Dose–Response Analysis of the Tubular and Glomerular Effects of Chronic Exposure to Environmental Cadmium
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Collection of Biological Specimens and Analyses
2.3. Estimated Glomerular Filtration Rate (eGFR)
2.4. Normalization of Excretion of Cd, β2M and NAG to Ecr and Ccr
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristics of the Study Subjects
3.2. Effects of Residential Location and Smoking Habit on Cadmium Excretion Levels
3.3. Associations of ECd/Ecr vs. ECd/Ccr with eGFR, β2M and NAG
3.4. Associations of Cadmium Excretion with Elevated Risks of Nephrotoxicity
3.5. Comparing eGFR Reductions and Increases in ENAG and Eβ2M among Subjects
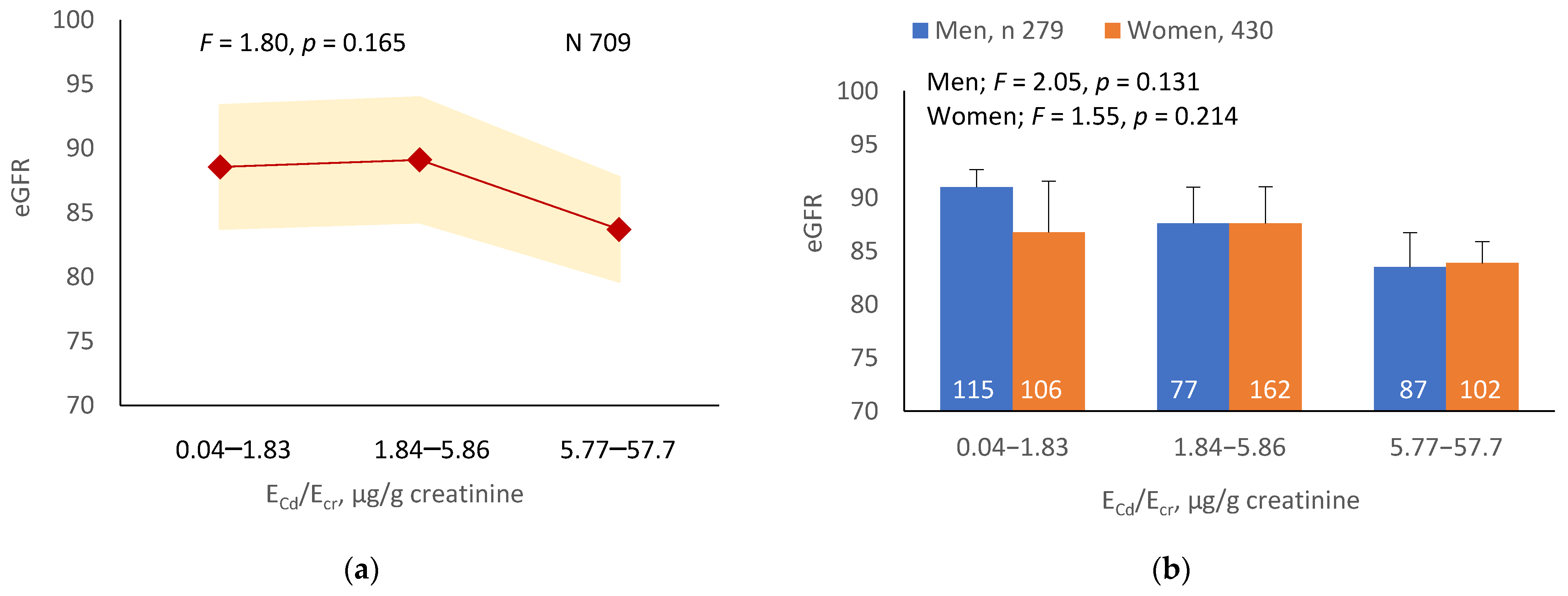
3.5.1. Cadmium-Dose-Dependent Reductions in eGFR
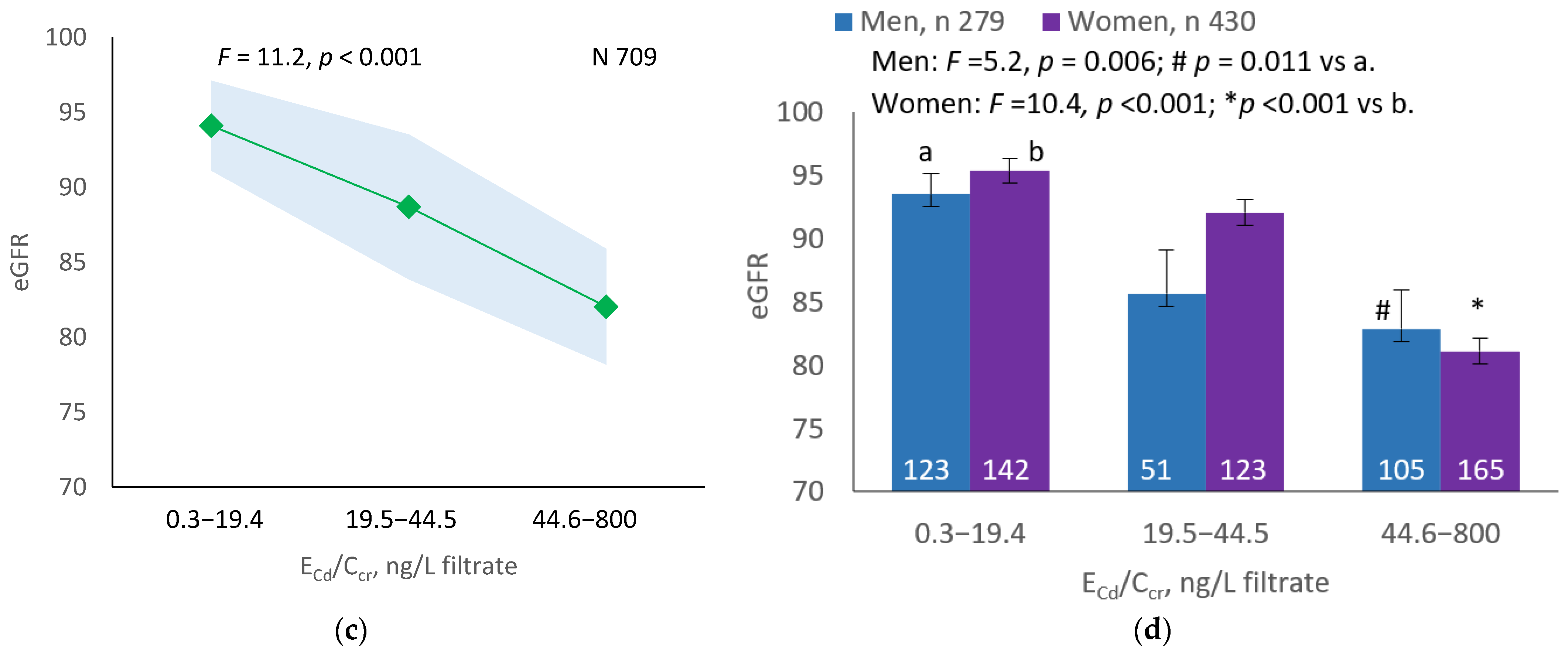
3.5.2. Cadmium-Dose-Dependent Increases in NAG Excretion
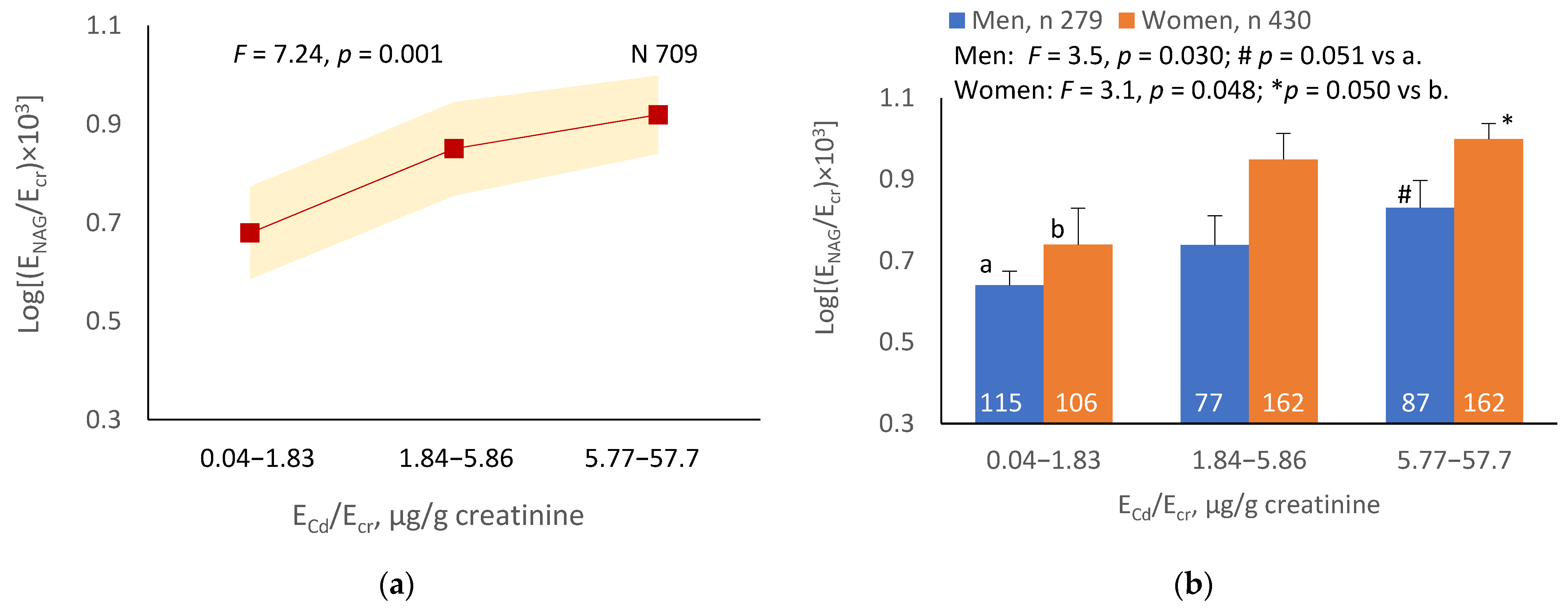
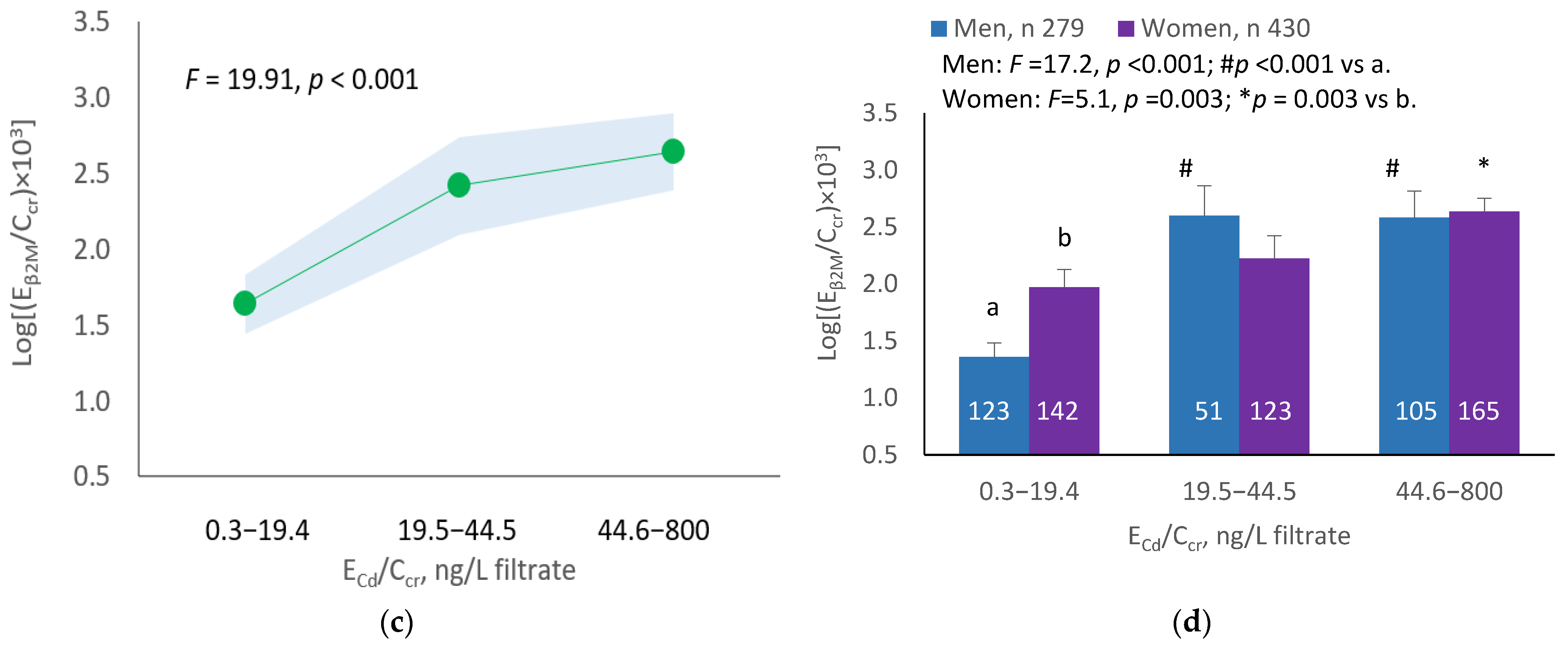
3.5.3. Cadmium-Dose-Dependent Increases in β2M Excretion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nordberg, M.; Nordberg, G.F. Metallothionein and cadmium toxicology-historical review and commentary. Biomolecules 2022, 12, 360. [Google Scholar] [CrossRef] [PubMed]
- Genchi, G.; Sinicropi, M.S.; Lauria, G.; Carocci, A.; Catalano, A. The effects of cadmium toxicity. Int. J. Environ. Res. Public Health 2020, 17, 3782. [Google Scholar] [CrossRef]
- Thévenod, F.; Lee, W.K.; Garrick, M.D. Iron and cadmium entry into renal mitochondria: Physiological and toxicological implications. Front. Cell Dev. Biol. 2020, 8, 848. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Vesey, D.A.; Gobe, G.C. Current health risk assessment practice for dietary cadmium: Data from different countries. Food Chem. Toxicol. 2017, 106, 430–445. [Google Scholar] [CrossRef] [PubMed]
- Aoshima, K. Epidemiology of renal tubular dysfunction in the inhabitants of a cadmium-polluted area in the Jinzu River basin in Toyama Prefecture. Tohoku J. Exp. Med. 1987, 152, 151–172. [Google Scholar] [CrossRef]
- Horiguchi, H.; Aoshima, K.; Oguma, E.; Sasaki, S.; Miyamoto, K.; Hosoi, Y.; Katoh, T.; Kayama, F. Latest status of cadmium accumulation and its effects on kidneys, bone, and erythropoiesis in inhabitants of the formerly cadmium-polluted Jinzu River Basin in Toyama, Japan, after restoration of rice paddies. Int. Arch. Occup. Environ. Health 2010, 83, 953–970. [Google Scholar] [CrossRef]
- Argyropoulos, C.P.; Chen, S.S.; Ng, Y.H.; Roumelioti, M.E.; Shaffi, K.; Singh, P.P.; Tzamaloukas, A.H. Rediscovering beta-2 microglobulin as a biomarker across the spectrum of kidney diseases. Front. Med. 2017, 4, 73. [Google Scholar] [CrossRef]
- Portman, R.J.; Kissane, J.M.; Robson, A.M. Use of B2-microglobulin to diagnose tubulo-interstitial renal lesions in children. Kidney Int. 1986, 30, 91–98. [Google Scholar] [CrossRef]
- Gauthier, C.; Nguyen-Simonnet, H.; Vincent, C.; Revillard, J.-P.; Pellet, M.V. Renal tubular absorption of beta 2 micro-globulin. Kidney Int. 1984, 26, 170–175. [Google Scholar] [CrossRef]
- JECFA. Proceedings of the Joint FAO/WHO Expert Committee on Food Additives and Contaminants, Seventy-Third Meeting, Geneva, Switzerland, 8–17 June 2010; Summary and Conclusions; JECFA/73/SC; Food and Agriculture Organization of the United Nations: Rome, Italy; World Health Organization: Geneva, Switzerland, 2011; Available online: https://apps.who.int/iris/handle/10665/44521 (accessed on 31 July 2022).
- Wong, C.; Roberts, S.M.; Saab, I.N. Review of regulatory reference values and background levels for heavy metals in the human diet. Regul. Toxicol. Pharmacol. 2022, 130, 105122. [Google Scholar] [CrossRef]
- Moffett, D.B.; Mumtaz, M.M.; Sullivan, D.W., Jr.; Whittaker, M.H. Chapter 13, General Considerations of Dose-Effect and Dose-Response Relationships. In Handbook on the Toxicology of Metals, 5th ed.; Volume I: General Considerations; Nordberg, G., Costa, M., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 299–317. [Google Scholar]
- Satarug, S.; Vesey, D.A.; Nishijo, M.; Ruangyuttikarn, W.; Gobe, G.C. The inverse association of glomerular function and urinary β2-MG excretion and its implications for cadmium health risk assessment. Environ. Res. 2019, 173, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, P.M.; Costanzi, S.; Naticchia, A.; Sturniolo, A.; Gambaro, G. Low level exposure to cadmium increases the risk of chronic kidney disease: Analysis of the NHANES 1999–2006. BMC Public Health 2010, 10, 304. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Boonprasert, K.; Gobe, G.C.; Ruenweerayut, R.; Johnson, D.W.; Na-Bangchang, K.; Vesey, D.A. Chronic exposure to cadmium is associated with a marked reduction in glomerular filtration rate. Clin. Kidney J. 2018, 12, 468–475. [Google Scholar] [CrossRef]
- Tsai, K.F.; Hsu, P.C.; Lee, C.T.; Kung, C.T.; Chang, Y.C.; Fu, L.M.; Ou, Y.C.; Lan, K.C.; Yen, T.H.; Lee, W.C. Association between enzyme-linked immunosorbent assay-measured kidney injury markers and urinary cadmium levels in chronic kidney disease. J. Clin. Med. 2021, 11, 156. [Google Scholar] [CrossRef] [PubMed]
- Win-Thu, M.; Myint-Thein, O.; Win-Shwe, T.-T.; Mar, O. Environmental cadmium exposure induces kidney tubular and glomerular dysfunction in the Myanmar adults. J. Toxicol. Sci. 2021, 46, 319–328. [Google Scholar] [CrossRef]
- Schnaper, H.W. The tubulointerstitial pathophysiology of progressive kidney disease. Adv. Chron. Kidney Dis. 2017, 24, 107–116. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Ruangyuttikarn, W.; Nishijo, M.; Gobe, G.C.; Phelps, K.R. The source and pathophysiologic significance of excreted cadmium. Toxics 2019, 7, 55. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Nishijo, M.; Ruangyuttikarn, W.; Gobe, G.C.; Phelps, K.R. The effect of cadmium on GFR is clarified by normalization of excretion rates to creatinine clearance. Int. J. Mol. Sci. 2021, 22, 1762. [Google Scholar] [CrossRef]
- Satarug, S.; Swaddiwudhipong, W.; Ruangyuttikarn, W.; Nishijo, M.; Ruiz, P. Modeling cadmium exposures in low- and high-exposure areas in Thailand. Environ. Health Perspect. 2013, 121, 531–536. [Google Scholar] [CrossRef]
- Hornung, R.W.; Reed, L.D. Estimation of average concentration in the presence of nondetectable values. Appl. Occup. Environ. Hyg. 1990, 5, 46–51. [Google Scholar] [CrossRef]
- Levey, A.S.; Becker, C.; Inker, L.A. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: A systematic review. JAMA 2015, 313, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Soveri, I.; Berg, U.B.; Björk, J.; Elinder, C.G.; Grubb, A.; Mejare, I.; Sterner, G.; Bäck, S.E.; SBU GFR Review Group. Measuring GFR: A systematic review. Am. J. Kidney Dis. 2014, 64, 411–424. [Google Scholar] [CrossRef] [PubMed]
- White, C.A.; Allen, C.M.; Akbari, A.; Collier, C.P.; Holland, D.C.; Day, A.G.; Knoll, G.A. Comparison of the new and traditional CKD-EPI GFR estimation equations with urinary inulin clearance: A study of equation performance. Clin. Chim. Acta 2019, 488, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Phelps, K.R.; Gosmanova, E.O. A generic method for analysis of plasma concentrations. Clin. Nephrol. 2020, 94, 43–49. [Google Scholar] [CrossRef]
- Jalili, C.; Kazemi, M.; Cheng, H.; Mohammadi, H.; Babaei, A.; Taheri, E.; Moradi, S. Associations between exposure to heavy metals and the risk of chronic kidney disease: A systematic review and meta-analysis. Crit. Rev. Toxicol. 2021, 51, 165–182. [Google Scholar] [CrossRef]
- Byber, K.; Lison, D.; Verougstraete, V.; Dressel, H.; Hotz, P. Cadmium or cadmium compounds and chronic kidney disease in workers and the general population: A systematic review. Crit. Rev. Toxicol. 2016, 46, 191–240. [Google Scholar] [CrossRef]
- Butler-Dawson, J.; James, K.A.; Krisher, L.; Jaramillo, D.; Dally, M.; Neumann, N.; Pilloni, D.; Cruz, A.; Asensio, C.; Johnson, R.J.; et al. Environmental metal exposures and kidney function of Guatemalan sugarcane workers. J. Expo. Sci. Environ. Epidemiol. 2022, 32, 461–471. [Google Scholar] [CrossRef]
- Akesson, A.; Lundh, T.; Vahter, M.; Bjellerup, P.; Lidfeldt, J.; Nerbrand, C.; Samsioe, G.; Strömberg, U.; Skerfving, S. Tubular and glomerular kidney effects in Swedish women with low environmental cadmium exposure. Environ. Health Perspect. 2005, 113, 1627–1631. [Google Scholar] [CrossRef]
- Barregard, L.; Sallsten, G.; Lundh, T.; Mölne, J. Low-level exposure to lead, cadmium and mercury, and histopathological findings in kidney biopsies. Environ. Res. 2022, 211, 113119. [Google Scholar] [CrossRef]
- Prozialeck, W.C.; Vaidya, V.S.; Liu, J.; Waalkes, M.P.; Edwards, J.R.; Lamar, P.C.; Bernard, A.M.; Dumont, X.; Bonventre, J.V. Kidney injury molecule-1 is an early biomarker of cadmium nephrotoxicity. Kidney Int. 2007, 72, 985–993. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.R.; Wang, P.; Liang, X.X.; Tan, C.S.; Tan, J.B.; Wang, J.; Huang, Q.; Huang, R.; Li, Z.X.; Chen, W.C.; et al. Associations between urinary excretion of cadmium and renal biomarkers in non-smoking females: A cross-sectional study in rural areas of South China. Int. J. Environ. Res. Public Health 2015, 12, 11988–12001. [Google Scholar] [CrossRef] [PubMed]
- Pennemans, V.; De Winter, L.M.; Munters, E.; Nawrot, T.S.; Van Kerkhove, E.; Rigo, J.M.; Reynders, C.; Dewitte, H.; Carleer, R.; Penders, J.; et al. The association between urinary kidney injury molecule 1 and urinary cadmium in elderly during long-term, low-dose cadmium exposure: A pilot study. Environ. Health 2011, 10, 77. [Google Scholar] [CrossRef] [PubMed]
- Prozialeck, W.C.; Edwards, J.R.; Lamar, P.C.; Liu, J.; Vaidya, V.S.; Bonventre, J.V. Expression of kidney injury molecule-1 (Kim-1) in relation to necrosis and apoptosis during the early stages of Cd-induced proximal tubular injury. Toxicol. Appl. Pharmacol. 2009, 238, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Ruangyuttikarn, W.; Panyamoon, A.; Nambunmee, K.; Honda, R.; Swaddiwudhipong, W.; Nishijo, M. Use of the kidney injury molecule-1 as a biomarker for early detection of renal tubular dysfunction in a population chronically exposed to cadmium in the environment. SpringerPlus 2013, 2, 533. [Google Scholar] [CrossRef]
- Navas-Acien, A.; Tellez-Plaza, M.; Guallar, E.; Muntner, P.; Silbergeld, E.; Jaar, B.; Weaver, V. Blood cadmium and lead and chronic kidney disease in US adults: A joint analysis. Am. J. Epidemiol. 2009, 170, 1156–1164. [Google Scholar] [CrossRef]
- Lin, Y.S.; Ho, W.C.; Caffrey, J.L.; Sonawane, B. Low serum zinc is associated with elevated risk of cadmium nephrotoxicity. Environ. Res. 2014, 134, 33–38. [Google Scholar] [CrossRef]
- Madrigal, J.M.; Ricardo, A.C.; Persky, V.; Turyk, M. Associations between blood cadmium concentration and kidney function in the U.S. population: Impact of sex, diabetes and hypertension. Environ. Res. 2018, 169, 180–188. [Google Scholar] [CrossRef]
- Crinnion, W.J. The CDC fourth national report on human exposure to environmental chemicals: What it tells us about our toxic burden and how it assists environmental medicine physicians. Altern. Med. Rev. 2010, 15, 101–108. [Google Scholar]
- Satarug, S.; Gobe, G.C.; Ujjin, P.; Vesey, D.A. A comparison of the nephrotoxicity of low doses of cadmium and lead. Toxics 2020, 8, 18. [Google Scholar] [CrossRef]
- Myong, J.-P.; Kim, H.-R.; Baker, D.; Choi, B. Blood cadmium and moderate-to-severe glomerular dysfunction in Korean adults: Analysis of KNHANES 2005-2008 data. Int. Arch. Occup. Environ. Health 2012, 85, 885–893. [Google Scholar] [CrossRef]
- Chung, S.; Chung, J.H.; Kim, S.J.; Koh, E.S.; Yoon, H.E.; Park, C.W.; Chang, Y.S.; Shin, S.J. Blood lead and cadmium levels and renal function in Korean adults. Clin. Exp. Nephrol. 2014, 18, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Lee, S.J. Association of blood heavy metal levels and renal function in Korean adults. Int. J. Environ. Res. Public Health 2022, 19, 6646. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Jafar, T.H.; Nitsch, D.; Neuen, B.L.; Perkovic, V. Chronic kidney disease. Lancet 2021, 398, 786–802. [Google Scholar] [CrossRef]

| Parameters | All Subjects, n 734 | Males, n 289 | Females, n 445 | p |
|---|---|---|---|---|
| From a low-exposure location (%) | 27.2 | 34.6 | 22.5 | <0.001 |
| Smoking (%) | 42.8 | 69.6 | 25.4 | <0.001 |
| Hypertension (%) | 31.7 | 29.1 | 33.5 | 0.209 |
| Diabetes (%) | 1.5 | 2.1 | 1.1 | 0.299 |
| Age, years | 48.1 ± 11.0 | 47.4 ± 13.5 | 48.6 ± 9.1 | 0.059 |
| BMI, kg/m2 | 23.2 ± 3.8 | 22.4 ± 3.3 | 23.7 ± 4.0 | <0.001 |
| eGFR a, mL/min/1.73 m2 | 91.0 ± 21.7 | 90.3 ± 22.9 | 91.4 ± 20.9 | 0.510 |
| Low eGFR b (%) | 9 | 10 | 8.3 | 0.426 |
| Plasma creatinine, mg/dL | 0.85 ± 0.28 | 1.00 ± 0.30 | 0.76 ± 0.22 | <0.001 |
| Urine creatinine, mg/dL | 85.59 ± 73.86 | 96.93 ± 73.34 | 78.95 ± 73.42 | <0.001 |
| Urine β2M, µg/L | 112 ± 24,510 | 98 ± 20,140 | 122 ± 26,989 | 0.401 |
| Urine NAG, U/L | 5.48 ± 9.96 | 4.97 ± 8.25 | 5.84 ± 10.86 | 0.045 |
| Urine Cd, µg/L | 2.34 ± 8.98 | 2.05 ± 10.87 | 2.54 ± 7.50 | 0.248 |
| Normalized to Ecr as Ex/Ecr c | ||||
| Eβ2M/Ecr, µg/g creatinine | 130 ± 20,620 | 101 ± 16,333 | 154 ± 22,997 | 0.016 |
| ENAG/Ecr, U/g creatinine | 6.40 ± 8.95 | 5.13 ± 4.73 | 7.39 ± 10.62 | <0.001 |
| ECd/Ecr, µg/g creatinine | 2.73 ± 6.61 | 2.12 ± 6.64 | 3.22 ± 6.57 | <0.001 |
| Normalized to Ccr as Ex/Ccr d | ||||
| Eβ2M/Ecr × 100, µg/L filtrate | 110 ± 29,676 | 101 ± 33,060 | 118 ± 27,253 | 0.320 |
| ENAG/Ecr × 100, U/L filtrate | 5.42 ± 9.40 | 5.11 ± 6.36 | 5.63 ± 10.91 | 0.166 |
| ECd/Ccr × 100, µg/L filtrate | 2.31 ± 7.82 | 2.11 ± 8.36 | 2.46 ± 7.44 | 0.249 |
| Parameters | Low-Exposure Area, n 200 | High-Exposure Area, n 534 | p |
|---|---|---|---|
| Smoking (%) | 23.5 | 50 | <0.001 |
| Diabetes (%) | 0 | 2.1 | 0.041 |
| Hypertension (%) | 19.5 | 36.3 | <0.001 |
| Mean age (range), years | 39.3 (16–60) | 51.4 (30–87) | <0.001 |
| Mean BMI (range), kg/m2 | 23.2 (13.1–39.0) | 23.2 (12.3–38.9) | 0.703 |
| Mean eGFR a (range) mL/min/1.73 m2 | 105.2 (65–138) | 85.6 (20–131) | <0.001 |
| Low eGFR b (%) | 0 | 12.4 | <0.001 |
| Plasma creatinine, mg/dL | 0.79 ± 0.17 | 0.87 ± 0.30 | <0.001 |
| Urine creatinine, mg/dL | 55.0 ± 66.0 | 101.0 ± 72.6 | <0.001 |
| Urine β2M, µg/L | 4.2 ± 119.3 | 382 ± 28,605 | <0.001 |
| Urine NAG, U/L | 3.68 ± 4.01 | 7.87 ± 9.77 | <0.001 |
| Urine Cd, µg/L | 0.23 ± 0.58 | 5.54 ± 9.67 | <0.001 |
| Normalized to Ecr as Ex/Ecr c | |||
| Eβ2M/Ecr, µg/g creatinine | 7.60 ± 118 | 379 ± 24,048 | <0.001 |
| ENAG/Ecr, U/g creatinine | 3.68 ± 4.01 | 7.87 ± 9.77 | <0.001 |
| ECd/Ecr, µg/g creatinine | 0.43 ± 0.44 | 5.48 ± 6.84 | <0.001 |
| Normalized to Ccr as Ex/Ccr d | |||
| Eβ2M/Ecr × 100, µg/L filtrate | 5.97 ± 111 | 330 ± 34,630 | <0.001 |
| ENAG/Ecr × 100, U/L filtrate | 2.90 ± 3.62 | 6.86 ± 10.42 | <0.001 |
| ECd/Ccr × 100, µg/L filtrate | 0.34 ± 0.38 | 4.77 ± 8.44 | <0.001 |
| Independent Variables/Factors | eGFR a, mL/min/1.73 m2 | Log[(ENAG/Ecr) × 103], µg/g Creatinine | Log[(Eβ2M/Ecr) × 103], µg/g Creatinine | |||
|---|---|---|---|---|---|---|
| β Coefficient b | p | β Coefficient | p | β Coefficient | p | |
| Age, years | −0.601 | <0.001 | −0.085 | 0.038 | 0.078 | 0.038 |
| Log2 [(ECd/Ecr) × 103], µg/g creatinine | −0.142 | <0.001 | 0.390 | <0.001 | 0.499 | <0.001 |
| BMI, kg/m2 | −0.027 | 0.344 | 0.083 | 0.019 | −0.040 | 0.216 |
| Sex | −0.084 | 0.008 | −0.178 | <0.001 | −0.037 | 0.291 |
| Hypertension | 0.036 | 0.202 | −0.180 | <0.001 | −0.091 | 0.004 |
| Diabetes | 0.070 | 0.011 | −0.024 | 0.486 | −0.008 | 0.788 |
| Smoking | 0.002 | 0.954 | −0.043 | 0.273 | −0.088 | 0.015 |
| Adjusted R2 | 0.485 | <0.001 | 0.222 | <0.001 | 0.347 | <0.001 |
| Independent Variables/Factors | eGFR a, mL/min/1.73 m2 | Log[(ENAG/Ccr) × 104], µg/L Filtrate | Log[(Eβ2M/Ccr) × 103], µg/L Filtrate | |||
|---|---|---|---|---|---|---|
| β Coefficient b | p | β Coefficient | p | β Coefficient | p | |
| Age, years | −0.513 | <0.001 | −0.012 | 0.775 | 0.062 | 0.100 |
| Log2 [(ECd/Ccr) × 105], µg/L filtrate | −0.300 | <0.001 | 0.455 | <0.001 | 0.540 | <0.001 |
| BMI, kg/m2 | −0.032 | 0.249 | 0.086 | 0.013 | −0.038 | 0.227 |
| Sex | −0.086 | 0.004 | −0.034 | 0.360 | −0.033 | 0.329 |
| Hypertension | 0.032 | 0.235 | −0.182 | <0.001 | −0.088 | 0.005 |
| Diabetes | 0.055 | 0.036 | −0.040 | 0.221 | −0.006 | 0.844 |
| Smoking | −0.023 | 0.455 | −0.037 | 0.338 | −0.081 | 0.021 |
| Adjusted R2 | 0.529 | <0.001 | 0.257 | <0.001 | 0.383 | <0.001 |
| Independent Variables/Factors | eGFR ≤ 60 mL/min/1.73 m2 | ENAG/Ecr ≥ 4 U/g Creatinine | Eβ2M/Ecr ≥ 300 µg/Creatinine | |||
|---|---|---|---|---|---|---|
| POR (95% CI) | p | POR (95% CI) | p | POR (95% CI) | p | |
| Age, years | 1.151 (1.112, 1.192) | <0.001 | 1.022 (1.002, 1.042) | 0.033 | 1.017 (0.999, 1.036) | 0.069 |
| BMI, kg/m2 | 1.074 (0.987, 1.168) | 0.096 | 1.012 (0.960, 1.068) | 0.654 | 0.996 (0.950, 1.045) | 0.880 |
| Diabetes | 2.211 (0.448, 10.92) | 0.330 | 1.121 (0.232, 5.421) | 0.887 | 0.653 (0.190, 2.241) | 0.498 |
| Sex | 1.140 (0.588, 2.329) | 0.719 | 1.653 (1.070, 2.553) | 0.023 | 1.004 (0.677, 1.489) | 0.986 |
| Smoking | 0.963 (0.469, 1.976) | 0.918 | 0.926 (0.589, 1.455) | 0.739 | 1.119 (0.760, 1,649) | 0.569 |
| Hypertension | 1.641 (0.852, 3.160) | 0.139 | 2.808 (1.745, 4.517) | <0.001 | 1.420 (0.990, 2.034) | 0.056 |
| ECd/Ecr, µg/g creatinine | ||||||
| 0.04–1.83 | Referent | Referent | Referent | |||
| 1.84–5.76 | 3.271 (0.705, 15.17) | 0.130 | 2.386 (1.469, 3.873) | <0.001 | 5.407 (3.281, 8.911) | <0.001 |
| 5.77–57.7 | 6.911 (1.545, 30.91) | 0.011 | 2.400 (1.415, 4.073) | 0.001 | 7.502 (4.440, 12.68) | <0.001 |
| Independent Variables/Factors | eGFR ≤ 60 mL/min/1.73 m2 | ENAG/Ccr × 100 ≥ 4 U/L Filtrate | Eβ2M/Ccr × 100 ≥ 300 µg/L Filtrate | |||
|---|---|---|---|---|---|---|
| POR (95% CI) | p | POR (95% CI) | p | POR (95% CI) | p | |
| Age, years | 1.146 (1.107, 1.188) | <0.001 | 1.043 (1.023, 1.064) | <0.001 | 1.028 (1.009, 1.027) | 0.003 |
| BMI, kg/m2 | 1.091 (1.000, 1.190) | 0.051 | 1.051 (1.001, 1.104) | 0.046 | 1.011 (0.965, 1.060) | 0.641 |
| Diabetes | 2.033 (0.417, 9.913) | 0.380 | 3.375 (0.407, 27.99) | 0.260 | 0.684 (0.197, 2.377) | 0.550 |
| Sex | 1.173 (0.568, 2.425) | 0.666 | 0.765 (0.506, 1.157) | 0.204 | 1.023 (0.691, 1.514) | 0.911 |
| Smoking | 0.914 (0.440, 1.897) | 0.809 | 1.258 (0.832, 1.904) | 0.277 | 1.246 (0.844, 1.841) | 0.269 |
| Hypertension | 1.717 (0.883, 3.338) | 0.111 | 2.399 (1.606, 3.582) | <0.001 | 1.494 (1.042, 2.142) | 0.029 |
| ECd/Ccr, ng/L filtrate | ||||||
| 0.3–19.4 | Referent | Referent | Referent | |||
| 19.5–44.5 | 7.814 (0.957, 63.81) | 0.055 | 2.689 (1.671, 4.328) | <0.001 | 2.842 (1.780, 4.538) | <0.001 |
| 44.6–800 | 23.75 (3.107, 181.6) | 0.002 | 2.016 (1.299, 3.128) | 0.002 | 4.782 (3.045, 7.512) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Satarug, S.; Vesey, D.A.; Gobe, G.C. Dose–Response Analysis of the Tubular and Glomerular Effects of Chronic Exposure to Environmental Cadmium. Int. J. Environ. Res. Public Health 2022, 19, 10572. https://doi.org/10.3390/ijerph191710572
Satarug S, Vesey DA, Gobe GC. Dose–Response Analysis of the Tubular and Glomerular Effects of Chronic Exposure to Environmental Cadmium. International Journal of Environmental Research and Public Health. 2022; 19(17):10572. https://doi.org/10.3390/ijerph191710572
Chicago/Turabian StyleSatarug, Soisungwan, David A. Vesey, and Glenda C. Gobe. 2022. "Dose–Response Analysis of the Tubular and Glomerular Effects of Chronic Exposure to Environmental Cadmium" International Journal of Environmental Research and Public Health 19, no. 17: 10572. https://doi.org/10.3390/ijerph191710572
APA StyleSatarug, S., Vesey, D. A., & Gobe, G. C. (2022). Dose–Response Analysis of the Tubular and Glomerular Effects of Chronic Exposure to Environmental Cadmium. International Journal of Environmental Research and Public Health, 19(17), 10572. https://doi.org/10.3390/ijerph191710572








