A Review of Converging Technologies in eHealth Pertaining to Artificial Intelligence
Abstract
:1. Introduction
- Supervised learning: learning starts with a set of example inputs and their correct outputs.
- Unsupervised learning: only input data are provided and the algorithm groups or clusters the data, giving it a structure.
- Semi-supervised learning: some of the data are missing training labels.
- Reinforcement learning: focused on learning through trial and error.
- Improvements in diagnosis accuracy, e.g., detecting heart failure [2].
- Clinical applications, e.g., nutrition assessment [6].
- Healthcare process optimization, e.g., the complexity and the potential of integrating AI into healthcare processes [7].
- Precision medicine, e.g., detecting sleep apnea through deep learning [10].
- Automate detection, e.g., automated acute myocardial infarction detection using ECGs from smartwatches [11].
- Improved quality of care, e.g., using AI to improve chronic disease care for type 2 diabetes mellitus patients [12].
- Reduced healthcare costs, e.g., predicting health and population well-being [13].
- Discovering adverse effects of medication, e.g., machine learning models discovering adverse drug effects on the gut microbiome [14].
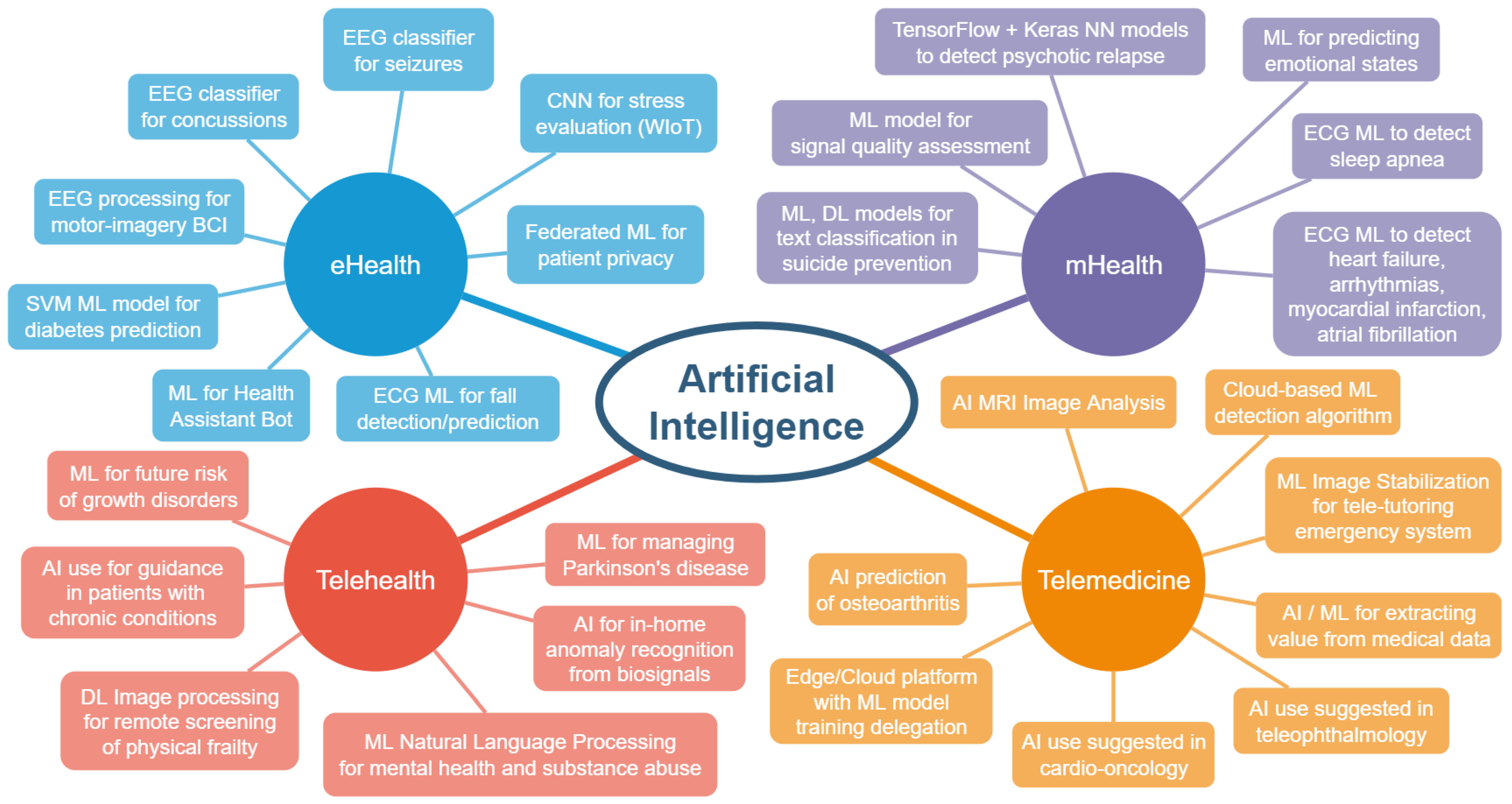
2. Overview of Healthcare Applications
- Remote patient monitoring (RPM)—refers to patient monitoring and the transmission of medical data such as blood pressure, heart rate, heart rhythm, oxygen saturation, glucose levels, weight, etc. Clinicians can often monitor this data in real time.
- Interactive patient care—offers live interactive communication between patients and healthcare service providers via video, phone or other secure channels.
- Store and forward—consists of recording and transmitting multimedia data such as image, sound or video.
2.1. eHealth
2.2. mHealth
- Advantages and disadvantages of wearable solutions for arrhythmia monitoring (outpatient telemetry);
- Wearables can also deliver therapy (electric shocks in life-threatening situations);
- they can improve the quality of life (early discharge, less outpatient visits, reassurances);
- Ultra-portable electrocardiogram patches (Zio Patch by iRhythm Technologies, San Francisco, CA, USA) that can last up to 14 days without recharging and can, in some scenarios, provide better diagnostic yield than Holter monitoring;
- Sleep apnea screening can be undertaken with wrist-worn reflective photoplethysmography, which has a promising correlation to standard polysomnography;
- Artificial intelligence algorithms can be used in conjunction with the data collected from wearables, automatically detecting multiple conditions, without the need for manual interpretation.
2.3. Telehealth
2.4. Telemedicine
- Digital health technologies such as mobile health (mHealth) and wearables help patients to monitor their own health and reduce the number of unneeded hospital visits, detect abnormal heart rates (Apple Watch), and collect and analyze health data, caring for patients while keeping them safe during the pandemic.
- In the field of telemedicine, many freely accessible cloud-based solutions have become compliant with laws that protect patient information, making cardio-oncology able to benefit from telehealth.
- Social media-assisted telehealth, through its various means of information propagation, has an important impact on prevention and innovation, especially in cardio-oncology.
- Artificial intelligence is without a doubt one of the foundation elements of many eHealth implementations, be it mHealth, wearables, remote patient monitoring or other applications. By connecting artificial intelligence algorithms with social media platforms, these systems can not only predict some conditions, but even help locate or get in contact with the patient.
3. Challenges of eHealth and AI Applications in Healthcare
3.1. Adoption
- Identifying the difficulties in utilizing the power of AI in care delivery;
- Creating education plans for multiple interventions;
- Determining curriculum issues;
- Increasing awareness, introducing certificate-based interventions for healthcare providers and for leaders, and providing coaching and innovation hubs;
- Performing evaluation studies;
- Encouraging sharing best practices and the creation of new knowledge.
3.2. Security and Privacy of Health Information
3.3. Usability of AI in eHealth
3.4. Accessibility and Affordability
3.5. Ethical and Social
4. Discussion
- Social networking tends to play an important role in our daily lives, even if we try to minimize it as much as possible. Teenagers and young adults are highly interconnected through this communication medium, meaning that they can more easily be influenced by wrong advice received from persons pretending to be medical professionals. To address this issue, we believe that some eHealth solutions should incorporate social components into their implementations, providing a trusted source of information. From [74], we are presented with the connection of social media and vaccine hesitancy, pointing out the importance of the presence of actual health experts in social media discussions.
- Surveillance camera presence is continuously increasing in many homes, marketplaces, public and industrial places. Still, a limited number of security cameras offer certain human movement detection. We strongly believe that this perpetually alert watchdog could safeguard our lives as well. COVID-19 has proven that cameras can be crucial in detecting face masks [75], aiding both healthcare and law enforcement agencies. One of the low-cost approaches to fall detection, according to the review in [76], is the use of camera-based devices. A future direction we see developing at least in testing, after taking into consideration privacy concerns and anonymizing the data, consists of surveillance nodes sending information to processing servers where fall-detection events could be confirmed and acted on to the extent of notifying healthcare services. This method could provide solutions for public or workplace accidents, where the only witness is the surveillance camera. The processing power could be provided by the healthcare service or an organization, unrelated to the detection node’s sector.
- Cryptocurrency is present in most modern fintech mobile applications, offering various benefits and capabilities that have yet to find applications in eHealth. In [77], a dedicated cryptocurrency coin called Wholesome Coin is introduced with the hope of making people healthier and reducing medical costs. With the development of WIoT, many new ways of motivating users to live healthier lives are emerging.
- The gamification of health could be another direction that provides improved health services with less traumatic experiences for children. The Xploro platform [78] has reduced the procedural anxiety of children attending hospitals.
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- El-Sherif, D.; Abouzid, M.; Elzarif, M.; Ahmed, A.; Albakri, A.; Alshehri, M. Telehealth and Artificial Intelligence Insights into Healthcare during the COVID-19 Pandemic. Healthcare 2022, 10, 385. [Google Scholar] [CrossRef] [PubMed]
- Yasmin, F.; Shah, S.; Naeem, A.; Shujauddin, S.; Jabeen, A.; Kazmi, S.; Siddiqui, S.; Kumar, P.; Salman, S.; Hassan, S.; et al. Artificial Intelligence in the Diagnosis and Detection of Heart Failure: The Past, Present, and Future. Rev. Cardiovasc. Med. 2021, 22, 1095–1113. [Google Scholar] [CrossRef] [PubMed]
- McGuire, R.; Yu, S.; Payne, P.; Lai, A.; Vazquez-Guillamet, M.; Kollef, M.; Michelson, A. A Pragmatic Machine Learning Model to Predict Carbapenem Resistance. Antimicrob. Agents Chemother. 2021, 65, e00063-21. [Google Scholar] [CrossRef]
- Van Smeden, M.; Heinze, G.; Van Calster, B.; Asselbergs, F.; Vardas, P.; Bruining, N.; de Jaegere, P.; Moore, J.; Denaxas, S.; Boulesteix, A.; et al. Critical Appraisal of Artificial Intelligence-Based Prediction Models for Cardiovascular Disease. Eur. Heart J. 2022, 43, 2921–2930. [Google Scholar] [CrossRef] [PubMed]
- Huttunen, J.; Karkkainen, L.; Honkala, M.; Lindholm, H. Deep Learning for Prediction of Cardiac Indices from Photoplethysmographic Waveform: A Virtual Database Approach. Int. J. Numer. Methods Biomed. Eng. 2020, 36, e3303. [Google Scholar] [CrossRef]
- Limketkai, B.; Mauldin, K.; Manitius, N.; Jalilian, L.; Salonen, B. The Age of Artificial Intelligence: Use of Digital Technology in Clinical Nutrition. Curr. Surg. Rep. 2021, 9, 20. [Google Scholar] [CrossRef]
- Schneider-Kamp, A. The Potential of AI in Care Optimization: Insights from the User-Driven Co-Development of a Care Integration System. Inq.-J. Health Care Organ. Provis. Financ. 2021, 58, 00469580211017992. [Google Scholar] [CrossRef]
- Dawoodbhoy, F.; Delaney, J.; Cecula, P.; Yu, J.; Peacock, I.; Tan, J.; Cox, B. AI in Patient Flow: Applications of Artificial Intelligence to Improve Patient Flow in NHS Acute Mental Health Inpatient Units. Heliyon 2021, 7, e06993. [Google Scholar] [CrossRef]
- Cecula, P.; Yu, J.; Dawoodbhoy, F.M.; Delaney, J.; Tan, J.; Peacock, I.; Cox, B. Applications of Artificial Intelligence to Improve Patient Flow on Mental Health Inpatient Units—Narrative Literature Review. Heliyon 2021, 7, e06626. [Google Scholar] [CrossRef]
- Zhang, Q.; Boente, R. IEEE DeepWave: Non-Contact Acoustic Receiver Powered by Deep Learning to Detect Sleep Apnea. In Proceedings of the 2020 IEEE 20th International Conference on Bioinformatics and Bioengineering (BIBE), Cincinnati, OH, USA, 26–28 October 2020; pp. 723–727. [Google Scholar]
- Han, C.; Song, Y.; Lim, H.; Tae, Y.; Jang, J.; Lee, B.; Lee, Y.; Bae, W.; Yoon, D. Automated Detection of Acute Myocardial Infarction Using Asynchronous Electrocardiogram Signals-Preview of Implementing Artificial Intelligence with Multichannel Electrocardiographs Obtained from Smartwatches: Retrospective Study. J. Med. Internet Res. 2021, 23, e31129. [Google Scholar] [CrossRef]
- Tarumi, S.; Takeuchi, W.; Chalkidis, G.; Rodriguez-Loya, S.; Kuwata, J.; Flynn, M.; Turner, K.; Sakaguchi, F.; Weir, C.; Kramer, H.; et al. Leveraging Artificial Intelligence to Improve Chronic Disease Care: Methods and Application to Pharmacotherapy Decision Support for Type-2 Diabetes Mellitus. Methods Inf. Med. 2021, 60, E32–E43. [Google Scholar] [CrossRef] [PubMed]
- Viljanen, M.; Meijerink, L.; Zwakhals, L.; van de Kassteele, J. A Machine Learning Approach to Small Area Estimation: Predicting the Health, Housing and Well-Being of the Population of Netherlands. Int. J. Health Geogr. 2022, 21, 4. [Google Scholar] [CrossRef] [PubMed]
- McCoubrey, L.; Elbadawi, M.; Orlu, M.; Gaisford, S.; Basit, A. Machine Learning Uncovers Adverse Drug Effects on Intestinal Bacteria. Pharmaceutics 2021, 13, 1026. [Google Scholar] [CrossRef] [PubMed]
- Jabarulla, M.; Lee, H. A Blockchain and Artificial Intelligence-Based, Patient-Centric Healthcare System for Combating the COVID-19 Pandemic: Opportunities and Applications. Healthcare 2021, 9, 1019. [Google Scholar] [CrossRef] [PubMed]
- Hurmuz, M.Z.M.; Jansen-Kosterink, S.M.; Beinema, T.; Fischer, K.; op den Akker, H.; Hermens, H.J. Evaluation of a Virtual Coaching System EHealth Intervention: A Mixed Methods Observational Cohort Study in the Netherlands. Internet Interv. 2022, 27, 100501. [Google Scholar] [CrossRef] [PubMed]
- Samie, F.; Paul, S.; Bauer, L.; Henkel, J. Highly Efficient and Accurate Seizure Prediction on Constrained IoT Devices. In Proceedings of the 2018 Design, Automation & Test in Europe Conference & Exhibition (DATE), Dresden, Germany, 19–23 March 2018; pp. 955–960. [Google Scholar]
- Wickramaratne, S.D.; Mahmud, M.S.; Ross, R.S. Use of Brain Electrical Activity to Classify People with Concussion: A Deep Learning Approach. In Proceedings of the ICC 2020—2020 IEEE International Conference on Communications (ICC), Dublin, Ireland, 7–11 June 2020; pp. 1–6. [Google Scholar]
- Fang, H.; Jin, J.; Daly, I.; Wang, X. Feature Extraction Method Based on Filter Banks and Riemannian Tangent Space in Motor-Imagery BCI. IEEE J. Biomed. Health Inform. 2022, 26, 2504–2514. [Google Scholar] [CrossRef]
- Jiang, S.; Firouzi, F.; Chakrabarty, K.; Elbogen, E. A Resilient and Hierarchical IoT-Based Solution for Stress Monitoring in Everyday Settings. IEEE Internet Things J. 2022, 9, 10224–10243. [Google Scholar] [CrossRef]
- Deebak, B.D.; Memon, F.H.; Cheng, X.; Dev, K.; Hu, J.; Khowaja, S.A.; Qureshi, N.M.F.; Choi, K.H. Seamless Privacy-Preservation and Authentication Framework for IoT-Enabled Smart EHealth Systems. Sustain. Cities Soc. 2022, 80, 103661. [Google Scholar] [CrossRef]
- La Blunda, L.; Gutierrez-Madronal, L.; Wagner, M.F.; Medina-Bulo, I. A Wearable Fall Detection System Based on Body Area Networks. IEEE Access 2020, 8, 193060–193074. [Google Scholar] [CrossRef]
- Sung, M.; Park, S.; Jung, S.; Lee, E.; Lee, J.; Park, Y.R. Developing a Mobile App for Monitoring Medical Record Changes Using Blockchain: Development and Usability Study. J. Med. Internet Res. 2020, 22, e19657. [Google Scholar] [CrossRef]
- Almogren, A.; Mohiuddin, I.; Din, I.U.; Almajed, H.; Guizani, N. FTM-IoMT: Fuzzy-Based Trust Management for Preventing Sybil Attacks in Internet of Medical Things. IEEE Internet Things J. 2021, 8, 4485–4497. [Google Scholar] [CrossRef]
- Polignano, M.; Narducci, F.; Iovine, A.; Musto, C.; De Gemmis, M.; Semeraro, G. HealthAssistantBot: A Personal Health Assistant for the Italian Language. IEEE Access 2020, 8, 107479–107497. [Google Scholar] [CrossRef]
- Sen, S.S.; Cicioglu, M.; Calhan, A. IoT-Based GPS Assisted Surveillance System with Inter-WBAN Geographic Routing for Pandemic Situations. J. Biomed. Inform. 2021, 116, 103731. [Google Scholar] [CrossRef]
- Sarker, I.H.; Faruque, M.F.; Alqahtant, H.; Kalim, A. K-Nearest Neighbor Learning Based Diabetes Mellitus Prediction and Analysis for EHealth Services. EAI Endorsed Trans. Scalable Inform. Syst. 2020, 7, 4. [Google Scholar] [CrossRef]
- Swain, K.; Cherukuri, M.; Mishra, S.K.; Appasani, B.; Patnaik, S.; Bizon, N. LI-Care: A LabVIEW and IoT Based EHealth Monitoring System. Electronics 2021, 10, 3137. [Google Scholar] [CrossRef]
- Sükei, E.; Norbury, A.; Perez-Rodriguez, M.M.; Olmos, P.M.; Artés, A. Predicting Emotional States Using Behavioral Markers Derived from Passively Sensed Data: Data-Driven Machine Learning Approach. JMIR Mhealth Uhealth 2021, 9, e24465. [Google Scholar] [CrossRef]
- Duncker, D.; Ding, W.; Etheridge, S.; Noseworth, P.; Veltmann, C.; Yao, X.; Bunch, T.; Gupta, D. Smart Wearables for Cardiac Monitoring-Real-World Use beyond Atrial Fibrillation. Sensors 2021, 21, 2539. [Google Scholar] [CrossRef]
- Adler, D.; Ben-Zeev, D.; Tseng, V.; Kane, J.; Brian, R.; Campbell, A.; Hauser, M.; Scherer, E.; Choudhury, T. Predicting Early Warning Signs of Psychotic Relapse from Passive Sensing Data: An Approach Using Encoder-Decoder Neural Networks. JMIR Mhealth Uhealth 2020, 8, e19962. [Google Scholar] [CrossRef]
- Xu, H.; Yan, W.; Lan, K.; Ma, C.; Wu, D.; Wu, A.; Yang, Z.; Wang, J.; Zang, Y.; Yan, M.; et al. Assessing Electrocardiogram and Respiratory Signal Quality of a Wearable Device (SensEcho): Semisupervised Machine Learning-Based Validation Study. JMIR Mhealth Uhealth 2021, 9, e25415. [Google Scholar] [CrossRef]
- Apergi, L.; Bjarnadottir, M.; Baras, J.; Golden, B.; Anderson, K.; Chou, J.; Shara, N. Voice Interface Technology Adoption by Patients with Heart Failure: Pilot Comparison Study. JMIR Mhealth Uhealth 2021, 9, e24646. [Google Scholar] [CrossRef]
- Bonini, N.; Vitolo, M.; Imberti, J.F.; Proietti, M.; Romiti, G.F.; Boriani, G.; Paaske Johnsen, S.; Guo, Y.; Lip, G.Y. Mobile Health Technology in Atrial Fibrillation. Expert Rev. Med. Devices 2022, 19, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Diniz, E.; Fontenele, J.; de Oliveira, A.; Bastos, V.; Teixeira, S.; Rabelo, R.; Calcada, D.; dos Santos, R.; de Oliveira, A.; Teles, A. Boamente: A Natural Language Processing-Based Digital Phenotyping Tool for Smart Monitoring of Suicidal Ideation. Healthcare 2022, 10, 698. [Google Scholar] [CrossRef] [PubMed]
- Zahiri, M.; Wang, C.; Gardea, M.; Nguyen, H.; Shahbazi, M.; Sharafkhaneh, A.; Ruiz, I.T.; Nguyen, C.K.; Bryant, M.S.; Najafi, B. Remote Physical Frailty Monitoring—The Application of Deep Learning-Based Image Processing in Tele-Health. IEEE Access 2020, 8, 219391–219399. [Google Scholar] [CrossRef] [PubMed]
- Rovini, E.; Maremmani, C.; Cavallo, F. Automated Systems Based on Wearable Sensors for the Management of Parkinson’s Disease at Home: A Systematic Review. Telemed. e-Health 2019, 25, 167–183. [Google Scholar] [CrossRef] [PubMed]
- Philip, N.Y.; Rodrigues, J.J.P.C.; Wang, H.; Fong, S.J.; Chen, J. Internet of Things for In-Home Health Monitoring Systems: Current Advances, Challenges and Future Directions. IEEE J. Sel. Areas Commun. 2021, 39, 300–310. [Google Scholar] [CrossRef]
- Pap, I.A.; Oniga, S.; Orha, I.; Alexan, A. IoT-Based EHealth Data Acquisition System. In Proceedings of the 2018 IEEE International Conference on Automation, Quality and Testing, Robotics (AQTR), Cluj-Napoca, Romania, 24–26 May 2018; Miclea, L., Stoian, I., Eds.; IEEE: Cluj-Napoca, Romania, 2018. [Google Scholar]
- Pap, I.A.; Oniga, S.; Alexan, A. Machine Learning EEG Data Analysis For EHealth IoT System. In Proceedings of the 2020 IEEE International Conference on Automation, Quality and Testing, Robotics (AQTR), Cluj-Napoca, Romania, 21–23 May 2020; Miclea, L., Stoian, I., Enyedi, S., Stan, O., Stefan, I., Raica, P., Abrudean, M., Valean, H., Sanislav, T., Gota, D., Eds.; IEEE: Cluj-Napoca, Romania, 2020; pp. 143–146. [Google Scholar]
- Hamil, H.; Zidelmal, Z.; Azzaz, M.; Sakhi, S.; Kaibou, R.; Djilali, S.; Abdeslam, D. Design of a Secured Telehealth System Based on Multiple Biosignals Diagnosis and Classification for IoT Application. Expert Syst. 2022, 39, e12765. [Google Scholar] [CrossRef]
- Baird, A.; Xia, Y.; Cheng, Y. Consumer Perceptions of Telehealth for Mental Health or Substance Abuse: A Twitter-Based Topic Modeling Analysis. JAMIA Open 2022, 5, ooac028. [Google Scholar] [CrossRef]
- Fernandez-Luque, L.; Al Herbish, A.; Al Shammari, R.; Argente, J.; Bin-Abbas, B.; Deeb, A.; Dixon, D.; Zary, N.; Koledova, E.; Savage, M. Digital Health for Supporting Precision Medicine in Pediatric Endocrine Disorders: Opportunities for Improved Patient Care. Front. Pediatrics 2021, 9, 715705. [Google Scholar] [CrossRef]
- Chia, M.; Turner, A. Benefits of Integrating Telemedicine and Artificial Intelligence into Outreach Eye Care: Stepwise Approach and Future Directions. Front. Med. 2022, 9, 835804. [Google Scholar] [CrossRef]
- Chong, J.; Tan, C.; Chen, D. Teleophthalmology and Its Evolving Role in a COVID-19 Pandemic: A Scoping Review. Ann. Acad. Med. Singap. 2021, 50, 61–76. [Google Scholar] [CrossRef]
- Ruscelli, A.; Cecchetti, G.; Barsanti, I.; Manciulli, M.; Paolini, P.; Castoldi, P. A Medical Tele-Tutoring System for the Emergency Service. In Proceedings of the 2021 IEEE International Conference on Pervasive Computing and Communications Workshops and other Affiliated Events (PerCom Workshops), Kassel, Germany, 22–26 March 2021; pp. 410–412. [Google Scholar]
- Leclercq, C.; Witt, H.; Hindricks, G.; Katra, R.; Albert, D.; Belliger, A.; Cowie, M.; Deneke, T.; Friedman, P.; Haschemi, M.; et al. Wearables, Telemedicine, and Artificial Intelligence in Arrhythmias and Heart Failure: Proceedings of the European Society of Cardiology: Cardiovascular Round Table. EP Eur. 2022, euac052. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.; Rhee, J.; Guha, A.; Rao, V. Innovation in Precision Cardio-Oncology during the Coronavirus Pandemic and into a Post-Pandemic World. Front. Cardiovasc. Med. 2020, 7, 145. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Bernard, L.; Jorgensen, C.; Dusfour, G.; Pers, Y. The Challenges of Telemedicine in Rheumatology. Front. Med. 2021, 8, 1843. [Google Scholar] [CrossRef]
- Yu, H.; Zhou, Z. Optimization of IoT-Based Artificial Intelligence Assisted Telemedicine Health Analysis System. IEEE Access 2021, 9, 85034–85048. [Google Scholar] [CrossRef]
- Sun, Y.; Lingying, O. Impact of Telemedicine System Automatic Reminder on Outcomes in Women with Gestational Glycosuria. Ethiop. J. Health Dev. 2021, 35, 276–280. [Google Scholar]
- Sanabria-Russo, L.; Serra, J.; Pubill, D.; Verikoukis, C. CURATE: On-Demand Orchestration of Services for Health Emergencies Prediction and Mitigation. IEEE J. Sel. Areas Commun. 2021, 39, 438–445. [Google Scholar] [CrossRef]
- Chew, H.; Achananuparp, P. Perceptions and Needs of Artificial Intelligence in Health Care to Increase Adoption: Scoping Review. J. Med. Internet Res. 2022, 24, e32939. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Fu, G. Artificial Intelligence-Based Family Health Education Public Service System. Front. Psychol. 2022, 13, 898107. [Google Scholar] [CrossRef]
- Velmovitsky, P.; Bevilacqua, T.; Alencar, P.; Cowan, D.; Morita, P. Convergence of Precision Medicine and Public Health into Precision Public Health: Toward a Big Data Perspective. Front. Public Health 2021, 9, 561873. [Google Scholar] [CrossRef]
- Wiljer, D.; Salhia, M.; Dolatabadi, E.; Dhalla, A.; Gillan, C.; Al-Mouaswas, D.; Jackson, E.; Waldorf, J.; Mattson, J.; Clare, M.; et al. Accelerating the Appropriate Adoption of Artificial Intelligence in Health Care: Protocol for a Multistepped Approach. JMIR Res. Protoc. 2021, 10, e30940. [Google Scholar] [CrossRef]
- Alruwaili, F. Artificial Intelligence and Multi Agent Based Distributed Ledger System for Better Privacy and Security of Electronic Healthcare Records. Peerj Comput. Sci. 2020, 6, e323. [Google Scholar] [CrossRef] [PubMed]
- Maathavan, K.; Venkatraman, S. A Secure Encrypted Classified Electronic Healthcare Data for Public Cloud Environment. Intell. Autom. Soft Comput. 2022, 32, 765–779. [Google Scholar] [CrossRef]
- Garcia-Penalvo, F.; Vazquez-Ingelmo, A.; Garcia-Holgado, A.; Sampedro-Gomez, J.; Sanchez-Puente, A.; Vicente-Palacios, V.; Dorado-Diaz, P.; Sanchez, P. Application of Artificial Intelligence Algorithms within the Medical Context for Non-Specialized Users: The CARTIER-IA Platform. Int. J. Interact. Multimed. Artif. Intell. 2021, 6, 46–53. [Google Scholar] [CrossRef]
- Adegbosin, A.; Stantic, B.; Sun, J. Efficacy of Deep Learning Methods for Predicting Under-Five Mortality in 34 Low-Income and Middle-Income Countries. BMJ Open 2020, 10, e034524. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, J. Digital Technologies and Data Science as Health Enablers: An Outline of Appealing Promises and Compelling Ethical, Legal, and Social Challenges. Front. Med. 2021, 8, 647897. [Google Scholar] [CrossRef] [PubMed]
- Murphy, K.; Di Ruggiero, E.; Upshur, R.; Willison, D.; Malhotra, N.; Cai, J.; Malhotra, N.; Lui, V.; Gibson, J. Artificial Intelligence for Good Health: A Scoping Review of the Ethics Literature. BMC Med. Ethics 2021, 22, 14. [Google Scholar] [CrossRef] [PubMed]
- Amin, H.; Weerts, J.; Brunner-La Rocca, H.; Knackstedt, C.; Sanders-van Wijk, S. Future Perspective of Heart Failure Care: Benefits and Bottlenecks of Artificial Intelligence and EHealth. Future Cardiol. 2021, 17, 917–921. [Google Scholar] [CrossRef]
- Blease, C.; Locher, C.; Leon-Carlyle, M.; Doraiswamy, M. Artificial Intelligence and the Future of Psychiatry: Qualitative Findings from a Global Physician Survey. Digit. Health 2020, 6, 2055207620968355. [Google Scholar] [CrossRef]
- Doraiswamy, P.; Blease, C.; Bodner, K. Artificial Intelligence and the Future of Psychiatry: Insights from a Global Physician Survey. Artif. Intell. Med. 2020, 102, 101753. [Google Scholar] [CrossRef]
- Shuaib, A.; Arian, H.; Shuaib, A. The Increasing Role of Artificial Intelligence in Health Care: Will Robots Replace Doctors in the Future? Int. J. Gen. Med. 2020, 13, 891–896. [Google Scholar] [CrossRef]
- Fink, O.; Wang, Q.; Svensen, M.; Dersin, P.; Lee, W.; Ducoffe, M. Potential, Challenges and Future Directions for Deep Learning in Prognostics and Health Management Applications. Eng. Appl. Artif. Intell. 2020, 92, 103678. [Google Scholar] [CrossRef]
- Giovagnoli, M.; Ciucciarelli, S.; Castrichella, L.; Giansanti, D. Artificial Intelligence in Digital Pathology: What Is the Future? Part 2: An Investigation on the Insiders. Healthcare 2021, 9, 1347. [Google Scholar] [CrossRef] [PubMed]
- Mirbabaie, M.; Stieglitz, S.; Frick, N. Artificial Intelligence in Disease Diagnostics: A Critical Review and Classification on the Current State of Research Guiding Future Direction. Health Technol. 2021, 11, 693–731. [Google Scholar] [CrossRef]
- Jabr, Y.; Sandhu, J. Limitations of Health Technology Implementation: A Commentary on “Artificial Intelligence, Regenerative Surgery, Robotics? What Is Realistic for the Future of Surgery?”. Ann. Med. Surg. 2020, 60, 702–703. [Google Scholar] [CrossRef]
- Harmon, D.; Attia, Z.; Friedman, P. Current and Future Implications of the Artificial Intelligence Electrocardiogram: The Transformation of Healthcare and Attendant Research Opportunities. Cardiovasc. Res. 2022, 118, E23–E25. [Google Scholar] [CrossRef]
- Comito, C.; Falcone, D.; Forestiero, A. Current Trends And Practices In Smart Health Monitoring And Clinical Decision Support. In Proceedings of the IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Seoul, Korea, 16–19 December 2020; pp. 2577–2584. [Google Scholar]
- Kocaballi, A.; Ijaz, K.; Laranjo, L.; Quiroz, J.; Rezazadegan, D.; Tong, H.; Willcock, S.; Berkovsky, S.; Coiera, E. Envisioning an Artificial Intelligence Documentation Assistant for Future Primary Care Consultations: A Co-Design Study with General Practitioners. J. Am. Med. Inform. Assoc. 2020, 27, 1695–1704. [Google Scholar] [CrossRef]
- Bar-Lev, S.; Reichman, S.; Barnett-Itzhaki, Z. Prediction of Vaccine Hesitancy Based on Social Media Traffic among Israeli Parents Using Machine Learning Strategies. Isr. J. Health Policy Res. 2021, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, Q.; Ahmad, M. An Enhanced Deep Learning Model for Automatic Face Mask Detection. Intell. Autom. Soft Comput. 2022, 31, 241–254. [Google Scholar] [CrossRef]
- Tanwar, R.; Nandal, N.; Zamani, M.; Manaf, A.A. Pathway of Trends and Technologies in Fall Detection: A Systematic Review. Healthcare 2022, 10, 172. [Google Scholar] [CrossRef]
- Alsalamah, H.A.; Nasser, S.; Alsalamah, S.; Almohana, A.; Alanazi, A.; Alrrshaid, F. Wholesome Coin: A PHealth Solution to Reduce High Obesity Rates in Gulf Cooperation Council Countries Using Cryptocurrency. Front. Blockchain 2021, 4, 654539. [Google Scholar] [CrossRef]
- Bray, L.; Sharpe, A.; Gichuru, P.; Fortune, P.; Blake, L.; Appleton, V. The Acceptability and Impact of the Xploro Digital Therapeutic Platform to Inform and Prepare Children for Planned Procedures in a Hospital: Before and after Evaluation Study. J. Med. Internet Res. 2020, 22, e17367. [Google Scholar] [CrossRef] [PubMed]
| Authors | Work Description | Results | Technologies Employed |
|---|---|---|---|
| [15] | Decentralized, patient-centric healthcare system framework | Interoperability between healthcare platform stakeholders; patients own their data; challenges include the volume of raw clinical data, privacy and security. | Artificial intelligence, blockchain |
| [16] | Virtual coaching system for older adults | Increasing elders’ engagement with a conversational agent-based eHealth platform to provide modern healthcare services to less tech-savvy patients; study limitations include selection bias, lack of personalized content and testing remotely because of COVID-19 restrictions. | Functional demonstrator of eHealth application COUCH |
| [17] | Epileptic seizure prediction embedded system using EEG | Good accuracy with reduced number of electrodes; low power consumption; running on IoT devices; measurements of energy consumption and execution time for processing EEG data segments; EEG data from ambulatory monitoring system with 16 electrodes, 400 Hz sampling rate in 10 min clips. | Texas Instruments MSP432 low-power device, EEG, IoT |
| [18] | System used to identify persons that suffered concussions through EEG analysis | High accuracy of classifier (92.86%); data consisted of 46 recordings with 63 channels, 4–6 min of EEG data; data analysis was challenging. | Artificial intelligence/deep learning model based on long short-term memory (LSTM) |
| [19] | Feature extraction for motor imagery brain–computer interface | New method with good classification accuracy evaluated on two datasets (used 22 EEG channels from the 9 participants included in BCI competition IV dataset 2a and 2b). | Brain–computer interface, novel filters, EEG |
| [20] | Stress monitoring system for everyday use | Hierarchical edge-cloud obtains lower response time by 77.89% and energy consumption by 78.56%; models in the cloud; high computational effort and missing data proved challenging. | Artificial intelligence, CNN, IoT, Wearable IoT |
| [21] | IoT smart eHealth system authentication that preserves privacy | Improved transmission rate resulting in more active users; verified by simulations with NS-3 tool. | Cryptosystem, MAC verification |
| [22] | Body area network-based wearable fall detection system | Efficient system that can analyze substantial amounts of data in real-time; data recorded from an ECG sensor with 3 channels and 4 accelerometer nodes. | Body area network (BAN), acceleration, ECG sensors |
| [23] | A blockchain-based system for detecting medical document changes and notifying patients | The system does not upload medical records but notifies the patients if the documents have been changed. | Blockchain, mobile app development |
| [24] | Fuzzy-based trust management for preventing Sybil attacks on Internet of Medical Things systems | Proposed model recognizes compromised Sybil nodes and declares them malicious; Sybil attacks are difficult to detect. | Internet of Medical Things (IoMT), trust management |
| [25] | Personal health assistant using the Italian language | System with conversational agent that monitors treatments and biological values and is able to suggest doctors; the generated probability dataset can be used for 217 diseases. | Artificial intelligence/machine learning, chatbot, Telegram-based |
| [26] | IoT-based eHealth surveillance system designed for pandemics | Using geographic routing algorithms to monitor persons for health conditions, social distancing, and mask-wearing status. | GPS, Node-RED, Influx, Grafana |
| [27] | A system for analyzing and predicting diabetes mellitus | Tested prediction results on real hospital data collected from 500 patients presenting risk factors of developing diabetes mellitus. | Artificial intelligence/machine learning, K-nearest neighbor |
| [28] | LI-Care system for health monitoring | Cost-efficient monitoring system with GUI offering powerful signal acquisition and processing; data rates of the sensors used in this work are between 120 B/s and 10 KB/s. | LabView, IoT, National Instruments myRIO-1900 |
| Authors | Work Description | Results | Technologies Employed |
|---|---|---|---|
| [29] | Emotional state prediction through machine learning techniques | Personalized models; data collected through eB2 MindCare; 943 users selected; limitations of the study include missing observations and sporadically reported emotional states information. | Artificial intelligence/machine learning, smartphones |
| [30] | Cardiac monitoring system based on smart wearables | Review of real-world use of arrhythmia and other cardiovascular devices | Artificial intelligence, remote patient monitoring, wearables, ECG |
| [31] | Predicting psychotic relapse in patients with schizophrenia spectrum disorders (SSDs) | Better prediction of anomalies in patients with SSDs; 20,137 days of data collected through CrossCheck study; anticipated challenges during deployment. | Artificial intelligence/machine learning, smartphones, Android application CrossCheck |
| [32] | Signal quality assessment algorithm to classify the signal quality of ECG and respiratory | Signal quality classification with good accuracy; challenges: signal quality misjudgment, most SQAs were not conducted by daily life use of wearable devices, best methods are supervised ML models. | Wearable device (SensEco) |
| [33] | Adoption of voice interface technology for patients with heart failure | Higher remote engagement between patients and providers for better heart failure prevention; data from 47 patients; challenges: engagement and ease of use. | Technology based on Amazon’s Alexa voice assistant (Alexa+) with Echo Dot devices; Avatar tablet application (Avatar); |
| [34] | Review on mobile health use in atrial fibrillation | Expert claims ECG, PPG (photoplethysmography) and MCG (mechanocardiography) use in medicine can reduce morbidity. | Wearables for PPG and ECG; handheld devices for MCG, PPG and ECG; remote monitoring |
| [35] | Boamente, a suicidal prediction mobile application | Identifies suicidal ideations from texts originating from a virtual keyboard; dataset built using Twitter API and labeling tweets by psychologists; dataset sharing restricted by Twitter’s policy. | Artificial intelligence/deep learning, neural language processing, digital phenotyping |
| Authors | Work Description | Results | Technologies Employed |
|---|---|---|---|
| [36] | Application capable of remotely screening patients for physical frailty | Using a technology as accessible as a tablet camera, this remote screening solution extracts kinetic features and calculates a frailty index; results were compared with other solutions; dataset built from 11 patients. | Artificial intelligence/deep learning, remote patient monitoring, tablet video recording, video processing |
| [37] | A review of Parkinson’s disease management systems at home | Remote management and automated assessment of Parkinson’s disease wearable systems | Wearables, accelerometers, gyroscopes, mobile apps, web technologies, SSL, SSH, VPN, TLS |
| [38] | A review of IoT in-home health monitoring systems | Presented works offer a wide view over IoT implementations for in-home health monitoring systems | IoT, ambient assisted living, LoraWan, Sigfox, NB-IoT, 3GPP, RESTAPI, ECG and other medical sensors, Zigbee, Bluetooth, BLE, NFC, RFID, etc. |
| [41] | Secured telehealth system for IoT capable of biosignals diagnosis | The system can handle multiple types of sensors through an Arduino board; a Raspberry Pi 3 model B+ is used for processing the data; uses 4 Physiobank databases: MIT-BIH Arrhythmia, MIT-BIH Normal Sinus Rhythm, BIDMC Congestive Heart Failure and MIT-BIH AF. | Artificial intelligence/machine learning, C# app, EEG, Xbee modules, e-Health sensor platform, Raspberry Pi |
| [42] | Mental health and substance abuse telehealth | Researchers analyzed tweets and concluded there were 4 times more tweets relating to mental health and substance abuse during the pandemic compared to before; data cleaning was challenging because some originated from organizations; selected 10,689 tweets. | Artificial intelligence / machine learning, natural language processing, social media, Twitter |
| [43] | Review relating to telehealth in pediatric endocrine disorders | Precision medicine; growth hormone therapy; diabetes patient care. | Artificial intelligence, IoT, specialized devices to deliver injections that use a web platform |
| Authors | Work Description | Results | Technologies Employed |
|---|---|---|---|
| [44] | Telemedicine solution for eyecare in remote Western Australia | Shorter patient waiting time for first consultation, reduction in costs, availability in remote regions, detecting multiple conditions remotely; faced logistical and geographical challenges; | Artificial intelligence, video conferencing, store and forward methods |
| [45] | A review about the evolving role of teleophthalmology in a COVID-19 pandemic | Describes the use of teleophthalmology, expanding [44]. | Artificial intelligence, video conferencing |
| [46] | A telemedicine system used to offer emergency assistance through a wearable helmet | The REC-VISIO 118 is used daily in the 118 Emergency Service of Pistoia on COVID-19 suspects; video data are transmitted via the 4G network. | Artificial intelligence/machine learning, WebRTC, webcam video recording and transmission, image stabilization, IoT (system based on Raspberry Pi 3), 4G communication |
| [47] | A review discussing cardiovascular problems offering telemedicine solutions | Various solutions are discussed, presenting advantages, challenges and solutions for digital health tools. | Artificial intelligence/machine learning, various wearables |
| [48] | Review regarding cardio-oncology patient care during COVID-19 | Presents possible ways of using big data, social media and AI to provide care for cancer survivors, because cardiovascular diseases are the second cause of death among this group. | Artificial intelligence/machine learning, social media, big data |
| [49] | Review about rheumatology challenges in telemedicine | Advantages and shortcomings of telemedicine in rheumatology, some studies even showing that telemedicine did not reduce the face-to-face consultations. | Artificial intelligence/machine learning, mobile applications, wearables, remote patient monitoring |
| [50] | Telemedicine health analysis system based on IoT | The researchers propose a cloud IoT architecture to improve the connection between health IoT and people, providing detailed analysis of different layers; challenges associated with big data management and processing. | Artificial intelligence, IoT, quality of service framework, quality of experience, cloud |
| [51] | Research the effect of telemedicine on gestational diabetic patients | A reminder system and telephone access were used to improve healthcare efficiency, while having little to no impact on the blood glucose levels; difficulties with computer access and low-income families; dataset of 80 patients equally split in intervention and randomizing dot control groups. | Short message service (SMS), interactive voice response (IVR) |
| [52] | On-demand orchestration of services for health emergency predictions | The CURATE system supports scaling to better respond to rising simultaneous prediction requests received from the edge; work presents benefits of continuous IoT health monitoring via 5G service orchestration two-tiered platform (edge-cloud); system used time series data from two ECG channels; training phase consists of 10 epochs of 200 steps; | Network Functions Virtualization Management and Orchestration (NFV MANO), 5G Public–Private Partnership Infrastructure Association, Cloud/Edge, Tensorflow/Keras (Python) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pap, I.A.; Oniga, S. A Review of Converging Technologies in eHealth Pertaining to Artificial Intelligence. Int. J. Environ. Res. Public Health 2022, 19, 11413. https://doi.org/10.3390/ijerph191811413
Pap IA, Oniga S. A Review of Converging Technologies in eHealth Pertaining to Artificial Intelligence. International Journal of Environmental Research and Public Health. 2022; 19(18):11413. https://doi.org/10.3390/ijerph191811413
Chicago/Turabian StylePap, Iuliu Alexandru, and Stefan Oniga. 2022. "A Review of Converging Technologies in eHealth Pertaining to Artificial Intelligence" International Journal of Environmental Research and Public Health 19, no. 18: 11413. https://doi.org/10.3390/ijerph191811413






