Pilot Feasibility Assessment of a Tailored Physical Activity Prescription in Overweight and Obese People in a Public Hospital
Abstract
:1. Introduction
2. Materials and Methods
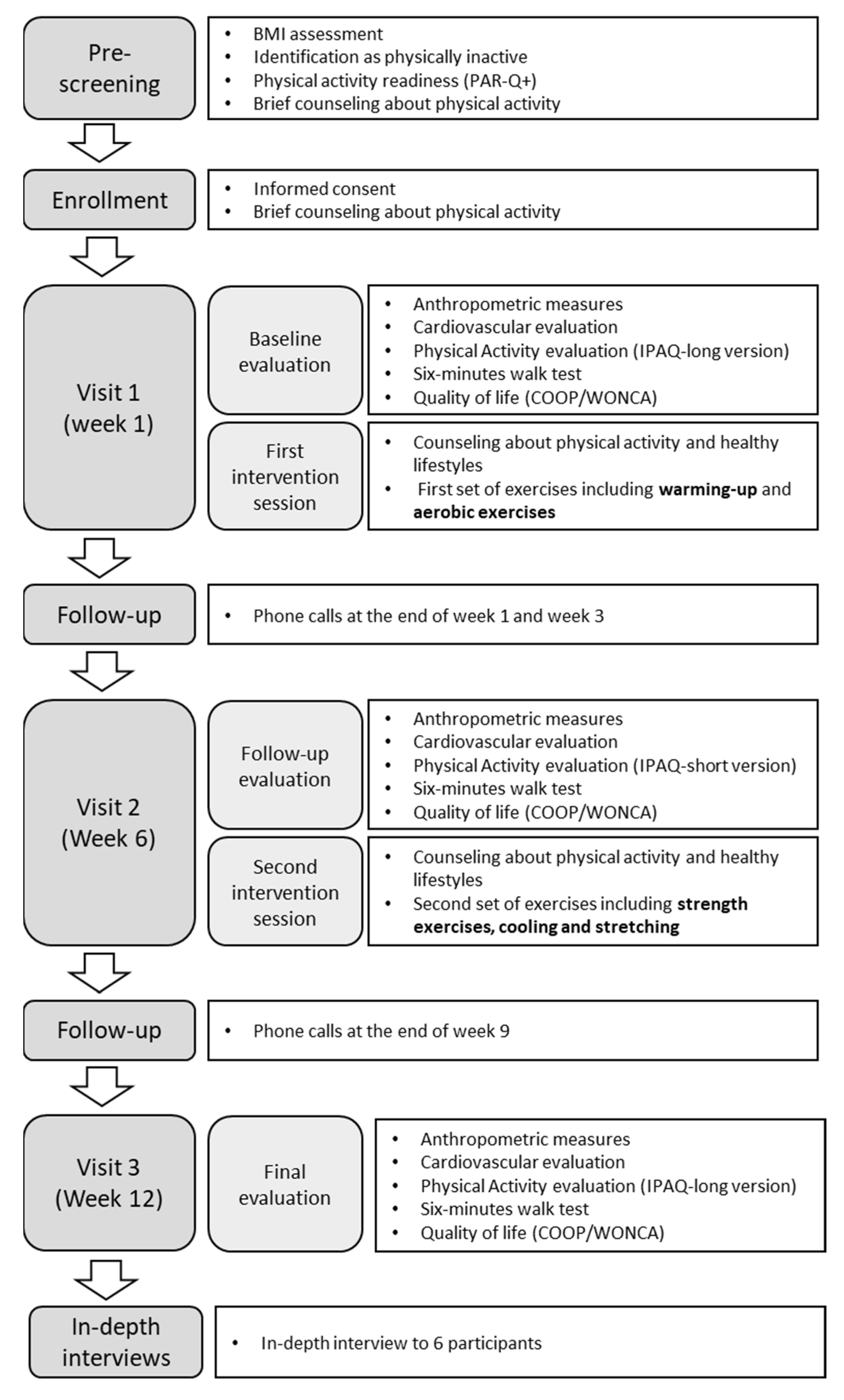
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Procedures
2.5. Assessment of Intervention Outcomes
2.6. Assessment of Feasibility Outcomes
2.7. Data Analysis
3. Results
3.1. Intervention Outcomes
3.2. Feasibility of the Intervention
3.2.1. Intervention Delivery Perceptions
“I am grateful for all the support they [Study staff]have given me and what they have taught me about the guidelines, how to do everything with love. I told the nutritionist that I had to do it by myself and he showed me the guidelines with the booklet, how you are going to do it. And I did it just as he told me.”—P16
“For me it was perfect the amount and the time that elapsed between them. It was neither too heavy nor to the point of forgetfulness.”—P46
“The manual was very didactic, and there was a personal who explained to me what I had to do and why I had to do it, and I also felt very well attended, very well attended by the professionals.”—P46
3.2.2. Barriers and Facilitators for PA
“I was motivated by the fact that I want to lose weight, because I have vitiligo, and I have to take my food with me, that is, not to gain weight, but now I have gained weight, I am weighing 91.9, I was weighing 89.5 and I have gained weight (...) I have made a total imbalance of eating at odd hours, right? There... here… I was not at my eating time, that’s why I decided to participate”—P44
“Yes, because the first few days I was shocked because I have always had an almost sedentary life and even more so with this disease I have. So, I could not have done nothing, I could have been in bed for almost more than a year... to start doing the exercises, that is, I realized that my body was not as my mind thought. I thought that I could still jump, that I could still do, for example, jump rope on both feet... and I realized that I could not because I am too overweight... I could not do it because I have too much weight.”—P16
“For example now I have knowledge of stretching exercises that I can do at home, the ailments have gone down as I tell you...I have a different rhythm, when I started walking I used to get very agitated, right? now I don’t get agitated the same way, my face doesn’t get hot anymore. So, I wanted to improve my physical condition, my mood and I have achieved it, right? (…) Well, I am enrolled in the gym, now I am working on project that needs some fieldwork, so I can keep doing my walks.”—P46
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Booth, F.W.; Roberts, C.K.; Thyfault, J.P.; Ruegsegger, G.N.; Toedebusch, R.G. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol. Rev. 2017, 97, 1351–1402. [Google Scholar] [CrossRef] [PubMed]
- OMS. Recomendaciones Mundiales Sobre Actividad Física Para la Salud; Organización Mundial de la Salud: Geneva, Switzerland, 2010; 58p.
- WHO. Physical Activity. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 24 July 2018).
- National Institute for Health and Care Excellence. Physical Activity: Exercise Referral Schemes; National Institute for Health and Care Excellence: London, UK, 2014. [Google Scholar]
- Haskell, W.L.; Lee, I.-M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical Activity and Public Health. Med. Sci. Sport. Exerc. 2007, 39, 1423–1434. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Katzmarzyk, P.T.; Rhodes, R.E.; Shephard, R.J.; Warburton, D.E.; Katzmarzyk, P.T.; Rhodes, R.E.; Shephard, R.J. Evidence-informed physical activity guidelines for Canadian adults. Appl. Physiol. Nutr. Metab. 2007, 32, 16–68. [Google Scholar] [CrossRef]
- Guthold, R.; Ono, T.; Strong, K.L.; Chatterji, S.; Morabia, A. Worldwide Variability in Physical Inactivity A 51-Country Survey. Am. J. Prev. Med. 2008, 34, 486–494. [Google Scholar] [CrossRef]
- Popkin, B.M.; Gordon-Larsen, P. The nutrition transition: Worldwide obesity dynamics and their determinants. Int. J. Obes. Relat. Metab. Disord. 2004, 28 (Suppl. 3), S2–S9. [Google Scholar] [CrossRef]
- Herazo-Beltrán, Y.; Pinillos, Y.; Vidarte, J.; Crissien, E.; Suarez, D.; García, R. Predictors of perceived barriers to physical activity in the general adult population: A cross-sectional study. Braz. J. Phys. Ther. 2017, 21, 44–50. [Google Scholar] [CrossRef]
- Sørensen, J.B.; Skovgaard, T.; Puggaard, L. Exercise on prescription in general practice: A systematic review. Scand. J. Prim. Health Care 2009, 24, 69–74. [Google Scholar] [CrossRef]
- Puig Ribera, A.; McKenna, J.; Riddoch, C. Attitudes and practices of physicians and nurses regarding physical activity promotion in the Catalan primary health-care system. Eur. J. Public Health 2005, 15, 569–575. [Google Scholar] [CrossRef]
- O’Regan, A.; Pollock, M.; D’Sa, S.; Niranjan, V. ABC of prescribing exercise as medicine: A narrative review of the experiences of general practitioners and patients. BMJ Open Sport Exerc. Med. 2021, 7, 1050. [Google Scholar] [CrossRef]
- Lawton, B.A.; Rose, S.B.; Fellow, R.; Raina Elley, C.; Lecturer, S.; Dowell, A.C.; Fenton, A.; Moyes, S.A. Exercise on prescription for women aged 40–74 recruited through primary care: Two year randomised controlled trial. BMJ 2017, 17, 576. [Google Scholar] [CrossRef] [Green Version]
- Holliday, A.; Burgin, A.; Vargas Fernandez, E.; Fenton, S.A.M.; Thielecke, F.; Blannin, A.K. Points-based physical activity: A novel approach to facilitate changes in body composition in inactive women with overweight and obesity. BMC Public Health 2018, 18, 261. [Google Scholar] [CrossRef] [PubMed]
- Olsson, S.J.G.; Börjesson, M.; Ekblom-Bak, E.; Hemmingsson, E.; Hellénius, M.-L.; Kallings, L. V Effects of the Swedish physical activity on prescription model on health-related quality of life in overweight older adults: A randomised controlled trial. BMC Public Health 2015, 15, 687. [Google Scholar] [CrossRef] [PubMed]
- Poggio, R.; Serón, P.; Calandrelli, M.; Ponzo, J.; Mores, N.; Matta, M.G.; Gutierrez, L.; Chung-Shiuan, C.; Lanas, F.; He, J.; et al. Prevalence, Patterns, and Correlates of Physical Activity Among the Adult Population in Latin America: Cross-Sectional Results from the CESCAS I Study. Glob. Heart 2016, 11, 81–88.e1. [Google Scholar] [CrossRef] [PubMed]
- Mamani, C.T.; Dongo, D.A.; Oriundo, P.E. Prevalencia y factores asociados a la baja actividad física de la población peruana. Nutr. Clín. Diet. Hosp. 2017, 37, 108–115. [Google Scholar] [CrossRef]
- Nolasco, M.F.T. Encuentro Clínico de Los Médicos Con Pacientes Con Sobrepeso y Obesidad en Consulta Externa de un Hospital Público de Lima; Universidad Peruana Cayetano Heredia: Lima, Peru, 2019. [Google Scholar]
- Creswell, J.W.; Plano Clarck, V.L.; Gutmann, M.; Hanson, W. Advance mixed methods research designs. In Handbook of Mixed Methods in Social & Behavioral Research; Tashakkori, A., Teddlie, C., Eds.; Sage: Thousand Oaks, CA, USA, 2003; pp. 209–240. [Google Scholar]
- Hospital Cayetano Heredia. 2018. Available online: http://www.hospitalcayetano.gob.pe/PortalWeb/historia (accessed on 20 September 2020).
- Rose, S.B.; Elley, C.R.; Lawton, B.A.; Dowell, A.C. A single question reliably identifies physically inactive women in primary care. N. Z. Med. J. 2008, 121, U2897. [Google Scholar] [PubMed]
- Bredin, S.S.D.; Gledhill, N.; Jamnik, V.K.; Warburton, D.E.R. Physical Activity Series PAR-Q+ and ePARmed-X+ New Risk Stratification and Physical Activity Clearance Strategy for Physicians and Patients Alike. Can. Fam. Physician 2013, 59, 273–277. [Google Scholar]
- Hansen, D.; Niebauer, J.; Cornelissen, V.; Barna, O.; Neunhäuserer, D.; Stettler, C.; Tonoli, C.; Greco, E.; Fagard, R.; Coninx, K.; et al. Exercise Prescription in Patients with Different Combinations of Cardiovascular Disease Risk Factors: A Consensus Statement from the EXPERT Working Group. Sports Med. 2018, 48, 1781–1797. [Google Scholar] [CrossRef]
- IPAQ Group. Downloadable questionnaires—International Physical Activity Questionnaire. 2010. Available online: https://sites.google.com/site/theipaq/questionnaire_links (accessed on 26 August 2018).
- Ara, A. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms Contents. 2005, p. 15. Available online: https://sites.google.com/site/theipaq/scoring-protocol (accessed on 25 March 2020).
- Gochicoa-Rangel, L.; Mora-Romero, U.; Guerrero-Zúñiga, S.; Silva-Cerón, M.; Cid-Juárez, S.; Velázquez-Uncal, M.; Durán-Cuéllar, A.; Salas-Escamilla, I.; Mejía-Alfaro, R.; Torre-Bouscoulet, L. Prueba de caminata de 6 minutos: Recomendaciones y procedimientos. Neumología y cirugía de tórax 2015, 74, 127–136. [Google Scholar] [CrossRef]
- Muntner, P.; Shimbo, D.; Carey, R.M.; Charleston, J.B.; Gaillard, T.; Misra, S.; Myers, M.G.; Ogedegbe, G.; Schwartz, J.E.; Townsend, R.R.; et al. Measurement of Blood Pressure in Humans: A Scientific Statement From the American Heart Association. Hypertension 2019, 73, E35–E66. [Google Scholar] [CrossRef]
- Lennon, O.C.; Carey, A.; Creed, A.; Durcan, S.; Blake, C. Reliability and validity of COOP/WONCA functional health status charts for stroke patients in primary care. J. Stroke Cerebrovasc. Dis. 2011, 20, 465–473. [Google Scholar] [CrossRef]
- Arsenijevic, J.; Groot, W. Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses Method: A systematic literature review and meta. BMJ Open 2017, 7, e012156. [Google Scholar] [CrossRef] [PubMed]
- Burgess, E.; Hassmén, P.; Pumpa, K.L. Determinants of adherence to lifestyle intervention in adults with obesity: A systematic review. Clin. Obes. 2017, 7, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Skea, Z.C.; Aceves-Martins, M.; Robertson, C.; De Bruin, M.; Avenell, A. Acceptability and feasibility of weight management programmes for adults with severe obesity: A qualitative systematic review. BMJ Open 2019, 9, e029473. [Google Scholar] [CrossRef]
- Bradshaw, P.T.; Monda, K.L.; Stevens, J. Metabolic syndrome in healthy obese, overweight, and normal weight individuals: The atherosclerosis risk in communities study. Obesity 2013, 21, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Gollwitzer, P.M. Implementation intentions: Strong effects of simple plans. Am Psychol. 1999, 54, 493–503. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Levy, S.S.; Readdy, R.T. Reliability of the international physical activity questionnaire in research settings: Last 7-Day self-administered long form. Meas. Phys. Educ. Exerc. Sci. 2009, 13, 191–205. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Silsbury, Z.; Goldsmith, R.; Rushton, A. Systematic review of the measurement properties of self-report physical activity questionnaires in healthy adult populations. BMJ Open 2015, 5, e008430. [Google Scholar] [CrossRef]
- Borresen, J.; Lambert, M.I. Autonomic control of heart rate during and after exercise: Measurements and implications for monitoring training status. Sport. Med. 2008, 38, 633–646. [Google Scholar] [CrossRef] [PubMed]
- Mahon, A.D.; Anderson, C.S.; Hipp, M.J.; Hunt, K.A. Heart Rate Recovery from Submaximal Exercise in Boys and Girls. Med. Sci. Sports Exerc. 2003, 35, 2093–2097. [Google Scholar] [CrossRef] [PubMed]
- Kinmonth, A.-L.; Wareham, N.J.; Hardeman, W.; Sutton, S.; Prevost, A.T.; Fanshawe, T.; Williams, K.M.; Ekelund, U.; Spiegelhalter, D.; Griffin, S.J. Efficacy of a theory-based behavioural intervention to increase physical activity in an at-risk group in primary care (ProActive UK): A randomised trial. Lancet 2008, 371, 41–48. [Google Scholar] [CrossRef]
- Eynon, M.; Foad, J.; Downey, J.; Bowmer, Y.; Mills, H. Assessing the psychosocial factors associated with adherence to exercise referral schemes: A systematic review. Scand. J. Med. Sci. Sports 2019, 29, 638–650. [Google Scholar] [CrossRef]
- Strasser, B. Physical activity in obesity and metabolic syndrome. Ann. N. Y. Acad. Sci. 2013, 1281, 141–159. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Webb, V.L.; Moran, C.H.; Bailer, B.A. Lifestyle modification for obesity: New developments in diet, physical activity, and behavior therapy. Circulation 2012, 125, 1157–1170. [Google Scholar] [CrossRef]
- Miranda, J.J.; Lazo-Porras, M.; Bernabe-Ortiz, A.; Pesantes, M.A.; Diez-Canseco, F.; Cornejo, S.D.P.; Trujillo, A.J. The effect of individual and mixed rewards on diabetes management: A feasibility randomized controlled trial. Wellcome Open Res. 2019, 3, 139. [Google Scholar] [CrossRef]
- Da Silva, M.A.V.; São-João, T.M.; Brizon, V.C.; Franco, D.H.; Mialhe, F.L. Impact of implementation intentions on physical activity practice in adults: A systematic review and meta-analysis of randomized clinical trials. PLoS ONE 2018, 13, e0206294. [Google Scholar] [CrossRef]
- Pratt, M.; Perez, L.G.; Goenka, S.; Brownson, R.C.; Bauman, A.; Sarmiento, O.L.; Hallal, P.C. Can Population Levels of Physical Activity be Increased? Global Evidence and Experience. Prog. Cardiovasc. Dis. 2015, 57, 356. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W.; Alkandari, J.R.; Andersen, L.B.; Blair, S.N.; Brownson, R.C.; et al. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]

| Outcome Measure | Model Adjusted by Sex and Age | |||||
|---|---|---|---|---|---|---|
| Follow-Up (6th Week) N = 11 | Final Evaluation (12th Week) N = 21 | |||||
| Coef. (IC 95%) | p-Value 1 | Coef. (IC 95%) | p-Value 1 | |||
| Primary | ||||||
| Physical Activity (METs-min/week) | ||||||
| Walking | −670 | (−1778.4–438.5) | 0.236 | 851.3 | (−98.0–1800.7) | 0.079 |
| Moderate Intensity | −710 | (−1588.0–166.7) | 0.112 | 837.2 | (−36.1–1710.4) | 0.060 |
| Vigorous Intensity | 2646.3 | (691.9–4600.8) | 0.008 | 724.4 | (−262.0–1710.7) | 0.150 |
| Sitting time (hours/day) | 0.1 | (−1.0–1.2) | 0.847 | 0.1 | (−1.4–1.6) | 0.881 |
| Six-minute walk test | ||||||
| BR diff | −1.5 | (−3.0–−0.1) | 0.039 | −1.1 | (−3.0–0.9) | 0.286 |
| HR diff | −8.6 | (−18.0–0.7) | 0.071 | −22.3 | (−30.9–−13.7) | 0.001 |
| SBP diff | −3.2 | (−9.1–2.7) | 0.285 | −0.4 | (−6.9–6.2) | 0.910 |
| DBP diff | 0.5 | (−9.1–0.6) | 0.867 | −4.2 | (−9.1–0.6) | 0.087 |
| Borg Scale diff | ||||||
| Dyspnea | −0.7 | (−2.1–0.6) | 0.297 | 1.1 | (−1.2–3.3) | 0.346 |
| Fatigue | −0.1 | (−1.9–1.7) | 0.918 | 1.3 | (−0.4–2.9) | 0.135 |
| Walk Distance (m) | −12.6 | (−51.0–25.8) | 0.521 | −45.4 | (−86.9–−3.8) | 0.032 |
| Secondary | ||||||
| Body weight (Kg) | 0.3 | (−0.5–1.1) | 0.506 | −0.2 | (−1.4–1.0) | 0.689 |
| BMI (Kg/cm2) | 0.2 | (−0.2–0.5) | 0.335 | −0.1 | (−0.6–0.4) | 0.696 |
| Waist circumference (cm) | −1 | (−2.7–0.7) | 0.248 | −1.6 | (−3.2–−0.02) | 0.048 |
| Heart rate | 1 | (−3.9–5.9) | 0.685 | 0.6 | (−3.1–4.3) | 0.744 |
| Blood pressure (mmHg) | ||||||
| SBP | −0.2 | (−4.3–4.0) | 0.932 | 0.4 | (−3.2–4.0) | 0.843 |
| DBP | −3.4 | (−9.4–2.7) | 0.279 | 3.6 | (0.4–6.8) | 0.027 |
| Quality of Life | ||||||
| Physical fitness | −0.2 | (−0.7–0.2) | 0.344 | −0.04 | (−0.5–0.4) | 0.874 |
| Feelings | 0.6 | (0.1–1.2) | 0.033 | 0.3 | (−0.3–0.9) | 0.378 |
| Daily activities | 0.1 | (−0.5–0.7) | 0.709 | 0.4 | (−0.2–0.9) | 0.202 |
| Social activities | 0.6 | (−0.1–1.3) | 0.114 | 0.4 | (−0.2–0.9) | 0.212 |
| Change in health | −0.5 | (−1.0–0.1) | 0.081 | 0.1 | (−0.5–0.6) | 0.858 |
| Overall health | −0.3 | (−0.8–0.3) | 0.313 | −0.3 | (−0.8–0.2) | 0.224 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tenorio-Mucha, J.; Busta-Flores, P.; De la Cruz-Saldaña, T.; Montufar-Crespo, S.M.; Malaga, G.; Bernabe-Ortiz, A.; Lazo-Porras, M. Pilot Feasibility Assessment of a Tailored Physical Activity Prescription in Overweight and Obese People in a Public Hospital. Int. J. Environ. Res. Public Health 2022, 19, 10774. https://doi.org/10.3390/ijerph191710774
Tenorio-Mucha J, Busta-Flores P, De la Cruz-Saldaña T, Montufar-Crespo SM, Malaga G, Bernabe-Ortiz A, Lazo-Porras M. Pilot Feasibility Assessment of a Tailored Physical Activity Prescription in Overweight and Obese People in a Public Hospital. International Journal of Environmental Research and Public Health. 2022; 19(17):10774. https://doi.org/10.3390/ijerph191710774
Chicago/Turabian StyleTenorio-Mucha, Janeth, Patricia Busta-Flores, Tania De la Cruz-Saldaña, Silvia Marcela Montufar-Crespo, German Malaga, Antonio Bernabe-Ortiz, and Maria Lazo-Porras. 2022. "Pilot Feasibility Assessment of a Tailored Physical Activity Prescription in Overweight and Obese People in a Public Hospital" International Journal of Environmental Research and Public Health 19, no. 17: 10774. https://doi.org/10.3390/ijerph191710774
APA StyleTenorio-Mucha, J., Busta-Flores, P., De la Cruz-Saldaña, T., Montufar-Crespo, S. M., Malaga, G., Bernabe-Ortiz, A., & Lazo-Porras, M. (2022). Pilot Feasibility Assessment of a Tailored Physical Activity Prescription in Overweight and Obese People in a Public Hospital. International Journal of Environmental Research and Public Health, 19(17), 10774. https://doi.org/10.3390/ijerph191710774






