Subcutaneous Implantable Cardioverter Defibrillators for the Prevention of Sudden Cardiac Death: Pediatric Single-Center Experience
Abstract
:1. Introduction
2. Materials and Methods
3. Results
- A 17-year-old male patient with hypertrophic cardiomyopathy with left ventricular outflow tract obstruction (HCM with LVOTO). Echocardiography revealed the following: significant degree of concentric myocardial hypertrophy, LVOTO with maximal systolic pressure gradient LV-Ao 108–112 mmHg, and mean pressure gradient 55 mmHg.
- A 17-year-old male patient with heart failure in the course of dilated cardiomyopathy, with gradually worsening left ventricular function and coexisting complex ventricular arrhythmia (VT episodes up to 170/min) and ventricular tachycardia (VT) with celiac disease, congenital IgA deficiency, and history of renal failure episode. The patient was qualified for heart transplant and LVAD (left ventricular assist device). A HeartMate 3 was implanted for left ventricular support as a bridge for heart transplantation. At the time of publication, the patient has not yet received a heart transplant. He is doing well, helps with lighter household chores, meets with friends, has a girlfriend, and describes his quality of life as satisfactory (Figure 1).
- A 17-year-old male patient with hypertrophic cardiomyopathy, obesity, insulin resistance, and arterial hypertension. Echocardiography revealed asymmetric LV hypertrophy and LV outflow tract obstruction with systolic pressure gradient LV-Ao up to 70 mmHg and complete obliteration of LV lumen during systole, hyperkinesis of both ventricles, mitral insufficiency, and left atrial enlargement. Non-sustained ventricular tachycardia (nsVT) was recorded in Holter ECG monitoring. During screening, correct sensing parameters were obtained for the electrode located on the right side of the sternum (Figure 2).
- 4.
- A 17-year-old male patient with dilated cardiomyopathy and severe heart failure, who was qualified for heart transplant. In echocardiography, significantly enlarged LV with impaired global myocardial contractility—LV EF 10–25%—and enlarged LA were found. CMR showed no signs of active or previous myocarditis, decreased left ventricular (EF 13%) and right ventricular (EF 16%) contractility, and myocardial fibrosis. In addition, imaging examinations revealed thrombus in the apical part of the left ventricle and treatment with low-molecular-weight heparin was introduced at a therapeutic dose, which led to regression of the lesion. Due to lack of thrombus in follow-up examination, defibrillation testing (DFT) was performed. Ten months after S-ICD implantation, the patient died of circulatory failure in the course of COVID-19 pneumonia. At the parents’ request, the device was not collected after the boy’s death. Reading was not possible due to epidemiological reasons.
- 5.
- A 17-year-old female patient with hypertrophic cardiomyopathy and pre-excitation in ECG (after two-fold RF ablation—radiofrequency catheter ablation), treated with Sotalol, in whom genetic testing revealed heterozygous deletion in the LAMP2 region typical for Danon disease. The findings of the echocardiographic examination were as follows: features of hypertrophic cardiomyopathy, LV diastolic dysfunction, borderline size of LA, and normal LV contractility. CMR showed the presence of a parietal LV thrombus, LV myocardial fibrosis, mixed hypertrophic cardiomyopathy, and LV myocardial noncompaction with normal LV contractility. ECG monitoring reported episodes of ventricular tachycardia and multiple narrow QRS complex tachycardias. Due to the presence of thrombus, no defibrillation test was performed.
- 6.
- A 16-year-old male patient with hypertrophic cardiomyopathy, whose echocardiographic examination showed extreme concentric left ventricular hypertrophy and almost complete obliteration of the ventricular lumen in systole. In CMR, visible signs of edema within LV myocardium and diffuse areas of myocardial fibrosis/necrosis of non-ischemic etiology were revealed. Self-limiting ventricular tachycardia and prolonged QT with a mean QTc 460 ms were recorded in Holter monitoring.
- 7.
- A 17-year-old male patient with complex ventricular arrhythmia and arrhythmogenic right ventricular cardiomyopathy. Holter monitoring revealed PVCs with increasing tendency (including single VEBs, 10% pairs of ventricular extrasystoles, and VT episodes). Positive family history—the boy’s brother died suddenly at age 13 years and the boy’s father died at age 40 years. In echocardiography, RV within the upper limit of normal, convex RV free wall, thick septo-marginal trabecula and increased trabeculation of the apical part of the right ventricle, and preserved systolic function of the right ventricle were found. The main criteria for the diagnosis of arrhythmogenic right ventricular cardiomyopathy (segmental wall dyskinesis, enlarged RV > 110 mL/m2, EF < 40%) in CMR were fulfilled.
- 8.
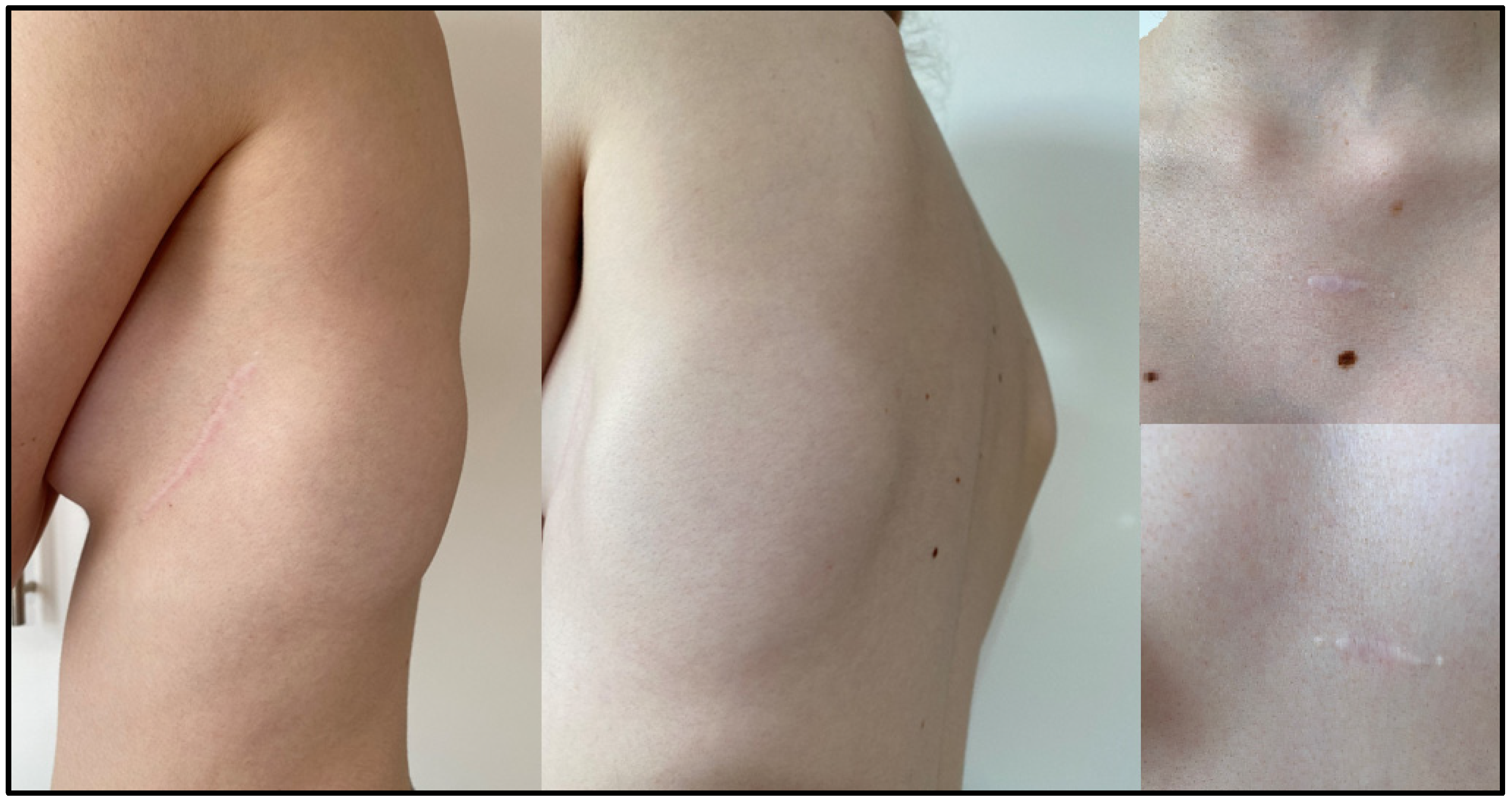
- A 14-year-old female patient, successfully defibrillated with an Automated External Defibrillator (AED) after outpatient cardiac arrest. The incident took place in a mall while shopping. Ventricular fibrillation was documented in AED records. Imaging examinations (ECHO) showed normal morphology of the heart structures. Diagnostic tests toward channelopathy were performed: no signs of prolonged QT were found in a series of ECG tests. Exercise stress test was negative—there was no arrythmia during the test and QTc in the 4th minute of rest was normal. Subsequently, a drug provocation test was conducted with adrenaline and ajmaline—both were negative. Therefore, idiopathic ventricular fibrillation was diagnosed. Beta-blocker treatment was introduced with good drug tolerance. The patient was very slim and implantation was technically difficult, but the cosmetic effect was very good (Figure 3 and Figure 4).
- 9.
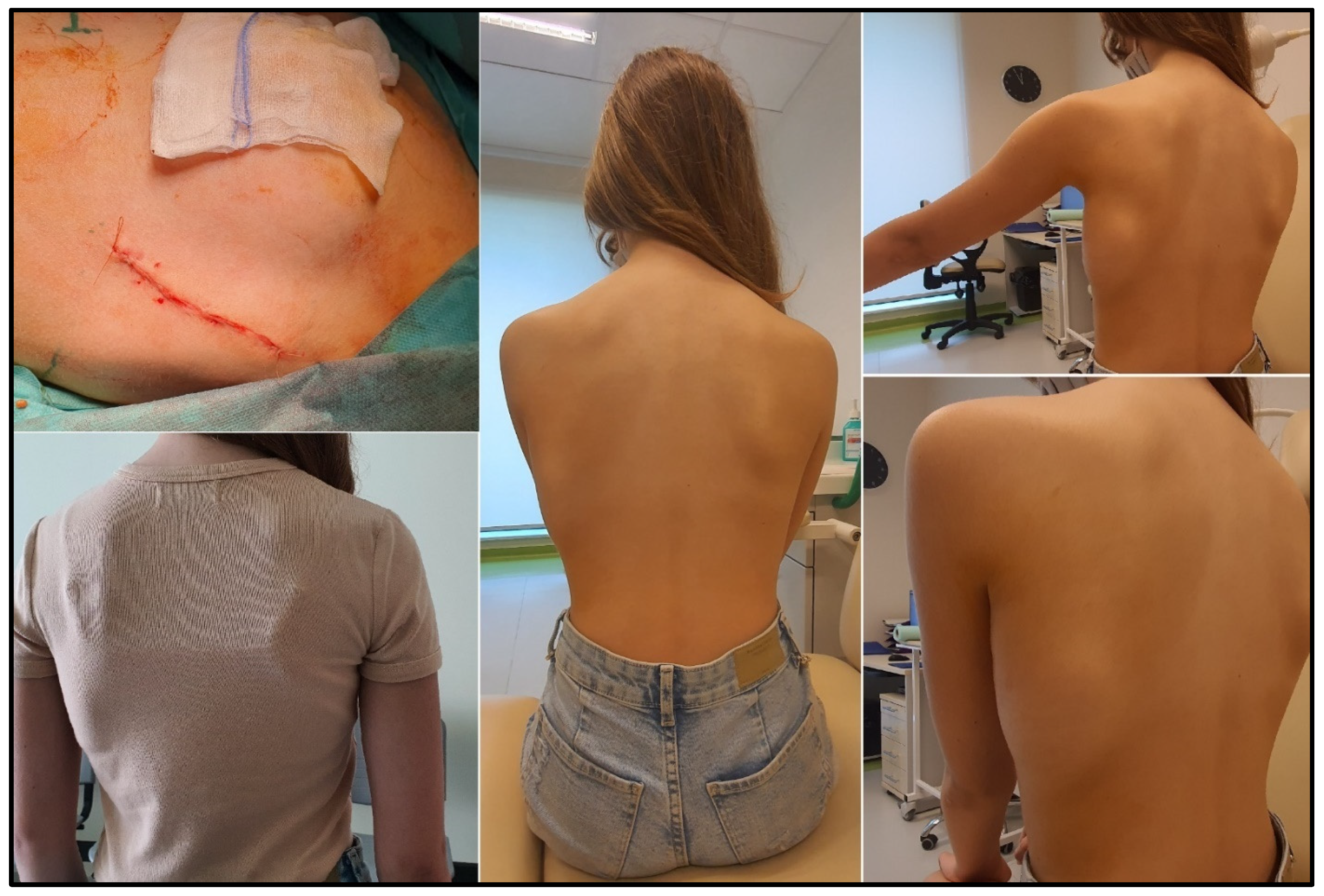
- A 12-year-old female patient with long QT syndrome (5 points on the Schwartz scale), confirmed by genetic testing, treated with propranolol. While playing in a pool (despite the ban, she bathed and played ball in the pool), the girl lost consciousness for about 2 min. The loss of consciousness was sudden and was not preceded by palpitations or a feeling of weakness, visual disturbances, or dizziness. During the period of unconsciousness, the girl first presented with tautness; she was pale, limp, and did not respond to stimuli. After being taken out of the pool, she was still unconscious, without a pulse. After consciousness returned, there was no confusion or excessive sleepiness. Since then, QTc 0.46–0.5 s has been observed. The girl’s older brother is also a patient of the Clinic; he was diagnosed with LQTS, which was genetically confirmed. During the course of diagnosis of both children, their mother was also diagnosed with prolongation of QT interval, as well as their grandmother. During the girl’s exercise stress test, QTc at the 4th minute after exercise was 0.49 s. Due to her very slim body structure and low weight (38 kg), the procedure was technically difficult, but it was possible to create an intramuscular pocket. The procedure was performed using a two-incision technique. There were no complications. On day 2, the patient was mobilized, and after about a week during a control visit, she presented without pain with almost the entire range of left-hand movement was recovered (Figure 5).
- 10.
- A 16-year-old male patient with sudden cardiac arrest that occurred at school during a sports lesson—the child collapsed without any warning symptoms after having performed physical activity. The teacher started CPR. At the scene of the incident, paramedics diagnosed the boy with ventricular fibrillation and performed defibrillation three times, restoring the sinus rhythm. Family history of SCD was negative. ECG showed normal sinus rhythm, with normal QTc and early repolarization features in leads II, III, aVF, V5, and V6. Holter monitoring ECG showed no arrhythmia. ECHO showed normal LV size and contractility. An exercise treadmill test was performed—no arrhythmia was observed with normal QTc at 4 min of rest. ECG with high right ventricular leads and provocative test with flecainide were performed and were both negative. Angio CT of the coronary arteries revealed a muscular bridge over the course of the left anterior descending coronary artery without narrowing in coronarography with nitroglycerines, with no ischemic features and no myocardial edema in CMR.
- 11.
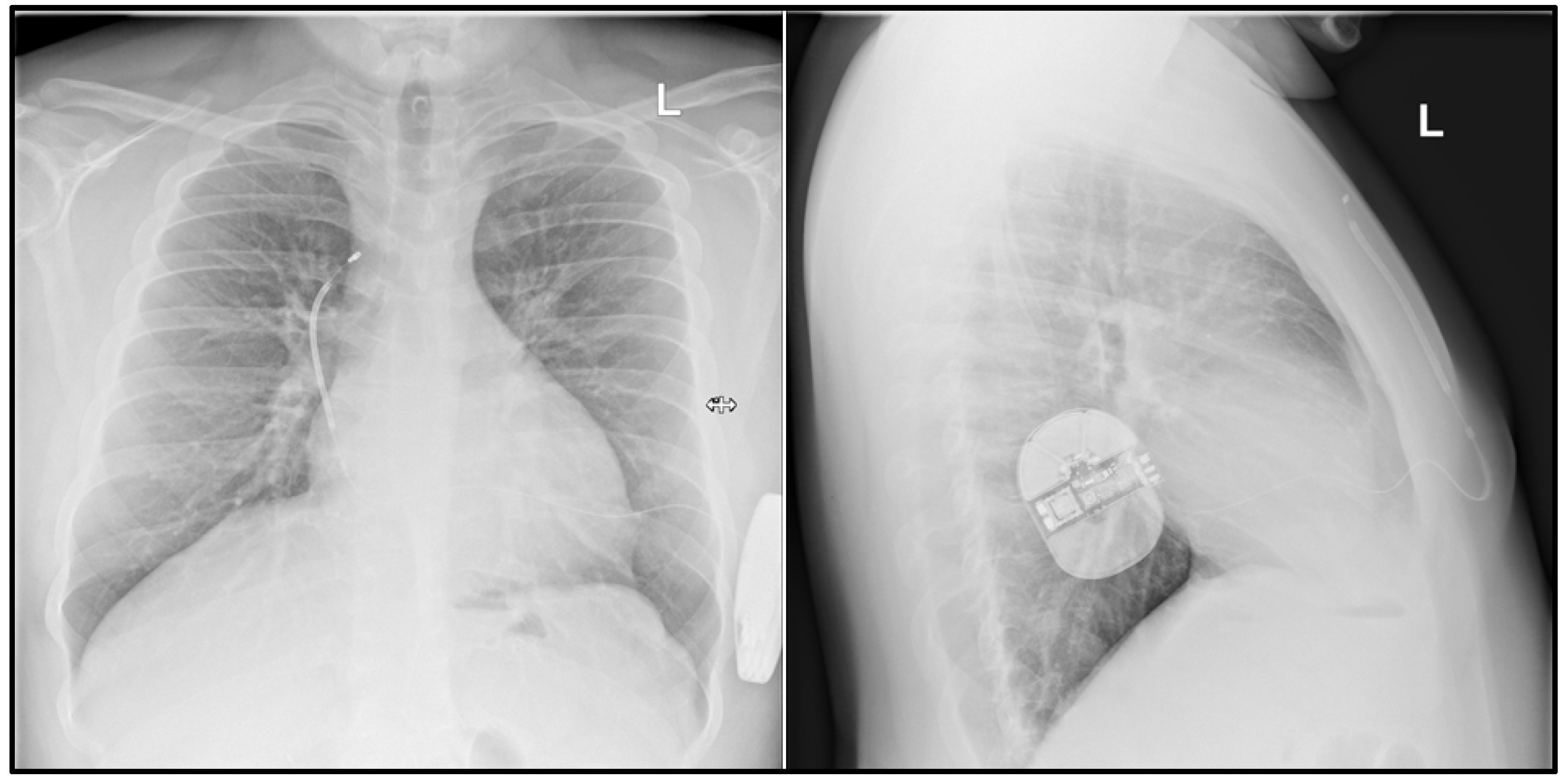
- A 16-year-old male patient diagnosed with Brugada syndrome, implanted with an ICD system, qualified for S-ICD implantation due to battery depletion and increasing defibrillation lead resistance. He had a history of several episodes of unconsciousness up to the age of 3 years and, at age 9 years, during an episode of SCA, the boy lost consciousness on the beach; he was assisted by a cardiologist present there, who started CPR. During hospitalization after the episode, he was diagnosed with Brugada syndrome. He was implanted with an ICD and one year after implantation, there was an episode of adequate defibrillation. It was decided that the transvenous system would be temporarily left and an S-ICD device implanted and, after healing, a decision would be made on the intracardiac lead removal.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Priori, S.G.; Blomström-Lundqvist, C.; Mazzanti, A.; Blom, N.; Borggrefe, M.; Camm, J.; Elliott, P.M.; Fitzsimons, D.; Hatala, R.; Hindricks, G.; et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 2015, 36, 2793–2867. [Google Scholar] [PubMed]
- Schneider, A.E.; Burkhart, H.M.; Ackerman, M.J.; Dearani, J.A.; Wackel, P.; Cannon, B.C. Minimally invasive epicardial implantable cardioverter-defibrillator placement for infants and children: An effective alternative to the transvenous approach. Heart Rhythm 2016, 13, 1905–1912. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, M.; Gawałko, M.; Michalak, M.; Cacko, A.; Kowara, M.; Kołodzińska, A.; Januszkiewicz, Ł.; Balsam, P.; Serdoz, L.V.; Winter, J.; et al. Initial experience with the subcutaneous implantable cardioverter-defibrillator with the real costs of hospitalization analysis in a single Polish center. Cardiol. J. 2019, 26, 360–367. [Google Scholar] [CrossRef]
- Kaczmarek, K.; Kempa, M.; Grabowski, M.; Tajstra, M.; Sokal, A.; Cygankiewicz, I.; Zwoliński, R.; Michalak, M.; Kowara, M.; Budrejko, S.; et al. Multicentre early experience with totally subcutaneous cardioverter-defibrillators in Poland. Arch. Med. Sci. 2020, 16, 764–771. [Google Scholar] [CrossRef]
- Sadownik, B.; Nowakowski, P.; Michalak, M.; Andruszkiewicz, P.; Grabowski, M. Regional anesthesia of the hemithorax for the implantation of a subcutaneous implantable cardioverter-defibrillator (S-ICD). Kardiologia Polska 2020, 78, 592–593. [Google Scholar] [CrossRef] [PubMed]
- Joy, P.S.; Kumar, G.; Poole, J.E.; London, B.; Olshansky, B. Cardiac implantable electronic device infections: Who is at greatest risk? Heart Rhythm 2017, 14, 839–845. [Google Scholar] [CrossRef]
- McLeod, C.J.; Boersma, L.; Okamura, H.; Friedman, P.A. The subcutaneous implantable cardioverter defibrillator: State-of-the-art review. Eur. Heart J. 2015, 38, 247–257. [Google Scholar] [CrossRef]
- Bardy, G.H.; Smith, W.M.; Hood, M.A.; Crozier, I.G.; Melton, I.C.; Jordaens, L.; Theuns, D.; Park, R.E.; Wright, D.J.; Connelly, D.T.; et al. An Entirely Subcutaneous Implantable Cardioverter–Defibrillator. New Engl. J. Med. 2010, 363, 36–44. [Google Scholar] [CrossRef]
- Kaczmarek, K.; Zwoliński, R.; Bartczak, K.; Ptaszynski, P.; Wranicz, J.K. A subcutaneous implantable cardioverter-defibrillator—The first implantation in Poland. Kardiologia Polska 2015, 73, 62. [Google Scholar] [CrossRef]
- Winter, J.; Siekiera, M.; Shin, D.-I.; Meyer, C.; Kröpil, P.; Clahsen, H.; O’Connor, S. Intermuscular technique for implantation of the subcutaneous implantable cardioverter defibrillator: Long-term performance and complications. Europace 2016, 19, 2036–2041. [Google Scholar] [CrossRef]
- Lewandowski, M.; Syska, P.; Kowalik, I. Children and young adults treated with transvenous and subcutaneous implantable cardioverter-defibrillators: A 22-year single-center experience and new perspectives. Kardiol. Pol. 2020, 78, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Boersma, L.; Barr, C.; Knops, R.; Theuns, D.; Eckardt, L.; Neuzil, P.; Scholten, M.; Hood, M.; Kuschyk, J.; Jones, P.; et al. Implant and Midterm Outcomes of the Subcutaneous Implantable Cardioverter-Defibrillator Registry: The EFFORTLESS Study. J. Am. Coll. Cardiol. 2017, 70, 830–841. [Google Scholar] [CrossRef] [PubMed]
- Basu-Ray, I.; Liu, J.; Jia, X.; Gold, M.; Ellenbogen, K.; DiNicolantonio, J.; Komócsi, A.; Vorobcsuk, A.; Kim, J.; Afshar, H.; et al. Subcutaneous Versus Transvenous Implantable Defibrillator Therapy: A Meta-Analysis of Case-Control Studies. JACC Clin. Electrophysiol. 2017, 3, 1475–1483. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, T.F.; Yilmaz, D.; Lindeboom, R.; Buiten, M.S.; Nordkamp, L.R.O.; Schalij, M.J.; Wilde, A.A.; van Erven, L.; Knops, R.E. Long-Term Clinical Outcomes of Subcutaneous Versus Transvenous Implantable Defibrillator Therapy. J. Am. Coll. Cardiol. 2016, 68, 2047–2055. [Google Scholar] [CrossRef] [PubMed]
- Bogush, N.; Espinosa, R.E.; Cannon, B.C.; Wackel, P.L.; Okamura, H.; Friedman, P.A.; McLeod, C.J. Selecting the right defibrillator in the younger patient: Transvenous, epicardial or subcutaneous? Int. J. Cardiol. 2018, 250, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Jarman, J.W.E.; Lascelles, K.; Wong, T.; Markides, V.; Clague, J.R.; Till, J. Clinical experience of entirely subcutaneous implantable cardioverter-defibrillators in children and adults: Cause for caution. Eur. Heart J. 2012, 33, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Von Alvensleben, J.C.; Dechert, B.; Bradley, D.J.; Fish, F.A.; Moore, J.P.; Pilcher, T.A.; Escudero, C.; Ceresnak, S.R.; Kwok, S.Y.; Balaji, S.; et al. Subcutaneous Implantable Cardioverter-Defibrillators in Pediatrics and Congenital Heart Disease: A Pediatric and Congenital Electrophysiology Society Multicenter Review. JACC Clin. Electrophysiol. 2020, 6, 1752–1761. [Google Scholar] [CrossRef]
- Bettin, M.; Larbig, R.; Rath, B.; Fischer, A.; Frommeyer, G.; Reinke, F.; Köbe, J.; Eckardt, L. Long-Term Experience with the Subcutaneous Implantable Cardioverter-Defibrillator in Teenagers and Young Adults. JACC Clin. Electrophysiol. 2017, 3, 1499–1506. [Google Scholar] [CrossRef]
- Silvetti, M.S.; Pazzano, V.; Verticelli, L.; Battipaglia, I.; Saputo, F.A.; Albanese, S.; Lovecchio, M.; Valsecchi, S.; Drago, F. Subcutaneous implantable cardioverter-defibrillator: Is it ready for use in children and young adults? A single-centre study. Europace 2018, 20, 1966–1973. [Google Scholar] [CrossRef]
- Quast, A.B.E.; Brouwer, T.F.; Kooiman, K.M.; van Dessel, P.F.H.M.; Blom, N.A.; Wilde, A.A.M.; Knops, R.E. Comparison of complications and shocks in paediatric and young transvenous and subcutaneous implantable cardioverter-defibrillator patients. Neth. Heart J. 2018, 26, 612–619. [Google Scholar] [CrossRef] [Green Version]
- Mitacchione, G.; Schiavone, M.; Gasperetti, A.; Viecca, M.; Curnis, A.; Forleo, G.B. Neglected lead tip erosion: An unusual case of S-ICD inappropriate shock. J. Cardiovasc. Electrophysiol. 2020, 31, 3322–3325. [Google Scholar] [CrossRef] [PubMed]


| No. of Patient | Sex | Age (Years) | Weight | Height | Indications for S-ICD | SCD Prevention | Prior CIED | NYHA Class | ECHO | CMR | Arrythmia | Indication for Pacing |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | M | 17 | 65 | 188 | HCM, LVOTO | Primary | No | - | LVEF 82% LVPWd 17–21 mm (n do 10.2). IVSd 22.8 mm (n do 10.7), LVOTO: max. 108–115; mean 55 mmHg | Fibrosis present Max LV: 28 mm IVS: 22 mm | PVCs | No |
| 2. | M | 17 | 50 | 168 | DCM, HF | Primary | No | Chronic HF; NYHA III; LVAD HeartMate3; Patient qualified for HTx | LVEF 24–28% | LVEF = 18%. Scattered areas of LV myocardial fibrosis/necrosis of non-ischemic aetiology | nsVT 130-170/min. | No |
| 3. | M | 16 | 123 | 177 | HCM, LVOTO | Primary | No | - | IVSd 24.3 mm, LVPWd 22.8 mm.; LVOTO 70 mmHg; IAo IIst. | Heterogenous myocardial structure, without areas of fibrosis/necrosis | PVCs | No |
| 4. | M | 17 | 67 | 166 | DCM; HF | Primary | No | Chronic HF; NYHA III; Patient qualified for HTx | LVEF 10–15–25% IMV I/II st. ITV I/II st. | LVEF 13% RVEF 16% Fibrosis of myocardium present | nsVT | No |
| 5. | F | 17 | 76 | 170 | HCM + LVNC Danon disease | Primary | No | - | IVSd 20 mm, LVPWd 16 mm | Mixed cardiomyopathy—HCM and LVNC | nsVT | No |
| 6. | M | 16 | 88 | 178 | HCM | Primary | No | - | IVSd 47.2 mm, LVPWd 29 mm | LV max 35 mm; IVS 48 mm Sings of myocardial edema in LV and scattered areas of fibrosis/necrosis of non-ischemic aetiology | nsVT | No |
| 7. | M | 17 | 73 | 177 | ARVC | Primary | no | right ventricle to the upper limit of normal—RV-EDV in ECHO 3D 194 mL (102 mL/m2) vs. LVEDV 174 mL. | large resonance criteria for the diagnosis of ARVC (segmental wall dyskinesia, increased RV > 110 mL/m2, EF < 40%). | PVCs, VT | ||
| 8. | F | 14 | 47 | 168 | SCA; VF | Secondary | No | - | PMV | no abnormalities | PVC, TdP, VT, IVF | No |
| 9. | F | 12 | 38 | 152 | LQTS | Secondary | No | - | no abnormalities | no abnormalities | Not found | No |
| 10. | M | 16 | 68 | 173 | SCA; VF | Secondary | No | - | no abnormalities | Generalized edema probably related to resuscitation. On follow-up no evidence of edema | Not found | No |
| 11. | M | 16 | 58 | 172 | Brugada syndrome; SCA | Secondary | Yes | - | bicuspid aortic valve | - | VT | No |
| No. of Patient | Anaesthesia | Physicians * | X-rays ** | S-ICD Pocket | Incisions | S-ICD Test | Time *** | Operative Time | Complication |
|---|---|---|---|---|---|---|---|---|---|
| 1. | General | CS, EP, CS * | Yes | Intermucsular | 3 | Yes 1st Effective (65 J) | 150 | 60 | None |
| 2. | General | CS, EP, PC * | Yes | Intermucsular | 3 | Yes 1st Effective (65 J) | 120 | 50 | None |
| 3. | General | CS, PC, EP * | Yes | Intermucsular | 3 | 2nd Effective (65 J rev.) | 120 | 45 | None |
| 4. | General | CS, PC, EP * | Yes | Intermucsular | 3 | Yes 1st Effective (65 J) | 90 | 40 | None |
| 5. | General | CS, PC, EP * | Yes | Intermucsular | 3 | No | 120 | 50 | None |
| 6. | General | CS, PC, EP * | Yes | Intermucsular | 3 | Yes 1st Effective (65 J) | 60 | 30 | None |
| 7. | General | CS, PC, EP * | No | Intermucsular | 3 | Yes 1st Effective (65 J) | 100 | 30 | None |
| 8. | General | CS, PC, EP * | Yes | Intermucsular | 3 | Yes 1st Effective (65 J) | 150 | 55 | None |
| 9. | General | CS, PC, EP * | Yes | Intermucsular | 2 | Yes 1st Effective (65 J) | 90 | 45 | None |
| 10. | General | CS, PC, EP * | Yes | Intermucsular | 2 | Yes 1st Effective (65 J) | 70 | 30 | None |
| 11. | General | CS, PC, EP * | Yes | Intermucsular | 3 | Yes 1st Effective (65 J) | 110 | 40 | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wieniawski, P.; Buczyński, M.; Grabowski, M.; Winter, J.; Werner, B. Subcutaneous Implantable Cardioverter Defibrillators for the Prevention of Sudden Cardiac Death: Pediatric Single-Center Experience. Int. J. Environ. Res. Public Health 2022, 19, 11661. https://doi.org/10.3390/ijerph191811661
Wieniawski P, Buczyński M, Grabowski M, Winter J, Werner B. Subcutaneous Implantable Cardioverter Defibrillators for the Prevention of Sudden Cardiac Death: Pediatric Single-Center Experience. International Journal of Environmental Research and Public Health. 2022; 19(18):11661. https://doi.org/10.3390/ijerph191811661
Chicago/Turabian StyleWieniawski, Piotr, Michał Buczyński, Marcin Grabowski, Joachim Winter, and Bożena Werner. 2022. "Subcutaneous Implantable Cardioverter Defibrillators for the Prevention of Sudden Cardiac Death: Pediatric Single-Center Experience" International Journal of Environmental Research and Public Health 19, no. 18: 11661. https://doi.org/10.3390/ijerph191811661
APA StyleWieniawski, P., Buczyński, M., Grabowski, M., Winter, J., & Werner, B. (2022). Subcutaneous Implantable Cardioverter Defibrillators for the Prevention of Sudden Cardiac Death: Pediatric Single-Center Experience. International Journal of Environmental Research and Public Health, 19(18), 11661. https://doi.org/10.3390/ijerph191811661







