Effects of Return Air Inlets’ Location on the Control of Fine Particle Transportation in a Simulated Hospital Ward
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Method
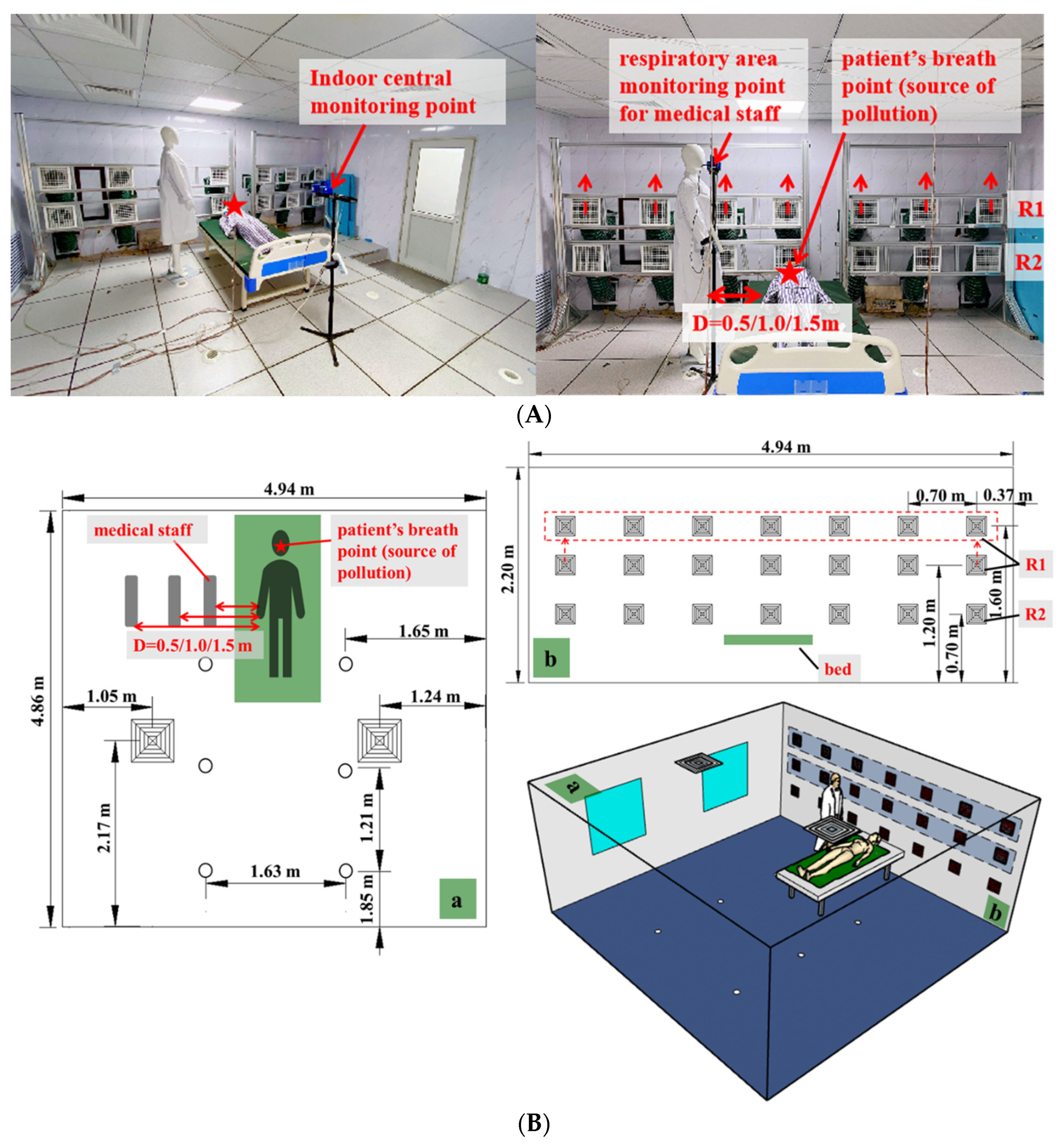
2.1.1. Experimental Setup
2.1.2. Experimental Method
2.2. Simulation Method
2.2.1. Model Development
2.2.2. Research on Grid Division and Grid Independence
2.2.3. Model Verification
2.2.4. TOPSIS Evaluation Method
2.2.5. Evaluation Index
Particle Concentration Decay Rate k
Inhalation Fraction Index IF
Particle Removal Efficiency ε
Energy Consumption of Ventilation System
Operation Cost-Effectiveness of Ventilation Filter System
3. Results and Discussion
3.1. Experimental Results
3.1.1. Influence of the Distance between Medical Staff and Patients on Evaluation Indicators
3.1.2. Influence of Return Air Inlets’ Height on Evaluation Indicators
3.2. Simulation Results
3.2.1. Energy Consumption of Ventilation Systems
3.2.2. TOPSIS Evaluation Results
3.3. Limitation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, S.; Zhao, X.; Nichols, S.R.; Bonilha, M.W.; Derwinski, T.; Auxier, J.T.; Chen, Q. Evaluation of airborne particle exposure for riding elevators. Build. Environ. 2022, 207, 108543. [Google Scholar] [CrossRef] [PubMed]
- Gennaro, F.D.; Pizzol, D.; Marotta, C.; Antunes, M.; Racalbuto, V.; Veronese, N.; Smith, L. Coronavirus Diseases (COVID-19) Current Status and Future Perspectives: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 2690. [Google Scholar] [CrossRef] [PubMed]
- Jr, A.; Mt, B.; An, B. Experimental study to quantify airborne particle deposition onto and resuspension from clothing using a fluorescent-tracking method. Build. Environ. 2022, 209, 108580. [Google Scholar]
- Papagiannis, D.; Malli, F.; Raptis, D.G.; Papathanasiou, I.V.; Gourgoulianis, K.I. Assessment of Knowledge, Attitudes, and Practices towards New Coronavirus (SARS-CoV-2) of Health Care Professionals in Greece before the Outbreak Period. Int. J. Environ. Res. Public Health 2020, 17, 4925. [Google Scholar] [CrossRef] [PubMed]
- Delgado, D.; Quintana, F.W.; Perez, G.; Liprandi, A.S.; Baranchuk, A. Personal Safety during the COVID-19 Pandemic: Realities and Perspectives of Healthcare Workers in Latin America. Int. J. Environ. Res. Public Health 2020, 17, 2798. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Tripepi, G.; Prinzio, R. Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 5218. [Google Scholar] [CrossRef]
- Satheesan, M.K.; Mui, K.W.; Ling, T.W. A numerical study of ventilation strategies for infection risk mitigation in general inpatient wards. Build. Simul. 2020, 13, 887–896. [Google Scholar] [CrossRef]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment—a multidisciplinary systematic review. Indoor Air 2007, 17, 2–18. [Google Scholar] [CrossRef]
- Li, H.; Shankar, S.N.; Witanachchi, C.T.; Lednicky, J.A.; Loeb, J.C.; Alam, M.M.; Fan, Z.H.; Mohamed, K.; Boyette, J.A.; Eiguren-Fernandez, A.; et al. Environmental Surveillance for SARS-CoV-2 in Two Restaurants from a Mid-scale City that Followed U.S. CDC Reopening Guidance. Aerosol. Air Qual. Res. 2022, 22, 210304. [Google Scholar] [CrossRef]
- Ss, A.; Xz, B.; Am, A.; Qc, C. Effective ventilation and air disinfection system for reducing coronavirus disease 2019 (COVID-19) infection risk in office buildings. Sustain. Cities Soc. 2021, 75, 103408. [Google Scholar]
- Kong, X.; Ren, Y.; Ren, J.; Duan, S.; Guo, C. Energy-saving performance of respiration-type double-layer glass curtain wall system in different climate zones of China: Experiment and simulation. Energ. Build. 2021, 252, 111464. [Google Scholar] [CrossRef]
- Zhao, L.; Liu, J.; Ren, J. Impact of various ventilation modes on IAQ and energy consumption in Chinese dwellings: First long-term monitoring study in Tianjin, China. Build. Environ. 2018, 143, 99–106. [Google Scholar] [CrossRef]
- Tian, X.; Li, B.; Ma, Y.; Liu, D.; Li, Y.; Cheng, Y. Experimental study of local thermal comfort and ventilation performance for mixing, displacement and stratum ventilation in an office. Sustain. Cities Soc. 2019, 50, 101630. [Google Scholar] [CrossRef]
- Lin, Z.; Wang, J.; Yao, T.; Chow, T.T. Investigation into anti-airborne infection performance of stratum ventilation. Build. Environ. 2012, 54, 29–38. [Google Scholar] [CrossRef]
- Kong, X.; Guo, C.; Lin, Z.; Duan, S.; He, J.; Ren, Y.; Ren, J. Experimental study on the control effect of different ventilation systems on fine particles in a simulated hospital ward. Sustain. Cities Soc. 2021, 73, 103102. [Google Scholar] [CrossRef]
- Awad, A.S.; Calay, R.K.; Badran, O.O.; Holdo, A.E. An experimental study of stratified flow in enclosures. Appl. Therm. Eng. 2008, 28, 2150–2158. [Google Scholar] [CrossRef]
- Yao, T.; Zhang, L. An experimental and numerical study on the effect of air terminal types on the performance of stratum ventilation. Build. Environ. 2014, 82, 75–86. [Google Scholar] [CrossRef]
- Zhang, L.; Mao, Y.; Tu, Q.; Wu, X.; Tan, L.; Zeeshan, A. Effects of Supply Parameters of Stratum Ventilation on Energy Utilization Efficiency and Indoor Thermal Comfort: A Computational Approach. Math. Probl. Eng. 2021, 2021, 1–16. [Google Scholar] [CrossRef]
- Filler, M. Best practices for underfloor air systems. ASHRAE J. 2004, 46, 39–46. [Google Scholar]
- Heidarinejad, G.; Fathollahzadeh, M.H.; Pasdarshahri, H. Effects of return air vent height on energy consumption, thermal comfort conditions and indoor air quality in an under floor air distribution system. Energ. Build. 2015, 97, 155–161. [Google Scholar] [CrossRef]
- Fan, Y.; Li, X.; Yan, Y.; Tu, J. Overall performance evaluation of underfloor air distribution system with different heights of return vents. Energ. Build. 2017, 147, 176–187. [Google Scholar] [CrossRef]
- Fathollahzadeh, M.H.; Heidarinejad, G.; Pasdarshahri, H. Prediction of thermal comfort, IAQ, and energy consumption in a dense occupancy environment with the under floor air distribution system. Build. Environ. 2015, 90, 96–104. [Google Scholar] [CrossRef]
- Cheng, Y.; Niu, J.; Liu, X.; Gao, N. Experimental and numerical investigations on stratified air distribution systems with special configuration: Thermal comfort and energy saving. Energ. Build. 2013, 64, 154–161. [Google Scholar] [CrossRef]
- Luo, X.; Huang, X.; Feng, Z.; Li, J.; Gu, Z. Influence of air inlet/outlet arrangement of displacement ventilation on local environment control for unearthed relics within site museum. Energ. Build. 2021, 246, 111116. [Google Scholar] [CrossRef]
- Rastogi, M.; Chauhan, A.; Vaish, R.; Kishan, A. Selection and performance assessment of Phase Change Materials for heating, ventilation and air-conditioning applications. Energ. Convers. Manag. 2015, 89, 260–269. [Google Scholar] [CrossRef]
- Mao, N.; Song, M.; Deng, S. Application of TOPSIS method in evaluating the effects of supply vane angle of a task/ambient air conditioning system on energy utilization and thermal comfort. Appl. Energ. 2016, 180, 536–545. [Google Scholar] [CrossRef]
- Ye, X.; Kang, Y.; Yan, Z.; Chen, B.; Zhong, K. Optimization study of return vent height for an impinging jet ventilation system with exhaust/return-split configuration by TOPSIS method. Build. Environ. 2020, 177, 106858. [Google Scholar] [CrossRef]
- G.B. Chinese. Architectural Design Code for Infectious Disease Hospital; G.B. Chinese: Beijing, China, 2014; pp. 50849–52014. [Google Scholar]
- G.B. Chinese. Code for Design of General Hospital; G.B. Chinese: Beijing, China, 2014; pp. 51039–52014. [Google Scholar]
- Liu, L.; Li, Y.; Nielsen, P.V.; Wei, J.; Jensen, R.L. Short-range airborne transmission of expiratory droplets between two people. Indoor Air 2017, 27, 452–462. [Google Scholar] [CrossRef]
- Verma, T.; Sinha, S. Experimental and Numerical Investigation of Contaminant Control in Intensive Care Unit: A Case Study of Raipur, India. J. Therm. Sci. Eng. Appl. 2020, 6, 736–750. [Google Scholar] [CrossRef]
- Lee, S.; Wang, B. Characteristics of emissions of air pollutants from burning of incense in a large environmental chamber. Atmos. Environ. 2004, 38, 941–951. [Google Scholar] [CrossRef]
- Ren, J.; Wade, M.; Corsi, R.L.; Novoselac, A. Particulate matter in mechanically ventilated high school classrooms. Build. Environ. 2020, 184, 106986. [Google Scholar] [CrossRef]
- Wang, W.; Wang, F.; Lai, D.; Chen, Q. Evaluation of SARS-COV-2 transmission and infection in airliner cabins. Indoor Air 2022, 32, e12979. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhang, N.; Lin, Z. Study on the particle size distribution of particulate matter and polycyclic aromatic hydrocarbons emitted from indoor combustion sources. Chin. J. Anal. Test. 2019, 38, 1171–1178. [Google Scholar]
- Yu, X.F.; Fu, D. A review of multi-index comprehensive evaluation methods. Stat. Decis. 2004, 11, 119–121. (In Chinese) [Google Scholar]
- Duan, Z.Z.; Zhou, W.W.; Wang, H.Y. Analysis of urban smart construction level based on entropy weight-topsis model: Taking Hefei City as an example. J. Kunming Univ. Sci. Technol. Soc. Sci. Ed. 2022, 22, 8. (In Chinese) [Google Scholar]
- Li, Z.X.; Liu, C.X.; Liu, D. Investment value evaluation of snack food industry based on entropy weight topsis model. J. Shanghai Lixin Inst. Account. Financ. 2020, 32, 12. (In Chinese) [Google Scholar]
- Ren, J.; Liu, J. Fine particulate matter control performance of a new kind of suspended fan filter unit for use in office buildings. Build. Environ. 2019, 149, 468–476. [Google Scholar] [CrossRef]
- Cao, G.; Awbi, H.; Yao, R.; Fan, Y.; Sirén, K.; Kosonen, R.; Zhang, J. A review of the performance of different ventilation and airflow distribution systems in buildings. Build. Environ. 2014, 73, 171–186. [Google Scholar] [CrossRef]
- Melikov, A.K.; Cermak, R.; Majer, M. Personalized ventilation: Evaluation of different air terminal devices. Energ. Build. 2002, 34, 829–836. [Google Scholar] [CrossRef]
- Month Tianjin of temperature. Available online: https://en.climate-data.org/asia/china/tianjin/tianjin-2606/ (accessed on 27 August 2022).
- Ren, J.; Liu, J.; Cao, X.; Hou, Y. Influencing factors and energy-saving control strategies for indoor fine particles in commercial office buildings in six Chinese cities. Energ. Build. 2017, 149, 171–179. [Google Scholar] [CrossRef]
- Noh, K.C.; Yook, S.J. Evaluation of clean air delivery rates and operating cost effectiveness for room air cleaner and ventilation system in a small lecture room. Energ. Build. 2016, 119, 111–118. [Google Scholar] [CrossRef]
- Lv, Y.; Wang, H.; Wei, S. The transmission characteristics of indoor particles under two ventilation modes. Energ. Build. 2018, 163, 1–9. [Google Scholar] [CrossRef]
- Berlanga, F.A.; Olmedo, I.; de Adana, M.R.; Villafruela, J.M.; José, J.F.S.; Castro, F. Experimental assessment of different mixing air ventilation systems on ventilation performance and exposure to exhaled contaminants in hospital rooms. Energ. Build. 2018, 177, 207–219. [Google Scholar] [CrossRef]
- Zhou, Y.; Ji, S. Experimental and numerical study on the transport of droplet aerosols generated by occupants in a fever clinic. Build. Environ. 2021, 187, 107402. [Google Scholar] [CrossRef]
- Kang, Z.; Zhang, Y.; Fan, H.; Feng, G. Numerical Simulation of Coughed Droplets in the Air-Conditioning Room. Procedia Eng. 2015, 121, 114–121. [Google Scholar] [CrossRef]
- Cheng, Y.; Yang, J.; Du, Z.; Peng, J. Investigations on the Energy Efficiency of Stratified Air Distribution Systems with Different Diffuser Layouts. Sustainability 2016, 8, 732. [Google Scholar] [CrossRef]
- Wang, L.; Kong, X.; Ren, J.; Fan, M.; Li, H. Novel hybrid composite phase change materials with high thermal performance based on aluminium nitride and nanocapsules. Energy 2021, 238, 121775. [Google Scholar] [CrossRef]
- Wang, L.; Guo, L.; Ren, J.; Kong, X. Using of heat thermal storage of PCM and solar energy for distributed clean building heating: A multi-level scale-up research. Appl. Energ. 2022, 321, 119345. [Google Scholar] [CrossRef]
- Ren, J.; He, J.; Kong, X.; Xu, W.; Kang, Y.; Yu, Z.; Li, H. A field study of CO2 and particulate matter characteristics during the transition season in the subway system in Tianjin, China. Energ. Build. 2022, 254, 111620. [Google Scholar] [CrossRef]
- Liu, J.; Lin, Z. Optimization of configurative parameters of stratum ventilated heating for a sleeping environment. J. Build. Eng. 2021, 38, 102167. [Google Scholar] [CrossRef]
- Zhang, S.; Lin, Z.; Ai, Z.; Wang, F.; Cheng, Y.; Huan, C. Effects of operation parameters on performances of stratum ventilation for heating mode. Build. Environ. 2019, 148, 55–66. [Google Scholar] [CrossRef]
- Zhao, X.; Liu, S.; Yin, Y.; Zhang, T.; Chen, Q. Airborne transmission of COVID-19 virus in enclosed spaces: An overview of research methods. Indoor Air 2022, 32, e13056. [Google Scholar] [CrossRef] [PubMed]










| Air Supply Type | Return Air Inlets’ Height (m) |
|---|---|
| Underfloor air supply | 0.7 |
| Underfloor air supply | 1.2 |
| Underfloor air supply | 1.6 |
| Top air supply | 0.7 |
| Top air supply | 1.2 |
| Top air supply | 1.6 |
| Side air supply | 1.2 supply and 0.7 return |
| Side air supply | 1.6 supply and 0.7 return |
| Air Exchange Rate (h−1) | Air Volume (m3/s) | Fan Energy Consumption (W) |
|---|---|---|
| 6 | 0.088 | 102.3 |
| 9 | 0.132 | 287.1 |
| 12 | 0.176 | 569.9 |
| Air Exchange Rate (h−1) | Energy Consumption (kW) | |||
|---|---|---|---|---|
| Spring | Summer | Autumn | Winter | |
| 6 | 0.10 | 1.35 | 0.10 | 5.00 |
| 9 | 0.29 | 2.16 | 0.29 | 7.98 |
| 12 | 0.60 | 3.09 | 0.60 | 10.40 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ren, J.; Duan, S.; Guo, L.; Li, H.; Kong, X. Effects of Return Air Inlets’ Location on the Control of Fine Particle Transportation in a Simulated Hospital Ward. Int. J. Environ. Res. Public Health 2022, 19, 11185. https://doi.org/10.3390/ijerph191811185
Ren J, Duan S, Guo L, Li H, Kong X. Effects of Return Air Inlets’ Location on the Control of Fine Particle Transportation in a Simulated Hospital Ward. International Journal of Environmental Research and Public Health. 2022; 19(18):11185. https://doi.org/10.3390/ijerph191811185
Chicago/Turabian StyleRen, Jianlin, Shasha Duan, Leihong Guo, Hongwan Li, and Xiangfei Kong. 2022. "Effects of Return Air Inlets’ Location on the Control of Fine Particle Transportation in a Simulated Hospital Ward" International Journal of Environmental Research and Public Health 19, no. 18: 11185. https://doi.org/10.3390/ijerph191811185





