What Does It Take to Get Somebody Back to Work after Severe Acquired Brain Injury? Service Actions within the Vocational Intervention Program (VIP 2.0)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Sample
2.2. The Vocational Intervention Program
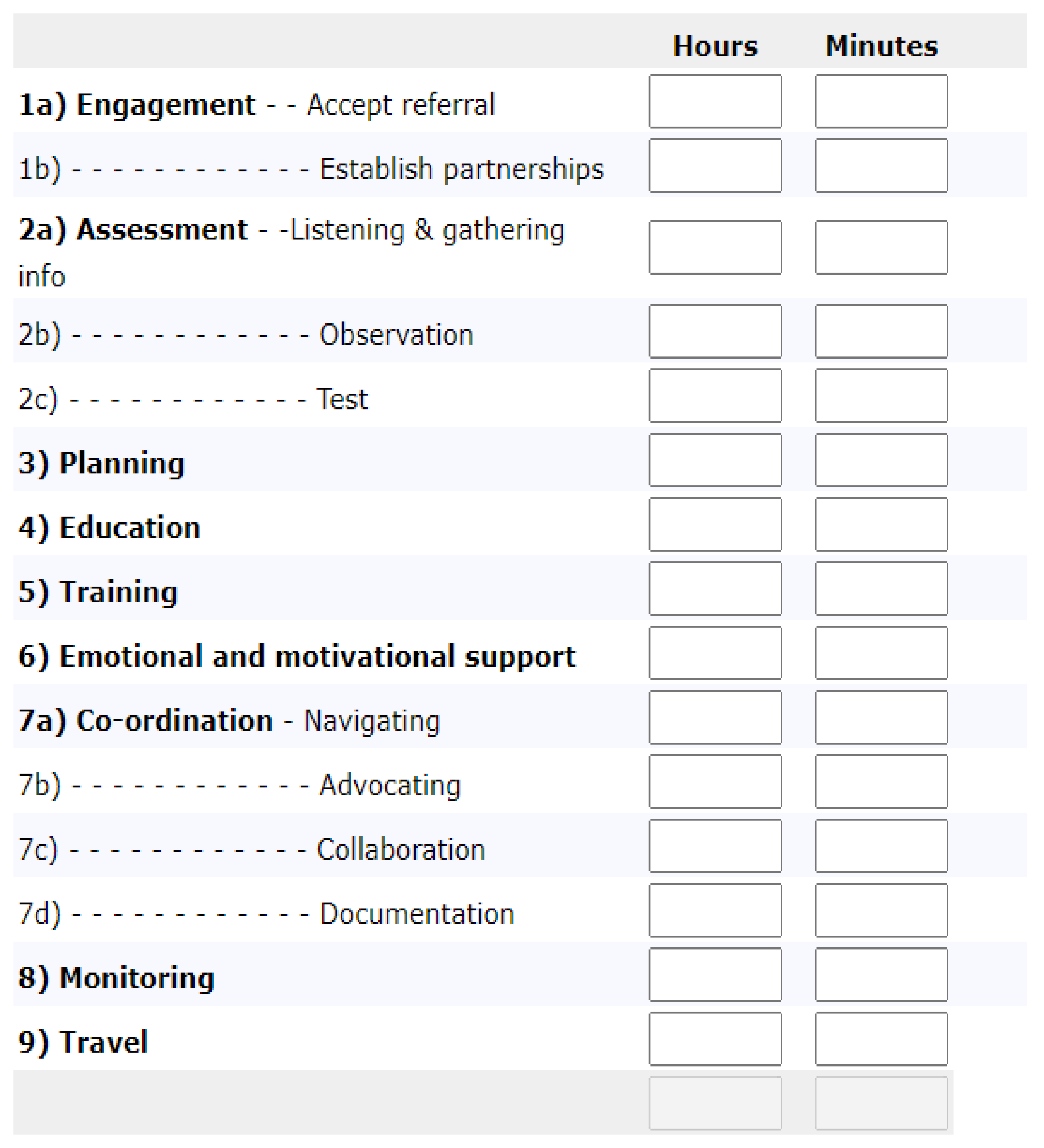
2.3. Measure
2.4. Procedures
2.4.1. Provider Selection
2.4.2. Data Collection
2.4.3. Data Analysis
3. Results
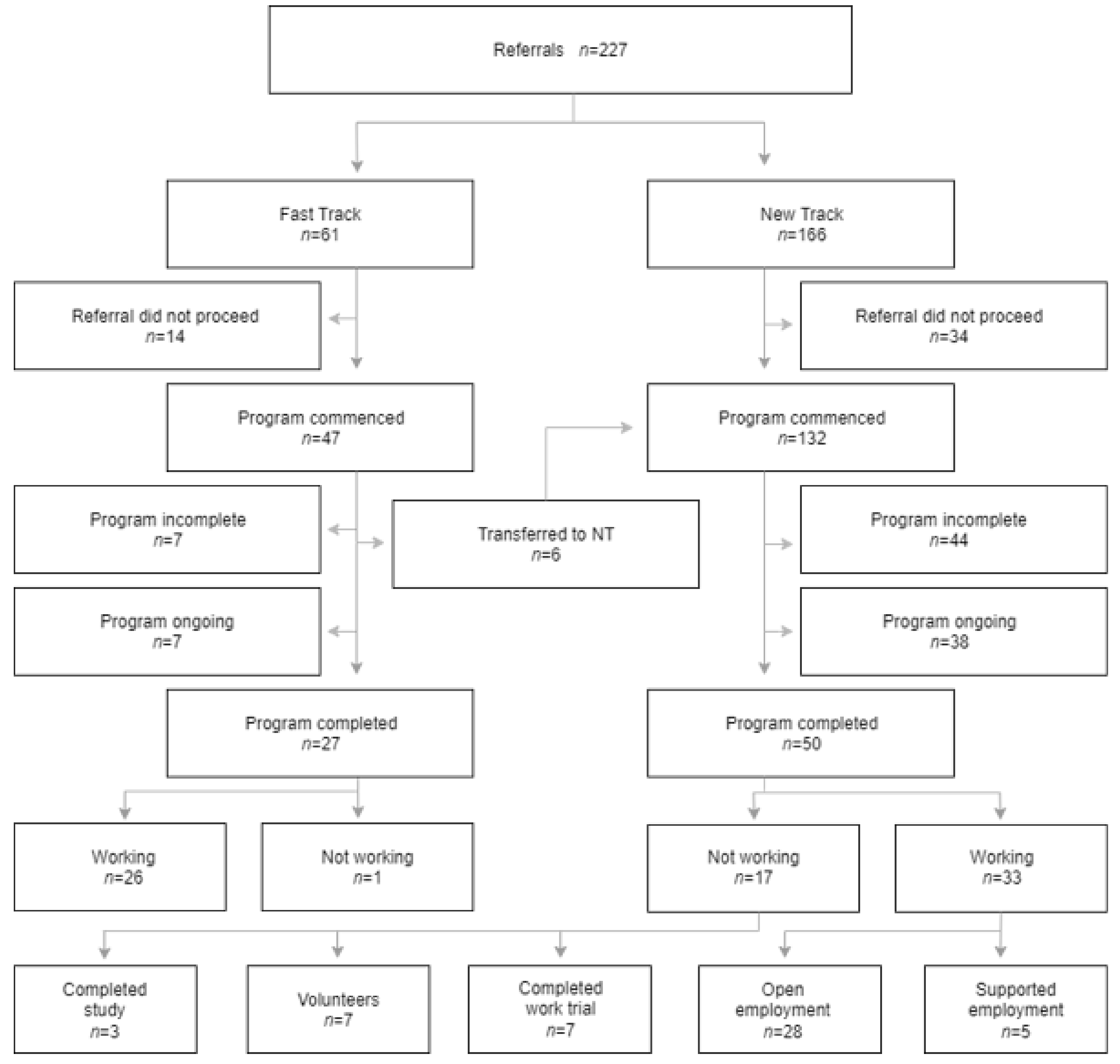
3.1. Outcomes
3.2. Service Intensity: Fast Track vs. New Track
3.3. Service Action Comparison: Fast Track vs. New Track
3.4. Service Action Comparison: DES vs. Private Providers
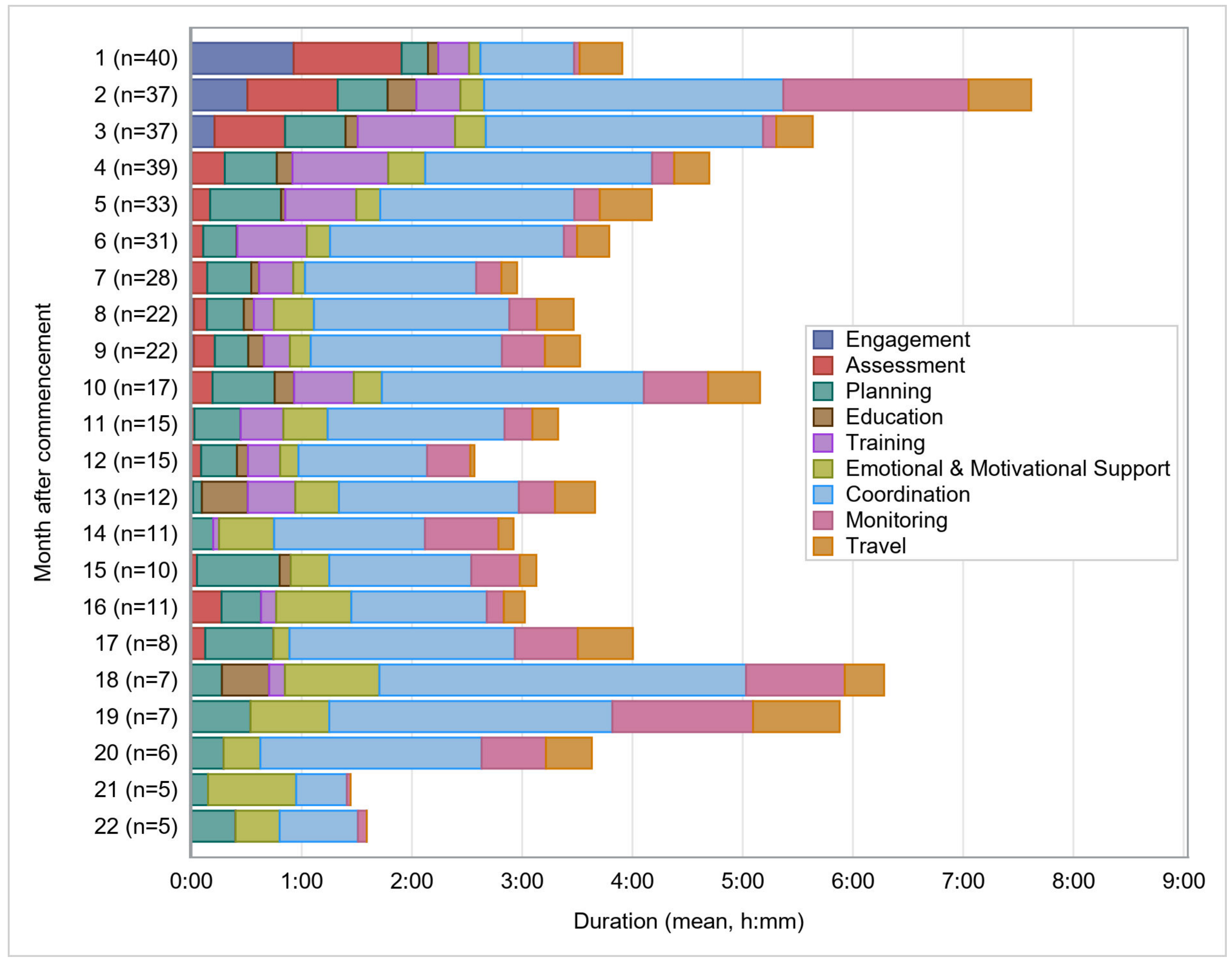
3.5. Duration
3.6. Service Actions by Pathway over Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2018, 130, 1080–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Escorpizo, R.; Brage, S.; Homa, D.; Stucki, G. Handbook of Vocational Rehabilitation and Disability Evaluation; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Access Economics. The Economic Cost of Spinal Cord Injury and Traumatic Brain Injury in Australia; Report by Access Economics for the Victorian Neurotrauma Initiative; Access Economics: Canberra, ACT, Australia, 2009. [Google Scholar]
- De Koning, M.E.; Spikman, J.M.; Coers, A.; Schönherr, M.C.; van der Naalt, J. Pathways of care the first year after moderate and severe traumatic brain injury—Discharge destinations and outpatient follow-up. Brain Inj. 2015, 294, 23–429. [Google Scholar] [CrossRef] [PubMed]
- Forslund, M.; Roe, C.; Arango-Lasprilla, J.; Sigurdardottir, S.; Andelic, N. Impact of personal and environmental factors on employment outcome two years after moderate-to-severe traumatic brain injury. J. Rehabil. Med. 2013, 45, 801–807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grauwmeijer, E.; Heijenbrok-Kal, M.H.; Haitsma, I.K.; Ribbers, G.M. A Prospective Study on Employment Outcome 3 Years After Moderate to Severe Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2012, 93, 993–999. [Google Scholar] [CrossRef]
- Ponsford, J.L.; Downing, M.; Olver, J.; Ponsford, M.; Acher, R.; Carty, M.; Spitz, G. Longitudinal Follow-Up of Patients with Traumatic Brain Injury: Outcome at Two, Five, and Ten Years Post-Injury. J. Neurotrauma 2014, 31, 64–77. [Google Scholar] [CrossRef]
- Sander, A.M.; Krentzer, J.S.; Rosenthal, M.; Delmonico, R.; Young, M.E. A Multicenter Longitudinal Investigation of Return to Work and Community Integration Following Traumatic Brain Injury. J. Head Trauma Rehabil. 1996, 11, 70–84. [Google Scholar] [CrossRef]
- Simpson, G.K.; McRae, P.; Hallab, L.; Daher, M.; Strettles, B. Participation in competitive employment after severe traumatic brain injury: New employment versus return to previous (pre-injury) employment. Neuropsychol. Rehabil. 2020, 30, 995–1012. [Google Scholar] [CrossRef]
- McRae, P.; Hallab, L.; Simpson, G. Navigating Employment Pathways and Supports Following Brain Injury in Australia: Client Perspectives. Aust. J. Rehabil. Couns. 2016, 22, 76–92. [Google Scholar] [CrossRef]
- Louise, O.R.; Fortune, N.; Australian Institute of Health and Welfare. Disability in Australia: Acquired Brain Injury; Bulletin, (55); Australian Institute of Health and Welfare: Darlinghurst, NSW, Australia, 2007. [Google Scholar]
- World Health Organization. WHO Global Strategy on Integrated People-Centred Health Services 2016–2026; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Petticrew, M. When are complex interventions ‘complex’? When are simple interventions ‘simple’? Eur. J. Public Health. 2011, 21, 298–397. [Google Scholar] [CrossRef]
- Murray, A.; Watter, K.; McLennan, V.; Vogler, J.; Nielsen, M.; Jeffery, S.; Ehlers, S.; Kennedy, A. Identifying models, processes, and components of vocational rehabilitation following acquired brain injury: A systematic scoping review. Disabil. Rehabil. 2021, 1–14. [Google Scholar] [CrossRef]
- Fadyl, J.K.; McPherson, K.M. Approaches to vocational rehabilitation after traumatic brain injury: A review of the evidence. J. Head Trauma Rehabil. 2009, 24, 195–212. [Google Scholar] [CrossRef]
- Whyte, J.; Hart, T. It’s more than a black box; it’sa Russian doll: Defining rehabilitation treatments. Am. J. Phys. Med. Rehabil. 2003, 82, 639–652. [Google Scholar] [CrossRef]
- González-Ortiz, L.G.; Calciolari, S.; Goodwin, N.; Stein, V. The Core Dimensions of Integrated Care: A literature review to support the development of a comprehensive framework for implementing integrated care. Int. J. Integr. Care 2018, 18, 10. [Google Scholar] [CrossRef] [Green Version]
- Lukersmith, S.; Millington, M.; Salvador-Carulla, L. What is Case Management? A Scoping and Mapping Review. Int. J. Integr. Care 2016, 16, 2. [Google Scholar] [CrossRef] [Green Version]
- Lukersmith, S. A Taxonomy of Case Management: Development, Dissemination and Impact; Faculty of Health Sciences, University of Sydney: Sydney, NSW, Australia, 2017. [Google Scholar]
- Lukersmith, S.; Fernandez, A.; Millington, M.; Salvador-Carulla, L. The brain injury case management taxonomy (BICM-T); A classification of community-based case management interventions for a common language. Disabil. Health J. 2015, 9, 272–280. [Google Scholar] [CrossRef] [Green Version]
- Stiekema, A.; Resch, C.; Donkervoort, M.; Jansen, N.; Jurrius, K.H.; Zadoks, J.M.; van Heugten, C.M. Case management after acquired brain injury compared to care as usual: Study protocol for a two- year pragmatic randomized controlled trial. Research Square 2020, 21, 982. [Google Scholar] [CrossRef]
- Nalder, E.J.; Saumur, T.M.; Batliwalla, Z.; Salvador-Carulla, L.; Putnam, M.; Spindel, A.; Lenton, E.; Hussein, H. A scoping review to characterize bridging tasks in the literature on aging with disability. BMC Health Serv. Res. 2020, 20, 170. [Google Scholar] [CrossRef] [Green Version]
- Stevens, H.D.G. The Effectiveness of a Case Management Approach to Care for Adults Who Suffer Trauma through Injury: Protocol for a Systematic Review. 2020. Available online: https://www.google.com.hk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwiz7J3yrar5AhWCmFYBHajJBW8QFnoECAUQAQ&url=https%3A%2F%2Fwww.cmsuk.org%2Ffiles%2FResearch%2FHeidi%2520Stevens%2520Research%2520Protocol.pdf&usg=AOvVaw1RJ1zdYteYi5T6TZDm2P4q (accessed on 11 June 2022).
- Alonso-Trujillo, F.; Salinas-Pérez, J.A.; Gutiérrez-Colosía, M.R.; González-Caballero, J.L.; Pinzón Pulido, S.; Jiménez González, S.; Gálvez Daza, P.; Martínez Domene, M.; Salvador-Carulla, L. Evaluación del impacto de un plan multisectorial de promoción de la salud y el bienestar social en Andalucía. Gac. Sanit. 2021, 34, 615–623. [Google Scholar] [CrossRef]
- Lukersmith, S.; Taylor, J.; Salvador-Carulla, L. Vagueness and ambiguity in communication of case management: A content analysis in the Australian National Disability Insurance Scheme. Int. J. Integr. Care 2021, 21. [Google Scholar] [CrossRef]
- Watter, K.; Kennedy, A.; McLennan, V.; Vogler, J.; Jeffery, S.; Murray, A.; Ehlers, S.; Nielsen, M. Consumer perspectives of vocational rehabilitation and return to work following acquired brain injury. Brain Impair. 2021, 1–21. [Google Scholar] [CrossRef]
- Simpson, G.K.; McRae, P.; Home, S.; Strettles, B.; Wyborn, J.; Daher, M.; Gates, T.; Christie, L. Vocational Intervention Program 2.0: Program Evaluation Report; South Western Sydney Local Health District: Warwick Farm, NSW, Australia, 2021. [Google Scholar]
- John Walsh Centre for Rehabilitation Research; Johnstone, D. Evaluation of the Vocational Intervention Program (VIP) Vocational Rehabilitation Services for People with Brain Injury: Evaluation Report; University of Sydney: Sydney, NSW, Australia, 2017. [Google Scholar]
- Devine, A.; Shields, M.; Dimov, S.; Dickinson, H.; Vaughan, C.; Bentley, R.; LaMontagne, A.D.; Kavanagh, A. Australia’s Disability Employment Services Program: Participant Perspectives on Factors Influencing Access to Work. Int. J. Environ. Res. Public Health 2021, 18, 11485. [Google Scholar] [CrossRef]
- NSW State Insurance Regulatory Authority. Statistical Bulletin, 2015–2016; NSW State Insurance Regulatory Authority: Sydney, NSW, Australia, 2018. [Google Scholar]
- Department of Employment. Disability Employment Services: DES Monthly Data. Australian Government, Canberra, Australia. Available online: https://data.gov.au/dataset/ds-dga-e258b678-eb6b-4ebb-92d8-0fe7c1122c42/details (accessed on 11 June 2022).
- Tate, R.L.; Simpson, G.K.; McRae, P. Traumatic brain injury. In Handbook of Vocational Rehabilitation and Disability Evaluation: Application and Implementation of the ICF; Escorpizo, B.S., Homa, R., Stucki, G.D., Eds.; Springer: New York, NY, USA, 2015. [Google Scholar]
- Simpson, G.K.; Daher, M.; Hodgkinson, A.; Strettles, B. Comparing the injury profile, service use, outcomes, and comorbidities of people with severe TBI across urban, regional, and remote populations in New South Wales: A multicentre study. J. Head Trauma Rehabil. 2016, 31, E26–E38. [Google Scholar] [CrossRef]
- Kopke, S.; McCleery, J. Systematic Reviews of Case Management: Too Complex to Manage? Cochrane Database Syst. Rev. 2015, 1, ED000096. [Google Scholar] [PubMed]
- WHO ICHI Development Project. International Classification of Health Interventions (ICHI) Alpha 2 Version 2013. Available online: http://sydney.edu.au/health-sciences/ncch/about.shtml (accessed on 11 June 2022).
- Howe, E.I.; Andelic, N.; Fure, S.C.R.; Røe, C.; Søberg, H.L.; Hellstrøm, T.; Spjelkavik, Ø.; Enehaug, H.; Lu, J.; Ugelstad, H.; et al. Cost-effectiveness analysis of combined cognitive and vocational rehabilitation in patients with mild-to-moderate TBI: Results from a randomized controlled trial. BMC Health Serv. Res. 2022, 22, 1–13. [Google Scholar] [CrossRef]
- Wehman, P.; Kregel, J.; Keyser-Marcus, L.; Sherron-Targett, P.; Campbell, L.; West, M.; Cifu, D. Supported employment for persons with traumatic brain injury: A preliminary investigation of long-term follow-up costs and program efficiency. Arch. Phys. Med. Rehabil. 2003, 84, 192–196. [Google Scholar] [CrossRef] [Green Version]
- Radford, K.; Phillips, J.; Drummond, A.; Sach, T.; Walker, M.; Tyerman, A.; Haboubi, N.; Jones, T. Return to work after traumatic brain injury: Cohort comparison and economic evaluation. Brain Inj. 2013, 27, 507–520. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J.H.; Zuger, R.R.; Fields, A.; Fraser, R.; Pruce, T. The program without walls: Innovative approach to state agency vocational rehabilitation of persons with traumatic brain injury. Arch. Phys. Med. Rehabil. 2004, 85, 68–72. [Google Scholar] [CrossRef]
- Tyerman, A. Vocational rehabilitation after traumatic brain injury: Models and services. NeuroRehabilitation 2012, 31, 51–62. [Google Scholar] [CrossRef]
- O’Brien, L. Achieving a successful and sustainable return to the workforce after ABI: A client-centred approach. Brain Inj. 2007, 21, 465–478. [Google Scholar] [CrossRef]
- Trexler, L.E.; Trexler, L.C.; Malec, J.F.; Klyce, D.; Parrott, D. Prospective randomized controlled trial of resource facilitation on community participation and vocational outcome following brain injury. J. Head Trauma Rehabil. 2010, 25, 440–446. [Google Scholar] [CrossRef]
- Hajfey, W.J.; Abrams, D.L. Employment outcomes for participants in a brain injury work reentry program: Preliminary findings. J. Head Trauma Rehabil. 1991, 6, 24–34. [Google Scholar] [CrossRef]
- World Health Organization. People-Centred and Integrated Health Services: An Overview of the Evidence; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Schneider, C.H.; Sturmberg, J.; Gillespie, J.; Wilson, A.; Lukersmith, S.; Salvador-Carulla, L. What is the State of the Art in Person-Centred Care? An Expert Commentary; A Report for an Australian Government Policy Agency; Menzies Centre for Health Policy and F.O.H. Sciences; University of Sydney: Sydney, NSW, Australia, 2016. [Google Scholar]
- Murphy, L.; Chamberlain, E.; Weir, J.; Berry, A.; Nathaniel-James, D.; Agnew, R. Effectiveness of vocational rehabilitation following acquired brain injury: Preliminary evaluation of a UK specialist rehabilitation programme. Brain Inj. 2006, 20, 1119–1129. [Google Scholar] [CrossRef] [PubMed]
- Gamble, D.; Moore, C.L. Supported employment: Disparities in vocational rehabilitation outcomes, expenditures and service time for persons with traumatic brain injury. J. Vocat. Rehabil. 2003, 19, 47–57. [Google Scholar]
- Wall, J.R.; Niemczura, J.G.; Rosenthal, M. Community-based training and employment: An effective program for persons with traumatic brain injury. NeuroRehabilitation 1998, 10, 39–49. [Google Scholar] [CrossRef]
- Davis, L.C.; Sander, A.M.; Bogaards, J.A.; Pappadis, M.R. Implementation of resource facilitation to assess referral needs and promote access to state vocational rehabilitation services in people with traumatic brain injury. Neuropsychol. Rehabil. 2018, 28, 1145–1160. [Google Scholar] [CrossRef]

| Circumstance | Components Description and Examples |
|---|---|
| Whom | focus or target of the case management action—which may be the person with the health condition, e.g., brain injury OR the employer OR workplace supervisor OR the training provider |
| Why | purpose of the case management service, e.g., to return to work in the same job, OR to return to work in a different job OR engage in purposeful occupation |
| When | timing and frequency in relation to the person and employer need |
| What context | person’s OR training provider OR workplace context |
| How (service) | theoretical underpinnings/model, e.g., strengths based, managed/administrative, broker model |
| Where | office OR workplace based OR community based |
| How (skills) | Case manager qualifications and skills (e.g., health or social care or work health and safety) |
| Whom (sector) | Across a range of health services, social services, education providers, transport, employment related and workplace based services |
| What action | the case manager interventions, what they do/the actions |
| Main Category | Sub-Category | Description |
|---|---|---|
| Engagement | Accept Referral | Time spent matching the client to consultant and funding system to commence servicing. |
| Establish Partnerships | Connecting with the client, family and others to establish a relationship, and develop partnerships. | |
| Assessment | Listening and Gathering Information | Initial assessment and gathering background information from the client and relevant others (incl. verbal and written reports from BIRP case managers s, employers). |
| Observation | Watching to acquire information about the work environment and/or client’s functioning. | |
| Test | Evaluating the client’s health using an assessment instrument (e.g., functioning assessment, vocational assessment). | |
| Planning | - | Setting goals, priorities, actions and responsibilities with the client, employer, BIRP case managers s, funding coordinator and relevant others. |
| Education | - | Providing information to the client and employer to improve understanding. |
| Training | - | Teaching or developing the client’s skills (workplace, interview skills, work behaviours, etc.) |
| Emotional and Motivational Support | - | Supporting the client’s employment through vocational counselling and encouragement. |
| Co-Ordination | Navigating | Researching and arranging the most appropriate option (incl. canvassing for work trainings, job seeking, facilitating training courses, negotiating RTW upgrades, etc.) |
| Advocating | Supporting the client in negotiations. | |
| Collaboration | Consulting, providing feedback and working with other service providers (incl. BIRPs, insurers, care agencies). | |
| Documentation | Recording notes and report writing. | |
| Monitoring | - | Continuous acquisition of information to monitor progress (with client, employer, other parties. Includes phone, email, face to face, worksite). |
| Travel | - | All travel related to servicing the client. |
| Variables | Total Sample (n = 173) | Fast Track (n = 47) | New Track (n = 126) | Test |
|---|---|---|---|---|
| Sex (n, %) | ||||
| Male | 125 (72.25%) | 33 (70.21%) | 92 (73.02%) | Χ2 = 0.13 p = 0.71 |
| Female | 48 (27.75%) | 14 (29.79%) | 34 (26.98%) | |
| Age at Program Start (Years) | ||||
| M (SD) | 38.50 (13.87) | 39.45 (14.02) | 38.15 (13.86) | t = −0.55 p = 0.59 |
| Med (IQR) | 37 (24.5) | 38 (26) | 36 (24.25) | |
| Range | 18–67 | 18–67 | 18–67 | |
| Time Post-Injury (Months) | ||||
| M (SD) | 33.79 (54.62) | 11.02 (14.94) | 42.28 (61.28) | U = 1286.50 p < 0.0001 |
| Med (IQR) | 13 (25) | 8 (7) | 18.5 (34.25) | |
| Range | 2–309 | 2–103 | 3–309 | |
| Marital Status (n, %) | (n = 171) | (n = 46) | (n = 125) | |
| Married/De Facto | 69 (40.35%) | 23 (50.00%) | 46 (36.80%) | Χ2 = 2.67 p = 0.26 |
| Single | 90 (52.63%) | 21 (45.65%) | 69 (55.20%) | |
| Separated/Divorced | 12 (7.02%) | 2 (4.35%) | 10 (8.00%) | |
| Years of Pre-Injury Education | (n = 117) | (n = 26) | (n = 91) | |
| M (SD) | 12.80 (2.50) | 12.88 (2.67) | 12.78 (2.46) | t = −0.19 p = 0.85 |
| Med (IQR) | 12 (4) | 12 (6) | 12 (4) | |
| Range | 8–19 | 9–18 | 8–19 | |
| Highest Education Achieved | (n = 154) | (n = 45) | (n = 109) | |
| Year 10 or less | 50 (32.47%) | 17 (37.78%) | 33 (30.28%) | Χ2 = 0.86 p = 0.84 |
| Year 12 | 31 (20.13%) | 8 (17.78%) | 23 (21.10%) | |
| TAFE | 41 (26.62%) | 11 (24.44%) | 30 (27.52%) | |
| University | 32 (20.78%) | 9 (20.00%) | 23 (21.10%) | |
| Employed at Injury (n, %) | ||||
| Employed | 133 (76.88%) | 46 (97.87%) | 87 (69.05%) | Χ2 = 16.00 p < 0.0001 |
| Not Employed | 40 (23.12%) | 1 (2.13%) | 39 (30.95%) | |
| Location | ||||
| Metropolitan * | 70 (40.46%) | 23 (48.94%) | 47 (37.30%) | Χ2 = 1.92 p = 0.17 |
| Rural/Regional | 103 (59.54%) | 24 (51.06%) | 79 (62.70%) | |
| Funding Source ** | ||||
| iCare | 63 (36.42%) | 18 (38.30%) | 45 (35.71%) | Χ2 = 4.82 p = 0.31 |
| Other Insurance | 10 (5.78%) | 5 (10.64%) | 5 (3.97%) | |
| NDIS | 12 (6.94%) | 3 (6.38%) | 9 (7.14%) | |
| DES | 61 (35.26%) | 17 (36.17%) | 44 (34.92%) | |
| Project Funding | 27 (15.60%) | 4 (8.51%) | 23 (18.25%) | |
| Type of Injury (n, %) | ||||
| TBI | 125 (72.25%) | 37 (78.72%) | 88 (69.84%) | Χ2 = 1.35 p = 0.25 |
| ABI | 48 (27.75%) | 10 (21.28%) | 38 (30.16%) | |
| PTA Duration (Days) (TBI Only) | (n = 108) | (n = 34) | (n = 74) | |
| M (SD) | 35.63 (39.83) | 34.94 (46.73) | 35.95 (36.58) | U = 1058.00 p = 0.19 |
| Med (IQR) | 22 (31) | 14.5 (38) | 26 (30) | |
| Range | <1–183 | 1–183 | <1–183 | |
| TBI Severity (PTA) (n, %) | (n = 111) | (n = 34) | (n = 77) | |
| Mild/Moderate (<1 day) | 5 (4.50%) | 2 (5.88%) | 3 (3.90%) | Χ2 = 3.42 p = 0.33 |
| Severe (1–7 days) | 14 (12.60%) | 7 (20.59%) | 7 (9.09%) | |
| Very Severe (8–28 days) | 44 (39.64%) | 13 (38.24%) | 31 (40.26%) | |
| Extremely Severe (>28 days) | 48 (43.24%) | 12 (35.29%) | 36 (46.75%) |
| Category | Fast Track (n = 25) | New Track (n = 47) | One Sided Wilcoxon Rank-Sum Test | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median | Min | Max | % of Total | Median | Min | Max | % of Total | W | p-Value | |
| Engagement | 01:12 | 00:00 | 02:50 | 3.7 | 01:05 | 00:00 | 06:30 | 3.7 | 545.0 | 0.309 |
| Assessment | 03:00 | 00:00 | 12:20 | 11.9 | 02:30 | 00:00 | 30:15 | 8.4 | 654.0 | 0.786 |
| Planning | 01:15 | 00:00 | 12:40 | 9.4 | 02:00 | 00:00 | 17:00 | 9.1 | 573.0 | 0.434 |
| Education | 00:00 | 00:00 | 02:00 | 1.0 | 00:00 | 00:00 | 06:00 | 2.4 | 457.0 | 0.045 |
| Training | 00:00 | 00:00 | 02:05 | 0.4 | 00:00 | 00:00 | 70:00 | 9.2 | 361.0 | 0.001 |
| Emotional and Motivational Support | 01:00 | 00:00 | 09:30 | 7.3 | 00:18 | 00:00 | 20:00 | 6.1 | 617.0 | 0.644 |
| Coordination | 09:54 | 00:00 | 50:10 | 41.7 | 14:24 | 00:25 | 78:00 | 42.3 | 461.0 | 0.068 |
| Monitoring | 03:55 | 00:00 | 12:30 | 13.5 | 01:24 | 00:00 | 60:00 | 10.0 | 740.0 | 0.965 |
| Travel | 02:10 | 00:00 | 12:15 | 11.1 | 02:00 | 00:00 | 24:00 | 8.7 | 634.0 | 0.712 |
| Total | 25:05 | 03:00 | 95:49 | 35:30 | 02:30 | 134:00 | 446.0 | 0.048 | ||
| Category | DES Providers (n = 27) | Private Providers (n = 44) | Two Sided Wilcoxon Rank-Sum Test | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median | Min | Max | % of Total | Median | Min | Max | % of Total | W | p-Value | |
| Engagement | 01:30 | 00:00 | 06:30 | 4.8 | 00:50 | 00:00 | 03:00 | 2.8 | 826.0 | 0.006 |
| Assessment | 04:15 | 00:00 | 30:15 | 12.3 | 02:27 | 00:00 | 06:24 | 7.1 | 761.5 | 0.048 |
| Planning | 04:30 | 00:00 | 17:00 | 12.0 | 01:00 | 00:00 | 15:48 | 7.2 | 846.5 | 0.003 |
| Education | 00:15 | 00:00 | 04:00 | 2.1 | 00:00 | 00:00 | 06:00 | 2.0 | 678.0 | 0.275 |
| Training | 00:00 | 00:00 | 70:00 | 8.8 | 00:00 | 00:00 | 30:30 | 5.4 | 708.0 | 0.115 |
| Emotional and Motivational Support | 03:15 | 00:00 | 20:00 | 9.9 | 00:00 | 00:00 | 17:30 | 3.9 | 903.0 | <0.001 |
| Coordination | 10:05 | 00:00 | 78:00 | 35.5 | 13:25 | 01:42 | 63:42 | 46.5 | 551.5 | 0.619 |
| Monitoring | 03:30 | 00:00 | 22:00 | 9.3 | 01:45 | 00:00 | 60:00 | 12.3 | 679.0 | 0.315 |
| Travel | 01:20 | 00:00 | 12:05 | 5.2 | 02:45 | 00:00 | 24:00 | 12.8 | 440.5 | 0.069 |
| Total | 36:20 | 03:00 | 134:00 | 29:05 | 02:30 | 121:30 | 710.5 | 0.169 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McRae, P.; Kobel, C.; Lukersmith, S.; Simpson, G. What Does It Take to Get Somebody Back to Work after Severe Acquired Brain Injury? Service Actions within the Vocational Intervention Program (VIP 2.0). Int. J. Environ. Res. Public Health 2022, 19, 9548. https://doi.org/10.3390/ijerph19159548
McRae P, Kobel C, Lukersmith S, Simpson G. What Does It Take to Get Somebody Back to Work after Severe Acquired Brain Injury? Service Actions within the Vocational Intervention Program (VIP 2.0). International Journal of Environmental Research and Public Health. 2022; 19(15):9548. https://doi.org/10.3390/ijerph19159548
Chicago/Turabian StyleMcRae, Philippa, Conrad Kobel, Sue Lukersmith, and Grahame Simpson. 2022. "What Does It Take to Get Somebody Back to Work after Severe Acquired Brain Injury? Service Actions within the Vocational Intervention Program (VIP 2.0)" International Journal of Environmental Research and Public Health 19, no. 15: 9548. https://doi.org/10.3390/ijerph19159548
APA StyleMcRae, P., Kobel, C., Lukersmith, S., & Simpson, G. (2022). What Does It Take to Get Somebody Back to Work after Severe Acquired Brain Injury? Service Actions within the Vocational Intervention Program (VIP 2.0). International Journal of Environmental Research and Public Health, 19(15), 9548. https://doi.org/10.3390/ijerph19159548






