The Determinants of User Acceptance of Mobile Medical Platforms: An Investigation Integrating the TPB, TAM, and Patient-Centered Factors
Abstract
:1. Introduction
2. Theoretical Background and Research Hypotheses
2.1. Theoretical Background
2.2. Research Hypotheses
2.2.1. Behavioral Intention, Attitude, and Perceived Effective Use
2.2.2. Perceived Usefulness, Perceived Ease of Use, and Attitude
2.2.3. Social Influence
2.2.4. Perceived Behavioral Control
2.2.5. Perceived Convenience
2.2.6. Perceived Credibility
2.2.7. Perceived Privacy Risk
3. Research Methodology
3.1. Participants
3.2. Instruments
3.3. Data Analysis
4. Results
4.1. Descriptive Statistics
4.2. Assessment of the Measurement Model
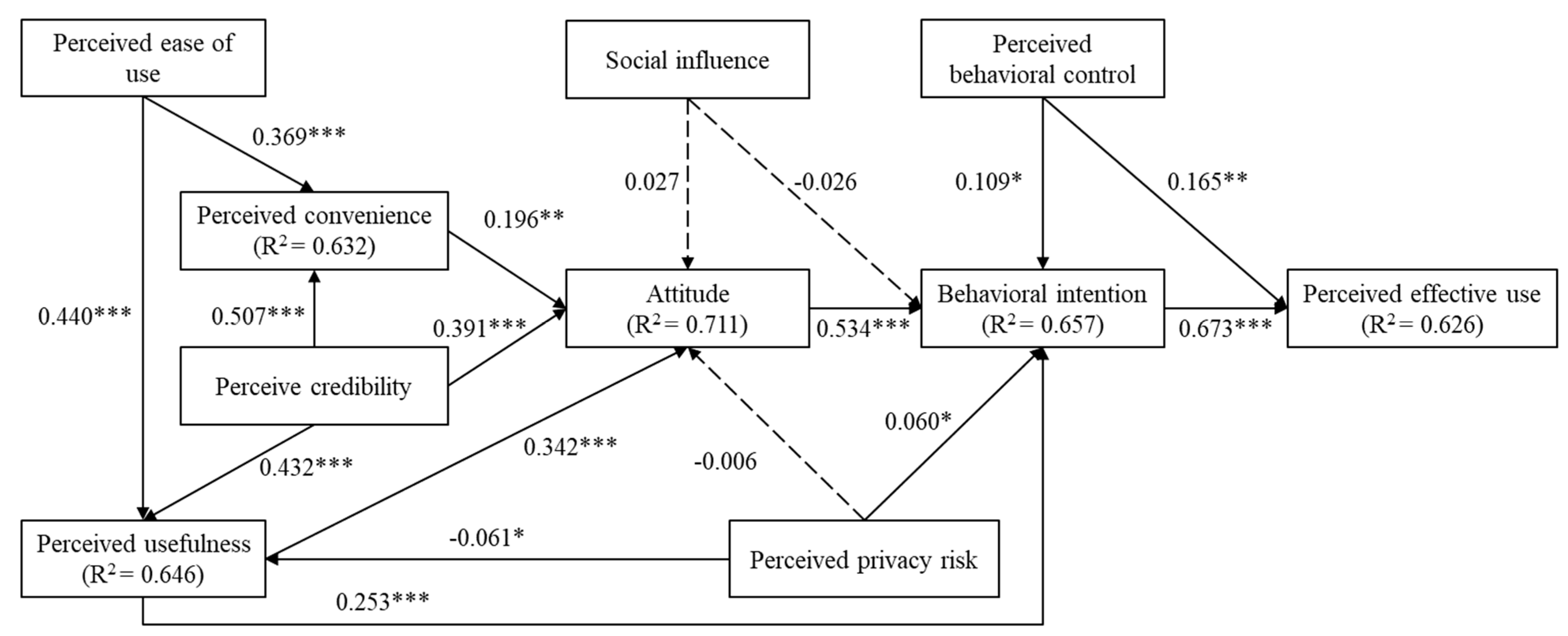
4.3. Structural Model Testing
5. Discussion
5.1. Primary Findings
5.2. Theoretical and Practical Implications
5.3. Limitations and Future Work
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hajat, C.; Stein, E. The global burden of multiple chronic conditions: A narrative review. Prev. Med. Rep. 2018, 12, 284–293. [Google Scholar] [CrossRef]
- Wang, L.M.; Chen, Z.H.; Zhang, M.; Zhao, Z.P.; Huang, Z.J.; Zhang, X.; Li, C.; Guan, Y.Q.; Wang, X.; Wang, Z.H.; et al. Study of the prevalence and disease burden of chronic disease in the elderly in China. Zhonghua Liuxingbingxue Zazhi 2019, 40, 277–283. [Google Scholar]
- Geng, J.; Chen, X.; Bao, H.; Qian, D.; Shao, Y.; Yu, H. Patients’ preferences for health insurance coverage of new technologies for treating chronic diseases in China: A discrete choice experiment. BMJ Open 2020, 10, e038051. [Google Scholar] [CrossRef]
- Deng, Z.; Liu, S.; Hinz, O. The health information seeking and usage behavior intention of Chinese consumers through mobile phones. Inf. Technol. People 2015, 28, 405–423. [Google Scholar] [CrossRef]
- Xing, W.; Hsu, P.Y.; Chang, Y.W.; Shiau, W.L. How does online doctor–patient interaction affect online consultation and offline medical treatment? Ind. Manag. Data Syst. 2020, 120, 196–214. [Google Scholar] [CrossRef]
- Guo, H.; Goldsman, D.; Tsui, K.-L.; Zhou, Y.; Wong, Z.S.-Y. Using simulation and optimisation to characterise durations of emergency department service times with incomplete data. Int. J. Prod. Res. 2016, 54, 6494–6511. [Google Scholar] [CrossRef]
- Zhang, J.; Luximon, Y.; Li, Q. Seeking medical advice in mobile applications: How social cue design and privacy concerns influence trust and behavioral intention in impersonal patient–physician interactions. Comput. Hum. Behav. 2022, 130, 107178. [Google Scholar] [CrossRef]
- Zhang, J.; Li, Q.; Luximon, Y. Building trust in mobile medical consultations: The roles of privacy concerns, personality traits, and social cues. In Proceedings of the 23rd HCI International Conference, Washington, DC, USA, 24–29 July 2021; pp. 293–304. [Google Scholar]
- Rahimi, B.; Nadri, H.; Afshar, H.L.; Timpka, T. A systematic review of the technology acceptance model in health informatics. Appl. Clin. Inform. 2018, 9, 604–634. [Google Scholar] [CrossRef]
- Doyle, M. Healthcare Apps: 2022 Mobile Customer Engagement Benchmarks. 2022. Available online: https://www.apptentive.com/blog/2022/03/29/healthcare-apps-mobile-customer-engagement-benchmarks/#:~:text=Collective%20average%2030%2Dday%20 retention,year%2Dover%2Dyear%20gain (accessed on 19 August 2022).
- Amagai, S.; Pila, S.; Kaat, A.J.; Nowinski, C.J.; Gershon, R.C. Challenges in participant engagement and retention using mobile health apps: Literature review. J. Med. Internet Res. 2022, 24, e35120. [Google Scholar] [CrossRef]
- Bansal, G.; Zahedi, F.; Gefen, D. The impact of personal dispositions on information sensitivity, privacy concern and trust in disclosing health information online. Decis. Support Syst. 2010, 49, 138–150. [Google Scholar] [CrossRef]
- Deng, Z.; Hong, Z.; Ren, C.; Zhang, W.; Xiang, F. What predicts patients’ adoption intention toward mhealth services in China: Empirical study. JMIR mHealth uHealth 2018, 6, e172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Epstein, R.M.; Fiscella, K.; Lesser, C.S.; Stange, K.C. Why the nation needs a policy push on patient-centered health care. Health Aff. 2010, 29, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- Holden, R.J.; Karsh, B.-T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Šumak, B.; Heričko, M.; Pušnik, M. A meta-analysis of e-learning technology acceptance: The role of user types and e-learning technology types. Comput. Hum. Behav. 2011, 27, 2067–2077. [Google Scholar] [CrossRef]
- Tao, D.; Wang, T.; Wang, T.; Zhang, T.; Zhang, X.; Qu, X. A systematic review and meta-analysis of user acceptance of consumer-oriented health information technologies. Comput. Hum. Behav. 2020, 104, 106147. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Tao, D.; Li, W.; Qin, M.; Cheng, M. Understanding students’ acceptance and usage behaviors of online learning in mandatory contexts: A three-wave longitudinal study during the COVID-19 pandemic. Sustainability 2022, 14, 7830. [Google Scholar] [CrossRef]
- Tao, D.; Fu, P.; Wang, Y.; Zhang, T.; Qu, X. Key characteristics in designing massive open online courses (MOOCs) for user acceptance: An application of the extended technology acceptance model. Interact. Learn. Environ. 2019, 30, 882–895. [Google Scholar] [CrossRef]
- Li, Q. Healthcare at your fingertips: The acceptance and adoption of mobile medical treatment services among Chinese users. Int. J. Environ. Res. Public Health 2020, 17, 6895. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Wang, L.; Zhang, Y.; Wang, J. Mobile health service adoption in China. Online Inf. Rev. 2019, 44, 1–23. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Processes 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Wilson, E.V.; Lankton, N.K. Modeling patients’ acceptance of provider-delivered e-health. J. Am. Med. Inform. Assoc. Jamia 2004, 11, 241–248. [Google Scholar] [CrossRef]
- Bao, Y.; Hoque, R.; Wang, S. Investigating the determinants of Chinese adult children’s intention to use online health information for their aged parents. Int. J. Med. Inform. 2017, 102, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.; Mo, X.; Liu, S. Comparison of the middle-aged and older users’ adoption of mobile health services in China. Int. J. Med. Inform. 2014, 83, 210–224. [Google Scholar] [CrossRef]
- Yoon, H.S.; Steege, L.M.B. Development of a quantitative model of the impact of customers’ personality and perceptions on Internet banking use. Comput. Hum. Behav. 2013, 29, 1133–1141. [Google Scholar] [CrossRef]
- Tao, D.; Shao, F.; Wang, H.; Yan, M.; Qu, X. Integrating usability and social cognitive theories with the technology acceptance model to understand young users’ acceptance of a health information portal. Health Inform. J. 2019, 26, 1347–1362. [Google Scholar] [CrossRef]
- Athilingam, P.; Labrador, M.A.; Remo, E.F.J.; Mack, L.; San Juan, A.B.; Elliott, A.F. Features and usability assessment of a patient-centered mobile application (HeartMapp) for self-management of heart failure. Appl. Nurs. Res. 2016, 32, 156–163. [Google Scholar] [CrossRef]
- Tuzovic, S.; Kuppelwieser, V. Developing a framework of service convenience in health care: An exploratory study for a primary care provider. Heal. Mark. Q. 2016, 33, 127–148. [Google Scholar] [CrossRef]
- Yun, E.K.; Park, H.-A. Consumers’ disease information-seeking behaviour on the internet in Korea. J. Clin. Nurs. 2010, 19, 2860–2868. [Google Scholar] [CrossRef]
- Li, H.; Wu, J.; Gao, Y.; Shi, Y. Examining individuals’ adoption of healthcare wearable devices: An empirical study from privacy calculus perspective. Int. J. Med Inform. 2016, 88, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tao, D.; Yu, N.; Qu, X. Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF. Int. J. Med Inform. 2020, 139, 104156. [Google Scholar] [CrossRef] [PubMed]
- Koenig-Lewis, N.; Marquet, M.; Palmer, A.; Zhao, A.L. Enjoyment and social influence: Predicting mobile payment adoption. Serv. Ind. J. 2015, 35, 537–554. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Li, J.; Ma, Q.; Chan, A.H.; Man, S. Health monitoring through wearable technologies for older adults: Smart wearables acceptance model. Appl. Ergon. 2019, 75, 162–169. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Rana, N.P.; Jeyaraj, A.; Clement, M.; Williams, M.D. Re-examining the unified theory of acceptance and use of technology (UTAUT): Towards a revised theoretical model. Inf. Syst. Front. 2019, 21, 719–734. [Google Scholar] [CrossRef]
- Chen, X.; Tao, D.; Zhou, Z. Factors affecting reposting behaviour using a mobile phone-based user-generated-content online community application among Chinese young adults. Behav. Inf. Technol. 2019, 38, 120–131. [Google Scholar] [CrossRef]
- Tao, D.; Yuan, J.; Shao, F.; Li, D.; Zhou, Q.; Qu, X. Factors affecting consumer acceptance of an online health information portal among young internet users. CIN Comput. Inform. Nurs. 2018, 36, 530–539. [Google Scholar] [CrossRef]
- Cho, J. The impact of post-adoption beliefs on the continued use of health apps. Int. J. Med. Inform. 2016, 87, 75–83. [Google Scholar] [CrossRef]
- Cimperman, M.; Brenčič, M.M.; Trkman, P. Analyzing older users’ home telehealth services acceptance behavior—Applying an extended UTAUT model. Int. J. Med. Inform. 2016, 90, 22–31. [Google Scholar] [CrossRef]
- Liu, K.; Tao, D. The roles of trust, personalization, loss of privacy, and anthropomorphism in public acceptance of smart healthcare services. Comput. Hum. Behav. 2022, 127, 107026. [Google Scholar] [CrossRef]
- Or, C.K.L.; Karsh, B.-T.; Severtson, D.J.; Burke, L.J.; Brown, R.L.; Brennan, P.F. Factors affecting home care patients’ acceptance of a web-based interactive self-management technology. J. Am. Med. Inform. Assoc. 2011, 18, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Tao, D.; Qu, X.; Zhang, X.; Lin, R.; Zhang, W. The roles of initial trust and perceived risk in public’s acceptance of automated vehicles. Transp. Res. Part C Emerg. Technol. 2019, 98, 207–220. [Google Scholar] [CrossRef]
- Marangunić, N.; Granić, A. Technology acceptance model: A literature review from 1986 to 2013. Univers. Access Inf. Soc. 2015, 14, 81–95. [Google Scholar] [CrossRef]
- Yousafzai, S.Y.; Foxall, G.R.; Pallister, J.G. Technology acceptance: A meta-analysis of the TAM: Part 2. J. Model. Manag. 2007, 2, 281. [Google Scholar] [CrossRef]
- Ifinedo, P. Applying uses and gratifications theory and social influence processes to understand students’ pervasive adoption of social networking sites: Perspectives from the Americas. Int. J. Inf. Manag. 2016, 36, 192–206. [Google Scholar] [CrossRef]
- Lunney, A.; Cunningham, N.R.; Eastin, M.S. Wearable fitness technology: A structural investigation into acceptance and perceived fitness outcomes. Comput. Hum. Behav. 2016, 65, 114–120. [Google Scholar] [CrossRef]
- Yan, M.; Or, C. A 12-week pilot study of acceptance of a computer-based chronic disease self-monitoring system among patients with type 2 diabetes mellitus and/or hypertension. Health Inform. J. 2019, 25, 828–843. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.; Xu, X. Consumer acceptance and use of information technology: Extending the unified theory of acceptance and use of technology. MIS Q. 2012, 36, 157–178. [Google Scholar] [CrossRef]
- Ozturk, A.B.; Bilgihan, A.; Nusair, K.; Okumus, F. What keeps the mobile hotel booking users loyal? Investigating the roles of self-efficacy, compatibility, perceived ease of use, and perceived convenience. Int. J. Inf. Manag. 2016, 36, 1350–1359. [Google Scholar] [CrossRef]
- Okazaki, S.; Mendez, F. Exploring convenience in mobile commerce: Moderating effects of gender. Comput. Hum. Behav. 2013, 29, 1234–1242. [Google Scholar] [CrossRef] [Green Version]
- Lazard, A.J.; Watkins, I.; Mackert, M.S.; Xie, B.; Stephens, K.; Shalev, H. Design simplicity influences patient portal use: The role of aesthetic evaluations for technology acceptance. J. Am. Med. Inform. Assoc. 2015, 23, e157–e161. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.E.; Han, S.S.; Yoo, K.H.; Yun, E.K. The impact of user’s perceived ability on online health information acceptance. Telemed. e-Health 2012, 18, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Tian, Y.; Tu, M. Exploring factors influencing Chinese user’s perceived credibility of health and safety information on weibo. Comput. Hum. Behav. 2015, 45, 21–31. [Google Scholar] [CrossRef]
- Marakhimov, A.; Joo, J. Consumer adaptation and infusion of wearable devices for healthcare. Comput. Hum. Behav. 2017, 76, 135–148. [Google Scholar] [CrossRef]
- Gao, Y.; Li, H.; Luo, Y. An empirical study of wearable technology acceptance in healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar] [CrossRef]
- Caron, X.; Bosua, R.; Maynard, S.B.; Ahmad, A. The internet of things (IoT) and its impact on individual privacy: An Australian perspective. Comput. Law Secur. Rev. 2016, 32, 4–15. [Google Scholar] [CrossRef]
- Hsu, C.-L.; Lin, J.C.-C. An empirical examination of consumer adoption of Internet of things services: Network externalities and concern for information privacy perspectives. Comput. Hum. Behav. 2016, 62, 516–527. [Google Scholar] [CrossRef]
- Li, Y. The impact of disposition to privacy, website reputation and website familiarity on information privacy concerns. Decis. Support Syst. 2014, 57, 343–354. [Google Scholar] [CrossRef]
- Taylor, S.; Todd, P.A. Understanding information technology usage: A test of competing models. Inf. Syst. Res. 1995, 6, 144–176. [Google Scholar] [CrossRef]
- Chang, C.-C.; Yan, C.-F.; Tseng, J.-S. Perceived convenience in an extended technology acceptance model: Mobile technology and English learning for college students. Australas. J. Educ. Technol. 2012, 28. [Google Scholar] [CrossRef] [Green Version]
- West, M.D. Validating a scale for the measurement of credibility: A covariance structure modeling approach. J. Q. 1993, 71, 159–168. [Google Scholar] [CrossRef]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Ringle, C.M.; Wende, S.; Becker, J.-M. SmartPLS 3. Boenningstedt: SmartPLS. Available online: https://www.smartpls.com (accessed on 24 August 2022).
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); SAGE: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Mena, J.A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2012, 40, 414–433. [Google Scholar] [CrossRef]
- Hair, J.F. Multivariate Data Analysis, 7th ed.; Pearson Education Limited: Harlow, UK, 2014. [Google Scholar]
- Zaiţ, A.; Bertea, P.E. Methods for testing discriminant validity. Manag. Mark. J. 2011, 9, 217–224. [Google Scholar]
- Yang, M.; Jiang, J.; Kiang, M.; Yuan, F. Re-examining the impact of multidimensional trust on patients’ online medical consultation service continuance decision. Inf. Syst. Front. 2021, 24, 983–1007. [Google Scholar] [CrossRef]
- Chen, Y.; Yang, L.; Zhang, M.; Yang, J. Central or peripheral? Cognition elaboration cues’ effect on users’ continuance intention of mobile health applications in the developing markets. Int. J. Med. Inform. 2018, 116, 33–45. [Google Scholar] [CrossRef]
- Wang, E.S.-T.; Lin, R.-L. Perceived quality factors of location-based apps on trust, perceived privacy risk, and continuous usage intention. Behav. Inf. Technol. 2017, 36, 2–10. [Google Scholar] [CrossRef]
- Laufer, R.S.; Wolfe, M. Privacy as a concept and a social issue: A multidimensional developmental theory. J. Soc. Issues 1977, 33, 22–42. [Google Scholar] [CrossRef]
- Yang, S.; Lu, Y.; Gupta, S.; Cao, Y.; Zhang, R. Mobile payment services adoption across time: An empirical study of the effects of behavioral beliefs, social influences, and personal traits. Comput. Hum. Behav. 2012, 28, 129–142. [Google Scholar] [CrossRef]
- Zhou, T.; Li, H. Understanding mobile SNS continuance usage in China from the perspectives of social influence and privacy concern. Comput. Hum. Behav. 2014, 37, 283–289. [Google Scholar] [CrossRef]
- Shiferaw, K.B.; Mehari, E.A. Modeling predictors of acceptance and use of electronic medical record system in a resource limited setting: Using modified UTAUT model. Inform. Med. Unlocked 2019, 17, 100182. [Google Scholar] [CrossRef]
- Dehghani, M.; Kim, K.J.; Dangelico, R.M. Will smartwatches last? factors contributing to intention to keep using smart wearable technology. Telemat. Inform. 2018, 35, 480–490. [Google Scholar] [CrossRef]

| Items | Type | Number of Participants | Percentage (%) |
|---|---|---|---|
| Gender | Male | 150 | 38.6% |
| Female | 239 | 61.4% | |
| Age | <18 | 27 | 6.9% |
| 18–30 | 224 | 57.6% | |
| 31–40 | 108 | 27.8% | |
| 41–50 | 24 | 6.2% | |
| 51 or above | 6 | 1.5% | |
| Education | High school or lower | 8 | 2.1% |
| College | 90 | 23.1% | |
| Bachelor’s degree | 270 | 69.4% | |
| Master’s degree or above | 21 | 5.4% | |
| Usage of smartphone (hours/day) | <1 | 3 | 0.8% |
| 1–4 | 135 | 34.7% | |
| 5–8 | 192 | 49.4% | |
| >8 | 59 | 15.2% | |
| Usage of mobile medical platforms | More than once/day | 14 | 3.6% |
| Once/day | 54 | 13.9% | |
| Once/week | 151 | 38.8% | |
| Once/month | 126 | 32.4% | |
| Once/6 months | 44 | 11.3% |
| Constructs | Items |
|---|---|
| Perceived ease of use (PEOU) [19] | PEOU1 Learning to use MMPs is easy for me. |
| PEOU2 I find it easy to get MMPs to do what I want them to do. | |
| PEOU3 It is easy for me to become skillful at using MMPs. | |
| PEOU4 I find MMPs easy to use. | |
| Perceived usefulness (PU) [19] | PU1 Using MMPs improves my ability of health management. |
| PU2 Using MMPs helps me save time in managing my health. | |
| PU3 Using MMPs enhances the effectiveness of my health management. | |
| PU4 I find MMPs to be useful in my health management. | |
| Attitude (ATT) [19] | ATT1 Using MMPs is a good idea. |
| ATT2 Using MMPs is a wise idea. | |
| ATT3 I like the idea of using MMPs. | |
| Social influence (SI) [25] | SI1 My family members influence my decision to use MMPs. |
| SI2 My friends influence my decision to use MMPs. | |
| Perceived behavioral control (PBC) [62] | PBC1 I have the ability to use MMPs to manage my health. |
| PBC2 I have the resources (including training opportunity) that allow me to use MMPs for my health management. | |
| Perceived convenience (PCV) [63] | PCV1 I can access health care services at any time via MMPs. |
| PCV2 I can access health care services at any place via MMPs. | |
| PCV3 MMPs are a convenient way for me to access health care services. | |
| Perceived privacy risks (PPR) [25] | PPR1 I am concerned that MMPs collect too much personal information from me. |
| PPR2 I am concerned that MMPs will share my personal information with other entities without my authorization. | |
| Perceived credibility (PCB) [64] | PCB1 The information provided by MMPs is up-to-date. |
| PCB2 The information provided by MMPs is accurate. | |
| PCB3 The information provided by MMPs is trustworthy. | |
| PCB4 The information provided by MMPs is authoritative. | |
| Behavioral intention (BI) [36] | BI1 I intent to use this MMP when I need it in the future. |
| BI2 I predict that I will use the mobile medical service in the future. | |
| BI3 I plan to use MMPs in the future. | |
| Perceived effective use (PEU) [44] | To what extent do you use MMPs as much as you should use it? |
| Constructs | Items | Mean | SD | 95%CI |
|---|---|---|---|---|
| Attitude (ATT) | ATT1 | 5.46 | 0.88 | [5.37, 5.55] |
| ATT2 | 5.40 | 0.92 | [5.31, 5.49] | |
| ATT3 | 5.38 | 0.96 | [5.28, 5.47] | |
| Behavioral intention (BI) | BI1 | 5.53 | 0.91 | [5.44, 5.63] |
| BI2 | 5.57 | 0.93 | [5.48, 5.67] | |
| BI3 | 5.55 | 0.94 | [5.46, 5.65] | |
| Perceived credibility (PCB) | PCB1 | 5.20 | 0.92 | [5.10, 5.29] |
| PCB2 | 5.04 | 0.91 | [4.95, 5.13] | |
| PCB3 | 5.16 | 0.93 | [5.07, 5.26] | |
| PCB4 | 4.95 | 0.98 | [4.85, 5.04] | |
| Perceived convenience (PCV) | PCV1 | 5.35 | 0.89 | [5.26, 5.44] |
| PCV2 | 5.32 | 0.99 | [5.22, 5.42] | |
| PCV3 | 5.52 | 0.96 | [5.42, 5.61] | |
| Perceived ease of use (PEOU) | PEOU1 | 5.53 | 0.90 | [5.44, 5.62] |
| PEOU2 | 5.39 | 0.96 | [5.29, 5.48] | |
| PEOU3 | 5.52 | 0.96 | [5.43, 5.62] | |
| PEOU4 | 5.55 | 0.97 | [5.45, 5.64] | |
| Perceived privacy risks (PPR) | PPR1 | 4.33 | 1.42 | [4.19, 4.47] |
| PPR2 | 4.46 | 1.61 | [4.30, 4.62] | |
| Perceived behavioral control (PBC) | PBC1 | 5.35 | 0.95 | [5.26, 5.45] |
| PBC2 | 4.92 | 1.18 | [4.80, 5.04] | |
| Perceived usefulness (PU) | PU1 | 5.35 | 0.97 | [5.25, 5.44] |
| PU2 | 5.60 | 1.00 | [5.50, 5.70] | |
| PU3 | 5.38 | 0.98 | [5.28, 5.48] | |
| PU4 | 5.47 | 0.93 | [5.38, 5.57] | |
| Social influence (SI) | SI1 | 4.56 | 1.27 | [4.43, 4.68] |
| SI2 | 4.60 | 1.23 | [4.48, 4.72] | |
| Perceived effective use (PEU) | PEU | 5.45 | 0.83 | [5.36, 5.53] |
| Constructs | Items | Item Loadings | t-Values | AVEs | Composite Reliability | Cronbach’s Alpha |
|---|---|---|---|---|---|---|
| Attitude (ATT) | ATT1 | 0.892 | 65.155 | 0.795 | 0.921 | 0.871 |
| ATT2 | 0.896 | 69.758 | ||||
| ATT3 | 0.887 | 62.023 | ||||
| Behavioral intention (BI) | BI1 | 0.919 | 85.643 | 0.840 | 0.940 | 0.905 |
| BI2 | 0.902 | 67.434 | ||||
| BI3 | 0.929 | 94.892 | ||||
| Perceived credibility (PCB) | PCB1 | 0.817 | 46.469 | 0.735 | 0.917 | 0.879 |
| PCB2 | 0.871 | 55.420 | ||||
| PCB3 | 0.889 | 66.637 | ||||
| PCB4 | 0.849 | 47.769 | ||||
| Perceived convenience (PCV) | PCV1 | 0.908 | 87.463 | 0.767 | 0.908 | 0.848 |
| PCV2 | 0.863 | 52.135 | ||||
| PCV3 | 0.856 | 47.187 | ||||
| Perceived ease of use (PEOU) | PEOU1 | 0.887 | 61.247 | 0.749 | 0.923 | 0.888 |
| PEOU2 | 0.845 | 49.959 | ||||
| PEOU3 | 0.867 | 54.512 | ||||
| PEOU4 | 0.864 | 47.859 | ||||
| Perceived privacy risks (PPR) | PPR1 | 0.949 | 36.093 | 0.925 | 0.961 | 0.920 |
| PPR2 | 0.974 | 51.399 | ||||
| Perceived behavioral control (PBC) | PBC1 | 0.914 | 86.912 | 0.747 | 0.855 | 0.671 |
| PBC2 | 0.812 | 20.231 | ||||
| Perceived usefulness (PU) | PU1 | 0.874 | 57.958 | 0.757 | 0.926 | 0.893 |
| PU2 | 0.852 | 43.988 | ||||
| PU3 | 0.866 | 56.348 | ||||
| PU4 | 0.889 | 66.871 | ||||
| Social influence (SI) | SI1 | 0.929 | 74.034 | 0.853 | 0.920 | 0.827 |
| SI2 | 0.918 | 67.289 | ||||
| Perceived effective use (PEU) | PEU | 1.000 | - | 1.000 | 1.000 |
| ATT | BI | PEOU | PCV | PVB | PEU | PPR | PBC | PU | SI | |
|---|---|---|---|---|---|---|---|---|---|---|
| ATT | 0.892 | |||||||||
| BI | 0.788 | 0.917 | ||||||||
| PEOU | 0.667 | 0.683 | 0.866 | |||||||
| PCV | 0.749 | 0.692 | 0.695 | 0.876 | ||||||
| PCB | 0.784 | 0.695 | 0.644 | 0.744 | 0.857 | |||||
| PEU | 0.743 | 0.783 | 0.636 | 0.674 | 0.655 | 1 | ||||
| PPR | −0.192 | −0.118 | −0.139 | −0.127 | −0.228 | −0.086 | 0.961 | |||
| PBC | 0.728 | 0.662 | 0.63 | 0.703 | 0.751 | 0.611 | −0.185 | 0.864 | ||
| PU | 0.773 | 0.723 | 0.727 | 0.781 | 0.729 | 0.692 | −0.221 | 0.736 | 0.870 | |
| SI | 0.354 | 0.298 | 0.313 | 0.309 | 0.377 | 0.247 | −0.021 | 0.395 | 0.369 | 0.923 |
| ATT | BI | PCB | PCV | PEOU | PEU | PPR | PBC | PU | SI | |
|---|---|---|---|---|---|---|---|---|---|---|
| ATT1 | 0.892 | 0.720 | 0.689 | 0.674 | 0.599 | 0.695 | −0.130 | 0.647 | 0.665 | 0.312 |
| ATT2 | 0.896 | 0.724 | 0.693 | 0.639 | 0.587 | 0.651 | −0.183 | 0.654 | 0.705 | 0.314 |
| ATT3 | 0.887 | 0.664 | 0.716 | 0.692 | 0.598 | 0.641 | −0.201 | 0.645 | 0.698 | 0.322 |
| BI1 | 0.727 | 0.919 | 0.656 | 0.647 | 0.652 | 0.722 | −0.106 | 0.629 | 0.680 | 0.311 |
| BI2 | 0.709 | 0.902 | 0.594 | 0.622 | 0.583 | 0.694 | −0.084 | 0.543 | 0.630 | 0.246 |
| BI3 | 0.732 | 0.929 | 0.658 | 0.633 | 0.642 | 0.735 | −0.135 | 0.646 | 0.677 | 0.263 |
| PCB1 | 0.685 | 0.609 | 0.817 | 0.716 | 0.580 | 0.598 | −0.125 | 0.689 | 0.681 | 0.351 |
| PCB2 | 0.668 | 0.600 | 0.871 | 0.620 | 0.575 | 0.539 | −0.213 | 0.637 | 0.608 | 0.315 |
| PCB3 | 0.707 | 0.647 | 0.889 | 0.648 | 0.588 | 0.599 | −0.255 | 0.654 | 0.650 | 0.303 |
| PCB4 | 0.619 | 0.512 | 0.849 | 0.548 | 0.447 | 0.496 | −0.192 | 0.581 | 0.544 | 0.322 |
| PCV1 | 0.696 | 0.654 | 0.709 | 0.908 | 0.653 | 0.632 | −0.112 | 0.670 | 0.719 | 0.286 |
| PCV2 | 0.602 | 0.559 | 0.618 | 0.863 | 0.565 | 0.519 | −0.048 | 0.580 | 0.619 | 0.281 |
| PCV3 | 0.666 | 0.600 | 0.624 | 0.856 | 0.604 | 0.615 | −0.171 | 0.592 | 0.710 | 0.245 |
| PEOU1 | 0.592 | 0.615 | 0.555 | 0.596 | 0.887 | 0.569 | −0.122 | 0.572 | 0.627 | 0.263 |
| PEOU2 | 0.557 | 0.567 | 0.562 | 0.595 | 0.845 | 0.550 | −0.113 | 0.544 | 0.643 | 0.283 |
| PEOU3 | 0.562 | 0.574 | 0.534 | 0.615 | 0.867 | 0.544 | −0.104 | 0.519 | 0.609 | 0.260 |
| PEOU4 | 0.598 | 0.608 | 0.577 | 0.600 | 0.864 | 0.537 | −0.142 | 0.545 | 0.638 | 0.278 |
| PEU | 0.743 | 0.783 | 0.655 | 0.674 | 0.636 | 1.000 | −0.086 | 0.611 | 0.692 | 0.247 |
| PPR1 | −0.155 | −0.097 | −0.192 | −0.089 | −0.103 | −0.054 | 0.949 | −0.139 | −0.176 | 0.040 |
| PPR2 | −0.207 | −0.126 | −0.24 | −0.146 | −0.156 | −0.104 | 0.974 | −0.207 | −0.24 | −0.063 |
| PBC1 | 0.713 | 0.662 | 0.711 | 0.682 | 0.625 | 0.606 | −0.182 | 0.914 | 0.704 | 0.279 |
| PBC2 | 0.521 | 0.456 | 0.574 | 0.513 | 0.440 | 0.427 | −0.133 | 0.812 | 0.552 | 0.439 |
| PU1 | 0.686 | 0.623 | 0.668 | 0.668 | 0.629 | 0.611 | −0.218 | 0.672 | 0.874 | 0.355 |
| PU2 | 0.629 | 0.598 | 0.588 | 0.699 | 0.650 | 0.549 | −0.187 | 0.612 | 0.852 | 0.321 |
| PU3 | 0.666 | 0.626 | 0.627 | 0.658 | 0.603 | 0.580 | −0.183 | 0.609 | 0.866 | 0.312 |
| PU4 | 0.708 | 0.669 | 0.654 | 0.696 | 0.649 | 0.664 | −0.183 | 0.666 | 0.889 | 0.296 |
| SI1 | 0.337 | 0.285 | 0.368 | 0.295 | 0.290 | 0.227 | −0.036 | 0.369 | 0.326 | 0.929 |
| SI2 | 0.317 | 0.265 | 0.328 | 0.275 | 0.288 | 0.229 | −0.001 | 0.361 | 0.356 | 0.918 |
| Hypotheses | Path Coefficients | t-Value | p Value | Support? (Yes/No) | |
|---|---|---|---|---|---|
| H1 | BI → PEU | 0.673 | 15.278 | <0.001 | Yes |
| H2 | ATT → BI | 0.534 | 10.564 | <0.001 | Yes |
| H3 | PU → ATT | 0.324 | 5.558 | <0.001 | Yes |
| H4 | PU → BI | 0.253 | 5.093 | <0.001 | Yes |
| H5 | PEOU → PU | 0.440 | 8.452 | <0.001 | Yes |
| H6 | SI → ATT | 0.027 | 0.877 | 0.381 | No |
| H7 | SI → BI | −0.026 | 0.743 | 0.458 | No |
| H8 | PBC → BI | 0.109 | 2.019 | 0.043 | Yes |
| H9 | PBC → PEU | 0.165 | 3.109 | 0.002 | Yes |
| H10 | PEOU → PCV | 0.369 | 7.443 | <0.001 | Yes |
| H11 | PCV → ATT | 0.196 | 3.294 | 0.001 | Yes |
| H12 | PCB → PCV | 0.507 | 10.444 | <0.001 | Yes |
| H13 | PCB → PU | 0.432 | 8.672 | <0.001 | Yes |
| H14 | PCB → ATT | 0.391 | 7.675 | <0.001 | Yes |
| H15 | PPR → PU | −0.061 | 1.981 | 0.048 | Yes |
| H16 | PPR → ATT | −0.006 | 0.200 | 0.842 | No |
| H17 | PPR → BI | 0.060 | 2.078 | 0.038 | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Zhang, J.; Luximon, Y.; Qin, M.; Geng, P.; Tao, D. The Determinants of User Acceptance of Mobile Medical Platforms: An Investigation Integrating the TPB, TAM, and Patient-Centered Factors. Int. J. Environ. Res. Public Health 2022, 19, 10758. https://doi.org/10.3390/ijerph191710758
Wang H, Zhang J, Luximon Y, Qin M, Geng P, Tao D. The Determinants of User Acceptance of Mobile Medical Platforms: An Investigation Integrating the TPB, TAM, and Patient-Centered Factors. International Journal of Environmental Research and Public Health. 2022; 19(17):10758. https://doi.org/10.3390/ijerph191710758
Chicago/Turabian StyleWang, Hailiang, Jiaxin Zhang, Yan Luximon, Mingfu Qin, Ping Geng, and Da Tao. 2022. "The Determinants of User Acceptance of Mobile Medical Platforms: An Investigation Integrating the TPB, TAM, and Patient-Centered Factors" International Journal of Environmental Research and Public Health 19, no. 17: 10758. https://doi.org/10.3390/ijerph191710758





