The Malaysian HEalth and WellBeing AssessmenT (MyHEBAT) Study Protocol: An Initiation of a National Registry for Extended Cardiovascular Risk Evaluation in the Community
Abstract
:1. Introduction
2. The Rationale of the Study
3. Malaysian Health and Wellbeing Assessment (MyHEBAT)
3.1. MyHEBAT Aims and Objectives
3.2. MyHEBAT Cardiovascular Risk Epidemiological Study (MyHEBAT-CRES)
3.3. MyHEBAT Familial Hypercholesterolaemia Study (MyHEBAT-FH)
4. Methods
4.1. Study Design and Population
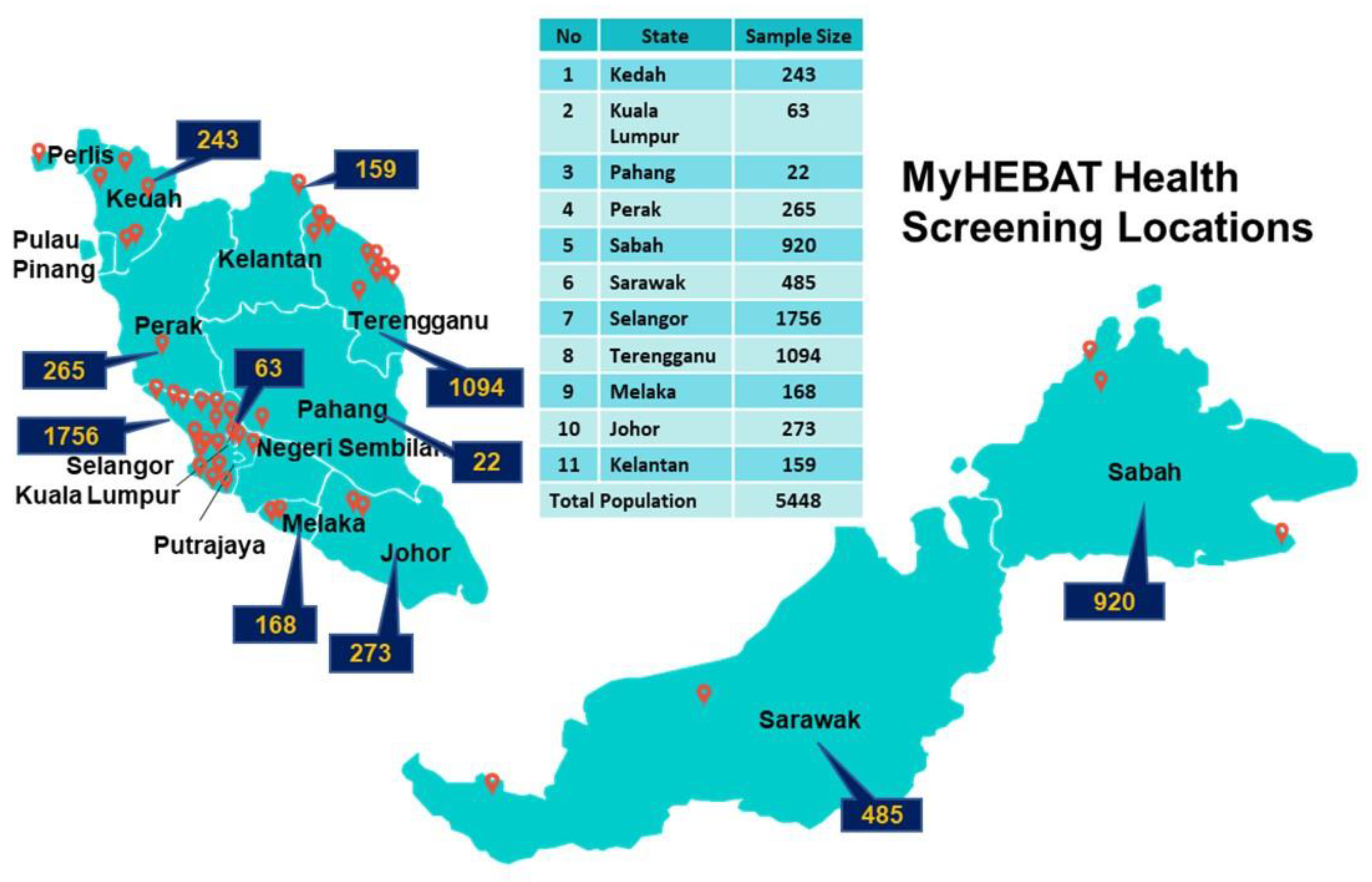
4.2. Sampling Methods: State and Site Selection
4.3. Sampling Methods: Subject Recruitment
4.4. Definitions of Study Variables
4.5. Cardiovascular Disease Risk Stratification
4.6. Familial Hypercholesterolaemia
4.7. Study Procedures
4.7.1. Blood Collection and Laboratory Analysis
4.7.2. Statistical Analysis Plan
4.7.3. Patient Management
5. Discussion
Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APOB | Apolipoprotein B |
| ASCVD | Atherosclerotic cardiovascular disease |
| BP | Blood pressure |
| BMI | Body mass index |
| CVD | Cardiovascular disease |
| CO | Central obesity |
| CPG | Clinical Practice Guidelines |
| CAD | Coronary artery disease |
| CRES | Coronary Risk Epidemiological Study |
| DM | Diabetes mellitus |
| DNA | Deoxyribonucleic acid |
| DLCN | Dutch Lipid Clinic Network Criteria |
| EDTA | Ethylenediaminetetraacetic acid |
| ESC/EAS | European Society of Cardiology/European Atherosclerosis Society |
| FH | Familial hypercholesterolaemia |
| FPG | Fasting plasma glucose |
| FRS-CVD | Framingham Risk Score Cardiovascular Disease |
| HDL-C | High-density lipoprotein cholesterol |
| HTG | Hypertriglyceridaemia |
| HC | Hypercholesterolaemia |
| HPT | Hypertension |
| IQR | Interquartile range |
| JFHMC | Japanese Familial Hypercholesterolaemia Management Criteria |
| Lp (a) | Lipoprotein (a) |
| LLD | Lipid lowering drug |
| LDL-C | Low-density lipoprotein cholesterol |
| MyHEBAT | Malaysian Health and Wellbeing Assessment |
| NHMS | National Health and Morbidity Survey |
| NSP-NCD | National Strategic Plan for Non-Communicable Diseases |
| PVD | Peripheral vascular disease |
| PCSK9 | Proprotein convertase subtilisin/kexin type 9 |
| RPG | Random plasma glucose |
| SB | Simon Broome’s Register Criteria |
| SD | Standard deviation |
| SCORE | Systematic Coronary Risk Estimation |
| TC | Total cholesterol |
| TG | Triglyceride |
| USMEDPED | United States Make Early Diagnosis to Prevent Early Deaths Criteria |
| WC | Waist circumference |
Appendix A. Malaysian HEalth and Well-Being AssessmenT (MyHEBAT) Research Investigators
References
- Stenling, A.; Häggström, C.; Norberg, M.; Norström, F. Lifetime Risk Predictions for Cardiovascular Diseases: Competing Risks Analyses on a Population-Based Cohort in Sweden. Atherosclerosis 2020, 312, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Vandersmissen, G.J.M.; Schouteden, M.; Verbeek, C.; Bulterys, S.; Godderis, L. Prevalence of High Cardiovascular Risk by Economic Sector. Int. Arch. Occup. Environ. Health 2020, 93, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Borhanuddin, B.; Nawi, A.M.; Shah, S.A.; Abdullah, N.; Zulkifli, S.; Zakaria, S.; Kamaruddin, M.A.; Velu, C.S.; Ismail, N.; Abdullah, M.S.; et al. 10-Year Cardiovascular Disease Risk Estimation Based on Lipid Profile-Based and BMI-Based Framingham Risk Scores across Multiple Sociodemographic Characteristics: The Malaysian Cohort Project. Sci. World J. 2018, 2018, 2979206. [Google Scholar] [CrossRef] [PubMed]
- Negesa, L.B.; Magarey, J.; Rasmussen, P.; Hendriks, J.M.L. Patients’ Knowledge on Cardiovascular Risk Factors and Associated Lifestyle Behaviour in Ethiopia in 2018: A Cross-Sectional Study. PLoS ONE 2020, 15, e0234198. [Google Scholar] [CrossRef]
- Ahmed, A.A.A.; Al-Shami, A.M.; Jamshed, S.; Zawiah, M.; Elnaem, M.H.; Ibrahim, M.I.M. Awareness of the Risk Factors for Heart Attack among the General Public in Pahang, Malaysia: A Cross-Sectional Study. Risk Manag. Healthc. Policy 2020, 13, 3089–3102. [Google Scholar] [CrossRef]
- Ismail, N.H.; Rosli, N.M.; Mahat, D.; Yusof, K.H.; Ph, M. Cardiovascular Risk Assessment between Urban and Rural Population in Malaysia. Med. J. Malays. 2016, 71, 331–337. [Google Scholar]
- National Institutes of Health; Ministry of Health Malaysia. National Health and Morbidity Survey (NHMS) 2019: NCDs-Non-Communicable Diseases: Risk Factors and Other Health Problems; National Institutes of Health: Shah Alam, Malaysia, 2019; Volume 1.
- Mahidin, M.U. Statistics on Causes of Death, Malaysia; Department of Statistics Malaysia: Putrajaya, Malaysia, 2020. [Google Scholar]
- Ministry of Health Malaysia. Prevention of Cardiovascular Disease in Women; Ministry of Health Malaysia: Putrajaya, Malaysia, 2016.
- Turkson-Ocran, R.A.N.; Nmezi, N.A.; Botchway, M.O.; Szanton, S.L.; Golden, S.H.; Cooper, L.A.; Commodore-Mensah, Y. Comparison of Cardiovascular Disease Risk Factors Among African Immigrants and African Americans: An Analysis of the 2010 to 2016 National Health Interview Surveys. J. Am. Heart Assoc. 2020, 9, e013220. [Google Scholar] [CrossRef] [PubMed]
- Aniza, I.; Nurmawati, A.; Hanizah, Y.; Ahmad Taufik, J. Modifiable Risk Factors of Cardiovascular Disease Among Adults In Rural Community of Malaysia: A Cross Sectional Study. Malays. J. Public Health Med. 2016, 16, 53–61. [Google Scholar]
- Kalra, S.; Chen, Z.; Deerochanawong, C.; Shyu, K.-G.; Tan, R.S.; Tomlinson, B.; Yeh, H.-I. Familial Hypercholesterolemia in Asia Pacific: A Review of Epidemiology, Diagnosis, and Management in the Region. J. Atheroscler. Thromb. 2021, 28, 417–434. [Google Scholar] [CrossRef]
- Vallejo-Vaz, A.J.; Stevens, C.A.T.; Lyons, A.R.M.; Dharmayat, K.I.; Freiberger, T.; Hovingh, G.K.; Mata, P.; Raal, F.J.; Santos, R.D.; Soran, H.; et al. Global Perspective of Familial Hypercholesterolaemia: A Cross-Sectional Study from the EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Lancet 2021, 398, 1713–1725. [Google Scholar] [CrossRef]
- Nawawi, H.M.; Chua, Y.A.; Watts, G.F. The Brave New World of Genetic Testing in the Management of the Dyslipidaemias. Curr. Opin. Cardiol. 2020, 35, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.C.; Charng, M.J. Genetic Diagnosis of Familial Hypercholesterolemia in Asia. Front. Genet. 2020, 11, 833. [Google Scholar] [CrossRef] [PubMed]
- Masana, L.; Zamora, A.; Plana, N.; Comas-Cufí, M.; Garcia-Gil, M.; Martí-Lluch, R.; Ponjoan, A.; Alves-Cabratosa, L.; Elosua, R.; Marrugat, J.; et al. Incidence of Cardiovascular Disease in Patients with Familial Hypercholesterolemia Phenotype: Analysis of 5 Years Follow-Up of Real-World Data from More than 1.5 Million Patients. J. Clin. Med. 2019, 8, 1080. [Google Scholar] [CrossRef] [PubMed]
- Tromp, T.R.; Hartgers, M.L.; Hovingh, G.K.; Vallejo-Vaz, A.J.; Ray, K.K.; Soran, H.; Freiberger, T.; Bertolini, S.; Harada-Shiba, M.; Blom, D.J.; et al. Worldwide Experience of Homozygous Familial Hypercholesterolaemia: Retrospective Cohort Study. Lancet 2022, 399, 719–728. [Google Scholar] [CrossRef]
- Chua, Y.-A.; Razman, A.Z.; Ramli, A.S.; Mohd Kasim, N.A.; Nawawi, H.M. Familial Hypercholesterolaemia in the Malaysian Community: Prevalence, Under-Detection and Under-Treatment. J. Atheroscler. Thromb. 2021, 28, 57026. [Google Scholar] [CrossRef] [PubMed]
- Vallejo-Vaz, A.J.; De Marco, M.; Stevens, C.A.T.; Akram, A.; Freiberger, T.; Hovingh, G.K.; Kastelein, J.J.P.; Mata, P.; Raal, F.J.; Santos, R.D.; et al. Overview of the Current Status of Familial Hypercholesterolaemia Care in over 60 Countries-The EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Atherosclerosis 2018, 277, 234–255. [Google Scholar] [CrossRef] [PubMed]
- Khera, A.V.; Won, H.-H.; Peloso, G.M.; Lawson, K.S.; Bartz, T.M.; Deng, X.; van Leeuwen, E.M.; Natarajan, P.; Emdin, C.A.; Bick, A.G.; et al. Diagnostic Yield and Clinical Utility of Sequencing Familial Hypercholesterolemia Genes in Patients With Severe Hypercholesterolemia. J. Am. Coll. Cardiol. 2016, 67, 2578–2589. [Google Scholar] [CrossRef]
- Wiegman, A.; Gidding, S.S.; Watts, G.F.; Chapman, M.J.; Ginsberg, H.N.; Cuchel, M.; Ose, L.; Averna, M.; Boileau, C.; Borén, J.; et al. Familial Hypercholesterolaemia in Children and Adolescents: Gaining Decades of Life by Optimizing Detection and Treatment. Eur. Heart J. 2015, 36, 2425–2437. [Google Scholar] [CrossRef]
- Nawawi, H.M.; Nor, I.M.; Noor, I.M.; Karim, N.A.; Arshad, F.; Khan, R.; Yusoff, K. Current Status of Coronary Risk Factors among Rural Malays in Malaysia; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2002; Volume 9. [Google Scholar]
- Feisul, I.M.; Tan, H.S.; Ahmad, A.A. Hypertension Prevention and Control in Malaysia: A Review. Int. J. Public Health Clin. Sci. 2020, 7, 19–31. [Google Scholar]
- Ahmad, W.; Sugathan, S.; Ismail, S.; Soe, M.M.; Ali, O. Cardiovascular Risk Factors in Rural Malays and Aborigines in Perak, Malaysia; an Alarming Situation. Med. Forum 2018, 29, 24–28. [Google Scholar]
- Amiri, M.; Majid, H.A.; Hairi, F.; Thangiah, N.; Bulgiba, A.; Su, T.T. Prevalence and Determinants of Cardiovascular Disease Risk Factors among the Residents of Urban Community Housing Projects in Malaysia. BMC Public Health 2014, 14, S3. [Google Scholar] [CrossRef] [PubMed]
- Su, T.T.; Amiri, M.; Mohd Hairi, F.; Thangiah, N.; Bulgiba, A.; Majid, H.A. Prediction of Cardiovascular Disease Risk among Low-Income Urban Dwellers in Metropolitan Kuala Lumpur, Malaysia. BioMed Res. Int. 2015. [Google Scholar] [CrossRef] [PubMed]
- Ghazali, S.M.; Seman, Z.; Cheong, K.C.; Hock, L.K.; Manickam, M.; Kuay, L.K.; Yusoff, A.F.; Mustafa, F.I.; Mustafa, A.N. Sociodemographic Factors Associated with Multiple Cardiovascular Risk Factors among Malaysian Adults. BMC Public Health 2015, 15, 68. [Google Scholar] [CrossRef]
- Ariaratnam, S.; Rodzlan Hasani, W.S.; Krishnapillai, A.D.; Abd Hamid, H.A.; Jane Ling, M.Y.; Ho, B.K.; Ghazali, S.S.; Tohit, N.M.; Mohd Yusoff, M.F. Prevalence of Obesity and Its Associated Risk Factors among the Elderly in Malaysia: Findings from the National Health and Morbidity Survey (NHMS) 2015. PLoS ONE 2020, 15, e238566. [Google Scholar] [CrossRef] [PubMed]
- Nordin, N.; Zahid, Z.; Ismail, Z.; Yassin, S.M.; Nawawi, H.M.; Hussin, S.A.S. Determination of the Obesity Prevalence and Its Associated Factors among Community in Selangor, Malaysia: An Ordinal Logistic Regression Approach. Indones. J. Electr. Eng. Comput. Sci. 2020, 19, 428–434. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. Primary & Secondary Prevention of Cardiovascular Disease 2017; Ministry of Health Malaysia: Putrajaya, Malaysia, 2017.
- Ministry of Health Malaysia. National Strategic Plan For Non-Communicable Disease (NSP-NCD) 2016–2025; Ministry of Health Malaysia: Putrajaya, Malaysia, 2016.
- Pang, J.; Chan, D.C.; Hu, M.; Muir, L.A.; Kwok, S.; Charng, M.J.; Florkowski, C.M.; George, P.M.; Lin, J.; Loi, D.D.; et al. Comparative Aspects of the Care of Familial Hypercholesterolemia in the “Ten Countries Study”. J. Clin. Lipidol. 2019, 13, 287–300. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. The Impact of Noncommunicable Diseases and Their Risk Factors on Malaysia’s Gross Domestic Product; Ministry of Health Malaysia: Putrajaya, Malaysia, 2020.
- Institute for Public Health; National Institutes of Health (NIH); Ministry of Health Malaysia. NHMS National Health and Morbidity Survey 2018 (NHMS 2018): Elderly Health; Institute for Public Health, National Institutes of Health (NIH), Ministry of Health Malaysia: Putrajaya, Malaysia, 2018; Volume 1, ISBN 9788578110796.
- Teh, X.R.; Lim, M.T.; Tong, S.F.; Husin, M.; Khamis, N.; Sivasampu, S. Quality of Hypertension Management in Public Primary Care Clinics in Malaysia: An Update. PLoS ONE 2020, 15, e237083. [Google Scholar] [CrossRef]
- D’Agostino, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General Cardiovascular Risk Profile for Use in Primary Care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- National Institute of Health USA. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) National Cholesterol Education Program; National Institute of Health USA: Gaithersburg, MD, USA, 2001.
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; de Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias: Lipid Modification to Reduce Cardiovascular Risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Catapano, A.L.; Graham, I.; de Backer, G.; Wiklund, O.; John Chapman, M.; Drexel, H.; Hoes, A.W.; Jennings, C.S.; Landmesser, U.; Pedersen, T.R.; et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur. Heart J. 2016, 37, 2999–3058. [Google Scholar] [CrossRef]
- Wong, B.; Kruse, G.; Kutikova, L.; Ray, K.K.; Mata, P.; Bruckert, E. Cardiovascular Disease Risk Associated With Familial Hypercholesterolemia: A Systematic Review of the Literature. Clin. Ther. 2016, 38, 1696–1709. [Google Scholar] [CrossRef] [PubMed]
- Versmissen, J.; Oosterveer, D.M.; Yazdanpanah, M.; Defesche, J.C.; Basart, D.C.G.; Liem, A.H.; Heeringa, J.; Witteman, J.C.; Lansberg, P.J.; Kastelein, J.J.P.; et al. Efficacy of Statins in Familial Hypercholesterolaemia: A Long Term Cohort Study. BMJ 2009, 337, a2423. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Razak, S.; Rahmat, R.; Mohd Kasim, A.; Rahman, T.A.; Muid, S.; Nasir, N.M.; Ibrahim, Z.; Kasim, S.; Ismail, Z.; Abdul Ghani, R.; et al. Diagnostic Performance of Various Familial Hypercholesterolaemia Diagnostic Criteria Compared to Dutch Lipid Clinic Criteria in an Asian Population. BMC Cardiovasc. Disord. 2017, 17, 264. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia. Clinical Practice Guideline Management of Hypertension, 5th ed.; Ministry of Health Malaysia: Putrajaya, Malaysia, 2018.
- Ministry of Health Malaysia. Clinical Practice Guidelines Management of Type 2 Diabetes Mellitus, 5th Edition, Guideline; Ministry of Health Malaysia: Putrajaya, Malaysia, 2015.
- Ministry of Health Malaysia. Clinical Practice Guidelines on Management of Obesity 2004; Ministry of Health Malaysia: Putrajaya, Malaysia, 2004.
- Ministry of Health Malaysia. 5th Edition of Clinical Practice Guidelines on Management of Dyslipidaemia 2017; Ministry of Health Malaysia: Putrajaya, Malaysia, 2017.
- Nordestgaard, B.G.; Chapman, M.J.; Humphries, S.E.; Ginsberg, H.N.; Masana, L.; Descamps, O.S.; Wiklund, O.; Hegele, R.A.; Raal, F.J.; Defesche, J.C.; et al. Familial Hypercholesterolaemia Is Underdiagnosed and Undertreated in the General Population: Guidance for Clinicians to Prevent Coronary Heart Disease. Eur. Heart J. 2013, 34, 3478–3490. [Google Scholar] [CrossRef] [Green Version]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimationof the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- De Backer, G.; Besseling, J.; Chapman, J.; Hovingh, G.K.; Kastelein, J.P.; Kotseva, K.; Ray, K.; Reiner, Z.; Wood, D.; De Bacquer, D. Prevalence and Management of Familial Hypercholesterolaemia Incoronary Patients: An Analysis of EUROASPIRE IV, a Study of TheEuropean Society of Cardiology. Atherosclerosis 2015, 241, 169–175. [Google Scholar] [CrossRef]
- Scientific Steering Committee on behalf of the Simon Broome Register Group. Risk of Fatal Coronary Heart Disease in Familial Hypercholesterolaemia. BMJ 1991, 303, 893–896. [Google Scholar] [CrossRef]
- Varghese, M.J. Familial Hypercholesterolemia: A Review. Ann. Pediatric Cardiol. 2014, 7, 107–117. [Google Scholar] [CrossRef]
- Williams, R.R.; Hunt, S.C.; Schumacher, M.C.; Hegele, R.A.; Leppert, M.F.; Ludwig, E.H.; Hopkins, P.N. Diagnosing Heterozygous Familial Hypercholesterolemia Using New Practical Criteria Validated by Molecular Genetics. Am. J. Cardiol. 1993, 72, 171–176. [Google Scholar] [CrossRef]
- Harada-Shiba, M.; Arai, H.; Oikawa, S.; Ohta, T.; Okada, T.; Okamura, T.; Nohara, A.; Bujo, H.; Yokote, K.; Wakatsuki, A.; et al. Special Report Guidelines for the Management of Familial Hypercholesterolemia. J. Atheroscler. Thromb. 2012, 19, 1043–1060. [Google Scholar] [CrossRef]
- Mohd Nor, N.S.; Chua, Y.-A.; Abdul Razak, S.; Ismail, Z.; Nawawi, H. Identification of Cardiovascular Risk Factors among Urban and Rural Malaysian Youths. BMC Cardiovasc. Disord. 2022, 22, 70. [Google Scholar] [CrossRef]
- van Ginkel, J.R.; Linting, M.; Rippe, R.C.A.; van der Voort, A. Rebutting Existing Misconceptions About Multiple Imputation as a Method for Handling Missing Data. J. Personal. Assess. 2020, 102, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, B. “P < 0.05” Might Not Mean What You Think: American Statistical Association Clarifies P Values. J. Natl. Cancer Inst. 2016, 108, 4–9. [Google Scholar] [CrossRef]
- Schütz, F.; Heidingsfelder, M.L.; Schraudner, M. Co-Shaping the Future in Quadruple Helix Innovation Systems: Uncovering Public Preferences toward Participatory Research and Innovation. She Ji J. Des. Econ. Innov. 2019, 5, 128–146. [Google Scholar] [CrossRef]
- Chan, Y.Y.; Sahril, N.; Rezali, M.S.; Kuay, L.K.; Baharudin, A.; Razak, M.A.A.; Kassim, M.S.A.; Yusoff, M.F.M.; Omar, M.A.; Ahmad, N.A. Self-Reported Modifiable Risk Factors of Cardiovascular Disease among Older Adults in Malaysia: A Cross-Sectional Study of Prevalence and Clustering. Int. J. Environ. Res. Public Health 2021, 18, 7941. [Google Scholar] [CrossRef]
- Tomaselli, G.; Roach, W.H.; Piña, I.L.; Oster, M.E.; Dietz, W.H.; Horton, K.; Borden, W.B.; Brownell, K.; Gibbons, R.J.; Otten, J.J.; et al. Government Continues to Have an Important Role in Promoting Cardiovascular Health. Am. Heart J. 2018, 198, 160–165. [Google Scholar] [CrossRef]
- Ab Majid, N.L.; Omar, M.A.; Khoo, Y.Y.; Mahadir Naidu, B.; Ling Miaw Yn, J.; Rodzlan Hasani, W.S.; Mat Rifin, H.; Abd Hamid, H.A.; Robert Lourdes, T.G.; Mohd Yusoff, M.F. Prevalence, Awareness, Treatment and Control of Hypertension in the Malaysian Population: Findings from the National Health and Morbidity Survey 2006–2015. J. Hum. Hypertens. 2018, 32, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Mat Rifin, H.; Robert Lourdes, T.G.; Abdul Majid, N.L.; Abd Hamid, H.A.; Rodzlan Hasani, W.S.; Ling, M.Y.; Saminathan, T.A.; Ismail, H.; Mohd Yusoff, M.F.; Omar, M.A. Hypercholesterolemia Prevalence, Awareness, Treatment and Control among Adults in Malaysia: The 2015 National Health and Morbidity Survey, Malaysia. Glob. J. Health Sci. 2018, 10, 11. [Google Scholar] [CrossRef]
- Chiu Lim, B.I.; Cheng Kueh, Y.I.; Nor Arifin, W.; Huan Ng, K.; Kerian, K.; Pahang Specialist Hospital, K. Modelling Knowledge, Health Beliefs, and Health-Promoting Behaviours Related to Cardiovascular Disease Prevention among Malaysian University Students. PLoS ONE 2021, 16, e250627. [Google Scholar] [CrossRef]
- Sariff, A.; Amin, A.M.; Mostafa, H. Public Knowledge and Awareness of Cardiovascular Diseases and the Expected Role of Community Pharmacists in the Prevention and Management of Cardiovascular Diseases in Penang, Malaysia. Chiang Mai Univ. J. Nat. Sci. 2014, 13, 355–369. [Google Scholar] [CrossRef]
- Fun, W.H.; Sararaks, S.; Tan, E.H.; Tang, K.F.; Chong, D.W.Q.; Low, L.L.; Sapian, R.A.; Ismail, S.A.; Govind, S.K.; Mahmud, S.H.; et al. Research Funding Impact and Priority Setting-Advancing Universal Access and Quality Healthcare Research in Malaysia. BMC Health Serv. Res. 2019, 19, 248. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.; Moy, F.M.; Awalludin, I.A.N.; Ali, Z.M.; Ismail, I.S. Effects of a Community-Based Healthy Lifestyle Intervention Program (Co-HELP) among Adults with Prediabetes in a Developing Country: A Quasi-Experimental Study. PLoS ONE 2016, 11, e0167123. [Google Scholar] [CrossRef] [PubMed]
- Mansor, M.; Harun, N.Z. Health Issues and Green Space as Reinforcement for a Healthy Lifestyle in Malaysia. J. ASIAN Behav. Stud. 2018, 3, 69–77. [Google Scholar] [CrossRef]
- Alissa, E.M.; Ferns, G.A. Functional Foods and Nutraceuticals in the Primary Prevention of Cardiovascular Diseases. J. Nutr. Metab. 2012, 2012, 569486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghaffari, S.; Roshanravan, N. The Role of Nutraceuticals in Prevention and Treatment of Hypertension: An Updated Review of the Literature. Food Res. Int. 2020, 128, 108749. [Google Scholar] [CrossRef] [PubMed]
- Wahid, A.; Manek, N.; Nichols, M.; Kelly, P.; Foster, C.; Webster, P.; Kaur, A.; Friedemann Smith, C.; Wilkins, E.; Rayner, M.; et al. Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2016, 5, e002495. [Google Scholar] [CrossRef] [PubMed]
- Lanier, J.B.; Richardson, S.W. Diet and Physical Activity for Cardiovascular Disease Prevention. Am. Fam. Physician 2016, 93, 1–6. [Google Scholar]
- Kraus, W.E.; Powell, K.E.; Haskell, W.L.; Janz, K.F.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. Physical Activity, All-Cause and Cardiovascular Mortality, and Cardiovascular Disease. Med. Sci. Sports Exerc. 2019, 51, 1270–1281. [Google Scholar] [CrossRef]
- Nouri, A.I.; Hassali, M.A.; Hashmi, F.K. Contribution of Pharmacy Education to Pharmaceutical Research and Development: Critical Insights from Educators. Perspect. Public Health 2020, 140, 62–66. [Google Scholar] [CrossRef]
- Sultana, N.; Khatib, A.J.; Alsarhan, A.; Al-Khatib, A.; Rafiq, M.; Kadir, A. Review on Some Malaysian Traditional Medicinal Plants with Therapeutic Properties. J. Basic Appl. Sci. 2014, 10, 149–159. [Google Scholar]
- Than, M.C.; Anam, A.; Nurfarahi, K.; Asma’, A.; Hayati, M.Y. Knowledge, Use of Complementary Alternative Medicine and Health-Related Quality of Life among Cardiovascular Disease Patients. Food Res. 2019, 3, 604–616. [Google Scholar] [CrossRef]
- Moss, J.W.E.; Williams, J.O.; Ramji, D.P. Nutraceuticals as Therapeutic Agents for Atherosclerosis. Biochim. Biophys. Acta-Mol. Basis Dis. 2018, 1864, 1562–1572. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.J.A.; Spence, J.D.; Giovannucci, E.L.; Kim, Y.I.; Josse, R.; Vieth, R.; Blanco Mejia, S.; Viguiliouk, E.; Nishi, S.; Sahye-Pudaruth, S.; et al. Supplemental Vitamins and Minerals for CVD Prevention and Treatment. J. Am. Coll. Cardiol. 2018, 71, 2570–2584. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Zhang, J.W.; Zang, G.Y.; Pu, J. The Primary Use of Artificial Intelligence in Cardiovascular Diseases: What Kind of Potential Role Does Artificial Intelligence Play in Future Medicine? J. Geriatr. Cardiol. 2019, 16, 585–591. [Google Scholar] [PubMed]
- Burke, L.E.; Ma, J.; Azar, K.M.J.; Bennett, G.G.; Peterson, E.D.; Zheng, Y.; Riley, W.; Stephens, J.; Shah, S.H.; Suffoletto, B.; et al. Current Science on Consumer Use of Mobile Health for Cardiovascular Disease Prevention: A Scientific Statement from the American Heart Association. Circulation 2015, 132, 1157–1213. [Google Scholar] [CrossRef]
- Buang, N.F.B.; Rahman, N.A.A.; Haque, M. Knowledge, Attitude and Practice Regarding Hypertension among Residents in a Housing Area in Selangor, Malaysia. Med. Pharm. Rep. 2019, 92, 145–152. [Google Scholar] [CrossRef]
- Baharudin, N.; Mohamed-Yassin, M.-S.; Daher, A.M.; Ramli, A.S.; Mohamed, N.-A.; Khan, N.; Abdul-Razak, S. Prevalence and Factors Associated with Lipid-Lowering Medications Use for Primary and Secondary Prevention of Cardiovascular Diseases among Malaysians: The REDISCOVER Study. BMC Public Health 2021, 22, 228. [Google Scholar] [CrossRef]
- Jackson, C.L.; Zordok, M.; Kullo, I.J. Familial Hypercholesterolemia in Southeast and East Asia. Am. J. Prev. Cardiol. 2021, 6, 100157. [Google Scholar] [CrossRef]
- Watts, G.F.; Shaw, J.E.; Pang, J.; Magliano, D.J.; Jennings, G.L.R.; Carrington, M.J. Prevalence and Treatment of Familial Hypercholesterolaemia in Australian Communities. Int. J. Cardiol. 2015, 185, 69–71. [Google Scholar] [CrossRef]

| No. | Abbreviation | Variables | Description | Type of Data | Reference |
|---|---|---|---|---|---|
| 1 | HPT | Hypertension | SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg or self-reported of having HPT with/without taking anti HPT medication | Nominal | [43] |
| 2 | DM | Diabetes mellitus type 2 | FPG ≥ 7.0 mmol/L or RPG ≥ 11.1 mmol/L or self-reported of having DM with/without anti DM medication. | Nominal | [44] |
| 3 | BMI | Body Mass Index | 1. Underweight (BMI < 18.5 kg/m2) 2. Normal (18.5 ≤ BMI ≥ 22.9) 3. Overweight (23 ≤ BMI ≥ 27.4 kg/m2) 4. Obese (BMI of ≥27.5) | Ordinal | [45] |
| 4 | CO | Central Obesity | Waist circumference ≥ 90 cm for males and ≥80 cm for females. | Nominal | [45] |
| 5 | Smoking | Smoking | 1. Smoker 2. Non-smoker 3. Ex-smoker | Nominal | [46] |
| 6 | Low HDL-C | Low high-density lipoprotein cholesterol | Male < 1.0 mmol/L, female < 1.2 mmol/L | Nominal | [46] |
| 7 | High LDL-C | High low-density lipoprotein cholesterol | Low-risk group > 3.4 mmol/L Moderate-risk group > 2.6 mmol/L High-risk group > 2.6 mmol/L Very high-risk group > 1.8 mmol/L | Nominal | [46] |
| 8 | HTG | Hypertriglyceridaemia | TG > 1.7 mmol/L | Nominal | [46] |
| HC | Hypercholesterolaemia | TC ≥ 5.2 mmol/L and/or taking lipid-lowering drug and/or self-reported of having HC | Nominal | [46] |
| FRS-CVD 2008 | ESC/EAS 2016 | ESC/EAS 2019 | |
|---|---|---|---|
| Low |
|
|
|
| Moderate |
|
|
|
| High |
|
|
|
| Very High |
|
|
|
| DLCN | SB | JFHMC | USMEDPED | |
|---|---|---|---|---|
| Diagnostic outcome categories | Definite Probable Possible Unlikely | Definite Possible Unlikely | Yes No | Yes No |
| Lipid data used | LDL-C | TC or LDL-C | TC or LDL-C | TC or LDL-C |
| Genetics evaluation | Yes | Yes | No | No |
| Personal history of PCAD | Yes | No | No | No |
| Family history PCAD | Yes | Yes | Yes | No |
| Family history of hypercholesterolaemia | Yes | Yes | No | No |
| Family History of FH | No | No | Yes | Yes |
| Physical examination of corneal arcus | Yes | No | No | No |
| Physical examination of tendon xanthomata | Yes | Yes | Yes | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Firus Khan, A.Y.; Ramli, A.S.; Abdul Razak, S.; Mohd Kasim, N.A.; Chua, Y.-A.; Ul-Saufie, A.Z.; Jalaludin, M.A.; Nawawi, H., on behalf of the MyHEBAT Study Investigators. The Malaysian HEalth and WellBeing AssessmenT (MyHEBAT) Study Protocol: An Initiation of a National Registry for Extended Cardiovascular Risk Evaluation in the Community. Int. J. Environ. Res. Public Health 2022, 19, 11789. https://doi.org/10.3390/ijerph191811789
Firus Khan AY, Ramli AS, Abdul Razak S, Mohd Kasim NA, Chua Y-A, Ul-Saufie AZ, Jalaludin MA, Nawawi H on behalf of the MyHEBAT Study Investigators. The Malaysian HEalth and WellBeing AssessmenT (MyHEBAT) Study Protocol: An Initiation of a National Registry for Extended Cardiovascular Risk Evaluation in the Community. International Journal of Environmental Research and Public Health. 2022; 19(18):11789. https://doi.org/10.3390/ijerph191811789
Chicago/Turabian StyleFirus Khan, Al’aina Yuhainis, Anis Safura Ramli, Suraya Abdul Razak, Noor Alicezah Mohd Kasim, Yung-An Chua, Ahmad Zia Ul-Saufie, Mohd Amin Jalaludin, and Hapizah Nawawi on behalf of the MyHEBAT Study Investigators. 2022. "The Malaysian HEalth and WellBeing AssessmenT (MyHEBAT) Study Protocol: An Initiation of a National Registry for Extended Cardiovascular Risk Evaluation in the Community" International Journal of Environmental Research and Public Health 19, no. 18: 11789. https://doi.org/10.3390/ijerph191811789





