The Effectiveness of Pharmacist Interventions in the Management of Patient with Renal Failure: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
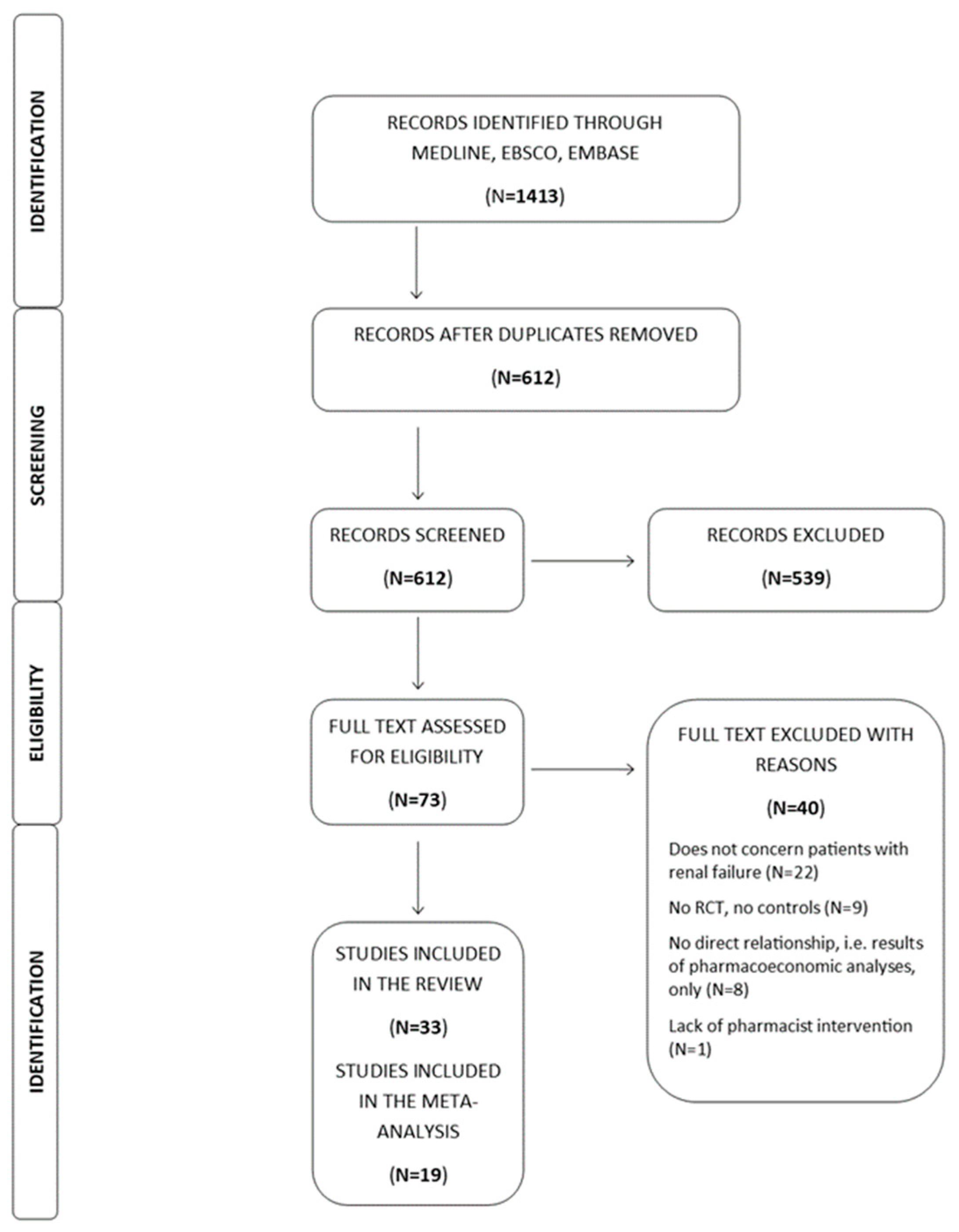
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction and Quality Assessment
2.4. Data Analysis
2.5. Outcomes
3. Results
3.1. Search Results and Description of Included Studies
3.2. Quality Assessment of Included Studies
3.2.1. Bias Arising from the Randomization Process
3.2.2. Bias Due to Deviations from the Intended Interventions
3.2.3. Bias Due to Missing Outcome Data
3.2.4. Bias in Measurement of the Outcome
3.2.5. Bias in Selection of the Reported Result
3.3. Study Characteristics
| Source/ Location | Study Type, Sample Size ¥, Follow up (Months) | Participants (Baseline Percentage of Patients with Renal Failure ¥) | Comorbidities | Key Components of Pharmacist Intervention | Measured Outcomes (Intervention vs. Usual Care) |
|---|---|---|---|---|---|
| Anderegg MD et al. 2018 [12] USA | Cluster RCT 227/108 9 | HTN (12.3/13.9%) | Arthritis, asthma/COPD, CAD, CKD, depression/anxiety, DM, Dys, HF, PVD, stroke/TIA | Pharmacists conducted MRs and assessed patient knowledge of BP medications, goals of therapy, medication dosages, potential side effects, contraindications, and monitoring; then created an individualized care plan with BP goal and medicine recommendations (1). | primary: SBP reduction at 9th month from baseline (8.64 mmHg; 95% CI −12.8–(−4.49); p < 0.001) #; BP control by the JNC−7 or JNC−8 inclusion (OR = 1.97; 95% CI 1.01−3.86; p = 0.047) or (OR = 2.16; 95% CI 1.21−3.85; p = 0.0102) |
| Carter BL et al. 2015 [13] USA | Cluster RCT 401/224 9 | HTN (47.4/54.0% *; 47.3/54.0% **) | CKD (3a–5) or DM | Pharmacist conducted MRs. The model recommended a telephone calls, structured face−to−face visits, and additional visits if BP remained uncontrolled. Dose adjustments (1). | primary: BP control at 9th month (OR = 1.57; 95% CI 0.99–2.50; p = 0.059); secondary: BP control at 12th, 18th and 24th month |
| Magid DJ et al. 2013 [14] USA | RCT 162/164 6 | HTN (46.3/50.9%) ^ | CKD (1–3b) or DM | Pharmacist conducted home BP telemonitoring, and reviewed current BP medication regimen, provided counselling on lifestyle changes, educational materials, and adjusted or changed antihypertensive medications as needed, including dosage (1). | primary: the proportion of patients who attained goal BP (<130/80 mmHg for CKD) at 6th month (adjusted OR = 3.84; 95% CI 2.08–7.10; p < 0.0001); secondary: change at 6th month from baseline in SBP (−15.4 mmHg; 95% CI; −21.0–(−9.8); p < 0.0001) and DBP (−7.3 mmHg; −10.4–(−4.1); p < 0.0001); change in antihypertensive medication intensity (70% vs. 25%; p < 0.001); hospitalizations (OR = 0.70; 95% CI 0.22–2.24; p > 0.05); change in medication intensity score (1.35 ± 1.37 vs. 0.15 ± 0.82; p < 0.001); medication usage: CCB (OR = 2.61; 95% CI 1.6−4.18; p < 0.0001); ACEI/ARB (OR = 1.59; 95% CI 0.98−2.58; p = 0.06); diuretic (OR = 8.80; 95% CI 4.66−16.61; p < 0.001) at 6th month. |
| Margolis KL et al. 2013 [15] USA | RCT 188/182 18 | HTN (17.1/14.6%) | CKD (3a–5), DM, obesity | Pharmacist conducted home BP telemonitoring, and reviewed the patient’s relevant history, instructed patients on BP telemonitor system and the individualized home BP goal using the home (1). | primary: BP control to <130/80 mmHg in patients with diabetes or kidney disease) at 6th (27.2%; 95% CI 13.4–40.0; p < 0.001) and 12th month (29.6%; 95% CI 13.1–46.0; p < 0.002); secondary: change in SBP (−10.70 mmHg; 95% CI −14.90–(7.31); p < 0.0001) #; change in DBP (−6.00 mmHg; 95% CI −8.61–(−3.39); p < 0.0001) #; patient satisfaction (0.15; 95% CI 0.03–0.28; p = 0.014) # at 18th month from baseline, BP control (14.7%; 95% CI 7.0–21.4; p < 0.003); medication adherence (OR = 1.50; 95% CI 0.98–2.31; p = 0.064) at 18th month; change in HRQoL–SF-12 physical function (0.28; 95% CI 0.15−0.41; p = 0.0001) #; SF-12 mental function (1.01; 95% CI 0.85−1.17; p < 0.0001) #; % of smoked in last 30 days (−2.0; 95% CI −2.44–(−1.56); p < 0.0001) # at 18th month from baseline. |
| Al Hamarneh YN et al. 2017 [16] Canada | RCT 286/287 3 | DM and at least 1 uncontrolled risk factor (40.9/42.2%) | AF, CAD, CKD (3–5), Dys, HF, HTN, MI, PVD, stroke/TIA | MTM: pharmacist assessed patient BP, waist circumference, weight and height measurements, A1C level, lipid profile, kidney function and status, individualized CV risk; provided treatment recommendations, prescription adaptations and/or initiation (1). | primary: change in estimated CV risk from baseline to 3 months after randomization (5.38; 95% CI 4.24−6.52; p < 0.001) #; secondary: differences in changes in medication use and dose changes |
| Al Hamarneh YN et al. 2018 [17] Canada | RCT 147/143 3–6 | CKD, stage 3a–5 (100%) | AF, CAD, DM, Dys, HF, HTN, MI, PVD, stroke/TIA | MTM: pharmacist assessed patient BP, waist circumference, weight and height measurements, A1C level, lipid profile, kidney function and status, individualized CV risk; provided treatment recommendations, prescription adaptations and/or initiation (1). | primary: change in estimated CV risk (5.03; 95% CI 3.4−6.65; p < 0.001) #; secondary: change in LDL (0.2 mmol/L; 95% CI 0.1−0.4; p = 0.004) #; HbA1c (0.7; 95% CI 0.4−0.9%; p < 0.001) #; tobacco cessation (19.6%; p = 0.04) and SBP (10.50 mmHg; 95% CI 7.40−13.50; p < 0.0001) # from baseline to 3 months |
| Chang AR et al. 2016 [18] USA | Cluster RCT 24/23 12 | CKD, stage 3a (100.0%) | CAD, DM, dys, HF, HTN | MTM: pharmacist conducted MRs, ordered lipid and ACR screening tests, and managed BP and lipid therapy. Patients were contacted by telephone and were scheduled for clinic visits with the pharmacist for medication initiation and/or titration (1). | primary: screening for proteinuria by urine ACR or protein/creatinine ratio at 24th month (OR = 2.6; 95% CI 0.5– 4.0; p > 0.05); secondary: BP control (OR = 0.9; 95% CI 0.3–3.0; p > 0.05); the proportion of patients who were on statins (OR = 0.4; 95% CI 0.12–1.3; p > 0.05) |
| Cooney D et al. 2015 [19] USA | RCT 441/429 12 | CKD, stage 3 (100.0%) | CAD, DM, HF, HTN | Multifactorial intervention: a phone−based pharmacist intervention, pharmacist−physician collaboration, patient education (informational pamphlet), and a CKD registry (1). | primary: BP control in subjects with poorly controlled hypertension at baseline (OR = 1.03; 95% CI 0.79−1.35; p > 0.05); measurement of PTH during the study (46.9% vs. 16.1%; p < 0.001); secondary: number of classes of antihypertensive drugs being prescribed (p = 0.02); change in HRQoL (52.0 ± 10.6 vs. 52.1 ± 9.6: p > 0.05); mortality (RR = 1.40; 95% CI 0.99−1.99; p = 0.06); medication adherence (6.8 ± 1.2 vs. 6.7 ± 1.2; p > 0.05). |
| Peralta CA et al. 2020 [20] USA | RCT 616/604 14 | CKD, stage 3a–5 (100.0%) | CAD, CVD, COPD, HF, Dys, malignancy, mental health disorders | An electronic letter to the primary care provider included an opt−in option to refer persons with newly detected CKD to a clinical pharmacist for MRs, drug adjustment, CKD education and counselling (1). | primary: change in SBP (−1.00 mmHg; 95% CI −1.69–(−0.31); p < 0.05) #; DBP (−1.00 mmHg; 95% CI −1.35–(−0.65); p < 0.05) # at 14th month from baseline; secondary: controlled BP at 14th month (62% vs. 64%; p > 0.05); medication usage: ACE/ARB (OR = 1.11; 95% CI 0.88−1.43; p > 0.05); diuretics (OR = 0.97; 95% CI 0.75−1.26; p > 0.05); statins (OR = 0.83; 95% CI 0.54−1.26; p > 0.05); NSAIDs (OR = 0.99; 95% CI 0.76−1.29; p > 0.05). |
| Peralta CA et al. 2020 [21] USA | Cluster RCT 171/188 12 | CKD, stage 3 (41.5/52.1%) | CAD, CVD, HF, DM, HTN, Dys | Pharmacist scheduled a follow−up visit by telephone in order to reinforce medication changes proposed by PCP, consulted patients about CKD and conducted MRs (1). | primary: change in SBP (−1.10 mmHg; 95% CI −6.69–4.49; p > 0.05); DBP (−0.40 mmHg; 95% CI −6.63–5.83; p > 0.05) at 12th month from baseline; secondary: controlled BP at 12th month (OR = 1.02; 95% CI 0.67–1.55; p > 0.05); PCP awareness of CKD at study end (OR = 2.57; 95% CI 1.46–4.54; p = 0.001); medication usage: ACEI/ARB (OR = 0.77; 95% CI 0.50−1.16; p > 0.05); diuretics (OR = 0.69; 95% CI 0.42−1.15; p > 0.05) |
| Santschi V et al. 2011 [22] Canada | Cluster RCT 48/41 6 | CKD, stage 3a–5 (100.0%) | CV, DM, Dys, HTN | ProFiL: patients’ clinical pharmacist summaries were sent to the community pharmacists to facilitate the detection of DRPs (list of patients’ health problems, eGFRs and medications). Community pharmacists could consult a nephrology pharmacist, when needed. Patient education (2). | Adjusted mean SBP (−11.60 mmHg; 95% CI −21.30–(−1.90)); p = 0.019) # and DBP changes (−2.60 mmHg; 95% CI −8.11–2.91; p > 0.05) # at 6th month from baseline. Patients with written recommendations had a greater decrease in mean systolic BP (−11.6 mmHg; p = 0.035), and BP was controlled in a higher proportion of them (RR = 2.14; p = 0.011); medication usage: diuretic (OR = 1.41; 95% CI 0.76–2.63; p > 0.05); ACEI/ARB (OR = 1.39; 95% CI 0.75–2.57; p > 0.05); CCB (OR = 1.38; 95% CI 0.71–2.65; p > 0.05). |
| Cypes IN et al. 2021 [23] USA | RCT 95/87 3 | CKD, stage 2–5 (70.5/64.4%) | Pharmacist conducted medication recommendations in order to identify and resolve medication-dosing errors and improve collaboration: providers–pharmacists (1). | primary: the number of medications requiring pharmacist intervention (22.1 vs. 19.5%); incorrect CKD staging (48.4% vs. 55.2%); rate of provider response to pharmacist−initiated medication recommendations (p > 0.05) | |
| Lalonde L et al. 2017 [24] Canada | Cluster RCT 304/138 12 | CKD, stage 2–5 (100.0%) | Anemia, CAD, DM, Dys, HTN | Pharmacists received interactive web−training program, a clinical pharmacist guide (a booklet on CKD drug therapy), a clinical pharmacist summary of their patients with information on their kidney function, and a consultation service with pharmacists working in a CKD clinic (2). | Change in DRPs per patient (−0.32; 95% CI −0.60 –(−0.0063); p = 0.04) #; improvements in knowledge (4.5%; 95% CI 1.6–7.4; p = 0.0024) and clinical competencies (7.4%; 95% CI 3.5–11.3; p = 0.0002) #; uncontrolled BP (−0.20 mmHg; 95% CI −0.41–0.10; p > 0.05) #; non−optimal adherence to drug therapy (−0.14; 95% CI −0.48–0.20; p > 0.005) #; drugs requiring dose adjustment in CKD (−0.03; 95% CI −0.12–0.06; p > 0.05) #; eGFR (2.5 mL/min 1.73 m2; 95% CI −1.8–6.7; p > 0.05) #; SBP (−1.2 mmHg; 95% CI −4.8–2.5; p > 0.05) #; DBP (0.01 mmHg; 95% CI −1.95–1.97; p > 0.05) #; LDL−C (20.1; 95% CI 20.2–0.1; p > 0.05) #; HbA1c (0.1%; 95% CI −0.2–0.1; p > 0.05) # 12th month from baseline |
| Quintana−Bárcena p et al. 2018 [25] Canada | Cluster RCT 304/137 12 | CKD, stage 2–5 (99.6/99.5%) | CAD, DM, Dys, HTN | ProFiL: patients’ clinical pharmacist summaries were sent to the community pharmacists for detection of DRPs (list of patients’ health problems, eGFRs and drugs). Community pharmacists could consult a nephrology pharmacist. Patient education (2). | The prevalence of DRPs per patient–mild (0.55 ± 0.98) and moderate (1.04 ± 1.51). An unadjusted change in moderate DRPs (0.32; 95% CI =−0.6–(−0.06); p < 0.05) # at 12th month from baseline. |
| Song YK et al. 2021 [26] South Korea | RCT 50/50 3 | CKD, stage 2–5; dialysis (100.0%) | Anemia, DM, Dys, HTN, mineral bone dis, hyperuricemia | DrugTEAM: pharmacists provided MRs, communicated with healthcare professionals, patients. Drugs were documented at discharge and the patient were counselled using educational materials (1). | primary: the number of DRPs per patient at discharge (0.9 ± 1.0 vs. 2.0 ± 1.3; p < 0.001); patients with any DRPs at discharge (OR = 0.14; 95% CI 0.04−0.046; p = 0.001); secondary: patients with increased MMAS score (OR = 2.46; 95% CI 0.96−6.27; p = 0.06) |
| Thanapongsatorn P et al. 2021 [27] Thailand | RCT 40/38 12 | AKI, CKD stage 2–3 (100.0%) | CAD, CVD, CKD, DM, HF, HTN, liver disease, malignancy | Multidisciplinary care team consisted of nephrologists, renal nurses, renal pharmacists, and nutritionists. Renal pharmacist conducted the drug reconciliation, alerted the nephrologists, dealt with dosing errors, drug interactions, or nephrotoxins, provided medication education and adjustment of the medication dosage based on the renal function (1). | primary: feasibility outcomes: rate of 3−d dietary record (100.0% vs. 0.0%; p < 0.0001), rate of drug reconciliation (100.0% vs. 0.0%; p < 0.0001), and rate of drug alerts (30.0% vs. 0.0%; p < 0.0001); secondary: eGFR at 12 months (66.74 ± 30.77 vs. 61.23 ± 35.16 mL/min 1.73 m2; p > 0.05); urine albumin: creatinine ratio (UACR) (36.83 mg/g; 95% CI 13.39−131.90 vs. 177.70 mg/g; 95% CI 47.12−745.71; p = 0.036); BP control (OR = 5.34; 95% CI 1.53−18.70; p = 0.0088); CKD progression (OR = 0.48; 95% CI 1.0.08−2.81; p > 0.05); mortality (RR = 1.28; 95% CI 0.44–3.74; p > 0.05); medication usage: ACEI/ARB use (OR = 1.37; 95% CI 0.51−3.70; p > 0.05) at 12th month |
| Theeranut A et al. 2021 [28] Thailand | RCT 166/168 3 | CKD, stage 2−3b (100.0%) | CAD, DM, Dys, gout, HTN | Chumpae model for delaying dialysis in CKD patients. The clinical pharmacist information system provided updated, systematic clinical pharmacist evidence for the patients and care team (1). | primary: change in eGFR (7.61 mL/min 1.73m2; 95% CI 5.83−9.39) # at 3th month from baseline; proportion of patients with eGFR decline greater than 4 mL/min/1.73 m2 (OR = 0.17; 95% CI 0.1−0.28; p < 0.001); difference in CKD stage from baseline (p < 0.001) |
| Tuttle KR et al. 2018 [29] USA | RCT 66/63 3 | CKD, stage 2–5 (92.7/97.2%) | DM, HTN | Pharmacist conducted MRs, taken medication action plan and personal medication list, within in−home visits 7 days after hospital discharge. The intervention was augmented by the Chronic Care Model and on the basis of an algorithm for the “5As” (Assessment, Advice, Agreement, Assistance, and Arrangements) process, including medication doses adjustment for kidney function (1). | primary: a composite of first acute care events (hospitalization and emergency department) within the 90−day period after index hospitalization (OR = 1.17; 95% CI 0.60–2.29; p > 0.05); secondary: hospitalization (OR = 1.02; 95% CI 0.48–2.15; p > 0.05); eGFR (0.01 mL/min 1.73 m2; 95% CI −0.96–0.96; p > 0.05) #; SBP (−1.00 mmHg; 95% CI −2.36–0.36; p > 0.05) #; DBP (1.99 mmHg; 95% CI; 1.21–2.77; p < 0.05) #; BP goal < 130/80 mmHg (OR = 1.33; 95% CI 0.65–2.73; p > 0.05); BP goal < 140/90 mmHg (OR = 1.19; 95% CI 0.55–2.59; p > 0.05); hemoglobin (0.01 g/dL; 95% CI −0.66–0.66; p > 0.05) #; HbA1c (−0.2%; 95% CI −0.27–(−0.13); p < 0.0001) # at 3rd month from baseline |
| Wilson FP et al. 2015 [30] USA | RCT 1201/1192 1 | AKI (100.0%) CKD (27/26%) | CVD, CKD (1–3b), DM, HF, metastatic disease | Automated, electronic alerts for AKI received by an intern, resident, or nurse practitioner and unit pharmacist (1). | primary: composite of relative maximum change in creatinine, dialysis, and death at 7 days after randomization (p > 0.05); median relative change in creatinine concentrations (0.0; IQR 0.0–18.4; vs. 0.6; IQR 0.0–17.5%; p > 0.05); rate of dialysis (OR = 1.25; 95% CI 0.90–1.74; p > 0.05); rate of death (OR = 1.16; 95% CI 0.81–1.68; p > 0.05). |
| Dashti–Khavidaki S et al. 2013 [31] Iran | Cluster RCT 34/26 6 | Hemodialysis (100.0%) | DM, HTN | Pharmacist provided nutrition consultation and motivational interviewing to patients, evaluated medication adherence and DRPs, educated about the disease, medications, lifestyle modification. Dose adjustment (1). | primary: difference in median HRQoL at the initiation and at the end of 6-month study (56.9; IQR 37.7–71.7 vs. 72.2; IQR 55.3–83.7; p = 0.001) in the intervention group; as well as in role−emotional, mental health, social functioning, and general health dimensions |
| Mateti UV et al. 2017 [32] India | RCT 78/75 12 | Hemodialysis (100.0%) | CAD, CVD, CTD, DM, hypothyroidism, HTN | Pharmacists provided patient motivation and education about drugs, disease, lifestyle modifications, and diet, performed personal interview, and MRs. Validated pictogram−based information leaflets could be used (1). | primary ¶: change in HRQoL, e.g., SF−12 physical function (11.43; 95% CI 9.59−13.26; p < 0.0001) #, ESRD–kidney function (9.12; 95% CI 3.90−14.34; p < 0.0006) # at 12th month from baseline |
| Pai AB et al. 2009 [33] USA | RCT 61/46 24 | Hemodialysis (100.0%) | DM, HTN | Nephrology−trained pharmacist conducted MRs, provided education, services optimizing drug therapy during rounds/formal reviews of the patients with the multidisciplinary health care team (1). | Total RQLP scores at year 1 (71 ± 34 vs. 88 ± 31; p = 0.03); Eating and Drinking score (4.4 ± 3.1 vs. 5.9 ± 3.3; p = 0.04); Physical Activities (30 ± 16.3 vs. 37 ± 13.6; p = 0.04); Leisure Time scores (5.9 ± 3.6 vs. 8.3 ± 3.4 p = 0.03). |
| Marouf BH et al. 2020 [34] Iraq | RCT 60/60 4 | Hemodialysis (100.0%) | DM, HTN | Pharmacist created in−hospital guidelines for proper use of recombinant human erythropoietin, provided drug information on CKD−associated anemia to physicians and nurses, performed intervention at the physician, drug, patient, and hospital level (1). | primary: change in serum hemoglobin (0.91 g/dL; 95% CI 0.79–1.01; p < 0.0001) #, transferrin saturation (5.00%; 95% CI 4.77–5.23; p < 0.0001) #; ferritin (−90.70 ng/mL; 95% CI −113.60–(−67.80); p < 0.0001) # at 4th month from baseline; secondary: change in serum vitamin B12 (91.80 ng/mL; 95% CI 85.23–98.31; p < 0.0001) # and folate (1.39 ng/mL; 95% CI 1.15–1.63; p < 0.0001) # at 4th month from baseline. |
| van den Oever FJ et al. 2020 [35] the Netherlands | RCT 65/62 13 | Intermittent, maintenance hemodialysis (100.0%) | Active malignancy, AF, CAD, HF, PVD, stroke/TIA | Pharmacist developed treatment algorithms for the dosing of DA and iron sucrose developed by pharmacist and provided dose advice (1). | primary: percentage in target range per patient for hemoglobin (6.8–7.4 mmol/L) (38.5; IQR 6.7–53.9 vs. 23.1; IQR 9.1–46.2%; p = 0.001); percentage of high hemoglobin levels (>8.1 mmol/L) (0.0; IQR 0.0–12.9 vs. 7.7; IQR 0.0–27.3%; p = 0.034); weekly dose of darbepoetin alfa (34.0; IQR 20.0–60.5 vs. 46.9; IQR 25.8–77.7 mcg; p = 0.020), iron sucrose dose (75; IQR 50–100 vs. 0.0; 0–100 mg/week; p < 0.001); mortality (RR = 0.6; 95% CI 0.34−1.03; p = 0.066). |
| Mateti UV et al. 2018 [36] India | RCT 78/75 12 | Hemodialysis (100.0%) | CAD, CVD, CTD, DM, HTN, hypothyroidism, COPD | Pharmacists provided patient motivation and education about drugs, disease, lifestyle modifications, and diet, performed personal interview, and MRs. Validated pictogram−based information leaflets could be used (1). | primary ¶: change in SBP (−6.26mmHg; 95% CI −7.49–(−5.03; p < 0.0001) #; DBP (−3.56 mmHg; 95% CI −4.19–(−2.93); p < 0.0001) #; medication adherence (1.07; 95% CI 0.94–1.20; p < 0.001) #; hemoglobin (0.35 g/dL; 95% CI 0.22–0.48); p < 0.0001) # at 12th month from baseline |
| Qudah B et al. 2016 [37] Jordan | RCT 29/27 3 | Hemodialysis (100.0%) | CV, DM, Dys | After obtaining home BP readings, pharmacist provided and discussed recommendations with the physician (acceptance or rejection). Educated and explained the goals for BP and daily weight gain (1). | primary: percentage of patients who reached weekly average home BP target of SBP < 135 mmHg and DBP < 85 mmHg (46% vs. 14.3; p = 0.02); change in average weekly home SBP (−14.40 mmHg; 95% CI −24.22–(−4.58); p = 0.004) # and DBP (−3.90 mmHg; 95% CI −10.02–2.22; p > 0.05) # at 3rd month from baseline |
| Pai AB et al. 2009 [38] USA | RCT 57/47 3 | Hemodialysis (100.0%) | DM, HTN | Nephrology trained pharmacist conducted one−on−one patient interviews, generated a drug therapy profile; identified and addressed various DRPs through MRs, and provided patient education (1). | All−cause hospitalizations normalized per 1000 patient−days (1.8 ± 2.4 vs. 3.1 ± 3; p = 0.02), the cumulative time hospitalized (9.7 ± 14.7 vs. 15.5 ± 16.3 days; p = 0.06); mortality (RR = 1.03; 95% CI 0.54−1.98; p > 0.05) |
| Bessa AB et al. 2016 [39] Brazil | RCT 64/64 3 | Kidney transplant (100.0%) | Pharmacist provided a predefined instructions given from day 3 to day 90 after kidney transplantation (1). | primary: %CV for tacrolimus concentrations (31.4% ± 12.3% vs. 32.5% ± 16.1%, p > 0.05); proportion of non−adherent patients at day 28 (17% vs. 26%, p > 0.05) and day 90 (27% vs. 25%, p > 0.05) | |
| Chisholm M et al. 2011 [40] USA | RCT 12/12 12 | Kidney transplant (100.0%) | Pharmacist conducted MRs, provided recommendations to the nephrologists, counselled patients about therapy, instructed on proper drug administration (1). | primary: compliance rate for immunosuppressive therapy (96.1 ± 4.7% vs. 81.6 ± 11.5%; p < 0.001) at the end of 1st year post−transplant; duration of compliance between the groups (p < 0.05). | |
| Fleming JN et al. 2021 [41] USA | RCT 68/68 6 | Kidney transplant (100.0%) | DM, HTN | Pharmacist conducted supplemental therapy monitoring and management, utilizing a smartphone−enabled mHealth app, integrated with risk−driven televisits and home−based BP. Conducted MRs at discharge, and provide recommendations to the patient (1). | secondary: the impact of the intervention on tacrolimus intrapatient variability over 12 months after randomization (p = 0.0133) |
| Gonzales H et al. 2021 [42] USA | RCT 68/68 12 | Kidney transplant (100.0%) | Pharmacist monitored therapy via a mobile health−based application, integrated with risk−guided televisits and home−based BP and glucose measurements (1). | primary: pharmacist intervention types were medication reconciliation and patient education, followed by medication changes; secondary: 15% decrease in high−risk patients and a corresponding 15% increase in medium- or low-risk patients at 12th month from baseline | |
| Gonzales H et al. 2021 [43] USA | RCT 68/68 12 | Kidney transplant (100.0%) | Pharmacist monitored therapy via a mobile health−based application, integrated with risk−guided televisits and home−based BP and glucose measurements (1). | primary: change in medication errors (RR = 0.39; 95% CI 0.28–0.55; p < 0.001); secondary: rate of hospitalizations (RR = 0.46; 95% CI 0.27–0.77; p = 0.005) | |
| Joost R et al. 2014 [44] Germany | quasi−exp 35/32 12 | Kidney transplant (100.0%) | In addition to standard transplant training, pharmacist provided educational, behavioral and technical interventions, and consultations (transplant rejection, immunosuppressive drug actions and dosing, drug−drug interactions, common adverse effects, and adherence) (1). | primary: patient daily adherence, according to MEMS–percentage of days with the correct dosing of mycophenolate mofetil (91%, 95% CI 90.52–91.94 vs. 75%, 95% CI 74.57–76.09; p = 0.014) during the 1st year after transplantation; secondary: TA (95% ± 7.15 vs. 82% ± 20.2; p = 0.006); TiA (95% ± 7.88 vs. 94% ± 7.33; p > 0.05); PC (97% ± 7.33 vs. 90% ± 11.99; p = 0.008). |
3.4. Data Synthesis and Analysis
3.4.1. Meta-Analysis Results on Selected Clinical Outcomes and Adherence
3.4.2. Systematic Review of Other Outcomes
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nicoll, R.; Robertson, L.; Gemmell, E.; Sharma, P.; Black, C.; Marks, A. Models of care for chronic kidney disease: A systematic review. Nephrology 2018, 23, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Drawz, P.; Rahman, M. Chronic kidney disease. Ann. Intern. Med. 2015, 162, ITC1–ITC16. [Google Scholar] [CrossRef] [PubMed]
- Hazzan, A.D.; Halinski, C.; Agoritsas, S.; Fishbane, S.; DeVita, M.V. Epidemiology and Challenges to the Management of Advanced CKD. Adv. Chronic. Kidney Dis. 2016, 23, 217–221. [Google Scholar] [CrossRef]
- Ravera, M.; Noberasco, G.; Weiss, U.; Re, M.; Gallina, A.M.; Filippi, A.; Cannavò, R.; Ravera, G.; Cricelli, C.; Deferrari, G. CKD awareness and blood pressure control in the primary care hypertensive population. Am. J. Kidney Dis. 2011, 57, 71–77. [Google Scholar] [CrossRef]
- Nakanishi, M.; Mizuno, T.; Mizokami, F.; Koseki, T.; Takahashi, K.; Tsuboi, N.; Katz, M.; Lee, J.K.; Yamada, S. Impact of pharmacist intervention for blood pressure control in patients with chronic kidney disease: A meta-analysis of randomized clinical trials. J. Clin. Pharm. 2021, 46, 114–120. [Google Scholar] [CrossRef]
- Khatib, R.; Schwalm, J.D.; Yusuf, S.; Haynes, R.B.; McKee, M.; Khan, M.; Nieuwlaat, R. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: A systematic review and meta-analysis of qualitative and quantitative studies. PLoS ONE 2014, 9, e84238. [Google Scholar] [CrossRef]
- Ampofo, A.G.; Khan, E.; Ibitoye, M.B. Understanding the role of educational interventions on medication adherence in hypertension: A systematic review and meta-analysis. Heart Lung 2020, 49, 537–547. [Google Scholar] [CrossRef]
- Walters, B.A.; Hays, R.D.; Spritzer, K.L.; Fridman, M.; Carter, W.B. Health-related quality of life, depressive symptoms, anemia, and malnutrition at hemodialysis initiation. Am. J. Kidney Dis. 2002, 40, 1185–1194. [Google Scholar] [CrossRef]
- Chakraborty, S.; Ghosh, S.; Banerjea, A.; De, R.R.; Hazra, A.; Mandal, S.K. Prescribing patterns of medicines in chronic kidney disease patients on maintenance hemodialysis. Indian J. Pharmacol. 2016, 48, 586–590. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Anderegg, M.D.; Gums, T.H.; Uribe, L.; MacLaughlin, E.J.; Hoehns, J.; Bazaldua, O.V.; Ives, T.J.; Hahn, D.L.; Coffey, C.S.; Carter, B.L. Pharmacist Intervention for Blood Pressure Control in Patients with Diabetes and/or Chronic Kidney Disease. Pharmacotherapy 2018, 38, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.L.; Coffey, C.S.; Ardery, G.; Uribe, L.; Ecklund, D.; James, P.; Egan, B.; Vander Weg, M.; Chrischilles, E.; Vaughn, T. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Magid, D.J.; Olson, K.L.; Billups, S.J.; Wagner, N.M.; Lyons, E.E.; Kroner, B.A. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Margolis, K.L.; Asche, S.E.; Bergdall, A.R.; Dehmer, S.P.; Groen, S.E.; Kadrmas, H.M.; Kerby, T.J.; Klotzle, K.J.; Maciosek, M.V.; Michels, R.D.; et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: A cluster randomized clinical trial. JAMA 2013, 310, 46–56. [Google Scholar] [CrossRef]
- Al Hamarneh, Y.N.; Hemmelgarn, B.R.; Hassan, I.; Jones, C.A.; Tsuyuki, R.T. The Effectiveness of Pharmacist Interventions on Cardiovascular Risk in Adult Patients with Type 2 Diabetes: The Multicentre Randomized Controlled RxEACH Trial. Can. J. Diabetes 2017, 41, 580–586. [Google Scholar] [CrossRef]
- Al Hamarneh, Y.N.; Tsuyuki, R.T.; Jones, C.A.; Manns, B.; Tonelli, M.; Scott-Douglass, N.; Jindal, K.; Tink, W.; Hemmelgarn, B.R. Effectiveness of Pharmacist Interventions on Cardiovascular Risk in Patients with CKD: A Subgroup Analysis of the Randomized Controlled RxEACH Trial. Am. J. Kidney Dis. 2018, 71, 42–51. [Google Scholar] [CrossRef]
- Chang, A.R.; Evans, M.; Yule, C.; Bohn, L.; Young, A.; Lewis, M.; Graboski, E.; Gerdy, B.; Ehmann, W.; Brady, J.; et al. Using pharmacists to improve risk stratification and management of stage 3A chronic kidney disease: A feasibility study. BMC Nephrol. 2016, 17, 168. [Google Scholar] [CrossRef]
- Cooney, D.; Moon, H.; Liu, Y.; Miller, R.T.; Perzynski, A.; Watts, B.; Drawz, P.E. A pharmacist based intervention to improve the care of patients with CKD: A pragmatic, randomized, controlled trial. BMC Nephrol. 2015, 16, 56. [Google Scholar] [CrossRef] [PubMed]
- Peralta, C.A.; Frigaard, M.; Rolon, L.; Seal, K.; Tuot, D.; Senyak, J.; Lo, L.; Powe, N.; Scherzer, R.; Chao, S.; et al. Screening for CKD To Improve Processes of Care among Nondiabetic Veterans with Hypertension: A Pragmatic Cluster-Randomized Trial. Clin. J. Am. Soc. Nephrol. 2020, 15, 174–181. [Google Scholar] [CrossRef]
- Peralta, C.A.; Livaudais-Toman, J.; Stebbins, M.; Lo, L.; Robinson, A.; Pathak, S.; Scherzer, R.; Karliner, L.S. Electronic Decision Support for Management of CKD in Primary Care: A Pragmatic Randomized Trial. Am. J. Kidney Dis. 2020, 76, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Santschi, V.; Lord, A.; Berbiche, D.; Lamarre, D.; Corneille, L.; Prud’homme, L.; Normandeau, M.; Lalonde, M. Impact of collaborative and multidisciplinary care on management of hypertension in chronic kidney disease outpatients. J. Pharm. Health Serv. Res. 2011, 2, 79–87. [Google Scholar] [CrossRef]
- Cypes, I.N.; Prohaska, E.S.; Melton, B.L. Pharmacist impact on medication dosing and billable coding accuracy in outpatients with chronic kidney disease. J. Am. Pharm. Assoc. 2021, 61, e153–e158. [Google Scholar] [CrossRef] [PubMed]
- Lalonde, L.; Quintana-Bárcena, P.; Lord, A.; Bell, R.; Clément, V.; Daigneault, A.M.; Legris, M.È.; Letendre, S.; Mouchbahani, M.; Jouini, G.; et al. Community Pharmacist Training-and-Communication Network and Drug-Related Problems in Patients with CKD: A Multicenter, Cluster-Randomized, Controlled Trial. Am. J. Kidney Dis. 2017, 70, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Quintana-Bárcena, P.; Lord, A.; Lizotte, A.; Berbiche, D.; Lalonde, L. Prevalence and Management of Drug-Related Problems in Chronic Kidney Disease Patients by Severity Level: A Subanalysis of a Cluster Randomized Controlled Trial in Community Pharmacies. J. Manag. Care Spec. Pharm. 2018, 24, 173–181. [Google Scholar] [CrossRef]
- Song, Y.K.; Jeong, S.; Han, N.; Na, H.; Jang, H.Y.; Sohn, M.; Kim, Y.S.; Joo, K.W.; Oh, K.H.; Kim, D.K.; et al. Effectiveness of Clinical Pharmacist Service on Drug-Related Problems and Patient Outcomes for Hospitalized Patients with Chronic Kidney Disease: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 1788. [Google Scholar] [CrossRef]
- Thanapongsatorn, P.; Chaikomon, K.; Lumlertgul, N.; Yimsangyad, K.; Leewongworasingh, A.; Kulvichit, W.; Sirivongrangson, P.; Peerapornratana, S.; Chaijamorn, W.; Avihingsanon, Y.; et al. Comprehensive versus standard care in post-severe acute kidney injury survivors, a randomized controlled trial. Crit. Care 2021, 25, 322. [Google Scholar] [CrossRef]
- Theeranut, A.; Methakanjanasak, N.; Surit, P.; Srina, J.; Sirivongs, D.; Adisuksodsai, D.; Lertsinudom, S.; Sawanyawisuth, K. Can a multidisciplinary approach slow renal progression in CKD patients? Int. J. Med. Sci. 2021, 18, 1975–1979. [Google Scholar] [CrossRef]
- Tuttle, K.R.; Alicic, R.Z.; Short, R.A.; Neumiller, J.J.; Gates, B.J.; Daratha, K.B.; Barbosa-Leiker, C.; McPherson, S.M.; Chaytor, N.S.; Dieter, B.P.; et al. Medication Therapy Management after Hospitalization in CKD: A Randomized Clinical Trial. Clin. J. Am. Soc. Nephrol. 2018, 13, 231–241. [Google Scholar] [CrossRef]
- Wilson, F.P.; Shashaty, M.; Testani, J.; Aqeel, I.; Borovskiy, Y.; Ellenberg, S.S.; Feldman, H.I.; Fernandez, H.; Gitelman, Y.; Lin, J.; et al. Automated, electronic alerts for acute kidney injury: A single-blind, parallel-group, randomised controlled trial. Lancet 2015, 385, 1966–1974. [Google Scholar] [CrossRef] [Green Version]
- Dashti-Khavidaki, S.; Sharif, Z.; Khalili, H.; Badri, S.; Alimadadi, A.; Ahmadi, F.; Gatmiri, M.; Rahimzadeh, S. The use of pharmaceutical care to improve health-related quality of life in hemodialysis patients in Iran. Int. J. Clin. Pharm. 2013, 35, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Mateti, U.V.; Nagappa, A.N.; Attur, R.P.; Nagaraju, S.P.; Rangaswamy, D. Impact of pharmaceutical care on the health-related quality of life among hemodialysis patients—A multicenter randomized controlled study. Saudi J. Kidney Dis. Transpl. 2017, 28, 1293–1306. [Google Scholar] [CrossRef] [PubMed]
- Pai, A.B.; Boyd, A.; Chavez, A.; Manley, H.J. Health-related quality of life is maintained in hemodialysis patients receiving pharmaceutical care: A 2-year randomized, controlled study. Hemodial. Int. 2009, 13, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Marouf, B.H.; Yusif, I.; Najim, R. Role of Pharmacist Intervention in the Management of Anemia Associated with Chronic Kidney Diseases at the Hemodialysis Setting. J. Young Pharm. 2020, 12, 162–168. [Google Scholar] [CrossRef]
- van den Oever, F.J.; Heetman-Meijer, C.F.M.; Birnie, E.; Vasbinder, E.C.; Swart, E.L.; Schrama, Y.C. A pharmacist-managed dosing algorithm for darbepoetin alfa and iron sucrose in hemodialysis patients: A randomized, controlled trial. Pharm. Res. Perspect. 2020, 8, e00628. [Google Scholar]
- Mateti, U.V.; Nagappa, A.N.; Attur, R.P.; Nagaraju, S.P.; Rangaswamy, D. Impact of pharmaceutical care on clinical outcomes among hemodialysis patients: A multicenter randomized controlled study. Saudi J. Kidney Dis. Transpl. 2018, 29, 801–808. [Google Scholar] [CrossRef]
- Qudah, B.; Albsoul-Younes, A.; Alawa, E.; Mehyar, N. Role of clinical pharmacist in the management of blood pressure in dialysis patients. Int. J. Clin. Pharm. 2016, 38, 931–940. [Google Scholar] [CrossRef]
- Pai, A.B.; Boyd, A.; Depczynski, J.; Chavez, I.M.; Khan, N.; Manley, H. Reduced drug use and hospitalization rates in patients undergoing hemodialysis who received pharmaceutical care: A 2-year, randomized, controlled study. Pharmacotherapy 2009, 29, 1433–1440. [Google Scholar] [CrossRef]
- Bessa, A.B.; Felipe, C.R.; Hannun, P.; Sayuri, P.; Felix, M.J.; Ruppel, P.; Ferreira, A.N.; Cristelli, M.P.; Viana, L.; Mansur, J.B.; et al. Prospective Randomized Trial Investigating the Influence of Pharmaceutical Care on the Intra-Individual Variability of Tacrolimus Concentrations Early After Kidney Transplant. Drug Monit. 2016, 38, 447–455. [Google Scholar] [CrossRef]
- Chisholm, M.A.; Mulloy, L.L.; Jagadeesan, M.; DiPiro, J.T. Impact of clinical pharmacy services on renal transplant patients’ compliance with immunosuppressive medications. Clin. Transpl. 2001, 15, 330–336. [Google Scholar] [CrossRef]
- Fleming, J.N.; Gebregziabher, M.; Posadas, A.; Su, Z.; McGillicuddy, J.W.; Taber, D.J. Impact of a pharmacist-led, mHealth-based intervention on tacrolimus trough variability in kidney transplant recipients: A report from the TRANSAFE Rx randomized controlled trial. Am. J. Health Syst. Pharm. 2021, 78, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, H.M.; Fleming, J.N.; Gebregziabher, M.; Posadas Salas, M.A.; McGillicuddy, J.W.; Taber, D.J. A Critical Analysis of the Specific Pharmacist Interventions and Risk Assessments During the 12-Month TRANSAFE Rx Randomized Controlled Trial. Ann. Pharm. 2022, 56, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, H.M.; Fleming, J.N.; Gebregziabher, M.; Posadas-Salas, M.A.; Su, Z.; McGillicuddy, J.W.; Taber, D.J. Pharmacist-Led Mobile Health Intervention and Transplant Medication Safety: A Randomized Controlled Clinical Trial. Clin. J. Am. Soc. Nephrol. 2021, 16, 776–784. [Google Scholar] [CrossRef] [PubMed]
- Joost, R.; Dörje, F.; Schwitulla, J.; Eckardt, K.U.; Hugo, C. Intensified pharmaceutical care is improving immunosuppressive medication adherence in kidney transplant recipients during the first post-transplant year: A quasi-experimental study. Nephrol Dial. Transpl. 2014, 29, 1597–1607. [Google Scholar] [CrossRef] [PubMed]
- Kamath, C.C.; Dobler, C.C.; McCoy, R.G.; Lampman, M.A.; Pajouhi, A.; Erwin, P.J.; Matulis, J.; Elrashidi, M.; Darcel, J.; Alsawas, M.; et al. Improving Blood Pressure Management in Primary Care Patients with Chronic Kidney Disease: A Systematic Review of Interventions and Implementation Strategies. J. Gen. Intern. Med. 2020, 35, 849–869. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.T.; Chiang, Y.C.; Lai, Y.H.; Lin, L.Y.; Hsieh, H.F.; Chen, J.L. Effectiveness of Multidisciplinary Care for Chronic Kidney Disease: A Systematic Review. Worldviews Evid. Based Nurs. 2021, 18, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Al Raiisi, F.; Stewart, D.; Fernandez-Llimos, F.; Salgado, T.M.; Mohamed, M.F.; Cunningham, S. Clinical pharmacy practice in the care of Chronic Kidney Disease patients: A systematic review. Int. J. Clin. Pharm. 2019, 41, 630–666. [Google Scholar] [CrossRef]
- Ha Dinh, T.T.; Bonner, A.; Clark, R.; Ramsbotham, J.; Hines, S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 210–247. [Google Scholar] [CrossRef]
- Greer, N.; Bolduc, J.; Geurkink, E.; Rector, T.; Olson, K.; Koeller, E.; MacDonald, R.; Wilt, T.J. Pharmacist-Led Chronic Disease Management: A Systematic Review of Effectiveness and Harms Compared With Usual Care. Ann. Intern. Med. 2016, 165, 30–40. [Google Scholar] [CrossRef]
- Radhakrishnan, K. The efficacy of tailored interventions for self-management outcomes of type 2 diabetes, hypertension or heart disease: A systematic review. J. Adv. Nurs. 2012, 68, 496–510. [Google Scholar] [CrossRef]
- Tan, J.P.; Cheng, K.K.F.; Siah, R.C. A systematic review and meta-analysis on the effectiveness of education on medication adherence for patients with hypertension, hyperlipidaemia and diabetes. J. Adv. Nurs. 2019, 75, 2478–2494. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, S.; Siegal, B. Compliance and noncompliance in patients with a functioning renal transplant: A multicenter study. Transplantation 1998, 66, 1718–1726. [Google Scholar] [CrossRef] [PubMed]
- Mason, N.A.; Bakus, J.L. Strategies for reducing polypharmacy and other medication-related problems in chronic kidney disease. Semin. Dial. 2010, 23, 55–61. [Google Scholar] [CrossRef]
- Royal Pharmaceutical Society. A Competency Framework for All Prescribers. Available online: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Prescribing%20Competency%20Framework/RPS%20English%20Competency%20Framework%203.pdf?ver=mctnrKo4YaJDh2nA8N5G3A%3d%3d.pdf (accessed on 26 September 2021).
- Mendes, S.J.; Farisco, M.; Leite, S.N.; Storpirtis, S. A broad view of pharmaceutical services in multidisciplinary teams of public Primary Healthcare Centers: A mixed methods study in a large city in Brazil. Prim. Health Care Res. Dev. 2022, 23, e31. [Google Scholar] [CrossRef] [PubMed]





| Measurement of Patient Adherence | Description |
|---|---|
| Compliance Rate (CR) | CR is calculated according to the formula: [number of medication agent doses filled by pharmacy/number of doses prescribed per time period] × 100%; with 80% as a minimum threshold [40]. |
| Medication Event Monitoring System (MEMS) | An electronic medication bottle cap that records whenever the bottle is opened. Adherence is calculated according to the formula: [number of times bottle is opened/number of pills prescribed] × 100% [44]. |
| Medication non-adherence | Patient takes less than 80% of prescribed doses or too many medication [24]. |
| Morisky Medication Adherence Scale-4 (MMAS-4) | A series of four closed questions, each question that is answered with a ‘No’ receives a score of 1. The possible scoring range is 0 to 4. A score of 4 indicates high adherence, a score of from 2 to 3–medium adherence, and a score of less than 2–means poor patient adherence [13,37]. |
| Morisky Medication Adherence Scale-4 (MMAS-4)-modified | MMAS-4 scale was modified for BP medications [15,44]. |
| Morisky Medication Adherence Scale-6 (MMAS-6) | A series of six closed questions, 2 new questions were added to MMAS-4 scale to create the Modified Morisky Adherence Scale (MMAS-6). For the motivation domain (3 questions), a scoring range is from 0 to 3; a total score of 0 to 1 indicates low motivation and if the score is >1, the motivation domain is scored as high. For the knowledge domain (3 questions), a scoring range is from 0 to 3; a total score of 0 to 1 indicates low knowledge; if the score is >1, the knowledge domain is scored as high [26]. |
| Morisky Medication Adherence Scale-8 (MMAS-8) | A series of eight closed questions, 4 new questions were added to MMAS-4 scale to create the Modified Morisky Adherence Scale (MMAS-8); each question that is answered with a ‘No’ receives a score of 1. A score of eight indicates high adherence; a score of six to seven indicates medium adherence and a score of less than six indicates poor adherence [19,36]. |
| Basel Assessment of Adherence to Immunosuppressive Medication Scale (BAASIS) questionnaire | A series of six closed questions within three domains: implementation (items 1a, 1b, 2, 3–all items start with a ‘Yes’/‘No’ question; for items 1a, 1b and 2, if patient answers ‘Yes’, this is followed by five response categories to document the frequency of implementation problems, i.e., once, twice, etc.), initiation (item 5 with a ‘Yes’/‘No’ answer) and persistence (item 4 with a ‘Yes’/‘No’ answer). Any ‘Yes’ on any of items 1a, 1b, 2 or 3 indicates an issue with implementation. ‘Yes’ on item 4 indicates non-persistence of immunosuppressive medication use [39]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jasińska-Stroschein, M. The Effectiveness of Pharmacist Interventions in the Management of Patient with Renal Failure: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 11170. https://doi.org/10.3390/ijerph191811170
Jasińska-Stroschein M. The Effectiveness of Pharmacist Interventions in the Management of Patient with Renal Failure: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(18):11170. https://doi.org/10.3390/ijerph191811170
Chicago/Turabian StyleJasińska-Stroschein, Magdalena. 2022. "The Effectiveness of Pharmacist Interventions in the Management of Patient with Renal Failure: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 18: 11170. https://doi.org/10.3390/ijerph191811170
APA StyleJasińska-Stroschein, M. (2022). The Effectiveness of Pharmacist Interventions in the Management of Patient with Renal Failure: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(18), 11170. https://doi.org/10.3390/ijerph191811170






