The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19
Abstract
:1. Introduction
1.1. Physiotherapy in Patients with Long COVID-19
1.2. Digital Physiotherapy Practice
1.3. Objectives
- -
- To explore the effectiveness and the magnitude of the effect of a digital physiotherapy intervention on functional recovery in patients diagnosed with Long COVID-19.Secondary objective:
- -
- To assess the level of therapeutic adherence to the digital physiotherapy intervention.
2. Methods
2.1. Study Design
2.2. Patients
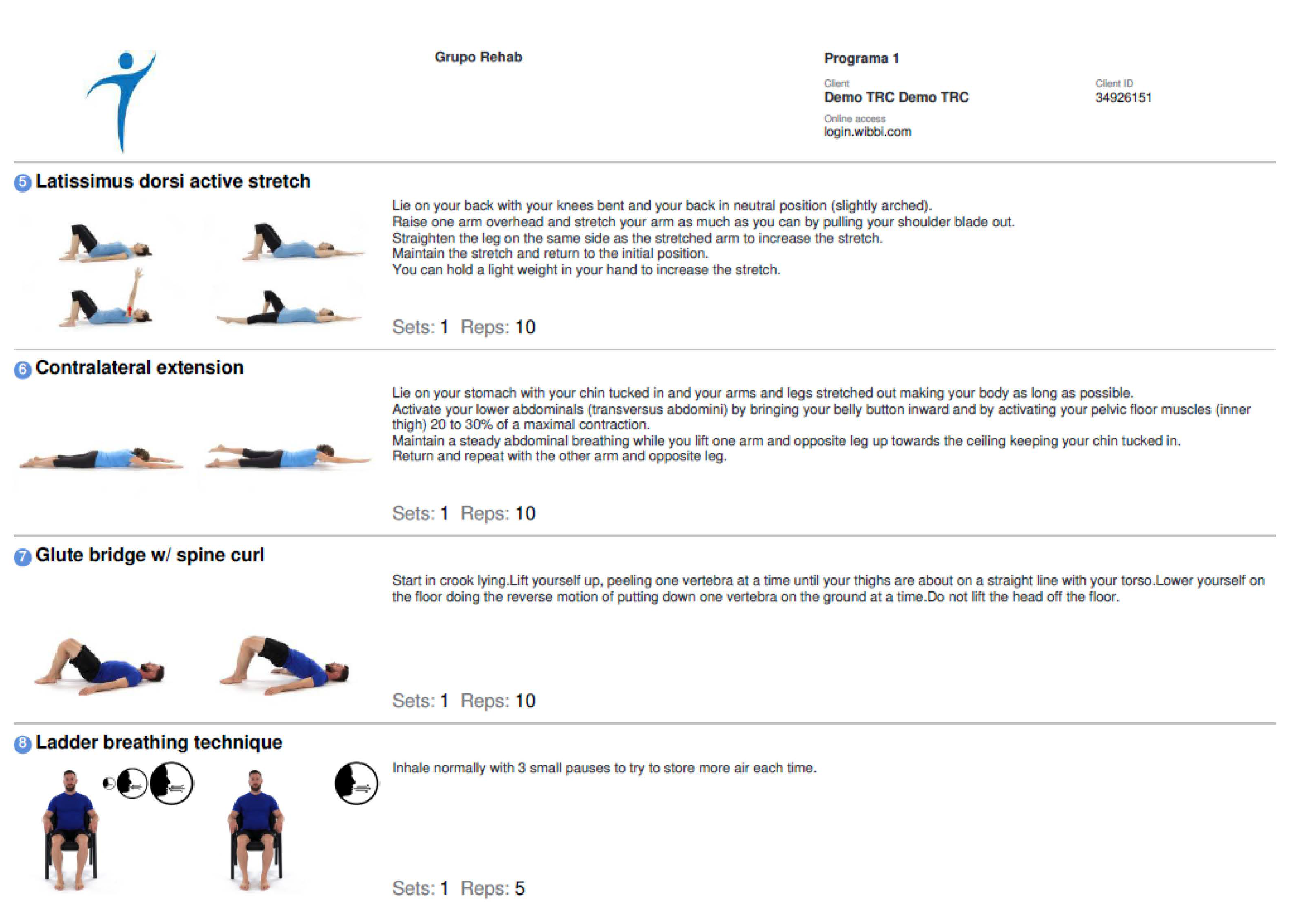
2.3. Intervention
2.4. Outcome Measures
2.4.1. Main Explanatory Variable
Functional Capacity
2.4.2. Secondary Explanatory Variable
Adherence
2.5. Data Collection Procedure and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus |
| COVID-19 | Coronavirus Disease2019 |
| SEMG | Spanish society of family and general practitioners |
| WCPT | The World Confederation for Physical Therapy |
| INPTRA | The International Network of Physical Therapy Regulatory Authorities |
| IC | confidence index |
| 1-min STS | sit-to-stand test in 1 min |
| 6MWT | 6-min walk test |
| SPPB | short performance physical battery test |
| CONSORT | Consolidated Standards of Reporting Trials |
| MCID | Minimal Clinically Important Difference |
References
- Del Rio, C.; Malani, P.N. Novel Coronavirus—Important Information for Clinicians. JAMA—J. Am. Med. Assoc. 2020, 323, 1039–1040. [Google Scholar] [CrossRef]
- Clinical Management of Severe Acute Respiratory Infection when COVID-19 is Suspected. Available online: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected (accessed on 20 May 2020).
- Agergaard, J.; Leth, S.; Pedersen, T.H.; Harbo, T.; Blicher, J.U.; Karlsson, P.; Østergaard, L.; Andersen, H.; Tankisi, H. Myopathic changes in patients with long-term fatigue after COVID-19. Clin. Neurophysiol. 2021, 132, 1974–1981. [Google Scholar] [CrossRef]
- WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online: https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19) (accessed on 21 May 2020).
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Hama Amin, B.J.; Kakamad, F.H.; Ahmed, G.S.; Ahmed, S.F.; Abdulla, B.A.; Mohammed, S.H.; Mikael, T.M.; Salih, R.Q.; Ali, R.K.; Salh, A.M.; et al. Post COVID-19 pulmonary fibrosis; a meta-analysis study. Ann. Med. Surg. 2022, 77, 103590. [Google Scholar] [CrossRef] [PubMed]
- van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.J.; Chau, B.; Lui, M.; Lam, G.-T.; Lin, N.; Humbert, S. Physical Medicine and Rehabilitation and Pulmonary Rehabilitation for COVID-19. Am. J. Phys. Med. Rehabil. 2020, 99, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus » National Guidance for Post-COVID Syndrome Assessment Clinics. Available online: https://www.england.nhs.uk/coronavirus/publication/national-guidance-for-post-covid-syndrome-assessment-clinics (accessed on 1 December 2021).
- La Fisioterapia, Clave en la Recuperación de la Función Pulmonar Afectada por el Coronavirus. Available online: https://www.consejo-fisioterapia.org/noticias/3288_La_Fisioterapia_clave_en_la_recuperacion_de_la_funcion_pulmonar_afectada_por_el_Coronavirus.html (accessed on 1 December 2021).
- Bangash, M.N.; Patel, J.; Parekh, D. COVID-19 and the liver: Little cause for concern. Lancet Gastroenterol. Hepatol. 2020, 5, 529–530. [Google Scholar] [CrossRef] [Green Version]
- Lista-Paz Dra, A.; González-Doniz Dra, L.; Souto-Camba Dra, S. ¿Qué papel desempeña la Fisioterapia en la pandemia mundial por COVID-19? Fisioterapia 2020, 42, 167. [Google Scholar] [CrossRef]
- MILAGROS PÉREZ OLIVA (Redacción El País) Los Hospitales Crean Unidades Para Atender Secuelas de la Enfermedad|Sociedad|EL PAÍS. Available online: https://elpais.com/sociedad/2020-05-26/los-hospitales-crean-unidades-para-atender-secuelas-de-la-enfermedad.html (accessed on 27 May 2020).
- Pastora-Bernal, J.-M.; Estebanez-Pérez, M.-J.; Molina-Torres, G.; García-López, F.-J.; Sobrino-Sánchez, R.; Martín-Valero, R. Telerehabilitation Intervention in Patients with COVID-19 after Hospital Discharge to Improve Functional Capacity and Quality of Life. Study Protocol for a Multicenter Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2021, 18, 2924. [Google Scholar] [CrossRef] [PubMed]
- Chinese Association of Rehabilitation Medicine; Respiratory rehabilitation committee of Chinese Association of Rehabilitation Medicine; Cardiopulmonary rehabilitation Group of Chinese Society of Physicai Medicine and Rehabilitation. [Recommendations for respiratory rehabilitation of COVID-19 in adult]. Zhonghua Jie He He Hu Xi Za Zhi 2020, 43, E029. [Google Scholar] [CrossRef]
- Almekhlafi, G.A.; Albarrak, M.M.; Mandourah, Y.; Hassan, S.; Alwan, A.; Abudayah, A.; Altayyar, S.; Mustafa, M.; Aldaghestani, T.; Alghamedi, A.; et al. Presentation and outcome of Middle East respiratory syndrome in Saudi intensive care unit patients. Crit. Care 2016, 20, 1–9. Available online: https://ccforum.biomedcentral.com/articles/10.1186/s13054-016-1303-8 (accessed on 21 May 2020). [CrossRef] [PubMed] [Green Version]
- Lau, H.M.C.; Ng, G.Y.F.; Jones, A.Y.M.; Lee, E.W.C.; Siu, E.H.K.; Hui, D.S.C. A randomised controlled trial of the effectiveness of an exercise training program in patients recovering from severe acute respiratory syndrome. Aust. J. Physiother. 2005, 51, 213–219. [Google Scholar] [CrossRef] [Green Version]
- Rinaldo, R.F.; Mondoni, M.; Parazzini, E.M.; Pitari, F.; Brambilla, E.; Luraschi, S.; Balbi, M.; Sferrazza Papa, G.F.; Sotgiu, G.; Guazzi, M.; et al. Deconditioning as main mechanism of impaired exercise response in COVID-19 survivors. Eur. Respir. J. 2021, 58, 2100870. [Google Scholar] [CrossRef] [PubMed]
- Skjørten, I.; Ankerstjerne, O.A.W.; Trebinjac, D.; Brønstad, E.; Rasch-Halvorsen, Ø.; Einvik, G.; Lerum, T.V.; Stavem, K.; Edvardsen, A.; Ingul, C.B. Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. Eur. Respir. J. 2021, 58, 2100996. [Google Scholar] [CrossRef] [PubMed]
- Peçanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am. J. Physiol. Circ. Physiol. 2020, 318, H1441–H1446. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.M.; Locke, E.R.; Woo, D.M.; Nguyen, E.H.K.; Press, V.G.; Layouni, T.A.; Trittschuh, E.H.; Reiber, G.E.; Fan, V.S. Inhaler Training Delivered by Internet-Based Home Videoconferencing Improves Technique and Quality of Life. Respir. Care 2017, 62, 1412–1422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ACPRC. COVID-19 Information—ACPRC. Available online: https://www.acprc.org.uk/resources/covid-19-information/physiotherapy-guidance-for-clinicians-and-managers/ (accessed on 22 May 2020).
- Cortijo, C.M.; Bejarano, F.J.Z.; Delgado, E.G.; Cortés, M.S.; Rubio, V.T.; Fisioterapeutas Hospital Universitario 12 de Octubre (Madrid). Guía De Fisioterapia En El Paciente Con Sospecha De COVID-19 O COVID-19 Confirmado. Available online: https://imas12.es/wp-content/uploads/2020/Repositorio/01.Guia_Fisioterapia_paciente_sospecha_COVID19_o_COVID_19_confirmado.pdf (accessed on 21 May 2020).
- Rehabilitation Considerations during the COVID-19 Outbreak. Available online: https://iris.paho.org/handle/10665.2/52035 (accessed on 22 June 2022).
- Living Guidance for Clinical Management of COVID-19. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 (accessed on 6 June 2022).
- Guía Clínica para la Atención al Paciente LONG COVID/COVID Persistente. Available online: https://www.semg.es/index.php/consensos-guias-y-protocolos/363-guia-clinica-para-la-atencion-al-paciente-long-covid-covid-persistente (accessed on 6 June 2022).
- Russell, T.G. Physical rehabilitation using telemedicine. J. Telemed. Telecare 2007, 13, 217–220. Available online: http://cyber.usask.ca/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2009653682&site=ehost-live (accessed on 16 March 2016). [CrossRef]
- Rosen, K.; Patel, M.; Lawrence, C.; Mooney, B. Delivering Telerehabilitation to COVID-19 Inpatients:A Retrospective Chart Review Suggests It Is a Viable Option. HSS J. 2020, 16, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Seelman, K.D.; Hartman, L.M. Telerehabilitation: Policy Issues and Research Tools. Int. J. Telerehabil. 2009, 1, 47–58. [Google Scholar] [CrossRef] [Green Version]
- Pastora-Bernal, J.M.; Martín-Valero, R.; Barón-López, F.J.; Estebanez-Pérez, M.J. Evidence of Benefit of Telerehabitation after Orthopedic Surgery: A Systematic Review. J. Med. Internet Res. 2017, 19, e142. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, R.S.; O’Hoski, S. Telemedicine in COPD. Chest 2014, 145, 945–949. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Shin, W.S.; Bang, D.H. Application of digital practice to improve head movement, visual perception and activities of daily living for subacute stroke patients with unilateral spatial neglect: Preliminary results of a single-blinded, randomized controlled trial. Medicine 2021, 100, e24637. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://world.physio/sites/default/files/2020-06/WCPT-INPTRA-Digital-Physical-Therapy-Practice-Task-force-March2020.pdf (accessed on 1 December 2021).
- Fekete, M.; Fazekas-Pongor, V.; Balazs, P.; Tarantini, S.; Nemeth, A.N.; Varga, J.T. Role of new digital technologies and telemedicine in pulmonary rehabilitation. Wien. Klin. Wochenschr. 2021, 133, 1201–1207. [Google Scholar] [CrossRef]
- McAlearney, A.S.; Sieck, C.J.; Gregory, M.E.; Di Tosto, G.; MacEwan, S.R.; DePuccio, M.J.; Lee, J.A.; Huerta, T.R.; Walker, D.M. Examining Patients’ Capacity to Use Patient Portals. Med. Care 2021, 59, 1067–1074. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Russell, T.G. Telehealth for musculoskeletal physiotherapy. Musculoskelet. Sci. Pract. 2020, 48, 102193. [Google Scholar] [CrossRef] [PubMed]
- Rhon, D.I.; Fritz, J.M.; Kerns, R.D.; McGeary, D.D.; Coleman, B.C.; Farrokhi, S.; Burgess, D.J.; Goertz, C.M.; Taylor, S.L.; Hoffmann, T. TIDieR-telehealth: Precision in reporting of telehealth interventions used in clinical trials—unique considerations for the Template for the Intervention Description and Replication (TIDieR) checklist. BMC Med. Res. Methodol. 2022, 22, 1–11. Available online: https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01640-7 (accessed on 21 July 2022). [CrossRef] [PubMed]
- Stoffels, A.A.; De Brandt, J.; Meys, R.; van Hees, H.W.; Vaes, A.W.; Klijn, P.; Burtin, C.; Franssen, F.M.; van den Borst, B.; Sillen, M.J.; et al. Short Physical Performance Battery: Response to Pulmonary Rehabilitation and Minimal Important Difference Estimates in Patients With Chronic Obstructive Pulmonary Disease. Arch. Phys. Med. Rehabil. 2021, 102, 2377–2384.e5. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, T.; de Bisschop, C.; Beaumont, M.; Ouksel, H.; Jean, V.; Dessables, F.; Chambellan, A. Is the 1-minute sit-to-stand test a good tool for the evaluation of the impact of pulmonary rehabilitation? Determination of the minimal important difference in COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 11, 2609–2616. Available online: https://pubmed.ncbi.nlm.nih.gov/27799759/ (accessed on 7 June 2022). [CrossRef] [PubMed] [Green Version]
- Eichler, S.; Rabe, S.; Salzwedel, A.; Müller, S.; Stoll, J.; Tilgner, N.; John, M.; Wegscheider, K.; Mayer, F.; Völler, H. Effectiveness of an interactive telerehabilitation system with home-based exercise training in patients after total hip or knee replacement: Study protocol for a multicenter, superiority, no-blinded randomized controlled trial. Trials 2017, 18, 1–7. Available online: https://pubmed.ncbi.nlm.nih.gov/28934966/ (accessed on 29 June 2022).
- Arbillaga, A.; Pardàs, M.; Escudero, R.; Rodríguez, R.; Alcaraz, V.; Llanes, S.; Herrero, B.; Gimeno, E.; Ríos, A. Fisioterapia Respiratoria en el Manejo del Paciente con COVID-19: Recomendaciones Generales Área de Fisioterapia Respiratoria Sociedad Española de Neumología y Cirugía Torácica-Separ-Versión 1.0-26 de Marzo 2020. Available online: https://svmefr.com/wp-content/uploads/2020/03/COVID19-SEPAR-26_03_20.pdf (accessed on 1 December 2021).
- Kaminsky, L.A.; Tuttle, M.S. Functional assessment of heart failure patients. Heart Fail. Clin. 2015, 11, 29–36. [Google Scholar] [CrossRef] [Green Version]
- Crook, S.; Büsching, G.; Schultz, K.; Lehbert, N.; Jelusic, D.; Keusch, S.; Wittmann, M.; Schuler, M.; Radtke, T.; Frey, M.; et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. Eur. Respir. J. 2017, 49, 2–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, M.C.; Lima, L.N.G.; Moreira, M.M.; Mendes, F.A.R. One minute sit-to-stand test as an alternative to measure functional capacity in patients with pulmonary arterial hypertension. J. Bras. Pneumol. 2022, 48, e20210483. [Google Scholar] [PubMed]
- Zampogna, E.; Paneroni, M.; Belli, S.; Aliani, M.; Gandolfo, A.; Visca, D.; Bellanti, M.T.; Ambrosino, N.; Vitacca, M. Pulmonary Rehabilitation in Patients Recovering from COVID-19. Respiration 2021, 100, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, Á.; Álvarez, G.; Russo, F.; San-José, B.; Sánchez-Tomero, J.A.; Barril, G. ¿Es útil el SPPB como método de screening de capacidad funcional en pacientes con enfermedad renal crónica avanzada? Nefrología 2019, 39, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Mugueta-Aguinaga, I.; Garcia-Zapirain, B. FRED: Exergame to prevent dependence and functional deterioration associated with ageing. A pilot three-week randomized controlled clinical trial. Int. J. Environ. Res. Public Health 2017, 14, 1439. Available online: https://www.researchgate.net/publication/350022792_Telerehabilitation_Intervention_in_Patients_with_COVID-19_after_Hospital_Discharge_to_Improve_Functional_Capacity_and_Quality_of_Life_Study_Protocol_for_a_Multicenter_Randomized_Clinical_Trial (accessed on 1 December 2021).
- Vrijens, B.; De Geest, S.; Hughes, D.A.; Przemyslaw, K.; Demonceau, J.; Ruppar, T.; Dobbels, F.; Fargher, E.; Morrison, V.; Lewek, P.; et al. A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 2012, 73, 691–705. Available online: https://pubmed.ncbi.nlm.nih.gov/22486599/ (accessed on 6 June 2022). [CrossRef]
- Kernebeck, S.; Busse, T.S.; Ehlers, J.P.; Vollmar, H.C. Adherence to digital health interventions: Definitions, methods, and open questions. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021, 64, 1278–1284. Available online: https://pubmed.ncbi.nlm.nih.gov/34559252/ (accessed on 6 June 2022). [CrossRef] [PubMed]
- Por Qué Reportar el Tamaño del Efecto?—Comunicar. Escuela de Autores. Available online: https://www.revistacomunicar.com/wp/escuela-de-autores/por-que-reportar-el-tamano-del-efecto/ (accessed on 18 July 2022).
- Cohen, J. Statistical Power Analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Salas Apaza, J.A.; Franco, J.V.A.; Meza, N.; Madrid, E.; Loézar, C.; Garegnani, L. Diferencia mínima clínicamente importante: Conceptos básicos. Medwave 2021, 21, e8149. [Google Scholar] [CrossRef] [PubMed]
- Ayoubkhani, D.; Bermingham, C.; Pouwels, K.B.; Glickman, M.; Nafilyan, V.; Zaccardi, F.; Khunti, K.; Alwan, N.A.; Walker, A.S. Trajectory of long COVID symptoms after COVID-19 vaccination: Community based cohort study. Br. Med. J. 2022, 377, e069676. [Google Scholar] [CrossRef]
- Haute Autorité de Santé—Symptômes Prolongés Suite à une COVID-19 de l’adulte—Diagnostic et Prise en Charge. Available online: https://www.has-sante.fr/jcms/p_3237041/fr/symptomes-prolonges-suite-a-une-covid-19-de-l-adulte-diagnostic-et-prise-en-charge (accessed on 22 June 2022).
- Sisó-Almirall, A.; Brito-Zerón, P.; Ferrín, L.C.; Kostov, B.; Moreno, A.M.; Mestres, J.; Sellarès, J.; Galindo, G.; Morera, R.; Basora, J.; et al. Long COVID-19: Proposed Primary Care Clinical Guidelines for Diagnosis and Disease Management. Int. J. Environ. Res. Public Health 2021, 18, 4350. [Google Scholar] [CrossRef] [PubMed]
- Sivan, M.; Taylor, S. NICE guideline on long COVID. Br. Med. J. 2020, 371, 1–2. Available online: https://www.bmj.com/content/371/bmj.m4938 (accessed on 9 June 2022). [CrossRef] [PubMed]
- Burke, M.J.; del Rio, C. Long COVID has exposed medicine’s blind-spot. Lancet Infect. Dis. 2021, 21, 1062–1064. [Google Scholar] [CrossRef]
- de Oliveira, J.M.; Spositon, T.; Cerci Neto, A.; Soares, F.M.C.; Pitta, F.; Furlanetto, K.C. Functional tests for adults with asthma: Validity, reliability, minimal detectable change, and feasibility. J. Asthma 2022, 59, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Olmos, F.J.; Gómez-Conesa, A.A.; García-Testal, A.; Ortega-Pérez-de-Villar, L.; Valtueña-Gimeno, N.; Gil-Gómez, J.A.; Garcia-Maset, R.; Segura-Ortí, E. An intradialytic non-immersive virtual reality exercise program: A crossover randomized controlled trial. Nephrol. Dial. Transplant 2022, 59, 169–177. [Google Scholar] [CrossRef]
- Halabchi, F.; Alizadeh, Z.; Sahraian, M.A.; Abolhasani, M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. 2017, 17, 185. [Google Scholar] [CrossRef]
- Samuel, S.R.; Maiya, A.G.; Fernandes, D.J.; Guddattu, V.; Saxena, P.P.; Kurian, J.R.; Lin, P.J.; Mustian, K.M. Effectiveness of exercise-based rehabilitation on functional capacity and quality of life in head and neck cancer patients receiving chemo-radiotherapy. Support. Care Cancer 2019, 27, 3913–3920. [Google Scholar] [CrossRef]
- Tang, Y.; Jiang, J.; Shen, P.; Li, M.; You, H.; Liu, C.; Chen, L.; Wang, Z.; Zhou, C.; Feng, Z. Liuzijue is a promising exercise option for rehabilitating discharged COVID-19 patients. Medicine 2021, 100, e24564. [Google Scholar] [CrossRef]
- Khan, F.; Amatya, B.; Kesselring, J.; Galea, M.P.G. Telerehabilitation for persons with multiple sclerosis. A Cochrane review. Eur. J. Phys. Rehabil. Med. 2015, 51, 311–325. [Google Scholar] [CrossRef]
- Tsai, L.L.Y.; McNamara, R.J.; Moddel, C.; Alison, J.A.; McKenzie, D.K.; McKeough, Z.J. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: The randomized controlled TeleR Study. Respirology 2017, 22, 699–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez-Blanco, C.; Gonzalez-Gerez, J.J.; Bernal-Utrera, C.; Anarte-Lazo, E.; Perez-Ale, M.; Saavedra-Hernandez, M. Short-Term Effects of a Conditioning Telerehabilitation Program in Confined Patients Affected by COVID-19 in the Acute Phase. A Pilot Randomized Controlled Trial. Medicine 2021, 57, 684. [Google Scholar] [CrossRef] [PubMed]
- Levy, C.E.; Silverman, E.; Jia, H.; Geiss, M.; Omura, D. Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomes. J. Rehabil. Res. Dev. 2015, 52, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Russell, T.G.; Buttrum, P.; Wootton, R.; Jull, G.A. Internet-Based Outpatient Telerehabilitation for Patients Following Total Knee Arthroplasty. J. Bone Jt. Surgery, Am. Vol. 2011, 93, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Hamel, M.; Fontaine, R.; Boissy, P. In-home telerehabilitation for geriatric patients. IEEE Eng. Med. Biol. Mag. 2008, 27, 29–37. [Google Scholar] [CrossRef]
- Finkelstein, J.; Wood, J.; Cha, E. Impact of physical telerehabilitation on functional outcomes in seniors with mobility limitations. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; Volume 2012, pp. 5827–5832. [Google Scholar]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; Lannin, N.A.; George, S.; Sherrington, C. Telerehabilitation services for stroke. Cochrane Database Syst. Rev. 2020, 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Taito, S.; Yamauchi, K.; Kataoka, Y. Telerehabilitation in Subjects with Respiratory Disease: A Scoping Review. Respir. Care 2021, 66, 686–698. [Google Scholar] [CrossRef] [PubMed]
- Curci, C.; Pisano, F.; Bonacci, E.; Camozzi, D.M.; Ceravolo, C.; Bergonzi, R.; De Franceschi, S.; Moro, P.; Guarnieri, R.; Ferrillo, M.; et al. Early rehabilitation in post-acute COVID-19 patients: Data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur. J. Phys. Rehabil. Med. 2020, 56, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Gerez, J.J.; Saavedra-Hernandez, M.; Anarte-Lazo, E.; Bernal-Utrera, C.; Perez-Ale, M.; Rodriguez-Blanco, C. Short-Term Effects of a Respiratory Telerehabilitation Program in Confined COVID-19 Patients in the Acute Phase: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 7511. [Google Scholar] [CrossRef]
- Ladds, E.; Rushforth, A.; Wieringa, S.; Taylor, S.; Rayner, C.; Husain, L.; Greenhalgh, T. Persistent symptoms after COVID-19: Qualitative study of 114 “long COVID” patients and draft quality principles for services. BMC Health Serv. Res. 2020, 20, 1144. [Google Scholar] [CrossRef] [PubMed]



| Participants (n = 32) | |
|---|---|
| Age (Mean/SD) | 45.93 ± 10.65 |
| Gender Woman % (n) | 71.9% (23) |
| Non-Hospitalised % (n) | 90.6% (29) |
| ICU % (n) | 6.3% (2) |
| Comorbidities Long COVID-19 | n = 32 | % |
|---|---|---|
| Orthopaedic Pathology (Spine Surgery, Herniated Disc, Scoliosis, Hyper lordosis, Sacral Lumbarisation, Sacroiliitis, Shoulder Tendinopathy, Osteochondritis, Osteomalacia, Osteoarthritis and Osteoarthritis) | 15 | 46.88% |
| Respiratory Pathology (Asthma, Bronchial Hyperresponsiveness and Chronic Pharyngitis) | 11 | 34.38% |
| Endocrine Pathology (Thyroid Pathology and Diabetes) | 4 | 12.50% |
| Circulatory Pathology (Heart disease, Varicose veins and Hypertension) | 3 | 9.38% |
| Inflammatory Pathology (Sarcoidosis and Pancreatitis) | 2 | 6.25% |
| Depression | 2 | 6.25% |
| Immunological disorders (seasonal allergies) | 2 | 6.25% |
| Viral Deseases (Herpes Zoster and Mononucleosis) | 2 | 6.25% |
| Headaches | 2 | 6.25% |
| Myasthenia | 1 | 3.13% |
| Colic | 1 | 3.13% |
| Ureter Reflux | 1 | 3.13% |
| Initial (M/SD) | Final (M/SD) | Correlation | Sig. | Cohen’s d | Effect Size r | Effect Size | |
|---|---|---|---|---|---|---|---|
| 1-min STS | 14.03/7.84 | 17.53/7.44 | 0.81 | 0.00 | 0.45 | 0.22 | Small |
| SPPB | 7.90/1.98 | 9.12/1.69 | 0.72 | 0.00 | 0.66 | 0.31 | Medium |
| Balance test (SPPB) | 3.65/0.60 | 3.96/0.17 | 0.50 | 0.00 | 0.70 | 0.33 | Medium |
| Gait Speed test (SPPB) | 2.87/1.09 | 3.34/0.90 | 0.72 | 0.00 | 0.46 | 0.22 | Small |
| Chair Stand test (SPPB) | 1.37/0.90 | 1.81/1.09 | 0.66 | 0.00 | 0.43 | 0.21 | Small |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Estebanez-Pérez, M.-J.; Pastora-Bernal, J.-M.; Martín-Valero, R. The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 9566. https://doi.org/10.3390/ijerph19159566
Estebanez-Pérez M-J, Pastora-Bernal J-M, Martín-Valero R. The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19. International Journal of Environmental Research and Public Health. 2022; 19(15):9566. https://doi.org/10.3390/ijerph19159566
Chicago/Turabian StyleEstebanez-Pérez, María-José, José-Manuel Pastora-Bernal, and Rocío Martín-Valero. 2022. "The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19" International Journal of Environmental Research and Public Health 19, no. 15: 9566. https://doi.org/10.3390/ijerph19159566
APA StyleEstebanez-Pérez, M.-J., Pastora-Bernal, J.-M., & Martín-Valero, R. (2022). The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19. International Journal of Environmental Research and Public Health, 19(15), 9566. https://doi.org/10.3390/ijerph19159566







