossRef]
- Wieling, E.; Utržan, D.S.; Witting, A.B.; Seponski, D.M. Global mental health, traumatic stress, and displaced families. In The Handbook of Systemic Family Therapy: Systemic Family Therapy and Global Health Issues; Wampler, K.S., Rastogi, M., Singh, R., Eds.; Wiley Blackwell: London, UK, 2020; Volume 4, pp. 215–241. [Google Scholar]
- Landau, J.; Mittal, M.; Wieling, E. Linking Human Systems: Strengthening Individuals, Families, and Communities in the Wake of Mass Trauma. J. Marital Fam. Ther. 2008, 34, 193–209. [Google Scholar] [CrossRef]
- Whyte, M.U.D.L.O. Cultural Differences in Conflict Styles: Vietnamese Refugees and Established Residents. Howard J. Commun. 1998, 9, 57–68. [Google Scholar] [CrossRef]
- Rees, S.; Fisher, J. COVID-19 and the Mental Health of People from Refugee Backgrounds. Int. J. Health Serv. 2020, 50, 415–417. [Google Scholar] [CrossRef]
- Rychetnik, L.; Frommer, M.; Hawe, P.; Shiell, A. Criteria for evaluating evidence on public health interventions. J. Epidemiol. Commun. Health 2002, 56, 119–127. [Google Scholar] [CrossRef]
- Bhugra, D.; Gupta, S. Migration and Mental Health; Cambridge University Press: Cambridge, UK, 2011; ISBN 978-0-52119-077-0. [Google Scholar]
- Shannon, P.; Im, H.; Becher, E.; Simmelink, J.; Wieling, E.; O’Fallon, A. Screening for War Trauma, Torture, and Mental Health Symptoms Among Newly Arrived Refugees: A National Survey of U.S. Refugee Health Coordinators. J. Immigr. Refug. Stud. 2012, 10, 380–394. [Google Scholar] [CrossRef]
- Shannon, P.J.; Wieling, E.; McCleary, J.S.; Becher, E. Exploring the Mental Health Effects of Political Trauma with Newly Arrived Refugees. Qual. Health Res. 2014, 25, 443–457. [Google Scholar] [CrossRef]
- Schmeidl, S. Exploring the causes of forced migration: A pooled time-series analysis, 1971–1990. Soc. Sci. Q. 1997, 78, 284–308. [Google Scholar]
- Black, R.; Adger, W.N.; Arnell, N.W.; Dercon, S.; Geddes, A.; Thomas, D. The effect of environmental change on human migration. Glob. Environ. Change 2011, 21, S3–S11. [Google Scholar] [CrossRef]
- Berthold, S.M.; Kong, S.; Mollica, R.F.; Kuoch, T.; Scully, M.; Franke, T. Comorbid Mental and Physical Health and Health Access in Cambodian Refugees in the US. J. Community Health 2014, 39, 1045–1052. [Google Scholar] [CrossRef]
- Shannon, P.J.; Wieling, E.; Simmelink-McCleary, J.; Becher, E. Beyond Stigma: Barriers to Discussing Mental Health in Refugee Populations. J. Loss Trauma 2014, 20, 281–296. [Google Scholar] [CrossRef]
- Bogic, M.; Njoku, A.; Priebe, S. Long-term mental health of war-refugees: A systematic literature review. BMC Int. Health Hum. Rights 2015, 15, 29. [Google Scholar] [CrossRef] [Green Version]
- Kim, W. Beyond Trauma: Post-resettlement Factors and Mental Health Outcomes among Latino and Asian Refugees in the United States. J. Immigr. Minor. Health 2015, 18, 740–748. [Google Scholar] [CrossRef]
- Sangalang, C.C.; Becerra, D.; Mitchell, F.M.; Lechuga-Peña, S.; Lopez, K.; Kim, I. Trauma, Post-Migration Stress, and Mental Health: A Comparative Analysis of Refugees and Immigrants in the United States. J. Immigr. Minor. Health 2018, 21, 909–919. [Google Scholar] [CrossRef] [Green Version]
- Carlson, E.B.; Rosser-Hogan, R. Trauma experiences, posttraumatic stress, dissociation, and depression in Cambodian refugees. Am. J. Psychiatry 1991, 148, 1548–1551. [Google Scholar] [CrossRef]
- Fazel, M.; Wheeler, J.; Danesh, J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. Lancet 2005, 365, 1309–1314. [Google Scholar] [CrossRef]
- Kirmayer, L.J.; Narasiah, L.; Munoz, M.; Rashid, M.; Ryder, A.G.; Guzder, J.; Hassan, G.; Rousseau, C.; Pottie, K. Common mental health problems in immigrants and refugees: General approach in primary care. Can. Med. Assoc. J. 2010, 183, E959–E967. [Google Scholar] [CrossRef] [Green Version]
- Mollica, R.F.; Wyshak, G.; Lavelle, J. The psychosocial impact of war trauma and torture on Southeast Asian refugees. Am. J. Psychiatry 1987, 144, 1567–1572. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.E.; Davidson, G.R.; Schweitzer, R.D. Review of refugee mental health interventions following resettlement: Best practices and recommendations. Am. J. Orthopsychiatry 2010, 80, 576–585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tracy, M.; Norris, F.H.; Galea, S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depress. Anxiety 2011, 28, 666–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berthold, S.M.; Loomis, A.M.; Kuoch, T.; Scully, M.; Hin-McCormick, M.M.; Casavant, B.; Buckley, T. Social Disconnection as a Risk Factor for Health among Cambodian Refugees and Their Offspring in the United States. J. Immigr. Minor. Health 2018, 21, 290–298. [Google Scholar] [CrossRef]
- Cohen, J.A.; Perel, J.M.; Debellis, M.D.; Friedman, M.J.; Putnam, F.W. Treating Traumatized Children: Clinical implications of the psychobiology of posttraumatic stress disorder. Trauma Violence Abuse 2002, 3, 91–108. [Google Scholar] [CrossRef]
- Hinton, D.; Ba, P.; Peou, S.; Um, K. Panic disorder among Cambodian refugees attending a psychiatric clinic. Gen. Hosp. Psychiatry 2000, 22, 437–444. [Google Scholar] [CrossRef]
- Hinton, D.E.; Nickerson, A.; Bryant, R.A. Worry, worry attacks, and PTSD among Cambodian refugees: A path analysis investigation. Soc. Sci. Med. 2011, 72, 1817–1825. [Google Scholar] [CrossRef] [Green Version]
- Pears, K.C.; Capaldi, D.M. Intergenerational transmission of abuse: A two-generational prospective study of an at-risk sample. Child Abuse Negl. 2001, 25, 1439–1461. [Google Scholar] [CrossRef]
- Rowland-Klein, D.; Dunlop, R. The Transmission of Trauma across Generations: Identification with Parental Trauma in Children of Holocaust Survivors. Aust. N. Z. J. Psychiatry 1998, 32, 358–369. [Google Scholar] [CrossRef]
- Yehuda, R.; Halligan, S.L.; Grossman, R. Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Dev. Psychopathol. 2001, 13, 733–753. [Google Scholar] [CrossRef]
- Hinton, D.; Barlow, D.H.; Reis, R.; de Jong, J. A transcultural model of the centrality of “thinking a lot” in psychopathologies across the globe and the process of localization: A Cambodian refugee example. Cult. Med. Psychiatry 2016, 40, 570–619. [Google Scholar] [CrossRef]
- Arnsten, A.F.T. Stress signalling pathways that impair prefrontal cortex structure and function. Nat. Rev. Neurosci. 2009, 10, 410–422. [Google Scholar] [CrossRef]
- Elbert, T.; Schauer, M.; Ruf, M.; Weierstall, R.; Neuner, F.; Rockstroh, B.; Junghöfer, M. The Tortured Brain: Imaging neural representations of traumatic stress experiences using RSVP with affective pictorial stimuli. J. Psychol. 2011, 219, 167–174. [Google Scholar] [CrossRef]
- Kozlowska, K.; Walker, P.; McLean, L.; Carrive, P. Fear and the Defense Cascade: Clinical implications and management. Harv. Rev. Psychiatry 2015, 23, 263–287. [Google Scholar] [CrossRef]
- Schauer, M.; Elbert, T. Dissociation following traumatic stress: Etiology and treatment. J. Psychol. 2010, 218, 109–127. [Google Scholar] [CrossRef]
- van der Kolk, B.A. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma; Penguin Books: New York, NY, USA, 2015; pp. 51–89. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Monson, C.M.; Taft, C.T.; Fredman, S.J. Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clin. Psychol. Rev. 2009, 29, 707–714. [Google Scholar] [CrossRef] [Green Version]
- Hanson-Bradley, C.; Wieling, E. Mental health. In Immigrant and Refugee Families: Global Perspectives on Displacement and Resettlement Experiences, 2nd ed.; Ballard, J., Wieling, E., Solheim, C., Dwanyen, L., Eds.; University of Minnesota Libraries Publishing: Minneapolis, MN, USA, 2020; pp. 99–124. [Google Scholar]
- Catani, C. Krieg im Zuhause—Ein Überblick zum Zusammenhang zwischen Kriegstraumatisierung und familiärer Gewalt. Verhaltenstherapie 2009, 20, 19–27. [Google Scholar] [CrossRef]
- Walsh, F. Traumatic loss and major disasters: Strengthening family and community resilience. Fam. Process 2007, 46, 207–227. [Google Scholar] [CrossRef]
- McIlwaine, F.; O’Sullivan, K. ‘Riding the Wave’: Working Systemically with Traumatised Families. Aust. N. Z. J. Fam. Ther. 2015, 36, 310–324. [Google Scholar] [CrossRef]
- Nickerson, A.; Bryant, R.A.; Brooks, R.; Steel, Z.; Silove, D.; Chen, J. The familial influence of loss and trauma on refugee mental health: A multilevel path analysis. J. Trauma. Stress 2011, 24, 25–33. [Google Scholar] [CrossRef]
- Weine, S.; Muzurovic, N.; Kulauzovic, Y.; Besic, S.; Lezic, A.; Mujagic, A.; Muzurovic, J.; Spahovic, D.; Feetham, S.; Ware, N.; et al. Family Consequences of Refugee Trauma. Fam. Process 2004, 43, 147–160. [Google Scholar] [CrossRef] [PubMed]
- Taft, C.T.; Schumm, J.A.; Panuzio, J.; Proctor, S.P. An examination of family adjustment among Operation Desert Storm veterans. J. Consult. Clin. Psychol. 2008, 76, 648–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ballard, J.; Witham, M.; Mittal, M. Intimate partner violence among immigrants and refugees. In Immigrant and Refugee Families: Global Perspectives on Displacement and Resettlement Experiences, 2nd ed.; Ballard, J., Wieling, E., Solheim, C., Dwanyen, L., Eds.; University of Minnesota Libraries Publishing: Minneapolis, MN, USA, 2020; pp. 125–150. [Google Scholar]
- Catani, C.; Jacob, N.; Schauer, E.; Kohila, M.; Neuner, F. Family violence, war, and natural disasters: A study of the effect of extreme stress on children’s mental health in Sri Lanka. BMC Psychiatry 2008, 8, 33. [Google Scholar] [CrossRef] [Green Version]
- Catani, C.; Schauer, E.; Elbert, T.; Missmahl, I.; Bette, J.-P.; Neuner, F. War trauma, child labor, and family violence: Life adversities and PTSD in a sample of school children in Kabul. J. Trauma. Stress 2009, 22, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Catani, C.; Schauer, E.; Neuner, F. Beyond Individual War Trauma: Domestic Violence against Children in Afghanistan and Sri Lanka. J. Marital Fam. Ther. 2008, 34, 165–176. [Google Scholar] [CrossRef]
- Morgan, E.; Wieling, E.; Hubbard, J.; Kraus, E. The Development and Implementation of a Multi-Couple Therapy Model with Torture Survivors in the Democratic Republic of the Congo. J. Marital Fam. Ther. 2017, 44, 235–247. [Google Scholar] [CrossRef]
- Siegel, J.P. Breaking the Links in Intergenerational Violence: An Emotional Regulation Perspective. Fam. Process 2013, 52, 163–178. [Google Scholar] [CrossRef]
- Gershoff, E.T. Corporal punishment by parents and associated child behaviors and experiences: A meta-analytic and theoretical review. Psychol. Bull. 2002, 128, 539–579. [Google Scholar] [CrossRef]
- Beardslee, W.R.; Gladstone, T.R.G.; Wright, E.J.; Cooper, A.B. A Family-Based Approach to the Prevention of Depressive Symptoms in Children at Risk: Evidence of Parental and Child Change. Pediatrics 2003, 112, e119–e131. [Google Scholar] [CrossRef] [Green Version]
- Gewirtz, A.; Forgatch, M.; Wieling, E. Parenting Practices as Potential Mechanisms for Child adjustment Following Mass Trauma. J. Marital Fam. Ther. 2008, 34, 177–192. [Google Scholar] [CrossRef]
- Wieling, E.; Mehus, C.; Möllerherm, J.; Neuner, F.; Achan, L.; Catani, C. Assessing the Feasibility of Providing a Parenting Intervention for War-Affected Families in Northern Uganda. Fam. Community Health 2015, 38, 252–267. [Google Scholar] [CrossRef]
- Ferguson, C.J. Spanking, corporal punishment and negative long-term outcomes: A meta-analytic review of longitudinal studies. Clin. Psychol. Rev. 2013, 33, 196–208. [Google Scholar] [CrossRef]
- Slep, A.M.S.; O’Leary, S.G. Multivariate models of mothers’ and fathers’ aggression toward their children. J. Consult. Clin. Psychol. 2007, 75, 739–751. [Google Scholar] [CrossRef]
- Smith, J.R. Correlates and Consequences of Harsh Discipline for Young Children. Arch. Pediatr. Adolesc. Med. 1997, 151, 777–786. [Google Scholar] [CrossRef]
- Catani, C.; Gewirtz, A.H.; Wieling, E.; Schauer, E.; Elbert, T.; Neuner, F. Tsunami, War, and Cumulative Risk in the Lives of Sri Lankan Schoolchildren. Child Dev. 2010, 81, 1176–1191. [Google Scholar] [CrossRef]
- Carlson, E.B.; Dalenberg, C.J. A Conceptual Framework for the Impact of Traumatic Experiences. Trauma Violence Abuse 2000, 1, 4–28. [Google Scholar] [CrossRef]
- Walsh, F. A Family Resilience Framework: Innovative Practice Applications. Fam. Relat. 2002, 51, 130–137. [Google Scholar] [CrossRef] [Green Version]
- Masten, A.S. Resilience in developmental systems: Principles, pathways, and protective processes in research and practice. In Multisystemic Resilience: Adaptation and Transformation in Contexts of Change; Ungar, M., Ed.; Oxford University Press: London, UK, 2021; pp. 113–134. [Google Scholar]
- Ungar, M. Resilience, Trauma, Context, and Culture. Trauma Violence Abuse 2013, 14, 255–266. [Google Scholar] [CrossRef]
- Wieling, E. Family Interventions for Populations Exposed to Traumatic Stress Related to War and Violence. J. Marital Fam. Ther. 2017, 44, 189–192. [Google Scholar] [CrossRef]
- Paat, Y.-F. Working with Immigrant Children and Their Families: An Application of Bronfenbrenner’s Ecological Systems Theory. J. Hum. Behav. Soc. Environ. 2013, 23, 954–966. [Google Scholar] [CrossRef]
- Ballard, J.; Wieling, E.; Forgatch, M. Feasibility of Implementation of a Parenting Intervention with Karen Refugees Resettled from Burma. J. Marital Fam. Ther. 2017, 44, 220–234. [Google Scholar] [CrossRef]
- Ballard, J.; Wieling, E.; Dwanyen, L. Parenting Practices in the Karen Refugee Community. Int. J. Fam. Ther. 2019, 42, 95–107. [Google Scholar] [CrossRef]
- El-Khani, A.; Haar, K.; Stojanovic, M.; Maalouf, W. Assessing the Feasibility of Providing a Family Skills Intervention, “Strong Families”, for Refugee Families Residing in Reception Centers in Serbia. Int. J. Environ. Res. Public Health 2021, 18, 4530. [Google Scholar] [CrossRef] [PubMed]
- Puffer, E.S.; Annan, J.; Sim, A.; Salhi, C.; Betancourt, T.S. The impact of a family skills training intervention among Burmese migrant families in Thailand: A randomized controlled trial. PLoS ONE 2017, 12, e0172611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Betancourt, T.S.; Berent, J.M.; Freeman, J.; Frounfelker, R.L.; Brennan, R.T.; Abdi, S.; Maalim, A.; Abdi, A.; Mishra, T.; Gautam, B.; et al. Family-Based Mental Health Promotion for Somali Bantu and Bhutanese Refugees: Feasibility and Acceptability Trial. J. Adolesc. Health 2020, 66, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Gotseva-Balgaranova, K.; Popivanov, I.D.; Mutafchieva, M. Impact evaluation of the evidence-based trauma stabilisation programme for refugee, asylum seeking and immigrant families. Zeitschrift für Psychodrama und Soziometrie 2020, 19, 147–160. [Google Scholar] [CrossRef]
- Weine, S.; Kulauzovic, Y.; Klebic, A.; Besic, S.; Mujagic, A.; Muzurovic, J.; Spahovic, D.; Sclove, S.; Pavkovic, I.; Feetham, S.; et al. Evaluating A Multiple-Family Group Access Intervention for Refugees with PTSD. J. Marital Fam. Ther. 2008, 34, 149–164. [Google Scholar] [CrossRef]
- Weine, S.M.; Raina, D.; Zhubi, M.; Delesi, M.; Huseni, D.; Feetham, S.; Kulauzovic, Y.; Mermelstein, R.; Campbell, R.T.; Rolland, J.; et al. The TAFES multi-family group intervention for Kosovar refugees: A descriptive study. J. Nerv. Ment. Dis. 2003, 191, 100–107. [Google Scholar] [CrossRef]
- Beehler, S.; Birman, D.; Campbell, R. The Effectiveness of Cultural Adjustment and Trauma Services (CATS): Generating Practice-Based Evidence on a Comprehensive, School-Based Mental Health Intervention for Immigrant Youth. Am. J. Community Psychol. 2011, 50, 155–168. [Google Scholar] [CrossRef]
- Birman, D.; Beehler, S.; Harris, E.M.; Everson, M.L.; Batia, K.; Liautaud, J.; Frazier, S.; Atkins, M.; Blanton, S.; Buwalda, J.; et al. International Family, Adult, and Child Enhancement Services (FACES): A community-based comprehensive services model for refugee children in resettlement. Am. J. Orthopsychiatry 2008, 78, 121–132. [Google Scholar] [CrossRef]
- Elswick, S.; Washington, G.; Mangrum-Apple, H.; Peterson, C.; Barnes, E.; Pirkey, P.; Watson, J. Trauma Healing Club: Utilizing Culturally Responsive Processes in the Implementation of an After-School Group Intervention to Address Trauma Among African Refugees. J. Child Adolesc. Trauma 2021, 15, 155–166. [Google Scholar] [CrossRef]
- Kataoka, S.H.; Stein, B.D.; Jaycox, L.H.; Wong, M.; Escudero, P.; Tu, W.; Zaragoza, C.; Fink, A. A School-Based Mental Health Program for Traumatized Latino Immigrant Children. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 311–318. [Google Scholar] [CrossRef] [Green Version]
- Möhlen, H.; Parzer, P.; Resch, F.; Brunner, R. Psychosocial Support for War-Traumatized Child and Adolescent Refugees: Evaluation of a Short-Term Treatment Program. Aust. N. Z. J. Psychiatry 2005, 39, 81–87. [Google Scholar] [CrossRef]
- Mollica, R.F.; Cui, X.; Mcinnes, K.; Massagli, M.P. Science-based policy for psychosocial interventions in refugee camps: A Cambodian example. J. Nerv. Ment. Dis. 2002, 190, 158–166. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J. Clin. Epidemiol. 2021, 134, 178–189. [Google Scholar] [CrossRef]
- Erdemir, E. Transactional relations and reciprocity between refugee mothers and their children: Changes in child, parenting, and concept of child. Eur. Early Child. Educ. Res. J. 2020, 29, 547–568. [Google Scholar] [CrossRef]
- Cabassa, L.J.; Baumann, A.A. A two-way street: Bridging implementation science and cultural adaptations of mental health treatments. Implement. Sci. 2013, 8, 90. [Google Scholar] [CrossRef] [Green Version]
- Bernal, G.; Bonilla, J.; Bellido, C. Ecological validity and cultural sensitivity for outcome research: Issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J. Abnorm. Child Psychol. 1995, 23, 67–82. [Google Scholar] [CrossRef]
- Powell, B.J.; Proctor, E.K.; Glass, J.E. A Systematic Review of Strategies for Implementing Empirically Supported Mental Health Interventions. Res. Soc. Work Pract. 2013, 24, 192–212. [Google Scholar] [CrossRef] [Green Version]
- Fixsen, D.L.; Blase, K.A.; Naoom, S.F.; Wallace, F. Core Implementation Components. Res. Soc. Work Pract. 2009, 19, 531–540. [Google Scholar] [CrossRef]
- Collins, P.Y.; Patel, V.; Joestl, S.S.; March, D.; Insel, T.R.; Daar, A.S.; Bordin, I.A.; Costello, E.J.; Durkin, M.; Fairburn, C.G.; et al. Grand challenges in global mental health. Nature 2011, 475, 27–30. [Google Scholar] [CrossRef] [PubMed]
- van der Velde, J.; Williamson, D.L.; Ogilvie, L.D. Participatory Action Research: Practical Strategies for Actively Engaging and Maintaining Participation in Immigrant and Refugee Communities. Qual. Health Res. 2009, 19, 1293–1302. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, M.; Hubbard, P. Walking, sensing, belonging: Ethno-mimesis as performative praxis. Vis. Stud. 2010, 25, 46–58. [Google Scholar] [CrossRef]
- Pittaway, E.; Bartolomei, L.; Hugman, R. Stop Stealing Our Stories: The Ethics of Research with Vulnerable Groups. J. Hum. Rights Pract. 2010, 2, 229–251. [Google Scholar] [CrossRef]
- Barrera, M.; Berkel, C.; Castro, F.G. Directions for the Advancement of Culturally Adapted Preventive Interventions: Local Adaptations, Engagement, and Sustainability. Prev. Sci. 2016, 18, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.M.D.; Baumann, A.; Schwartz, A.L. Cultural Adaptation of an Evidence Based Intervention: From Theory to Practice in a Latino/a Community Context. Am. J. Community Psychol. 2010, 47, 170–186. [Google Scholar] [CrossRef] [PubMed]
- Kumpfer, K.; Magalhães, C.; Xie, J. Cultural Adaptation and Implementation of Family Evidence-Based Interventions with Diverse Populations. Prev. Sci. 2016, 18, 649–659. [Google Scholar] [CrossRef]
- Powell, B.J.; Beidas, R.S.; Lewis, C.C.; Aarons, G.A.; McMillen, J.C.; Proctor, E.K.; Mandell, D.S. Methods to Improve the Selection and Tailoring of Implementation Strategies. J. Ment. Health Adm. 2015, 44, 177–194. [Google Scholar] [CrossRef] [Green Version]
- Shannon, P.; McCleary, J.; Wieling, E.; Im, H.; Becher, E.; O’Fallon, A. Exploring Mental Health Screening Feasibility and Training of Refugee Health Coordinators. J. Immigr. Refug. Stud. 2015, 13, 80–102. [Google Scholar] [CrossRef]
- Weisz, J.R.; Jensen-Doss, A.; Hawley, K. Evidence-based youth psychotherapies versus usual clinical care: A meta-analysis of direct comparisons. Am. Psychol. 2006, 61, 671–689. [Google Scholar] [CrossRef]
- Palic, S.; Elklit, A. Psychosocial treatment of posttraumatic stress disorder in adult refugees: A systematic review of prospective treatment outcome studies and a critique. J. Affect. Disord. 2011, 131, 8–23. [Google Scholar] [CrossRef]
| Keywords | Databases | Articles Found |
|---|---|---|
| We entered into each database with similar set of keywords: “Traumatic stress” OR “PTSD”, AND “Family”, AND “Prevention” OR “Intervention”, AND “Culture” OR “Refugees” OR “Immigrants”, AND “Displacement” OR “Resettlement” | APA PsycArticles | 4 |
| APA PsycInfo | 15 | |
| Social Sciences Citation Index | 38 | |
| Psychology and Behavioral Science Collection | 5 | |
| CINAHL | 4 | |
| ERIC | 0 | |
| PubMed | 3 | |
| TOTAL | 69 | |
| Other sources: Articles that met criteria for inclusion and articles from the previous review by Slobodin and de Jong (2015) [4] | 11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mak, C.; Wieling, E. A Systematic Review of Evidence-Based Family Interventions for Trauma-Affected Refugees. Int. J. Environ. Res. Public Health 2022, 19, 9361. https://doi.org/10.3390/ijerph19159361
Mak C, Wieling E. A Systematic Review of Evidence-Based Family Interventions for Trauma-Affected Refugees. International Journal of Environmental Research and Public Health. 2022; 19(15):9361. https://doi.org/10.3390/ijerph19159361
Chicago/Turabian StyleMak, Chansophal, and Elizabeth Wieling. 2022. "A Systematic Review of Evidence-Based Family Interventions for Trauma-Affected Refugees" International Journal of Environmental Research and Public Health 19, no. 15: 9361. https://doi.org/10.3390/ijerph19159361
APA StyleMak, C., & Wieling, E. (2022). A Systematic Review of Evidence-Based Family Interventions for Trauma-Affected Refugees. International Journal of Environmental Research and Public Health, 19(15), 9361. https://doi.org/10.3390/ijerph19159361






