STIs during the COVID-19 Pandemic in Hungary: Gonorrhea as a Potential Indicator of Sexual Behavior
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Retrieval
2.2. Laboratory Tests
2.3. Statistical Analysis
3. Results
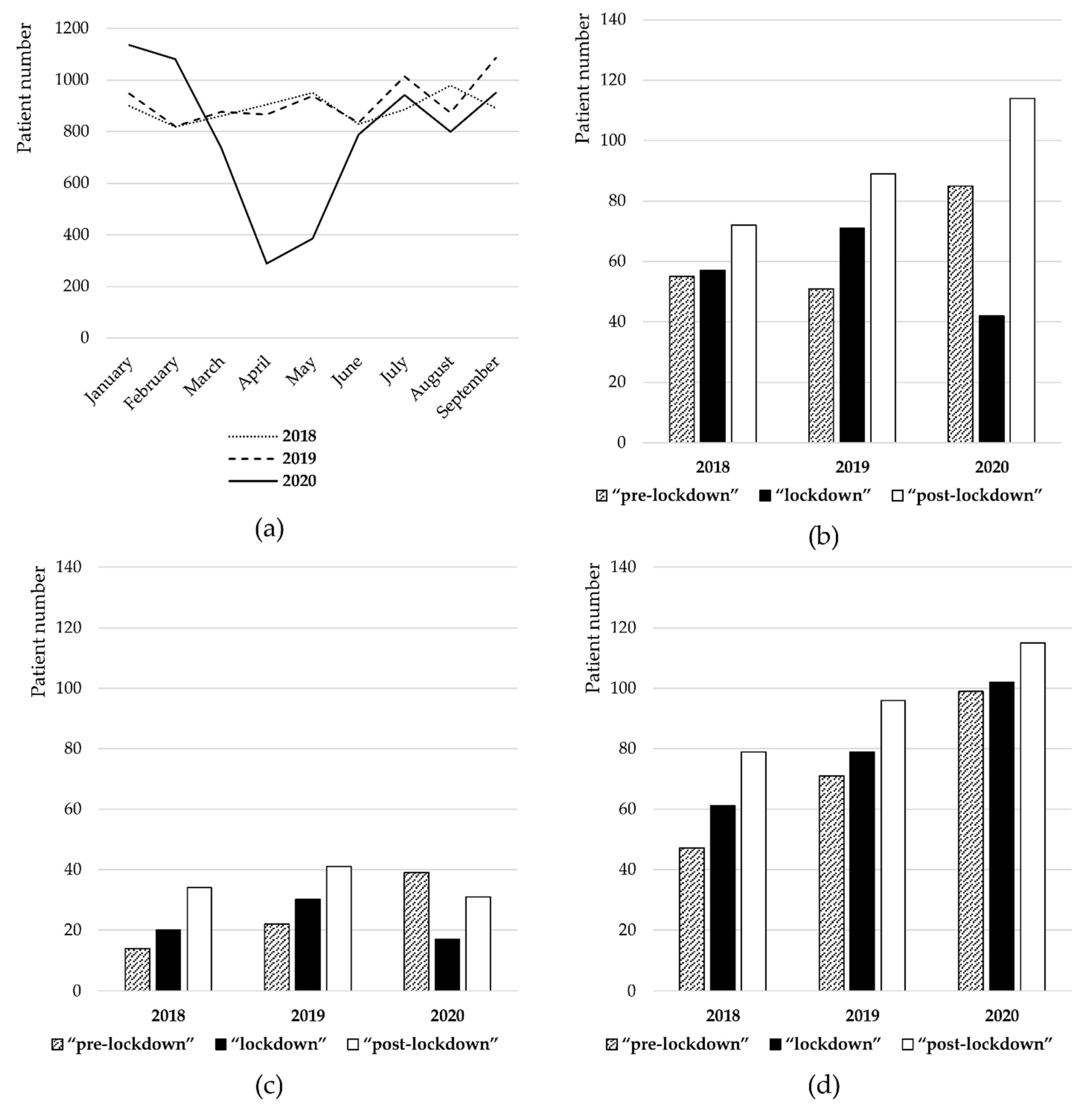
3.1. Patient Influx
3.2. Number of Patients Diagnosed by STI Screening
3.3. Syphilis Stages
3.4. Chlamydia Serotypes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| 2018 | 2019 | 2020 | |
|---|---|---|---|
| SYPHILIS | |||
| “pre-lockdown” | 55 | 51 | 85 |
| “lockdown” | 57 | 71 | 42 |
| “post-lockdown” | 72 | 89 | 114 |
| CHLAMYDIA | |||
| “pre-lockdown” | 14 | 22 | 39 |
| “lockdown” | 20 | 30 | 17 |
| “post-lockdown” | 34 | 41 | 31 |
| GONORRHEA | |||
| “pre-lockdown” | 47 | 71 | 99 |
| “lockdown” | 61 | 79 | 102 |
| “post-lockdown” | 79 | 96 | 115 |
| 2018 | 2019 | 2020 | p Value # | ||||
|---|---|---|---|---|---|---|---|
| Patients Diagnosed by Screening | Patients with Acute Symptoms | Patients Diagnosedby Screening | Patients with Acute Symptoms | Patients Diagnosed by Screening | Patients with Acute Symptoms | ||
| SYPHILIS | |||||||
| “pre-lockdown” | 32 (58.2%) | 23 (41.8%) | 30 (58.8%) | 21 (41.2%) | 52 (61.2%) | 33 (38.8%) | 0.0099 * |
| “lockdown” | 23 (40.4%) | 34 (59.6%) | 42 (59.2%) | 29 (40.8%) | 16 (38.1%) | 26 (61.9%) | |
| “post-lockdown” | 33 (45.8%) | 39 (54.2%) | 56 (62.9%) | 33 (37.1%) | 66 (57.9%) | 48 (42.1%) | 0.022 * |
| CHLAMYDIA | |||||||
| “pre-lockdown” | 3 (21.4%) | 11 (78.6%) | 1 (4.5%) | 21 (95.5%) | 24 (61.5%) | 15 (38.5%) | 0.0006 * |
| “lockdown” | 4 (20.0%) | 16 (80.0%) | 6 (20.0%) | 24 (80.0%) | 2 (11.8%) | 15 (88.2%) | |
| “post-lockdown” | 6 (17.6%) | 28 (82.4%) | 11 (26.8%) | 30 (73.2%) | 15 (48.4%) | 16 (51.6%) | 0.011 * |
| GONORRHEA | |||||||
| “pre-lockdown” | 2 (4.2%) | 45 (95.7%) | 6 (8.5%) | 65 (91.5%) | 28 (28.3%) | 71 (71.7%) | 0.712 |
| “lockdown” | 7 (11.5%) | 54 (88.5%) | 10 (12.7%) | 69 (87.3%) | 25 (24.5%) | 77 (75.5%) | |
| “post-lockdown” | 8 (10.1%) | 71 (89.9% | 17 (17.7%) | 79 (82.3%) | 35 (30.4%) | 80 (69.8%) | 0.30 |
| 2018 | 2019 | 2020 | p Value # | ||||
|---|---|---|---|---|---|---|---|
| Latent Stage Syphilis | Early-Stage Syphilis | Latent Stage Syphilis | Early-Stage Syphilis | Latent Stage Syphilis | Early-Stage Syphilis | ||
| “pre-lockdown” | 32 (58.2%) | 23 (41.8%) | 36 (70.6%) | 15 (29.4%) | 66 (77.6%) | 19 (22.4%) | 0.017 * |
| “lockdown” | 32 (56.1%) | 25 (43.9%) | 48 (67.6%) | 23 (32.4%) | 24 (57.1%) | 18 (42.9%) | |
| “post-lockdown” | 37 (51.4%) | 35 (48.6%) | 67 (75.3%) | 22 (24.7%) | 95 (83.3%) | 19 (16.7%) | 0.019 * |
| 2018 | 2019 | 2020 | p Value | ||||
|---|---|---|---|---|---|---|---|
| Chlamydia Trachomatis (D-K) | Chlamydia Trachomatis (L1-L3) | Chlamydia Trachomatis (D-K) | Chlamydia Trachomatis(L1-L3) | Chlamydia Trachomatis (D-K) | Chlamydia Trachomatis(L1-L3) | 2020 Compared to 2018 | 2020 Compared to 2019 |
| 53 (79.9%) | 15 (22.1%) | 68 (73.1%) | 25 (26.9%) | 77 (88.5%) | 10 (11.5%) | 0.0455 * | 0.074 * |
References
- Merkely, B.; Szabó, A.J.; Kosztin, A.; Berényi, E.; Sebestyén, A.; Lengyel, C.; Merkely, G.; Karády, J.; Várkonyi, I.; Papp, C.; et al. Novel coronavirus epidemic in the Hungarian population, a cross-sectional nationwide survey to support the exit policy in Hungary. Geroscience 2020, 42, 1063–1074. [Google Scholar] [CrossRef] [PubMed]
- Apalla, Z.; Lallas, A.; Mastraftsi, S.; Giannoukos, A.; Noukari, D.; Goula, M.; Kalantzi, P.; Zapridou, M.; Lallas, K.; Kyrgidis, A.; et al. Impact of COVID-19 pandemic on STIs in Greece. Sex. Transm. Infect. 2022, 98, 70. [Google Scholar] [CrossRef] [PubMed]
- Crane, M.A.; Popovic, A.; Stolbach, A.I.; Ghanem, K.G. Reporting of sexually transmitted infections during the COVID-19 pandemic. Sex. Transm. Infect. 2021, 97, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Whitlock, G.G.; McOwan, A.; Nugent, D. Gonorrhoea during COVID-19 in London, UK. Sex. Transm. Infect. 2021, 97, 622–623. [Google Scholar] [CrossRef] [PubMed]
- Petrovay, F.; Balla, E.; Erdősi, T. Emergence of the lymphogranuloma venereum L2c genovariant, Hungary 2012 to 2016. EuroSurveillance 2017, 22, 30455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mercer, C.H.; Clifton, S.; Riddell, J.; Tanton, C.; Freeman, L.; Copas, A.J.; Dema, E.; Pérez, R.B.; Gibbs, J.; Macdowall, W.; et al. Impacts of COVID-19 on sexual behaviour in Britain: Findings from a large, quasi-representative survey (Natsal-COVID). Sex. Transm. Infect. 2021. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lőrincz, K.; Meznerics, F.A.; Jobbágy, A.; Kiss, N.; Madarász, M.; Belvon, L.; Tóth, B.; Tamási, B.; Wikonkál, N.M.; Marschalkó, M.; et al. STIs during the COVID-19 Pandemic in Hungary: Gonorrhea as a Potential Indicator of Sexual Behavior. Int. J. Environ. Res. Public Health 2022, 19, 9627. https://doi.org/10.3390/ijerph19159627
Lőrincz K, Meznerics FA, Jobbágy A, Kiss N, Madarász M, Belvon L, Tóth B, Tamási B, Wikonkál NM, Marschalkó M, et al. STIs during the COVID-19 Pandemic in Hungary: Gonorrhea as a Potential Indicator of Sexual Behavior. International Journal of Environmental Research and Public Health. 2022; 19(15):9627. https://doi.org/10.3390/ijerph19159627
Chicago/Turabian StyleLőrincz, Kende, Fanni Adél Meznerics, Antal Jobbágy, Norbert Kiss, Mária Madarász, Laura Belvon, Béla Tóth, Béla Tamási, Norbert Miklós Wikonkál, Márta Marschalkó, and et al. 2022. "STIs during the COVID-19 Pandemic in Hungary: Gonorrhea as a Potential Indicator of Sexual Behavior" International Journal of Environmental Research and Public Health 19, no. 15: 9627. https://doi.org/10.3390/ijerph19159627
APA StyleLőrincz, K., Meznerics, F. A., Jobbágy, A., Kiss, N., Madarász, M., Belvon, L., Tóth, B., Tamási, B., Wikonkál, N. M., Marschalkó, M., & Bánvölgyi, A. (2022). STIs during the COVID-19 Pandemic in Hungary: Gonorrhea as a Potential Indicator of Sexual Behavior. International Journal of Environmental Research and Public Health, 19(15), 9627. https://doi.org/10.3390/ijerph19159627








