Validation of StepTest4all for Assessing Cardiovascular Capacity in Young Adults
Abstract
:1. Introduction
2. Material and Methods
2.1. Participants and Samples
2.2. Data Collection
2.3. StepTest4all Protocol
2.4. Statistical Analysis
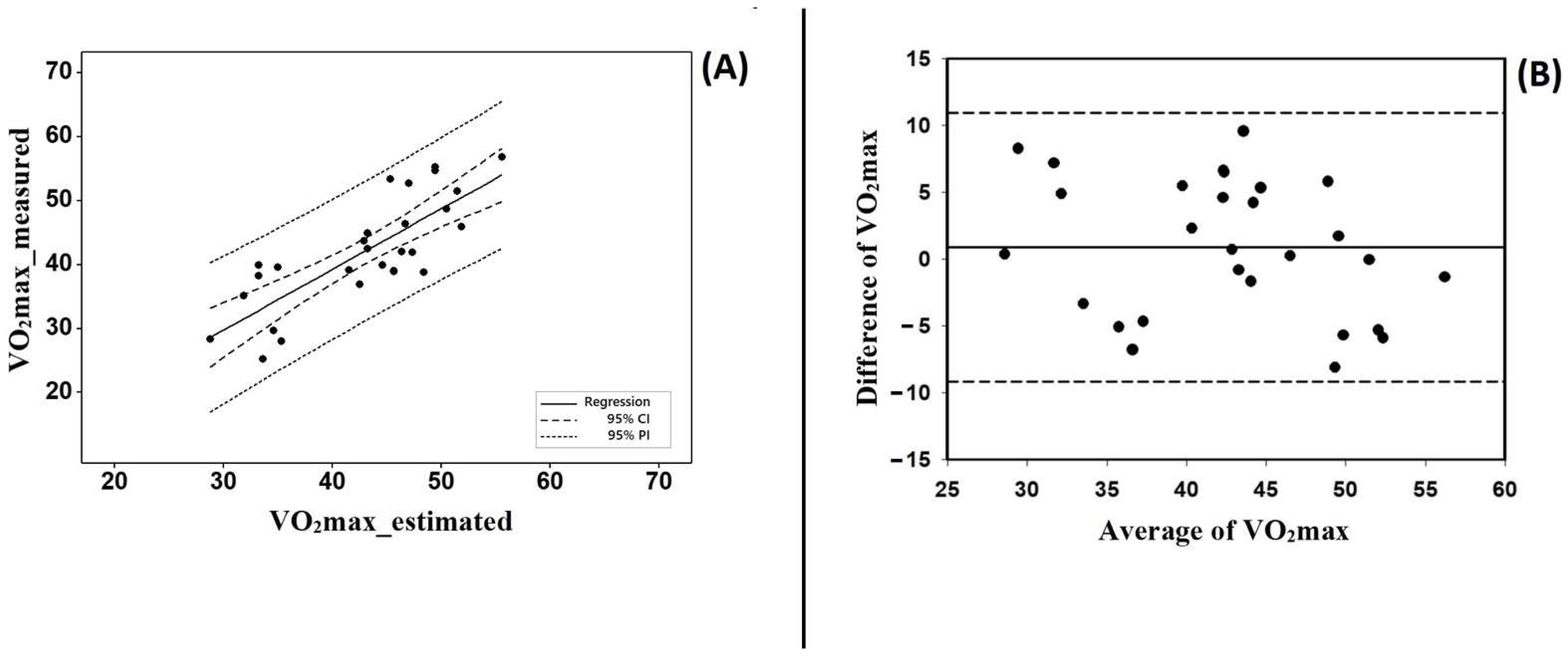
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Snader, C.E.; Lauer, M.S. Heart-rate recovery immediately after exercise as a predictor of mortality. N. Engl. J. Med. 1999, 341, 1351–1357. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S. Cardiorespiratory Fitness as a Quantitative Predictor of All-Cause Mortality and Cardiovascular Events in Healthy Men and Women: A Meta-Analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- Jae, S.Y.; Kurl, S.; Laukkanen, J.A.; Zaccardi, F.; Choi, Y.H.; Fernhall, B.; Carnethon, M.; Franklin, B.A. Exercise Heart Rate Reserve and Recovery as Predictors of Incident Type 2 Diabetes. Am. J. Med. 2016, 129, 536.e7–536.e12. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.Y.; Jee, J.H.; Bae, J.C.; Hong, W.J.; Jin, S.M.; Kim, J.H.; Lee, M.K. Delayed heart rate recovery after exercise as a risk factor of incident type 2 diabetes mellitus after adjusting for glycometabolic parameters in men. Int. J. Cardiol. 2016, 221, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Messinger-Rapport, B.; Pothier Snader, C.E.; Blackstone, E.H.; Yu, D.; Lauer, M.S. Value of exercise capacity and heart rate recovery in older people. J. Am. Geriatr. Soc. 2003, 51, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Kurl, S.; Jae, S.Y.; Voutilainen, A.; Hagnäs, M.; Laukkanen, J.A. Exercise heart rate reserve and recovery as risk factors for sudden cardiac death. Prog. Cardiovasc. Dis. 2021, 68, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Peçanha, T.; Bartels, R.; Brito, L.C.; Paula-Ribeiro, M.; Oliveira, R.S.; Goldberger, J.J. Methods of assessment of the post-exercise cardiac autonomic recovery: A methodological review. Int. J. Cardiol. 2017, 227, 795–802. [Google Scholar] [CrossRef]
- Adali, M.K.; Varol, E.; Aksoy, F.; Icli, A.; Ersoy, I.H.; Ozaydin, M.; Erdogan, D.; Dogan, A. Impaired heart rate recovery in patients with endemic fluorosis. Biol. Trace Elem. Res. 2013, 152, 310–315. [Google Scholar] [CrossRef]
- Sydó, N.; Sydó, T.; Gonzalez Carta, K.A.; Hussain, N.; Farooq, S.; Murphy, J.G.; Merkely, B.; Lopez-Jimenez, F.; Allison, T.G. Prognostic Performance of Heart Rate Recovery on an Exercise Test in a Primary Prevention Population. J. Am. Heart Assoc. 2018, 7, e008143. [Google Scholar] [CrossRef]
- Trevizani, G.A.; Benchimol-Barbosa, P.R.; Nadal, J. Effects of age and aerobic fitness on heart rate recovery in adult men. Arq. Bras. Cardiol. 2012, 99, 802–810. [Google Scholar] [CrossRef]
- Qiu, S.; Cai, X.; Sun, Z.; Li, L.; Zuegel, M.; Steinacker, J.M.; Schumann, U. Heart Rate Recovery and Risk of Cardiovascular Events and All-Cause Mortality: A Meta-Analysis of Prospective Cohort Studies. J. Am. Heart Assoc. 2017, 6, e005505. [Google Scholar] [CrossRef]
- Jin, Q.; Li, X.; Zhang, Y.; Zhao, Z.; Zhao, Q.; Yan, L.; Duan, A.; Luo, Q.; Liu, Z. Heart Rate Recovery at 1 Min after Exercise Is a Marker of Disease Severity and Prognosis in Chronic Thromboembolic Pulmonary Hypertension. Respiration 2022, 101, 455–464. [Google Scholar] [CrossRef]
- Petrella, R.; Koval, J.; Cunningham, D.; Paterson, D. A self-paced step test to predict aerobic fitness in older adults in the primary care clinic. J Am Geriatr Soc 2001; 49:632e8.Bennett, H.; Parfitt, G.; Davison, K.; Eston, R. Validity of Submaximal Step Tests to Estimate Maximal Oxygen Uptake in Healthy Adults. Sports Med. 2016, 46, 737–750. [Google Scholar] [CrossRef]
- Hughes, A.D.; Chaturvedi, N. Estimation of Maximal Oxygen Consumption and Heart Rate Recovery Using the Tecumseh Sub-Maximal Step Test and their Relationship to Cardiovascular Risk Factors. Artery Res. 2017, 18, 29–35. [Google Scholar] [CrossRef]
- Pepera, G.; Panagiota, Z. Comparison of heart rate response and heart rate recovery after step test among smoker and non-smoker athletes. Afr. Health Sci. 2021, 21, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Morita, A.A.; Silva, L.K.O.; Bisca, G.W.; Oliveira, J.M.; Hernandes, N.A.; Pitta, F.; Furlanetto, K.C. Heart Rate Recovery, Physical Activity Level, and Functional Status in Subjects with COPD. Respir. Care. 2018, 63, 1002–1008. [Google Scholar] [CrossRef]
- Haraldsdottir, K.; Brickson, S.; Sanfilippo, J.; Dunn, W.; Watson, A. In-season changes in heart rate recovery are inversely related to time to exhaustion but not aerobic capacity in rowers. Scand. J. Med. Sci. Sports. 2018, 28, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Daanen, H.A.; Lamberts, R.P.; Kallen, V.L.; Jin, A.; Van Meeteren, N.L. A systematic review on heart-rate recovery to monitor changes in training status in athletes. Int. J. Sports Physiol. Perform. 2012, 7, 251–260. [Google Scholar] [CrossRef]
- Rodríguez-Fernández, A.; Sanchez-Sanchez, J.; Ramirez-Campillo, R.; Nakamura, F.Y.; Rodríguez-Marroyo, J.A.; Villa-Vicente, J.G. Relationship between Repeated Sprint Ability, Aerobic Capacity, Intermittent Endurance, and Heart Rate Recovery in Youth Soccer Players. J. Strength Cond. Res. 2019, 33, 3406–3413. [Google Scholar] [CrossRef]
- Harry, K.; Booysen, M.J. Faster Heart Rate Recovery Correlates with High-Intensity Match Activity in Female Field Hockey Players-Training Implications. J. Strength Cond. Res. 2020, 34, 1150–1157. [Google Scholar] [CrossRef]
- Suzic Lazic, J.; Dekleva, M.; Soldatovic, I.; Leischik, R.; Suzic, S.; Radovanovic, D.; Djuric, B.; Nesic, D.; Lazic, M.; Mazic, S. Heart rate recovery in elite athletes: The impact of age and exercise capacity. Clin. Physiol. Funct. Imaging 2017, 37, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.; Wheen, P.; Brandon, L.; Finucane, C.; Kenny, R.A.; Maree, A. Impaired autonomic function after incomplete revascularisation. Open Heart 2021, 8, e001835. [Google Scholar] [CrossRef] [PubMed]
- Hansen, D.; Jacobs, N.; Bex, S.; D’Haene, G.; Dendale, P.; Claes, N. Are fixed-rate step tests medically safe for assessing physical fitness? Eur. J. Appl. Physiol. 2011, 111, 2593–2599. [Google Scholar] [CrossRef]
- Fecchio, R.Y.; Brito, L.; Leicht, A.S.; Forjaz, C.L.M.; Peçanha, T. Reproducibility of post-exercise heart rate recovery indices: A systematic review. Auton Neurosci. 2019, 221, 102582. [Google Scholar] [CrossRef]
- Mackenzie, B. Harvard Step Test [WWW]. 2007. Available online: https://www.brianmac.co.uk/havard.htm (accessed on 29 August 2022).
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Heyward, V.H. Advanced Fitness Assessment and Exercise Prescription, 3rd ed.; Library of Congress: Washington, DC, USA, 1997.
- Jamnick, N.A.; By, S.; Pettitt, C.D.; Pettitt, R.W. Comparison of the YMCA and a Custom Submaximal Exercise Test for Determining VO2max. Med. Sci. Sports Exerc. 2016, 48, 254–259. [Google Scholar] [CrossRef]
- Andersen, R.E.; Wadden, T.A. Validation of a cycle ergometry equation for predicting steady-rate VO2 in obese women. Med. Sci. Sports Exerc. 1995, 27, 1457–1460. [Google Scholar] [CrossRef]
- Evans, H.J.; Ferrar, K.E.; Smith, A.E.; Parfitt, G.; Eston, R.G. A systematic review of methods to predict maxi-mal oxygen uptake from submaximal, open circuit spirometry in healthy adults. J. Sci. Med. Sport. 2015, 18, 183–188. [Google Scholar] [CrossRef]
- Bennett, H.; Davison, K.; Parfitt, G.; Eston, R. Validity of a perceptually-regulated step test protocol for assessing cardiorespiratory fitness in healthy adults. Eur. J. Appl. Physiol. 2016, 116, 2337–2344. [Google Scholar] [CrossRef]
- Hopkins, W.G. A scale of magnitude for effect statistics. In A New View of Statistics; Will, G., Ed.; Hopkins: Melbourne, Australia, 2002; p. 50. [Google Scholar]
- Barbosa, T.M.; Ramos, R.; Silva, A.J.; Marinho, D.A. Assessment of passive drag in swimming by numerical simulation and analytical procedure. J. Sports Sci. 2018, 36, 492–498. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- ACSM. Guidelines for Exercise Testing and Prescription, 10th ed.; Library of Congress: Washington, DC, USA, 2018.
- Okutucu, S.; Karakulak, U.N.; Aytemir, K.; Oto, A. Heart rate recovery: A practical clinical indicator of abnormal cardiac autonomic function. Expert Rev. Cardiovasc. Ther. 2011, 9, 1417–1430. [Google Scholar] [CrossRef] [PubMed]
- Latchman, P.L.; Yang, Q.; Kong, L.; Zhang, H.; Sebagisha, J.; De Meersman, R.E. Heart Rate Recovery, Central Systolic Pressure, and Augmentation Index in Young Healthy Individuals. Vasc. Health Risk Manag. 2022, 18, 17–25. [Google Scholar] [CrossRef]
- Jaafar, Z.; Lim, Y.Z. A comparison of low and high dose of moderate intensity aerobic exercise on heart rate recovery of the sedentary adults: A pragmatic randomised controlled trial. J. Sports Med. Phys. Fitness. 2022, 27, 35620954. [Google Scholar] [CrossRef]
- Adabag, S.; Pierpont, G.L. Exercise heart rate recovery: Analysis of methods and call for standards. Heart 2013, 99, 1711–1712. [Google Scholar] [CrossRef]
- Gupta, M.; Bansal, V.; Chhabra, S.K. Abnormal heart rate recovery and chronotropic incompetence on exercise in chronic obstructive pulmonary disease. Chron. Respir. Dis. 2013, 10, 117–126. [Google Scholar] [CrossRef]
- McArdle, W.D. Fisiologia do Exercício: Energia, Nutrição e Desempenho Humano; Guanabara Koogan: Rio de Janeiro, Brazil, 2003. [Google Scholar]
- TANITA. Available online: https://tanita.eu/blog/could-improving-your-vo2-max-be-the-secret-of-success (accessed on 28 July 2022).
- Bragada et al. Available online: https://www.facebook.com/StepTest4all (accessed on 28 July 2022).
| Equation Group | Validation Group | |||||
|---|---|---|---|---|---|---|
| Mean ± 1SD | Mean ± 1SD | |||||
| Women (n = 10) | Men (n =18) | Total EG | Women (n = 9) | Men (n = 19) | Total VG | |
| Age [years] | 21.60 ± 1.84 | 21.17 ± 1.98 | 21.32 ± 1.90 | 20.44 ± 2.88 | 22.89 ± 3.80 | 22.11 ± 3.67 |
| Body mass [kg] | 61.45 ± 5.06 | 72.06 ± 8.83 | 68.27 ± 9.19 | 53.11 ± 5.42 | 72.92 ± 6.75 | 66.55 ± 13.31 |
| Height [m] | 1.63 ± 0.04 | 1.77 ± 0.07 | 1.72 ± 0.09 | 1.60 ± 0.04 | 1.75 ± 0.07 | 1.71 ± 0.10 |
| BMI [kg/m2] | 23.13 ± 3.02 | 22.93 ± 2.22 | 23.00 ± 2.48 | 20.75 ± 2.38 | 23.72 ± 2.11 | 22.77 ± 2.58 |
| HRR1min [bpm] | 35.50 ± 10.23 | 40.22 ± 10.99 | 38.54 ± 10.79 | 34.89 ± 10.71 | 38.42 ± 10.42 | 37.29 ± 10.45 |
| VO2max [mL/kg/min] | 34.41 ± 6.39 | 47.75 ± 6.71 | 42.99 ± 9.18 | 33.51 ± 5.64 | 46.15 ± 6.23 | 42.09 ± 8.45 |
| HRR_rest [bpm] | 81.90 ± 12.00 | 69.11 ± 10,94 | 73.68 ± 12.75 | 80.76 ± 10.60 | 64.37 ± 10.88 | 69.64 ± 13.16 |
| VO2_rest [mL/kg/min] | 3.60 ± 0.86 | 3.61 ± 0.54 | 3.61 ± 0.66 | 3,54 ± 0.44 | 3.66 ± 0.64 | 3.62 ± 0.58 |
| VO2max Measured [mL/kg/min] | VO2max Estimated [mL/kg/min] | |||
|---|---|---|---|---|
| Mean ± 1SD | Mean ± 1SD | Mean difference (95CI) | t-test (p value) | d [descriptor] |
| 42.09 ± 8.45 | 42.99 ± 7.10 | −0.899 (−2.889 to 1.089) | −0.928 (0.362) | 0.12 [trivial] |
| CVC_Classification | HRR1min | Men | Women | ||
|---|---|---|---|---|---|
| VO2max | McArdle et al., 2003 [42] | VO2max | McArdle et al., 2003 [42] | ||
| Poor | <20 | <40 | <36.5 | <28 | <29 |
| Moderate | 20–34 | 42–44.2 | 36.5–42.4 | 28–32.2 | 29–32 |
| Good | 35–49 | 44.3–49 | 42.5–46.4 | 32.3–36.9 | 33–36 |
| Excellent | ≥50 | ≥49 | ≥46.5 | ≥37 | ≥37 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bragada, J.A.; Bartolomeu, R.F.; Rodrigues, P.M.; Magalhães, P.M.; Bragada, J.P.; Morais, J.E. Validation of StepTest4all for Assessing Cardiovascular Capacity in Young Adults. Int. J. Environ. Res. Public Health 2022, 19, 11274. https://doi.org/10.3390/ijerph191811274
Bragada JA, Bartolomeu RF, Rodrigues PM, Magalhães PM, Bragada JP, Morais JE. Validation of StepTest4all for Assessing Cardiovascular Capacity in Young Adults. International Journal of Environmental Research and Public Health. 2022; 19(18):11274. https://doi.org/10.3390/ijerph191811274
Chicago/Turabian StyleBragada, José A., Raul F. Bartolomeu, Pedro M. Rodrigues, Pedro M. Magalhães, João P. Bragada, and Jorge E. Morais. 2022. "Validation of StepTest4all for Assessing Cardiovascular Capacity in Young Adults" International Journal of Environmental Research and Public Health 19, no. 18: 11274. https://doi.org/10.3390/ijerph191811274
APA StyleBragada, J. A., Bartolomeu, R. F., Rodrigues, P. M., Magalhães, P. M., Bragada, J. P., & Morais, J. E. (2022). Validation of StepTest4all for Assessing Cardiovascular Capacity in Young Adults. International Journal of Environmental Research and Public Health, 19(18), 11274. https://doi.org/10.3390/ijerph191811274









