Smoking Cessation Programs Are Less Effective in Smokers with Low Socioeconomic Status Even When Financial Incentives for Quitting Smoking Are Offered—A Community-Randomized Smoking Cessation Trial in Denmark
Abstract
:1. Introduction
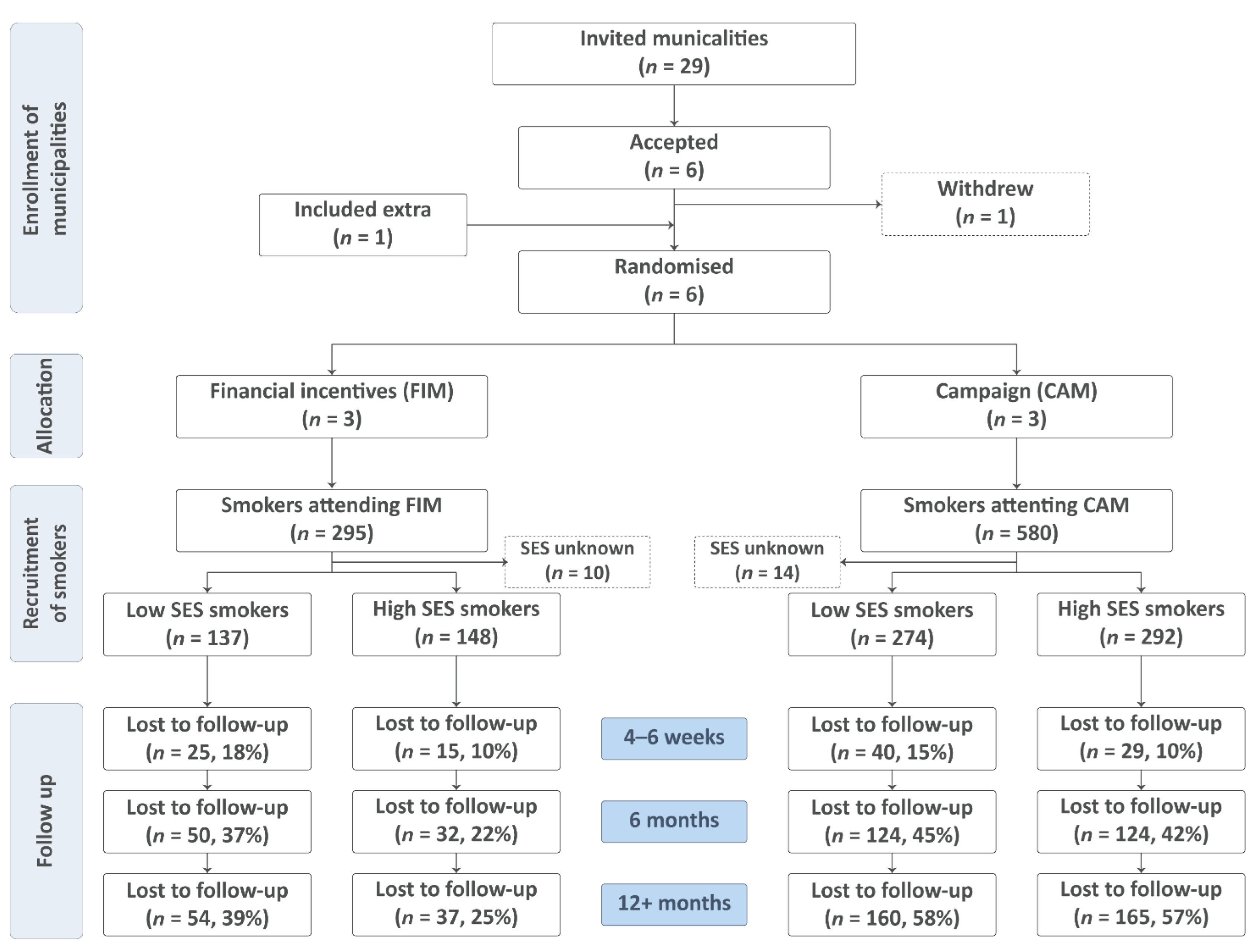
2. Materials and Methods
2.1. Participants
2.2. Randomization and Blinding
2.3. Interventions in the Randomized Trial
2.3.1. Intervention in Financial Incentives Municipalities (FIMs)
2.3.2. Intervention in Campaign Municipalities (CAMs)
2.4. Outcome
2.5. Statistics
3. Results
3.1. Attrition and Loss to Follow-Up
3.2. Baseline Characteristics of Smokers
3.3. Recruitment
3.4. Abstinence
3.5. Adjusted ITT Analyses
3.6. Complete Case Analyses (Appendix C)
4. Discussion
4.1. Strengths
4.2. Weaknesses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B

Appendix C
| Unadjusted Analyses | Adjusted Analyses | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | OR | [CI 95%] | p | OR | [CI 95%] | p | ||
| Low SES | ||||||||
| CAMs | 1.00 | |||||||
| FIMs (4–6 weeks) | 2.55 | [1.51, 4.30] | ≤0.001 | * | 2.89 | [1.31, 6.38] | 0.009 | * |
| FIMs (6 months) | 1.01 | [0.58, 1.76] | 0.963 | 0.72 | [0.29, 1.81] | 0.490 | ||
| FIMs (12+-months) | 0.80 | [0.43, 1.48] | 0.475 | 0.74 | [0.37, 1.46] | 0.381 | ||
| High SES | ||||||||
| CAMs | 1.00 | |||||||
| FIMs (4–6 weeks) | 2.41 | [1.37, 4.24] | 0.002 | * | 2.74 | [1.28, 5.84] | 0.009 | * |
| FIMs (6 months) | 1.50 | [0.93, 2.41] | 0.095 | 1.64 | [0.90, 2.98] | 0.107 | ||
| FIMs (12+-months) | 1.43 | [0.85, 2.43] | 0.179 | 1.53 | [0.87, 2.68] | 0.136 | ||
References
- GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021, 397, 2337–2360. [Google Scholar] [CrossRef]
- Zhou, X.; Vohs, K.D.; Baumeister, R.F. The symbolic power of money: Reminders of money alter social distress and physical pain. Psychol. Sci. 2009, 20, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Notley, C.; Gentry, S.; Livingstone-Banks, J.; Bauld, L.; Perera, R.; Hartmann-Boyce, J. Incentives for smoking cessation. Cochrane Database Syst. Rev. 2019, 7, Cd004307. [Google Scholar] [CrossRef] [PubMed]
- Pisinger, C.; Toxværd, C.G.; Rasmussen, M. Are financial incentives more effective than health campaigns to quit smoking? A community-randomised smoking cessation trial in Denmark. Prev. Med. 2022, 154, 106865. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Das, S.; Young-Wolff, K.C. Smoking, Mental Illness, and Public Health. Annu. Rev. Public Health 2017, 38, 165–185. [Google Scholar] [CrossRef]
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2014.
- Hiscock, R.; Bauld, L.; Amos, A.; Fidler, J.A.; Munafò, M. Socioeconomic status and smoking: A review. Ann. N. Y. Acad. Sci. 2012, 1248, 107–123. [Google Scholar] [CrossRef]
- Milcarz, M.; Polanska, K.; Bak-Romaniszyn, L.; Kaleta, D. Tobacco Health Risk Awareness among Socially Disadvantaged People-A Crucial Tool for Smoking Cessation. Int. J. Env. Res. Public Health 2018, 15, 2244. [Google Scholar] [CrossRef]
- Cockerham, W.C.; Hamby, B.W.; Oates, G.R. The Social Determinants of Chronic Disease. Am. J. Prev. Med. 2017, 52, S5–S12. [Google Scholar] [CrossRef]
- Rasmussen, M.; Fernández, E.; Tønnesen, H. Effectiveness of the Gold Standard Programme compared with other smoking cessation interventions in Denmark: A cohort study. BMJ Open 2017, 7, e013553. [Google Scholar] [CrossRef]
- Neumann, T.; Rasmussen, M.; Ghith, N.; Heitmann, B.L.; Tønnesen, H. The Gold Standard Programme: Smoking cessation interventions for disadvantaged smokers are effective in a real-life setting. Tob. Control 2013, 22, e9. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, M.; Tønnesen, H. The Danish smoking cessation database. Clin. Health Promot. 2016, 6, 36–41. [Google Scholar] [CrossRef]
- Goldstein, A.O.; Gans, S.P.; Ripley-Moffitt, C.; Kotsen, C.; Bars, M. Use of Expired Air Carbon Monoxide Testing in Clinical Tobacco Treatment Settings. Chest 2018, 153, 554–562. [Google Scholar] [CrossRef]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerström, K.O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef]
- Kotz, D.; West, R. Explaining the social gradient in smoking cessation: It’s not in the trying, but in the succeeding. Tob. Control 2009, 18, 43–46. [Google Scholar] [CrossRef]
- Siahpush, M.; McNeill, A.; Borland, R.; Fong, G.T. Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: Findings from the International Tobacco Control (ITC) Four Country Survey. Tob. Control 2006, 15 (Suppl. S3), iii71–iii75. [Google Scholar] [CrossRef] [PubMed]
- Boland, V.C.; Mattick, R.P.; McRobbie, H.; Siahpush, M.; Courtney, R.J. I’m not strong enough; I’m not good enough. I can’t do this, I’m failing—A qualitative study of low-socioeconomic status smokers’ experiences with accesssing cessation support and the role for alternative technology-based support. Int. J. Equity Health 2017, 16, 196. [Google Scholar] [CrossRef] [PubMed]
- Hiscock, R.; Judge, K.; Bauld, L. Social inequalities in quitting smoking: What factors mediate the relationship between socioeconomic position and smoking cessation? J. Public Health 2011, 33, 39–47. [Google Scholar] [CrossRef]
- Courtney, R.J.; Naicker, S.; Shakeshaft, A.; Clare, P.; Martire, K.A.; Mattick, R.P. Smoking Cessation among Low-Socioeconomic Status and Disadvantaged Population Groups: A Systematic Review of Research Output. Int. J. Environ. Res. Public Health 2015, 12, 6403–6422. [Google Scholar] [CrossRef]
- Berlin, I.; Berlin, N.; Malecot, M.; Breton, M.; Jusot, F.; Goldzahl, L. Financial incentives for smoking cessation in pregnancy: Multicentre randomised controlled trial. BMJ 2021, 375, e065217. [Google Scholar] [CrossRef]
- Ladapo, J.A.; Tseng, C.H.; Sherman, S.E. Financial Incentives for Smoking Cessation in Hospitalized Patients: A Randomized Clinical Trial. Am. J. Med. 2020, 133, 741–749. [Google Scholar] [CrossRef]
- White, J.S.; Lowenstein, C.; Srivirojana, N.; Jampaklay, A.; Dow, W.H. Incentive programmes for smoking cessation: Cluster randomized trial in workplaces in Thailand. BMJ 2020, 371, m3797. [Google Scholar] [CrossRef]
- Kurti, A.N.; Nighbor, T.D.; Tang, K.; Bolívar, H.A.; Evemy, C.G.; Skelly, J.; Higgins, S.T. Effect of Smartphone-Based Financial Incentives on Peripartum Smoking Among Pregnant Individuals: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2211889. [Google Scholar] [CrossRef]
- Parks, M.J.; Hughes, K.D.; Keller, P.A.; Lachter, R.B.; Kingsbury, J.H.; Nelson, C.L.; Slater, J.S. Financial incentives and proactive calling for reducing barriers to tobacco treatment among socioeconomically disadvantaged women: A factorial randomized trial. Prev. Med. 2019, 129, 105867. [Google Scholar] [CrossRef] [PubMed]
- Stotts, A.L.; Northrup, T.F.; Green, C.; Suchting, R.; Hovell, M.F.; Khan, A.; Villarreal, Y.R.; Schmitz, J.M.; Velasquez, M.M.; Hammond, S.K.; et al. Reducing Tobacco Smoke Exposure in High-Risk Infants: A Randomized, Controlled Trial. J. Pediatr. 2020, 218, 35–41.e1. [Google Scholar] [CrossRef] [PubMed]
- Businelle, M.S.; Kendzor, D.E.; Kesh, A.; Cuate, E.L.; Poonawalla, I.B.; Reitzel, L.R.; Okuyemi, K.S.; Wetter, D.W. Small financial incentives increase smoking cessation in homeless smokers: A pilot study. Addict. Behav. 2014, 39, 717–720. [Google Scholar] [CrossRef]
- Kendzor, D.E.; Businelle, M.S.; Poonawalla, I.B.; Cuate, E.L.; Kesh, A.; Rios, D.M.; Ma, P.; Balis, D.S. Financial incentives for abstinence among socioeconomically disadvantaged individuals in smoking cessation treatment. Am. J. Public Health 2015, 105, 1198–1205. [Google Scholar] [CrossRef] [PubMed]
- Fraser, D.L.; Fiore, M.C.; Kobinsky, K.; Adsit, R.; Smith, S.S.; Johnson, M.L.; Baker, T.B. A Randomized Trial of Incentives for Smoking Treatment in Medicaid Members. Am. J. Prev. Med. 2017, 53, 754–763. [Google Scholar] [CrossRef] [PubMed]
- Mundt, M.P.; Baker, T.B.; Fraser, D.L.; Smith, S.S.; Piper, M.E.; Fiore, M.C. Paying Low-Income Smokers to Quit? The Cost-Effectiveness of Incentivizing Tobacco Quit Line Engagement for Medicaid Recipients Who Smoke. Value Health 2019, 22, 177–184. [Google Scholar] [CrossRef]
- Van den Brand, F.A.; Candel, M.; Nagelhout, G.E.; Winkens, B.; van Schayck, C.P. How Financial Incentives Increase Smoking Cessation: A Two-Level Path Analysis. Nicotine Tob. Res. 2021, 23, 99–106. [Google Scholar] [CrossRef]
- Waters, A.F.; Businelle, M.S.; Frank, S.G.; Hébert, E.T.; Kendzor, D.E. Understanding the link between contingency management and smoking cessation: The roles of sex and self-efficacy. Addict. Behav. 2018, 84, 99–105. [Google Scholar] [CrossRef]
- Alexander, A.C.; Hébert, E.T.; Businelle, M.S.; Kendzor, D.E. Greater perceived importance of earning abstinence-contingent incentives is associated with smoking cessation among socioeconomically disadvantaged adults. Addict. Behav. 2019, 95, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.; Platt, S.; Amos, A. Equity impact of European individual-level smoking cessation interventions to reduce smoking in adults: A systematic review. Eur. J. Public Health 2014, 24, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Judge, K.; Bauld, L.; Chesterman, J.; Ferguson, J. The English smoking treatment services: Short-term outcomes. Addiction 2005, 100 (Suppl. S2), 46–58. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.; Bauld, L.; Chesterman, J.; Judge, K. The English smoking treatment services: One-year outcomes. Addiction 2005, 100 (Suppl. S2), 59–69. [Google Scholar] [CrossRef] [PubMed]
- Bauld, L.; Judge, K.; Platt, S. Assessing the impact of smoking cessation services on reducing health inequalities in England: Observational study. Tob. Control 2007, 16, 400–404. [Google Scholar] [CrossRef]
- Thomas, S.; Fayter, D.; Misso, K.; Ogilvie, D.; Petticrew, M.; Sowden, A.; Whitehead, M.; Worthy, G. Population tobacco control interventions and their effects on social inequalities in smoking: Systematic review. Tob. Control 2008, 17, 230–237. [Google Scholar] [CrossRef]
- Hu, Y.; van Lenthe, F.J.; Platt, S.; Bosdriesz, J.R.; Lahelma, E.; Menvielle, G.; Regidor, E.; Santana, P.; de Gelder, R.; Mackenbach, J.P. The Impact of Tobacco Control Policies on Smoking Among Socioeconomic Groups in Nine European Countries, 1990–2007. Nicotine Tob. Res. 2017, 19, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Mundt, M.P.; Baker, T.B.; Piper, M.E.; Smith, S.S.; Fraser, D.L.; Fiore, M.C. Financial incentives to Medicaid smokers for engaging tobacco quit line treatment: Maximising return on investment. Tob. Control 2020, 29, 320–325. [Google Scholar] [CrossRef]
- Boyd, K.A.; Briggs, A.H.; Bauld, L.; Sinclair, L.; Tappin, D. Are financial incentives cost-effective to support smoking cessation during pregnancy? Addiction 2016, 111, 360–370. [Google Scholar] [CrossRef]
- McCabe, C.; Claxton, K.; Culyer, A.J. The NICE cost-effectiveness threshold: What it is and what that means. Pharmacoeconomics 2008, 26, 733–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tappin, D.; Bauld, L.; Purves, D.; Boyd, K.; Sinclair, L.; MacAskill, S.; McKell, J.; Friel, B.; McConnachie, A.; de Caestecker, L.; et al. Financial incentives for smoking cessation in pregnancy: Randomised controlled trial. BMJ 2015, 350, h134. [Google Scholar] [CrossRef] [PubMed]
- Halpern, S.D.; Harhay, M.O.; Saulsgiver, K.; Brophy, C.; Troxel, A.B.; Volpp, K.G. A Pragmatic Trial of E-Cigarettes, Incentives, and Drugs for Smoking Cessation. N. Engl. J. Med. 2018, 378, 2302–2310. [Google Scholar] [CrossRef] [PubMed]
- Weng, X.; Wu, Y.; Luk, T.T.; Li, W.H.C.; Cheung, D.Y.T.; Tong, H.S.C.; Lai, V.; Lam, T.H.; Wang, M.P. Active referral plus a small financial incentive upon cessation services use on smoking abstinence: A community-based, cluster-randomised controlled trial. Lancet Reg. Health West Pac. 2021, 13, 100189. [Google Scholar] [CrossRef]
- Moores, C.J.; Miller, J.; Perry, R.A.; Chan, L.L.H.; Daniels, L.A.; Vidgen, H.A.; Magarey, A.M. CONSORT to community: Translation of an RCT to a large-scale community intervention and learnings from evaluation of the upscaled program. BMC Public Health 2017, 17, 918. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Characteristics | Financial Incentives Municipalities | Campaign Municipalities | ||||||
|---|---|---|---|---|---|---|---|---|
| Low SES | High SES | Low SES | High SES | |||||
| n | % | n | % | n | % | n | % | |
| Total | 137 | 48.1% | 148 | 51.9% | 274 | 48.4% | 292 | 51.6% |
| Sex | ||||||||
| Men | 57 | 41.6% | 59 | 39.9% | 114 | 41.6% | 121 | 41.4% |
| Women | 80 | 58.4% | 89 | 60.1% | 160 | 58.4% | 171 | 58.6% |
| Age | ||||||||
| Up to 24 | 8 | 5.8% | 29 | 10.6% | 12 | 4.1% | ||
| 25–34 | 12 | 8.8% | 12 | 8.1% | 35 | 12.8% | 33 | 11.3% |
| 35–44 | 21 | 15.3% | 21 | 14.2% | 41 | 15.0% | 41 | 14.0% |
| 45–54 | 38 | 27.7% | 30 | 20.3% | 56 | 20.4% | 70 | 24.0% |
| 55–66 | 49 | 35.8% | 42 | 28.4% | 90 | 32.8% | 76 | 26.0% |
| 67+ | 9 | 6.6% | 43 | 29.1% | 23 | 8.4% | 60 | 20.5% |
| Heavy smokers | ||||||||
| No (1–14 cigarettes/day) | 21 | 15.3% | 31 | 20.9% | 71 | 25.9% | 88 | 30.1% |
| Yes (15+ cigarettes/day) | 116 | 84.7% | 117 | 79.1% | 203 | 74.1% | 204 | 69.9% |
| Fagerström score a | ||||||||
| Low (0–6) | 89 | 65.0% | 106 | 71.6% | 169 | 61.7% | 231 | 79.1% |
| High (7–10) | 48 | 35.0% | 42 | 28.4% | 105 | 38.3% | 61 | 20.9% |
| Free/subsidized NRT b | ||||||||
| No | 113 | 82.5% | 99 | 66.9% | 134 | 48.9% | 149 | 51.0% |
| Yes | 24 | 17.5% | 49 | 33.1% | 140 | 51.1% | 143 | 49.0% |
| Financial Incentives Municipalities | Campaign Municipalities | |||||||
|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2017 | 2018 | |||||
| n | % | n | % | n | % | n | % | |
| Socioeconomic status | ||||||||
| Low SES | 84 | 44.4% | 137 | 48.1% | 146 | 47.9% | 274 | 48.4% |
| High SES | 105 | 55.6% | 148 | 51.9% | 159 | 52.1% | 292 | 51.6% |
| Unadjusted Analyses | Adjusted Analyses | |||||
|---|---|---|---|---|---|---|
| Intervention | OR | [CI 95%] | p | OR | [CI 95%] | p |
| Low SES | ||||||
| CAMs | 1.00 | |||||
| FIMs (4–6 weeks) | 1.77 | [1.16, 2.70] | 0.008 * | 1.16 | [0.62, 2.18] | 0.639 |
| FIMs (6 months) | 1.22 | [0.74, 2.01] | 0.437 | 0.62 | [0.26, 1.45] | 0.268 |
| FIMs (12+-months) | 1.29 | [0.73, 2.28] | 0.375 | 1.17 | [0.55, 2.51] | 0.677 |
| High SES | ||||||
| CAMs | 1.00 | |||||
| FIMs (4–6 weeks) | 1.84 | [1.17, 2.91] | 0.009 * | 1.51 | [0.63, 3.62] | 0.344 |
| FIMs (6 months) | 2.16 | [1.41, 3.30] | ≤0.001 * | 2.35 | [1.21, 4.55] | 0.011 * |
| FIMs (12+-months) | 2.69 | [1.68, 4.33] | ≤0.001 * | 2.59 | [1.59, 4.22] | ≤0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pisinger, C.; Toxværd, C.G.; Rasmussen, M. Smoking Cessation Programs Are Less Effective in Smokers with Low Socioeconomic Status Even When Financial Incentives for Quitting Smoking Are Offered—A Community-Randomized Smoking Cessation Trial in Denmark. Int. J. Environ. Res. Public Health 2022, 19, 10879. https://doi.org/10.3390/ijerph191710879
Pisinger C, Toxværd CG, Rasmussen M. Smoking Cessation Programs Are Less Effective in Smokers with Low Socioeconomic Status Even When Financial Incentives for Quitting Smoking Are Offered—A Community-Randomized Smoking Cessation Trial in Denmark. International Journal of Environmental Research and Public Health. 2022; 19(17):10879. https://doi.org/10.3390/ijerph191710879
Chicago/Turabian StylePisinger, Charlotta, Cecilie Goltermann Toxværd, and Mette Rasmussen. 2022. "Smoking Cessation Programs Are Less Effective in Smokers with Low Socioeconomic Status Even When Financial Incentives for Quitting Smoking Are Offered—A Community-Randomized Smoking Cessation Trial in Denmark" International Journal of Environmental Research and Public Health 19, no. 17: 10879. https://doi.org/10.3390/ijerph191710879
APA StylePisinger, C., Toxværd, C. G., & Rasmussen, M. (2022). Smoking Cessation Programs Are Less Effective in Smokers with Low Socioeconomic Status Even When Financial Incentives for Quitting Smoking Are Offered—A Community-Randomized Smoking Cessation Trial in Denmark. International Journal of Environmental Research and Public Health, 19(17), 10879. https://doi.org/10.3390/ijerph191710879







