The Origin, Application and Mechanism of Therapeutic Climbing: A Narrative Review
Abstract
:1. Introduction
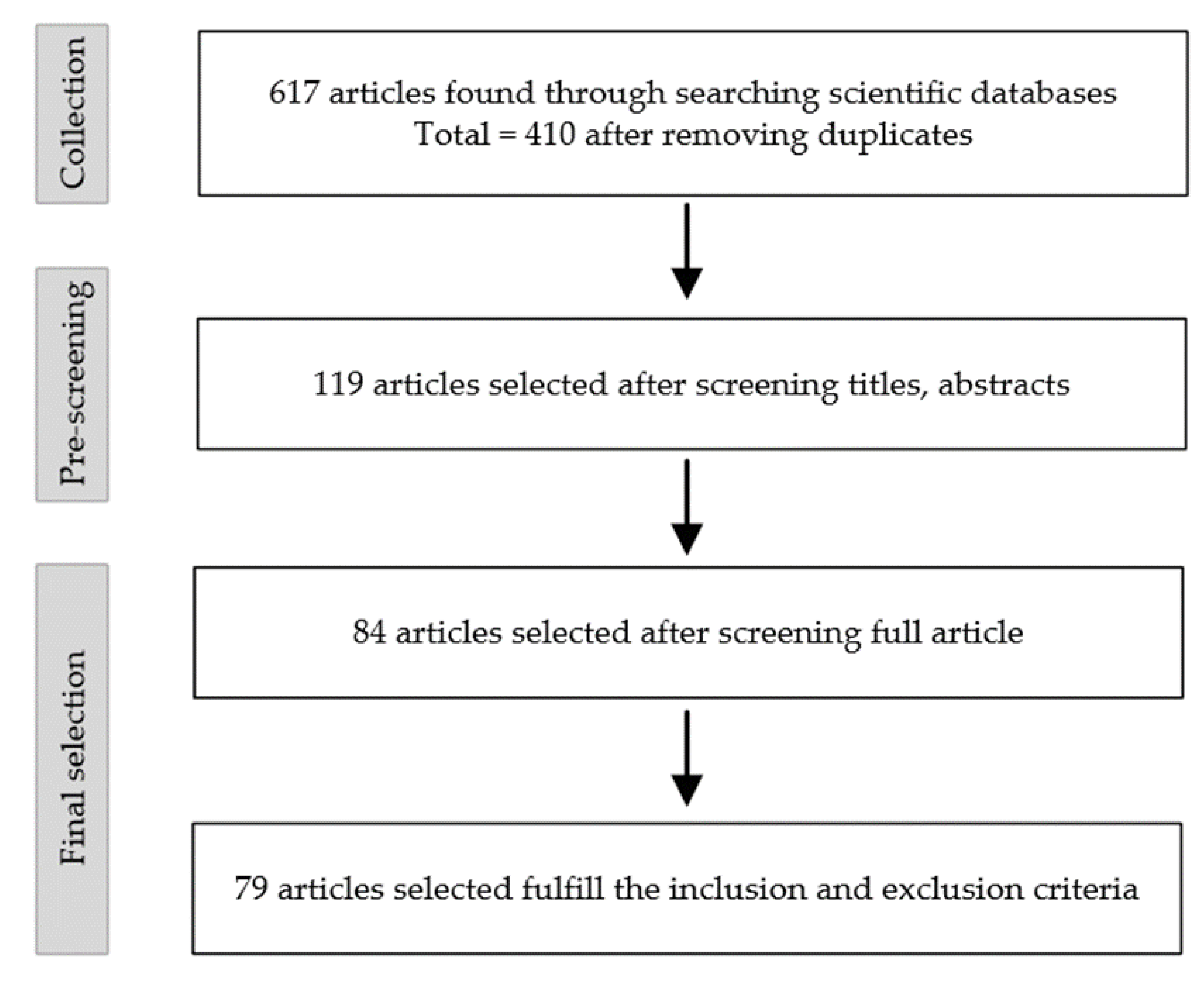
2. Methods
3. The Origin and Development of TC
4. The Effects of TC
4.1. Depression
4.2. Lower Back Pain
4.3. Multiple Sclerosis
4.4. Other Diseases
4.5. Limitations of TC
5. Potential Mechanisms of TC
5.1. Physiological Mechanisms
5.2. Psychological Mechanisms
5.2.1. Social Support Hypothesis
5.2.2. Distraction Hypothesis
5.2.3. Self-Efficacy Hypothesis
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Han, C. Development Dilemma and Promotion Path of the Integration of Sports and Medicine Under Healthy China Strategy. Sports Cult. Guide 2021, 1, 61–66. [Google Scholar]
- Zhao, M.J.; Li, S.Q. Latest advances in mechanisms of non-pharmacological interventions to improve multiple chroniccondi-tions. Chin. Gen. Pract. 2021, 24, 3369–3376. [Google Scholar]
- Maccarone, M.C.; Magro, G.; Solimene, U.; Scanu, A.; Masiero, S. From in vitro research to real life studies: An extensive narrative review of the effects of balneotherapy on human immune response. Sport Sci. Health 2021, 17, 817–835. [Google Scholar] [CrossRef] [PubMed]
- Demers, M.; Thomas, A.; Wittich, W.; McKinley, P. Implementing a novel dance intervention in rehabilitation: Perceived barriers and facilitators. Disabil. Rehabil. 2015, 37, 1066–1072. [Google Scholar] [CrossRef] [PubMed]
- Pereira, A.P.S.; Marinho, V.; Gupta, D.; Magalhaes, F.; Ayres, C.; Teixeira, S. Music Therapy and Dance as Gait Rehabilitation in Patients With Parkinson Disease: A Review of Evidence. J. Geriatr. Psychiatry Neur. 2019, 32, 49–56. [Google Scholar] [CrossRef]
- Masiero, S.; Maccarone, M.C. Health resort therapy interventions in the COVID-19 pandemic era: What next? Int. J. Biometeorol. 2021, 65, 1995–1997. [Google Scholar] [CrossRef]
- Tognolo, L.; Coraci, D.; Fioravanti, A.; Tenti, S.; Scanu, A.; Magro, G.; Maccarone, M.C.; Masiero, S. Clinical Impact of Balneotherapy and Therapeutic Exercise in Rheumatic Diseases: A Lexical Analysis and Scoping Review. Appl. Sci. 2022, 12, 7379. [Google Scholar] [CrossRef]
- Physioclimb. Therapeutic Climbing. Available online: https://physioclimb.de/therapeutisches-klettern/ (accessed on 10 December 2021).
- Fruhauf, A.; Sevecke, K.; Kopp, M. Current state of the scientific literature on effects of therapeutic climbing on mental health—conclusion: A lot to do. Neuropsychiatrie 2019, 33, 1–7. [Google Scholar] [CrossRef]
- Grzybowski, C.; Eils, E. Therapeutic climbing-barely explored but widely used. Sportverletz. Sportsc. 2011, 25, 87–92. [Google Scholar] [CrossRef]
- Wallner, S. Psychological Climbing. Climbing as an instrument of clinical and health psychological treatment. Psychol. Oster 2010, 30, 396–403. [Google Scholar]
- Lukowski, T.; Schmitt, J.; Reinisch, A.; Kern, C. Therapeutic climbing in psychotherapy. Med. Sci. 2013, 9, 1–9. [Google Scholar]
- Kittel, R.M.T.; Granacher, U. Therapeutic climbing on equipment: Possibilities and practical implementation. Physiother. Med. 2013, 3, 11–17. [Google Scholar]
- Schnitzler, E. Letting Go in Order to Move On—Clinical Report: Therapeutic Climbing in Psychosomatic Rehabilitation. Die Rehabil. 2009, 48, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Michailov, M.L. Workload characteristic, performance limiting factors and methods for strength and endurance training in rock climbing. Med. Sport. 2014, 18, 97–106. [Google Scholar]
- Grant, S.; Hynes, V.; Whittaker, A.; Aitchison, T. Anthropometric, strength, endurance and flexibility characteristics of elite and recreational climbers. J. Sports Sci. 1996, 14, 301–309. [Google Scholar] [CrossRef]
- Grant, S.; Hasler, T.; Davies, C.; Aitchison, T.C.; Wilson, J.; Whittaker, A. A comparison of the anthropometric, strength, endurance and flexibility characteristics of female elite and recreational climbers and non-climbers. J. Sports Sci. 2001, 19, 499–505. [Google Scholar] [CrossRef]
- Schöffl, V.R.; Hoffmann, G.; Küpper, T. Acute Injury Risk and Severity in Indoor Climbing—A Prospective Analysis of 515,337 Indoor Climbing Wall Visits in 5 Years. Wilderness Environ. Med. 2013, 24, 187–194. [Google Scholar] [CrossRef] [Green Version]
- Aras, D.; Ewert, A.W. The effects of eight weeks sport rock climbing training on anxiety. Acta Med. Mediterr. 2016, 32, 223–230. [Google Scholar]
- Frühauf, A.; Heußner, J.; Niedermeier, M.; Kopp, M. Expert Views on Therapeutic Climbing—A Multi-Perspective, Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 3535. [Google Scholar] [CrossRef]
- Kowald, A.-C.; Zajetz, A.K. Therapeutic Climbing: Fields of Application in Psychotherapy and Pedagogy; Schattauer Verlag: Stuttgart, Germany, 2014. [Google Scholar]
- Bienia, J. Rock climbing as a factor in therapeutic rehabilitation. Chir. Narz. Ruchu I Ortop. Pol. 1962, 27, 643–651. [Google Scholar]
- Kern, C. Development of a Therapeutic Climbing Program and Evaluation of Its Effects on Individuals with Multiple Sclerosis. Ph.D. Thesis, Munich University of Technology, München, Germany, 2014. [Google Scholar]
- Fryer, S. Physiological and Psychological Contributions to On-Sight Rock Climbing, and the Haemodynamic Responses to Sustained and Intermittent Contractions. Ph.D. Thesis, University of Canterbury, Christchurch, New Zealand, 2013. [Google Scholar]
- Mcclung, S.B. A Rock-Climbing Program as Therapy for the Chronically Mentally Ill; Northern Arizona University: Flagstaff, AZ, USA, 1984. [Google Scholar]
- Lamprecht, T. Climbing with Mentally Handicapped People: A Teaching and Learning Concept with Practical Exercise Examples; Ars Una: Munich, Germany, 1999. [Google Scholar]
- Niggehoff, S. Climbing as an experiential educational medium in the treatment of drug addiction. Prax. Der Psychomot. 2003, 28, 191–195. [Google Scholar]
- Velikonja, O.; Curic, K.; Ozura, A.; Jazbec, S.S. Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clin. Neurol. Neurosurg. 2010, 112, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, G.; Byś, A.; Baszczowski, M.; Ginszt, M.; Suwała, M.; Majcher, P. The influence of sport climbing on depression and anxiety levels-literature review. J. Educ. Health Sport 2018, 8, 336–344. [Google Scholar]
- Dorscht, L.; Karg, N.; Book, S.; Graessel, E.; Kornhuber, J.; Luttenberger, K. A German climbing study on depression: A bouldering psychotherapeutic group intervention in outpatients compared with state-of-the-art cognitive behavioural group therapy and physical activation—Study protocol for a multicentre randomised controlled trial. BMC Psychiatry 2019, 19, 154. [Google Scholar] [CrossRef] [Green Version]
- Book, S.; Luttenberger, K. A new way in the treatment of depressive symptoms. DNP-Der Neurol. Und Psychiater 2015, 16, 30–34. [Google Scholar] [CrossRef]
- World Health, O. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- DiLorenzo, T.M.; Bargman, E.P.; Stucky-Ropp, R.; Brassington, G.S.; Frensch, P.A.; LaFontaine, T. Long-term effects of aerobic exercise on psychological outcomes. Prev. Med. 1999, 28, 75–85. [Google Scholar] [CrossRef] [Green Version]
- Knapen, J.; Vancampfort, D.; Morien, Y.; Marchal, Y. Exercise therapy improves both mental and physical health in patients with major depression. Disabil. Rehabil. 2015, 37, 1490–1495. [Google Scholar] [CrossRef]
- Kratzer, A.; Luttenberger, K.; Karg-Hefner, N.; Weiss, M.; Dorscht, L. Bouldering psychotherapy is effective in enhancing perceived self-efficacy in people with depression: Results from a multicenter randomized controlled trial. BMC Psychol. 2021, 9, 126. [Google Scholar] [CrossRef]
- Choi, K.-S.; Hong, S.-G. The Effect of Climbing Exercise Program on Self-efficacy for the College Students. J. Adv. Concr. Technol. 2019, 9, 243–247. [Google Scholar]
- Luttenberger, K.; Stelzer, E.M.; Forst, S.; Schopper, M.; Kornhuber, J.; Book, S. Indoor rock climbing (bouldering) as a new treatment for depression: Study design of a waitlist-controlled randomized group pilot study and the first results. BMC Psychiatry 2015, 15, 201–211. [Google Scholar] [CrossRef] [Green Version]
- Stelzer, E.M.; Book, S.; Graessel, E.; Hofner, B.; Kornhuber, J.; Luttenberger, K. Bouldering psychotherapy reduces depressive symptoms even when general physical activity is controlled for: A randomized controlled trial. Heliyon 2018, 4, e00580. [Google Scholar] [CrossRef] [PubMed]
- Fruhauf, A.; Niedermeier, M.; Sevecke, K.; Haid-Stecher, N.; Albertini, C.; Richter, K.; Schipflinger, S.; Kopp, M. Affective responses to climbing exercises in children and adolescents during in-patient treatment for mental health disorders a pilot study on acute effects of different exercise interventions. Psychiatry Res. 2020, 291, 113245. [Google Scholar] [CrossRef] [PubMed]
- Kleinstauber, M.; Reuter, M.; Doll, N.; Fallgatter, A.J. Rock climbing and acute emotion regulation in patients with major depressive disorder in the context of a psychological inpatient treatment: A controlled pilot trial. Psychol. Res. Behav. Manag. 2017, 10, 277–281. [Google Scholar] [CrossRef] [Green Version]
- Barrios Lafragüeta, M. Therapeutic Climbing: Pilot Study on the Influence of Bouldering on the Improvement of Depression Symptomatology; University of Zaragoza: Huesca, Spain, 2018. [Google Scholar]
- Schwarz, L.; Dorscht, L.; Book, S.; Stelzer, E.M.; Kornhuber, J.; Luttenberger, K. Long-term effects of bouldering psychotherapy on depression: Benefits can be maintained across a 12-month follow-up. Heliyon 2019, 5, e02929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fischer, L. Long-Term Effects of a Therapeutic Bouldering Group on Depression: Results of the Follow-Up Investigation of the Study "Climbing and Mood "Twelve Months after the Start of the Study; Friedrich-Alexander University, Erlangen-Nuremberg (FAU): Erlangen, Germany, 2021. [Google Scholar]
- Karg, N.; Dorscht, L.; Kornhuber, J.; Luttenberger, K. Bouldering psychotherapy is more effective in the treatment of depression than physical exercise alone: Results of a multicentre randomised controlled intervention study. BMC Psychiatry 2020, 20, 116. [Google Scholar] [CrossRef] [Green Version]
- Krall, C. The Use of Bouldering Psychotherapy (BPT) as an Effective Treatment for Depression. Master’s Thesis, Pacific University, Forest Grove, OR, USA, 2021. [Google Scholar]
- Luttenberger, K.; Karg-Hefner, N.; Berking, M.; Kind, L.; Weiss, M.; Kornhuber, J.; Dorscht, L. Bouldering psychotherapy is not inferior to cognitive behavioural therapy in the group treatment of depression: A randomized controlled trial. Br. J. Clin. Psychol. 2021, 61, 465–493. [Google Scholar] [CrossRef] [PubMed]
- Schwarzkopf, L.; Dorscht, L.; Kraus, L.; Luttenberger, K. Is bouldering-psychotherapy a cost-effective way to treat depression when compared to group cognitive behavioral therapy–results from a randomized controlled trial. BMC Health Serv. Res. 2021, 21, 1162. [Google Scholar] [CrossRef]
- Kang, Y.; Yu, H. Effects of Exercise on Low Back Pain:a Meta-analysis. China Sport Sci. 2019, 39, 63–72. [Google Scholar]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [Green Version]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 2006, 15, s192–s300. [Google Scholar] [CrossRef] [Green Version]
- Heitkamp, H.C.; Worner, C.; Horstmann, T. Sport climbing with adolescents: Effect on spine stabilising muscle strength. Sportverletz. Sportsc. 2005, 19, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Mally, F.; Litzenberger, S.; Sabo, A. Surface electromyography measurements of dorsal muscle cross-activation in therapeutic climbing. Procedia Eng. 2013, 60, 22–27. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.-H.; Lee, J.-I. Comparison of trunk muscle activity during static standing position and standing position on therapeutic climbing wall. J. Kor. Phys. Ther. 2014, 26, 27–32. [Google Scholar]
- Engbert, K.; Weber, M. The effects of therapeutic climbing in patients with chronic low back pain: A randomized controlled study. Spine 2011, 36, 842–849. [Google Scholar] [CrossRef] [PubMed]
- Dittrich, M.E.G.; Bosse, A.; Beyer, W.F. Therapeutic climbing for chronic non-specific back pain. OUP 2014, 12, 581–583. [Google Scholar]
- Buechter, R.B.; Fechtelpeter, D. Climbing for preventing and treating health problems: A systematic review of randomized controlled trials. Ger. Med. Sci. 2011, 9, 1–9. [Google Scholar] [CrossRef]
- Kim, S.H.; Seo, D.Y. Effects of a therapeutic climbing program on muscle activation and SF-36 scores of patients with lower back pain. J. Phys. Ther. Sci. 2015, 27, 743–746. [Google Scholar] [CrossRef] [Green Version]
- Schinhan, M.; Neubauer, B.; Pieber, K.; Gruber, M.; Kainberger, F.; Castellucci, C.; Olischar, B.; Maruna, A.; Windhager, R.; Sabeti-Aschraf, M. Climbing Has a Positive Impact on Low Back Pain: A Prospective Randomized Controlled Trial. Clin. J. Sport Med. 2016, 26, 199–205. [Google Scholar] [CrossRef]
- Qiu, W.; Xu, Y. Chinese Expert Consensus on the Diagnosis and Treatment of Multiple Sclerosis (2018 Edition). Chin. J. Neuroimmunol. Neurol. 2018, 25, 387–394. [Google Scholar]
- Dobson, R.; Giovannoni, G. Multiple sclerosis—A review. Eur. J. Neurol. 2019, 26, 27–40. [Google Scholar] [CrossRef] [Green Version]
- Pilutti, L.; Dlugonski, D.; Sandroff, B.; Klaren, R.; Motl, R. Randomized controlled trial of a behavioral intervention targeting symptoms and physical activity in multiple sclerosis. Mult. Scler. J. 2014, 20, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; Pilutti, L.A. The benefits of exercise training in multiple sclerosis. Nat. Rev. Neurol. 2012, 8, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Kern, C.; Elmenhorst, J.; Oberhoffer, R. Effect of sport climbing on patients with multiple sclerosis–Hints or evidence? Neurol. Und Rehabil. 2013, 19, 247–256. [Google Scholar]
- Hof, F.-V. Climbing and Multiple Sclerosis: Influence on Psychosocial and Motor Parameters. Master’s Thesis, Kiel University, Kiel, Germany, 2014. [Google Scholar]
- Steimer, J.; Weissert, R. Effects of Sport Climbing on Multiple Sclerosis. Front. Physiol. 2017, 8, 1021–1231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muehlbauer, T.; Granacher, U.; Jockel, B.; Kittel, R. Muscle activation during therapeutic climbing exercises. Sportverletz. Sportsc. 2013, 27, 162–168. [Google Scholar] [CrossRef]
- Kim, E.-J.; Kim, S.-H. A comparison of shoulder stabilizer muscle activities of therapeutic climbing and isometric exercise in patients with shoulder impingement syndrome. J. Kor. Phys. Ther. 2016, 28, 88–94. [Google Scholar] [CrossRef] [Green Version]
- Puhringer, M.; Strutzenberger, G.; Leitl, D.; Holzner, K.; Schwameder, H. Possibilities of altering arm and shoulder muscle activation in a static therapeutic climbing exercise through arm position, hand support and wall inclination. Eur. J. Sport Sci. 2017, 17, 1212–1219. [Google Scholar] [CrossRef] [Green Version]
- Grzybowski, C.; Donath, L.; Wagner, H. Relationship between trunk muscle activity and wall inclination in static climbing positions: Implications for climbing therapy. Sportverletz. Sportsc. 2014, 28, 75–84. [Google Scholar]
- Gaulrapp, H.; Eckstein, S.; Auracher, M. Bilateral calcaneus fracture in a paraglider pilot: Rehabilitation using climbing therapy. Phys. Med. Rehabil. Med. Spa Med. 2000, 10, 65–70. [Google Scholar]
- Schluep, A. Climbing as an Intervention for Idiopathic Scoliosis: The Effects of Therapeutic Climbing on Trunk Muscles and the Transfer of Findings to the Treatment of Scoliosis Patients. Bachelor’s Thesis, Zurich University of Applied Sciences, Winterthur, Switzerland, 2016. [Google Scholar]
- Tiedemann, C. Therapeutic Climbing for Supportive Treatment of Obsessive-Compulsive Disorder in Children and Adolescents; University of Applied Science: Neubrandenburg, Germany, 2010. [Google Scholar]
- Reiter, M.; Heimbeck, A.; Müller, M.; Voderholzer, U. Movement therapy and therapeutic climbing. Der Neurol. Und Psychiater 2014, 15, 62–66. [Google Scholar] [CrossRef]
- Stemberger, M.; Schmit, E.; Czepa, D.; Kurnik, K.; Spannagl, M. Climbing therapy under PK-tailored prophylaxis. Hamostaseologie 2014, 34, 13–16. [Google Scholar] [CrossRef]
- Stemberger, M.; Schmit, E.; Kurnik, K.; Spannagl, M. Motivational effects of top-rope climbing therapy under individualized prophylaxis: A pilot study in young adults with severe haemophilia. Haemophilia 2015, 21, e504–e507. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, C.; Kallenbach, F.; Volland, L.; Barnes, R.F.; Moran, C.M.; Geyer, C.; von Velsen, R.; von Drygalski, A.; Stemberger, M.A. “Hemophilia Vertical”: Effects of Therapeutic Rock Climbing on Joint Health in Hemophilia Patients with Severe Arthropathies. Blood 2016, 128, 4754. [Google Scholar] [CrossRef]
- Schroeder, C.; Barnes, R.F.; Volland, L.; Nguyen, S.; von Drygalski, A. Effects of top rope climbing therapy on joint health in adult haemophilia patients with severe arthropathies. J. Haemoph. Prac. 2018, 5, 93–102. [Google Scholar] [CrossRef] [Green Version]
- Soravia, L.; Stocker, E.; Schläfli, K.; Schönenberger, N.; Dittrich, T.; Grossniklaus, C. Climbing as an opportunity in addiction treatment: Effects of therapeutic climbing on anxiety, self-esteem, and self-efficacy expectancy in patients with alcohol dependence. Addict. Ther. 2015, 16, 13–18. [Google Scholar]
- Hörl, D. Therapeutic Climbing—A Qualitative Analysis of the Effects and Effective Factors Using the Treatment of Anxiety and Obsessive-Compulsive Disorders as an Example. Master’s Thesis, University of Applied Sciences Landshut, Landshut, Germany, 2015. [Google Scholar]
- Böhm, H.; Rammelmayr, M.K.; Döderlein, L. Effects of climbing therapy on gait function in children and adolescents with cerebral palsy—A randomized, controlled crossover trial. Eur. J. Physiother. 2014, 17, 1–8. [Google Scholar] [CrossRef]
- Christensen, M.S.; Jensen, T.; Voigt, C.B.; Nielsen, J.B.; Lorentzen, J. To be active through indoor-climbing: An exploratory feasibility study in a group of children with cerebral palsy and typically developing children. BMC Neurol. 2017, 17, 112. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.S.; Song, C.S. Effects of therapeutic climbing activities wearing a weighted vest on a child with attention deficit hyperactivity disorder: A case study. J. Phys. Ther. Sci. 2015, 27, 3337–3339. [Google Scholar] [CrossRef] [Green Version]
- Crawford, J.J.; Vallance, J.K.; Holt, N.L.; Bell, G.J.; Steed, H.; Courneya, K.S. A Pilot Randomized, Controlled Trial of a Wall Climbing Intervention for Gynecologic Cancer Survivors. Oncol. Nurs. Forum 2017, 44, 77–86. [Google Scholar] [CrossRef]
- Kokaridas, D.; Demerouti, I.; Margariti, P.; Krommidas, C. The Effect of an Indoor Climbing Program on Improving Handgrip Strength and Traverse Speed of Children with and without Autism Spectrum Disorder. Palaestra 2018, 32, 39–44. [Google Scholar]
- Taylor, J.A. The Effects of Rock Climbing on Functional Strength, Spatial Reasoning, and Executive Function in Children with Autism. Ph.D. Thesis, Ohio Dominican University, Columbus, OH, USA, 2017. [Google Scholar]
- Daggelmann, J.; Prokop, A.; Losse, V.; Maas, V.; Otten, S.; Bloch, W. Indoor Wall Climbing with Childhood Cancer Survivors: An Exploratory Study on Feasibility and Benefits. Klin. Padiatr. 2020, 232, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Bibro, M.A.; Zarow, R. The Influence of Climbing Activities on Physical Fitness of People with Intellectual Disabilities. Int. J. Disabil. Dev. Ed. 2021, 68, 1–10. [Google Scholar] [CrossRef]
- Marianne Anke, S.; Sylvie, K.; Jérôme, P.; Shahid, B.; Thomas, F.; Dieter Georg, R.; Karin, D. Effect of long-term climbing training on cerebellar ataxia: A case series. Rehabil. Res. Pract. 2011, 2011, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Park, C.-B.; Kim, B.-G.; Lee, S.-I. Effects of Therapeutic Climbing Training on Upper Limb Function and Quality of Life in Stroke Patients. J. Korea Acad.-Ind. Coop. Soc. 2019, 20, 292–299. [Google Scholar] [CrossRef]
- Lee, S.; Ko, M.; Park, S. Effects of Therapeutic Climbing Training on the Balance and Gait Ability in Chronic Stroke Patients. J. Int. Acad. Phys. Ther. Res. 2020, 11, 2126–2134. [Google Scholar] [CrossRef]
- Langer, A.; Hasenauer, S.; Flotz, A.; Gassner, L.; Pokan, R.; Dabnichki, P.; Wizany, L.; Gruber, J.; Roth, D.; Zimmel, S. A randomised controlled trial on effectiveness and feasibility of sport climbing in Parkinson’s disease. NPJ Parkinson’s Dis. 2021, 7, 49. [Google Scholar] [CrossRef] [PubMed]
- Woolstenhulme, J.G.; Aguero, N.; Ruckert, E.; Leach, S.J. Rock Climbing as a Novel Intervention to Improve Function in Parkinson’s Disease: A Case Series. Med. Sci. Sports Exerc. 2017, 49, 28. [Google Scholar] [CrossRef]
- Telebuh, M.; Grozdek-Čovčić, G.; Schuster, S. Physiotherapy and recreation in spinal cord injury—A case study. Acta Kinesiol. 2017, 11, 77–82. [Google Scholar]
- Lobelo, F.; Duperly, J.; Frank, E. Physical activity habits of doctors and medical students influence their counselling practices. Br. J. Sports Med. 2009, 43, 89–92. [Google Scholar] [CrossRef]
- Huang, X.; Li, X.; Liu, S.; Li, Y.; Xu, H.; Pang, W. Advance in Neural Control in Eccentric Exercise. Chin. J. Rehabil. Theory Pract. 2021, 27, 97–101. [Google Scholar]
- Shi, S.; Pang, W. Application Progress of Eccentric Exercise. Train. Rehabil. 2018, 24, 173–178. [Google Scholar]
- Bahrke, M.S.; Morgan, W.P. Anxiety reduction following exercise and meditation. Cogn. Ther. Res. 1978, 2, 323–333. [Google Scholar] [CrossRef]
- Morgan, W.P. Affective beneficence of vigorous physical activity. Med. Sci. Sports Exerc. 1985, 17, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Leith, L.M. Foundations of Exercise and Mental Health; Fitness Information Technology: Morgantown, WV, USA, 2010. [Google Scholar]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 1, 139–161. [Google Scholar] [CrossRef]
| Study | Disease Type | N | Sex | Age (Years) | Study Design | Main Conclusions |
|---|---|---|---|---|---|---|
| Stemberger et al. [74] | Hemophilia | 1 | M | 25 | 34 weeks TC | Bleeding rate ↓, joint health ↑, quality of life ↑, rock climbing ability ↑ |
| Stemberger et al. [75] | Hemophilia | 9 | - | 16–35 | 2 h × 34 weeks TC | Bleeding rate ↓, joint health ↑, quality of life ↑ |
| Schroeder et al. [76] | Hemophilia | 12 | M | 31 | 12 times TC | Range of motion ↑, rock climbing ability ↑, quality of life ↑, inflammation ↓ |
| Schroeder et al. [77] | Hemophilia | 6 | M | ≥21 | 12 times TC | Bleeding rate ↓, joint health and dorsiflexion ↑, quality of life ↑, rock climbing ability ↑ |
| Lee et al. [82] | Attention deficit hyperactivity disorder | 1 | M | 7 | 3 times × 4 weeks × 60 min TC | Brain waves and attention ↑ |
| Crawford et al. [83] | Gynecologic cancer | E: 24 | F | 52.5 ± 12.7 | 2 times × 8 weeks × 2 h TC | the E is superior to the C for the 6 min walk, 30 s chair stand, 30 s arm curls, sit and reach, 8-foot up-and-go, grip strength-right, and grip strength-left assessments. |
| C: 11 | F | 54.1 ± 10.5 | 2 times × 8 weeks × 2 h regular exercise | |||
| Böhm et al. [80] | Cerebral palsy | E: 8 | 6M2F | 13 ± 4.3 | 2 times × 6 weeks × 1.5 h TC and then traditional exercise | Walking speed ↑, step length ↑ |
| C: 8 | 6M2F | 13 ± 4.3 | 2 times × 6 weeks × 1.5 h traditional exercise and then TC | Gait profile score ↑, ankle dorsiflexion ↑, knee flexion ↑, walking speed ↑, step length ↑ | ||
| Christensen et al. [81] | Cerebral palsy | E:11 | 4M7F | 11.6 ± 0.8 | 3 times × 3 weeks × 150 min TC | Climbing ability ↑, number of climbing routes ↑, sitting-standing test ↑, muscle coherence ↑,maximal hand or finger strength-,cognitive abilities or psychological well-being - |
| C:6 | 4F2M | 11.8 ± 0.9 | Climbing ability ↑, Climbing speed↑, maximal hand or finger strength-, cognitive abilities or psychological well-being - | |||
| Kokaridas et al. [84] | Autism spectrum disorder | E:3 | M | 9 | 2 times × 12 weeks × 40 min TC | Grip strength ↑, speed ↑ |
| C:3 | M | 9 | ||||
| Daggelmann et al. [86] | Cancer | 13 | 5F8M | 11.5 ± 4.47 | 1 time × 8 weeks × 60 min TC | Dorsiflexion strength ↑, Ankle dorsifleion-range of motion ↑, legs flexed ↑ |
| Bibro et al. [87] | Intellectual disabilities | E: 32 | 13F19M | 21.8 ± 2.5 | 2 times × 15 weeks × 60 min TC | Balance ↑, arm hang test↑, distance to push a 2 kg solid ball ↑, grip strength ↑ |
| C: 36 | 8F28M | 19.8 ± 2 | No intervention | No significant change | ||
| Taylor et al. [85] | Autism | 7 | M | 8–14 | 1 time × 6 weeks × 90 min TC | Cognitive tracking test and grip strength ↑ |
| Marianne et al. [88] | Cerebellar ataxia | 4 | M | 22–56 | 6 weeks of TC | Speed ↑, balance ↑, hand flexibility ↑ |
| Park et al. [89] | Stroke | E: 7 | 6M1F | 45.43 ± 16.46 | 3 times × 6 weeks × 30 min TC | Compared with the control group, the experimental group showed quality of life ↑, upper limb function ↑, vitality ↑, mental health ↑ |
| C:7 | 5M2F | 55.57 ± 7.39 | Traditional treatment | |||
| Lee et al. [90] | Stroke | E: 7 | 6M1F | 45.43 ± 16.46 | 5 times × 60 min × 6 weeks standard rehabilitation exercise + 3 times 30 min × 6 weeks TC | Compared with the control group, the experimental group showed balance ability and walking ability ↑ |
| C: 7 | 5M2F | 55.57 ± 7.39 | 5 times × 60 min × 6 weeks standard rehabilitation | |||
| Kim et al. [67] | Shoulder impingement syndrome | E: 10 | 5M5F | 54 ± 4.1 | 3 times × 8 weeks of TC | DASH score ↓, flexion and abduction ↑, external and internal rotation ↑, upper trapezius activity ↑ |
| C:10 | 6M4F | 55.6 ± 7.4 | 8 weeks general isometric exercise | DASH score ↓, flexion and abduction ↑, serratus anterior and lower trapezius activity ↑ | ||
| Woolstenhulme et al. [92] | Parkinson’s disease | 3 | M | 70–73 | 3 × 8 weeks of TC | Confidence ↑, leg strength ↑, dynamic balance ↑ |
| Telebuh et al. [93] | Spinal cord injury | 1 | M | 34 | 1–2 times × 12 weeks × 90 min TC + 30 min home exercise | Static balance ↑, gait ↑ |
| Langer et al. [91] | Parkinson’s disease | 48 | 30M18F | 64 ± 8 | 12 weeks TC vs. 12 weeks physical exercise | MDS-UPDRS III score ↓, symptoms of bradykinesia, rigidity and tremor ↓ vs. no significant change |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, S.; Gong, X.; Li, H.; Li, Y. The Origin, Application and Mechanism of Therapeutic Climbing: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 9696. https://doi.org/10.3390/ijerph19159696
Liu S, Gong X, Li H, Li Y. The Origin, Application and Mechanism of Therapeutic Climbing: A Narrative Review. International Journal of Environmental Research and Public Health. 2022; 19(15):9696. https://doi.org/10.3390/ijerph19159696
Chicago/Turabian StyleLiu, Sheng, Xiaoqin Gong, Hanping Li, and Yuan Li. 2022. "The Origin, Application and Mechanism of Therapeutic Climbing: A Narrative Review" International Journal of Environmental Research and Public Health 19, no. 15: 9696. https://doi.org/10.3390/ijerph19159696





