Illness Experience and Quality of Life in Sjögren Syndrome Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Sample
2.3. Procedure
2.3.1. Life Experiences of Chilean Women with SS
2.3.2. Quality of Life
2.3.3. General Quality of Life
2.3.4. Oral Health-Related Quality of Life
2.4. Statistical Analyses
3. Results
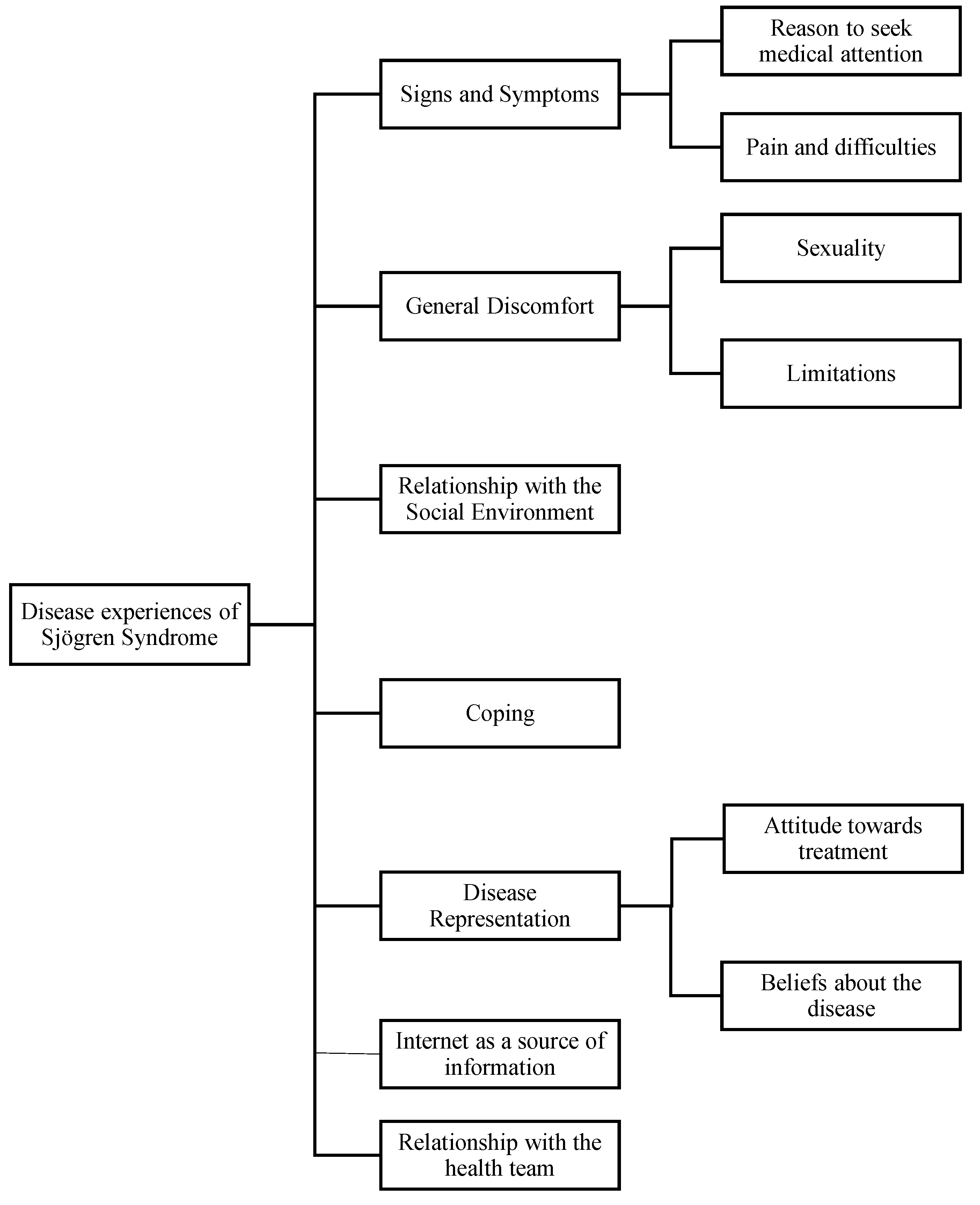
3.1. Objective 1: Concept Analysis
3.2. Objective 2: Level of Agreement with Experiences
3.3. Objective 3: Quality of Life
4. Discussion
4.1. Experiences of Disease and Level of Agreement with Experiences
4.2. General Measures of Health-Related Quality of Life
4.3. Specific Measures of Oral Health-Related Quality of Life
4.4. Meaning of the Study for Clinicians and Policy Makers
4.5. Unresolved Questions and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| My Experience with Sjögren’s Syndrome Is That | Agree | Somewhat Agree | Somewhat Disagree | Disagree | p |
|---|---|---|---|---|---|
| (1) A doctor sent me to another professional. | 51.6 (16) | 16.1 (5) | 6.5 (2) | 25.8 (8) | 0.08 |
| (2) I had never heard of this disease before. | 83.9 (26) | 0 (0) | 3.2 (1) | 12.9 (4) | <0.001 1 |
| (3) I try not to think about the disease or talk about it. | 35.5 (11) | 38.7 (12) | 19.4 (6) | 6.5 (2) | 0.004 1 |
| (4) I have not had support with my illness. | 16.1 (5) | 25.8 (8) | 12.9 (4) | 45.2 (14) | 0.081 |
| (5) The doctor told me that I don’t have to look for more information. | 9.7 (3) | 19.4 (6) | 6.5 (2) | 64.5 (20) | 0.001 1 |
| (6) I don’t understand some information from the internet. | 22.6 (7) | 19.4 (6) | 19.4 (6) | 38.7 (12) | 0.264 |
| (7) Sometimes I want to stop (or have stopped) the medication due to adverse reactions. | 35.5 (11) | 16.1 (5) | 6.5 (2) | 41.9 (13) | 0.779 |
| (8) I don’t know how I will feel tomorrow. | 74.2 (23) | 9.7 (3) | 0 (0) | 16.1 (5) | 0.001 1 |
| (9) My doctor doesn’t inform me enough about my illness. | 22.6 (7) | 32.3 (10) | 9.7 (3) | 35.5 (11) | 0.678 |
| (10) Some days I can’t open my eyes and the sun bothers them. | 54.8 (17) | 29 (9) | 6.5 (2) | 9.7 (3) | <0.001 1 |
| (11) The pain in my eyes motivated myself to ask to the doctor. | 29 (9) | 12.9 (4) | 6.5 (2) | 51.6 (16) | 0.187 |
| (12) I didn’t dare to ask the doctor more about it. | 19.4 (6) | 6.5 (2) | 25.8 (8) | 48.4 (15) | 0.023 1 |
| (13) People that don’t suffer this disease, don’t understand it. | 80.6 (25) | 9.7 (3) | 3.2 (1) | 6.5 (2) | <0.001 1 |
| (14) Even if I feel bad, I encourage myself and try to be independent. | 87.1 (27) | 9.7 (3) | 3.2 (1) | 0 (0) | <0.001 1 |
| (15) When I have a lot of pain I can’t do housework and my daily routine. | 58.1 (18) | 19.4 (6) | 3.2 (1) | 19.4 (6) | 0.008 1 |
| (16) It has a hereditary component. | 22.6 (7) | 25.8 (8) | 16.1 (5) | 35.5 (11) | 0.485 |
| (17) It bothers me to be constantly taking medicine, using drops, etc. | 67.6 (21) | 22.6 (7) | 6.5 (2) | 3.2 (1) | <0.001 1 |
| (18) I think that my illness will never end, that I will always be sick. | 74.2 (23) | 16.1 (5) | 0 (0) | 9.7 (3) | <0.001 1 |
| (19) I don’t say it and I don’t explain it to anyone because it is difficult to understand. | 29 (9) | 32.3 (10) | 12.9 (4) | 25.8 (8) | 0.492 |
| (20) This permanent disease generates other diseases. | 58.1 (18) | 19.4 (6) | 16.1 (5) | 6.5 (2) | <0.001 1 |
| (21) I don’t research on websites because there is information that I don’t like or scares me. | 25.8 (8) | 22.6 (7) | 12.9 (4) | 38.7 (12) | 0.489 |
| (22) I plan several things to do, but for fatigue, I only finish one. | 48.4 (15) | 25.8 (8) | 3.2 (1) | 22.6 (7) | 0.041 1 |
| (23) I have isolated myself socially. | 22.6 (7) | 25.8 (8) | 6.5 (2) | 45.2 (14) | 0.244 |
| (24) I live tired, living tired is very uncomfortable. | 51.6 (16) | 22.6 (7) | 9.7 (3) | 16.1 (5) | 0.010 1 |
| (25) I have lowered my efficiency in my daily activities. | 45.2 (14) | 41.9 (13) | 9.7 (3) | 3.2 (1) | <0.05 1 |
| (26) When I was diagnosed, I felt relieved because I already knew what I had. | 41.9 (13) | 3.2 (1) | 16.1 (5) | 38.7 (12) | 0.958 |
| (27) I feel joint pain and fatigue. | 71 (22) | 16.1 (5) | 3.2 (1) | 9.7 (3) | <0.001 1 |
| (28) It is very difficult to ask for an appointment with the doctor or specialist. | 54.8 (17) | 16.1 (5) | 3.2 (1) | 25.8 (8) | 0.052 |
| (29) With and without medication I feel the same, or worse. | 25.8 (8) | 9.7 (3) | 22.6 (7) | 41.9 (13) | 0.194 |
| (30) I can’t eat dry foods. | 54.8 (17) | 9.7 (3) | 22.6 (7) | 12.9 (4) | 0.01 1 |
| (31) I got used to living with pain. | 38.7 (12) | 29 (9) | 12.9 (4) | 19.4 (6) | 0.085 |
| (32) The treatments are expensive. | 83.9 (26) | 9.7 (3) | 3.2 (1) | 3.2 (1) | <0.001 1 |
| (33) There are doctors and dentists who don’t know the disease. | 54.8 (17) | 19.4 (6) | 6.5 (2) | 19.4 (6) | 0.014 1 |
| (34) I want, but i can’t cry. | 48.4 (15) | 6.5 (2) | 16.1 (5) | 29 (9) | 0.275 |
| (35) My doctor has always been very willing and responsive. | 54.8 (17) | 16.1 (5) | 16.1 (5) | 12.9 (4) | 0.005 1 |
| (36) I feel pain in my legs. | 67.7 (21) | 16.1 (5) | 9.7 (3) | 6.5 (2) | <0.001 1 |
| (37) I always need to eat sweets, gum or drink a lot of water. | 80.6 (25) | 16.1 (5) | 0 (0) | 3.2 (1) | <0.001 1 |
| (38) The system is hostile; they punish you for being sick. | 29 (9) | 25.8 (8) | 9.7 (3) | 35.5 (11) | 0.895 |
| (39) Sometimes I don’t have the energy to have sex. | 61.3 (19) | 25.8 (8) | 3.2 (1) | 9.7 (3) | <0.001 1 |
| (40) Sometimes I look good on the outside, so people don’t understand that I’m sick. | 83.9 (26) | 3.2 (1) | 6.5 (2) | 6.5 (2) | <0.001 1 |
| (41) Sometimes doctors don’t believe you. | 41.9 (13) | 19.4 (6) | 9.7 (3) | 29 (9) | 0.319 |
| (42) This disease is activated on the emotional side. | 67.7 (21) | 19.4 (6) | 6.5 (2) | 6.5 (2) | <0.001 1 |
| (43) When I feel bad, I try not to let them realize it so as not to worry them. | 54.8 (17) | 16.1 (5) | 12.9 (4) | 16.1 (5) | 0.010 1 |
| (44) My family is always aware of my illness. | 54.8 (17) | 9.7 (3) | 19.4 (6) | 16.1 (5) | 0.018 1 |
| (45) Those who work with patients are unkind and don’t put themselves in our shoes. | 22.6 (7) | 32.3 (10) | 22.6 (7) | 22.6 (7) | 0.785 |
| (46) I have not looked for more information, I only know what the doctor told me. | 12.9 (4) | 9.7 (3) | 9.7 (3) | 67.7 (21) | 0.001 1 |
| (47) I don’t believe everything that I find on the internet. | 45.2 (14) | 32.3 (10) | 6.5 (2) | 16.1 (5) | 0.011 1 |
| (48) I have been learning about the disease through the internet. | 32.3 (10) | 45.2 (14) | 9.7 (3) | 12.9 (4) | 0.013 1 |
| (49) There are days when I wake up very well and suddenly, I feel bad. | 71 (22) | 19.4 (6) | 3.2 (1) | 6.5 (2) | <0.001 1 |
| (50) I thought that dry mouth was normal, and not a symptom of this disease. | 61.3 (19) | 16.1 (5) | 3.2 (1) | 19.4 (6) | 0.006 1 |
| (51) As long as I take care of myself, everything will be fine, because it depends on me. | 45.2 (14) | 29 (9) | 22.6 (7) | 3.2 (1) | 0.001 1 |
| (52) My teeth have been badly affected. | 61.3 (19) | 12.9 (4) | 6.5 (2) | 19.4 (6) | 0.008 1 |
| (53) My partner has been understanding about the consequences of the disease in sexual relations. | 54.8 (17) | 12.9 (4) | 6.5 (2) | 25.8 (8) | 0.062 |
| (54) I avoid having sex because of my vaginal dryness. | 35.5 (11) | 29 (9) | 9.7 (3) | 25.8 (8) | 0.286 |
| (55) I wish there were more treatment alternatives or that it was more comprehensive. | 93.5 (29) | 6.5 (2) | 0 (0) | 0 (0) | <0.001 1 |
| (56) When I found out about the diagnosis, I was sad. | 61.3 (19) | 19.4 (6) | 6.5 (2) | 12.9 (4) | 0.001 1 |
| (57) I have continued my normal life; I have not deprived myself due to the illness. | 41.9 (13) | 41.9 (13) | 6.5 (2) | 9.7 (3) | 0.001 1 |
| (58) It bothers me to think that this is not going to end. | 61.3 (19) | 22.6 (7) | 3.2 (1) | 12.9 (4) | 0.001 1 |
| (59) I don’t ask for help, nor do I tell how I feel, so as not to bother. | 38.7 (12) | 25.8 (8) | 12.9 (4) | 22.6 (7) | 0.167 |
| (60) You must face people and say things clearly. | 41.9 (13) | 22.6 (7) | 25.8 (8) | 9.7 (3) | 0.022 1 |
| (61) I feel that doctors don’t have time to attend. | 29 (9) | 22.6 (7) | 19.4 (6) | 29 (9) | 0.943 |
| (62) I was motivated to see the doctor because of my dry eyes. | 32.3 (10) | 19.4 (6) | 3.2 (1) | 45.2 (14) | 0.546 |
| (63) I feel burning and dry eyes. | 74.2 (23) | 16.1 (5) | 6.5 (2) | 3.2 (1) | <0.001 1 |
| (64) They tell you about the symptoms you might have, but it is different when you really live it. | 74.2 (23) | 16.1 (5) | 6.5 (2) | 3.2 (1) | <0.001 1 |
| (65) There is no effective treatment that will assure you that it will work. | 67.7 (21) | 16.1 (5) | 9.7 (3) | 6.5 (2) | <0.001 1 |
| (66) When I was diagnosed, I didn’t give it more importance. | 19.4 (6) | 16.1 (5) | 9.7 (3) | 54.8 (17) | 0.029 1 |
| (67) It hurts me to have sex. | 35.5 (11) | 19.4 (6) | 22.6 (7) | 22.6 (7) | 0.401 |
| (68) What motivated me to see the doctor was my pain in the extremities and joints. | 45.2 (14) | 6.5 (2) | 9.7 (3) | 38.7 (12) | 0.719 |
| (69) I have to do what the doctors say and take care of myself. | 48.4 (15) | 38.7 (12) | 9.7 (3) | 3.2 (1) | <0.001 1 |
| (70) Illness happens to you because it is your turn. | 35.5 (11) | 19.4 (6) | 16.1 (5) | 29 (9) | 0.618 |
References
- Jonsson, R.; Brokstad, K.A.; Jonsson, M.V.; Delaleu, N.; Skarstein, K. Current Concepts on Sjögren’s Syndrome—Classification Criteria and Biomarkers. Eur. J. Oral Sci. 2018, 126, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Narváez, J.; Sánchez-Fernández, S.Á.; Seoane-Mato, D.; Díaz-González, F.; Bustabad, S. Prevalence of Sjögren’s Syndrome in the General Adult Population in Spain: Estimating the Proportion of Undiagnosed Cases. Sci. Rep. 2020, 10, 10627. [Google Scholar] [CrossRef] [PubMed]
- Qin, B.; Wang, J.; Yang, Z.; Yang, M.; Ma, N.; Huang, F.; Zhong, R. Epidemiology of Primary Sjögren’s Syndrome: A Systematic Review and Meta-Analysis. Ann. Rheum. Dis. 2015, 74, 1983–1989. [Google Scholar] [CrossRef]
- Vivino, F.B. Sjogren’s Syndrome: Clinical Aspects. Clin. Immunol. 2017, 182, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Leone, M.C.; Alunno, A.; Cafaro, G.; Valentini, V.; Marcucci, E.; Bartoloni, E.; Gerli, R. The Clinical Spectrum of Primary Sjögren’s Syndrome: Beyond Exocrine Glands. Reumatismo 2017, 69, 93–100. [Google Scholar] [CrossRef]
- Cui, Y.; Xia, L.; Li, L.; Zhao, Q.; Chen, S.; Gu, Z. Anxiety and Depression in Primary Sjögren’s Syndrome: A Cross-Sectional Study. BMC Psychiatry 2018, 18, 131. [Google Scholar] [CrossRef]
- Milic, V.; Grujic, M.; Barisic, J.; Marinkovic-Eric, J.; Duisin, D.; Cirkovic, A.; Damjanov, N. Personality, Depression and Anxiety in Primary Sjogren’s Syndrome—Association with Sociodemographic Factors and Comorbidity. PLoS ONE 2019, 14, e0210466. [Google Scholar] [CrossRef]
- Hays, R.D.; Reeve, B.B. Measurement and Modeling of Health-Related Quality of Life. In International Encyclopedia of Public Health; Heggenhougen, H.K., Ed.; Academic Press: Oxford, UK, 2008; pp. 241–252. ISBN 978-0-12-373960-5. [Google Scholar]
- Ngo, D.Y.J.; Thomson, W.M.; Nolan, A.; Ferguson, S. The Lived Experience of Sjögren’s Syndrome. BMC Oral Health 2016, 16, 7. [Google Scholar] [CrossRef]
- Herrera, A.; Sánchez, G.; Espinoza, I.; Wurmann, P.; Bustos, C.; Leiva, L.; Geenen, R.; Rojas-Alcayaga, G. Illness Experiences of Chilean Women with Sjögren’s Syndrome: The Patient Perspective. Arthritis Care Res. 2021, 73, 1210–1218. [Google Scholar] [CrossRef]
- Vitali, C.; Bombardieri, S.; Jonsson, R.; Moutsopoulos, H.M.; Alexander, E.L.; Carsons, S.E.; Daniels, T.E.; Fox, P.C.; Fox, R.I.; Kassan, S.S.; et al. Classification Criteria for Sjögren’s Syndrome: A Revised Version of the European Criteria Proposed by the American-European Consensus Group. Ann. Rheum. Dis. 2002, 61, 554–558. [Google Scholar] [CrossRef]
- Olivares-Tirado, P. Calidad de Vida Relacionada a La Salud (HR-QoL) En Población General de Chile Chile; Departamento de Estudios y Desarrollo, Superintendencia de Salud, Gobierno de Chile: Santiago, Chile, 2010. [Google Scholar]
- León, S.; Bravo-Cavicchioli, D.; Correa-Beltrán, G.; Giacaman, R.A. Validation of the Spanish Version of the Oral Health Impact Profile (OHIP-14Sp) in Elderly Chileans. BMC Oral Health 2014, 14, 95. [Google Scholar] [CrossRef] [PubMed]
- Van Reenen, M.; Janssen, B. EQ-5D-5L User Guide: Basic Information on How to Use the EQ-5D-5L Instrument. Rotterdam EuroQol Res. Found. 2015, 9. [Google Scholar]
- Slade, G.D. Derivation and Validation of a Short-Form Oral Health Impact Profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- Broom, A. Virtually He@lthy: The Impact of Internet Use on Disease Experience and the Doctor-Patient Relationship. Qual. Health Res. 2005, 15, 325–345. [Google Scholar] [CrossRef]
- Iverson, S.A.; Howard, K.B.; Penney, B.K. Impact of Internet Use on Health-Related Behaviors and the Patient-Physician Relationship: A Survey-Based Study and Review. J. Am. Osteopath. Assoc. 2008, 108, 699–711. [Google Scholar]
- Anderson, J.G.; Rainey, M.R.; Eysenbach, G. The Impact of CyberHealthcare on the Physician-Patient Relationship. J. Med. Syst. 2003, 27, 67–84. [Google Scholar] [CrossRef]
- Murray, E.; Lo, B.; Pollack, L.; Donelan, K.; Catania, J.; White, M.; Zapert, K.; Turner, R. The Impact of Health Information on the Internet on the Physician-Patient Relationship: Patient Perceptions. Arch. Intern. Med. 2003, 163, 1727–1734. [Google Scholar] [CrossRef]
- Nwosu, C.R.; Cox, B.M. The Impact of the Internet on the Doctor-Patient Relationship. Health Inform. J. 2000, 6, 156–161. [Google Scholar] [CrossRef]
- Laugesen, J.; Hassanein, K.; Yuan, Y. The Impact of Internet Health Information on Patient Compliance: A Research Model and an Empirical Study. J. Med. Internet Res. 2015, 17, e143. [Google Scholar] [CrossRef]
- Lackner, A.; Ficjan, A.; Stradner, M.H.; Hermann, J.; Unger, J.; Stamm, T.; Stummvoll, G.; Dür, M.; Graninger, W.B.; Dejaco, C. It’s More than Dryness and Fatigue: The Patient Perspective on Health-Related Quality of Life in Primary Sjögren’s Syndrome—A Qualitative Study. PLoS ONE 2017, 12, e0172056. [Google Scholar] [CrossRef]
- Koh, J.H.; Kwok, S.K.; Lee, J.; Son, C.N.; Kim, J.-M.; Kim, H.O.; Park, S.H.; Sung, Y.K.; Choe, J.Y.; Lee, S.S.; et al. Pain, Xerostomia, and Younger Age Are Major Determinants of Fatigue in Korean Patients with Primary Sjögren’s Syndrome: A Cohort Study. Scand. J. Rheumatol. 2017, 46, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Theander, E.; Andersson, S.I.; Manthorpe, R.; Jacobsson, L.T.H. Proposed Core Set of Outcome Measures in Patients with Primary Sjögren’s Syndrome: 5 Year Follow Up. J. Rheumatol. 2005, 32, 1495–1502. [Google Scholar]
- Mertzanis, P.; Abetz, L.; Rajagopalan, K.; Espindle, D.; Chalmers, R.; Snyder, C.; Caffery, B.; Edrington, T.; Simpson, T.; Nelson, J.D.; et al. The Relative Burden of Dry Eye in Patients’ Lives: Comparisons to a U.S. Normative Sample. Investig. Ophthalmol. Vis. Sci. 2005, 46, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Priori, R.; Minniti, A.; Derme, M.; Antonazzo, B.; Brancatisano, F.; Ghirini, S.; Valesini, G.; Framarino-dei-Malatesta, M. Quality of Sexual Life in Women with Primary Sjögren Syndrome. J. Rheumatol. 2015, 42, 1427–1431. [Google Scholar] [CrossRef] [PubMed]
- van Nimwegen, J.F.; Arends, S.; van Zuiden, G.S.; Vissink, A.; Kroese, F.G.M.; Bootsma, H. The Impact of Primary Sjögren’s Syndrome on Female Sexual Function. Rheumatology 2015, 54, 1286–1293. [Google Scholar] [CrossRef] [PubMed]
- Koçer, B.; Tezcan, M.E.; Batur, H.Z.; Haznedaroğlu, Ş.; Göker, B.; İrkeç, C.; Çetinkaya, R. Cognition, Depression, Fatigue, and Quality of Life in Primary Sjögren’s Syndrome: Correlations. Brain Behav. 2016, 6, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Dong, Z.; Liang, X.; Liu, J.; Xuan, L.; Wang, J.; Zhang, G.; Hao, W. Health-Related Quality of Life and Psychological Status of Women with Primary Sjögren’s Syndrome. Medicine 2017, 96, e9208. [Google Scholar] [CrossRef]
- Hyphantis, T.; Mantis, D.; Voulgari, P.V.; Tsifetaki, N.; Drosos, A.A. The Psychological Defensive Profile of Primary Sjögren’s Syndrome Patients and Its Relationship to Health-Related Quality of Life. Clin. Exp. Rheumatol. 2011, 29, 485–493. [Google Scholar]
- Miyamoto, S.T.; Valim, V.; Fisher, B.A. Health-Related Quality of Life and Costs in Sjögren’s Syndrome. Rheumatology 2019, 60, 2588–2601. [Google Scholar] [CrossRef]
- Lendrem, D.; Mitchell, S.; McMeekin, P.; Gompels, L.; Hackett, K.; Bowman, S.; Price, E.; Pease, C.T.; Emery, P.; Andrews, J.; et al. Do the EULAR Sjögren’s Syndrome Outcome Measures Correlate with Health Status in Primary Sjögren’s Syndrome? Rheumatology 2015, 54, 655–659. [Google Scholar] [CrossRef]
- Azuma, N.; Katada, Y.; Kitano, S.; Sekiguchi, M.; Kitano, M.; Nishioka, A.; Hashimoto, N.; Matsui, K.; Iwasaki, T.; Sano, H. Correlation between Salivary Epidermal Growth Factor Levels and Refractory Intraoral Manifestations in Patients with Sjögren’s Syndrome. Mod. Rheumatol 2014, 24, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.M.; Berg, K.M.; Cha, S.; Reeves, W.H. Salivary Dysfunction and Quality of Life in Sjögren Syndrome: A Critical Oral-Systemic Connection. J. Am. Dent. Assoc. 2008, 139, 291–299; quiz 358–359. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Patschan, S.; Patschan, D.; Ziebolz, D. Oral-Health-Related Quality of Life in Adult Patients with Rheumatic Diseases—A Systematic Review. J. Clin. Med. 2020, 9, 1172. [Google Scholar] [CrossRef] [PubMed]
- Napeñas, J.J.; Rouleau, T.S. Oral Complications of Sjögren’s Syndrome. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 55–62. [Google Scholar] [CrossRef]
- Castro, M.F.; López-Pintor, R.M.; Serrano, J.; Ramírez, L.; Sanz, M.; Andreu, J.L.; Fernández, S.M.; Vallejo, G.H.; Blázquez, M.Á.; Bohórquez, C. Evaluación Protocolizada Odontológica En El Paciente Con Síndrome de Sjögren Primario. Proyecto EPOX-SSp: Metodología y Objetivos. Reumatol. Clínica 2021, 17, 25–31. [Google Scholar] [CrossRef]
- Amaral, J.; Sanches, C.; Marques, D.; Vaz Patto, J.; Barcelos, F.; Mata, A. Validation of Oral Health Impact Profile-14 and Its Association with Hypossialia in a Sjögren Syndrome Portuguese Population. Acta Reum. Port. 2018, 43, 137–145. [Google Scholar]
| Characteristic (n = 31) | Mean (SD), Range or Number and Percentage (%) |
|---|---|
| Age in years | 43.5 (13.38), range = 21–68 |
| Age of onset of the first symptoms | 34.8 (12.06), range = 17–59 |
| Age of diagnosis | 38.5 (11.44), range = 20–60 |
| Symptom duration before Diagnosis | 3.2 (3.91), range = 0–11 |
| Marital status | |
| Married or cohabiting | 13 (41.9) |
| Divorced | 6 (19.4) |
| Widowed | 2 (6.5) |
| Single | 10 (32.3) |
| Highest level of completed education | |
| Incomplete secondary education | 4 (12.9) |
| Complete secondary education | 7 (22.6) |
| Incomplete university education | 2 (6.5) |
| Complete university education | 14 (45.2) |
| Postgraduate | 4 (12.9) |
| Self-report of symptoms | |
| Eye dryness | 23 (74.2) |
| Oral dryness | 23 (74.2) |
| Muscle/Joint pain | 16 (51.6) |
| Fatigue | 9 (29.0) |
| Parotiditis | 6 (19.4) |
| Vaginal dryness | 5 (16.1) |
| Dry skin | 4 (12.9) |
| Respiratory problems | 3 (9.8) |
| Eye problems | 3 (9.8) |
| Dry nose | 3 (9.8) |
| Dental problems | 2 (6.5) |
| Dysphagia | 1 (3.2) |
| Dimension | Item | n (%) |
|---|---|---|
| Mobility | I have no problems walking about | 15 (48.4) |
| I have slight problems walking about | 9 (29.0) | |
| I have moderate problems walking about | 6 (19.4) | |
| I have severe problems walking about | 1 (3.2) | |
| I am unable to walk about | 0 | |
| Self-care | I have no problems washing or dressing myself | 22 (71.0) |
| I have slight problems washing or dressing myself | 6 (19.4) | |
| I have moderate problems washing or dressing myself | 3 (9.7) | |
| I have severe problems washing or dressing myself | 0 | |
| I am unable to wash or dress myself | 0 | |
| Usual activities | I have no problems doing my usual activities | 12 (38.7) |
| I have slight problems doing my usual activities | 9 (29.0) | |
| I have moderate problems doing my usual activities | 6 (19.4) | |
| I have severe problems doing my usual activities | 2 (6.5) | |
| I am unable to do my usual activities | 2 (6.5) | |
| Pain/discomfort | I have no pain or discomfort | 4 (12.9) |
| I have slight pain or discomfort | 8 (25.8) | |
| I have moderate pain or discomfort | 15 (48.4) | |
| I have severe pain or discomfort | 3 (9.7) | |
| I have extreme pain or discomfort | 1 (3.2) | |
| Anxiety/depression | I am not anxious or depressed | 14 (45.2) |
| I am slightly anxious or depressed | 7 (22.6) | |
| I am moderately anxious or depressed | 6 (19.4) | |
| I am severely anxious or depressed | 3 (9.7) | |
| I am extremely anxious or depressed | 1 (3.2) |
| EQ-5D-5L Dimensions | Correlation Coefficient | p Value |
|---|---|---|
| Mobility | −0.507 | 0.004 1 |
| Self-care | −0.311 | 0.088 |
| Usual activities | −0.691 | <0.05 1 |
| Pain/discomfort | −0.589 | <0.05 1 |
| Anxiety/depression | −0.347 | 0.056 |
| OHIP-14sp Dimensions | Average | Standard Deviation | 95% CI |
|---|---|---|---|
| Functional limitation | 3.12 | 1.65 | 2.54–3.73 |
| Physical Pain | 4.45 | 2.42 | 3.56–5.34 |
| Psychological discomfort | 3.55 | 2.79 | 2.52–4.57 |
| Physical disability | 2.04 | 2.47 | 1.19–3.00 |
| Psychological disability | 3.22 | 2.22 | 2.41–4.03 |
| Social disability | 2.19 | 2.56 | 1.25–3.13 |
| Handicap | 1.48 | 2.42 | 0.60–2.37 |
| OHIP-14Sp | Correlation Coefficient | p Value |
|---|---|---|
| Score sum | −0.343 | 0.059 |
| Dimensions | ||
| Functional limitation | −0.361 | 0.046 1 |
| Physical pain | −0.171 | 0.357 |
| Psychological discomfort | −0.224 | 0.225 |
| Physical disability | −0.19 | 0.305 |
| Psychological disability | −0.415 | 0.02 1 |
| Social disability | −0.27 | 0.142 |
| Handicap | −0.194 | 0.296 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojas-Alcayaga, G.; Herrera, A.; Espinoza, I.; Rios-Erazo, M.; Aguilar, J.; Leiva, L.; Shakhtur, N.; Wurmann, P.; Geenen, R. Illness Experience and Quality of Life in Sjögren Syndrome Patients. Int. J. Environ. Res. Public Health 2022, 19, 10969. https://doi.org/10.3390/ijerph191710969
Rojas-Alcayaga G, Herrera A, Espinoza I, Rios-Erazo M, Aguilar J, Leiva L, Shakhtur N, Wurmann P, Geenen R. Illness Experience and Quality of Life in Sjögren Syndrome Patients. International Journal of Environmental Research and Public Health. 2022; 19(17):10969. https://doi.org/10.3390/ijerph191710969
Chicago/Turabian StyleRojas-Alcayaga, Gonzalo, Andrea Herrera, Iris Espinoza, Matías Rios-Erazo, Jacqueline Aguilar, Loreto Leiva, Nailah Shakhtur, Pamela Wurmann, and Rinie Geenen. 2022. "Illness Experience and Quality of Life in Sjögren Syndrome Patients" International Journal of Environmental Research and Public Health 19, no. 17: 10969. https://doi.org/10.3390/ijerph191710969
APA StyleRojas-Alcayaga, G., Herrera, A., Espinoza, I., Rios-Erazo, M., Aguilar, J., Leiva, L., Shakhtur, N., Wurmann, P., & Geenen, R. (2022). Illness Experience and Quality of Life in Sjögren Syndrome Patients. International Journal of Environmental Research and Public Health, 19(17), 10969. https://doi.org/10.3390/ijerph191710969






