Long Working Hours and the Risk of Glucose Intolerance: A Cohort Study
Abstract
1. Introduction
2. Materials and Methods
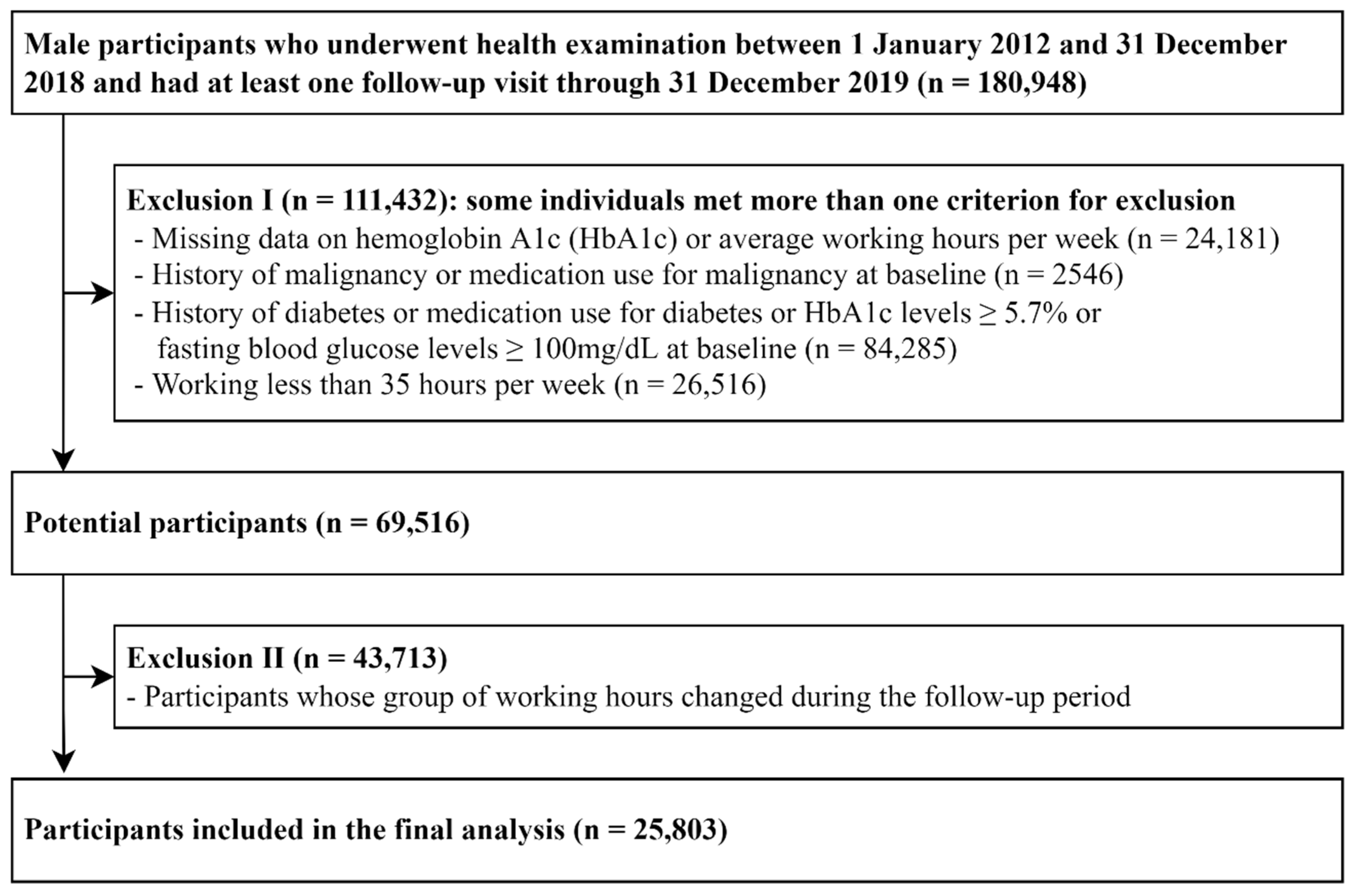
2.1. Study Population
2.2. Measurements
2.3. Statistical Analysis
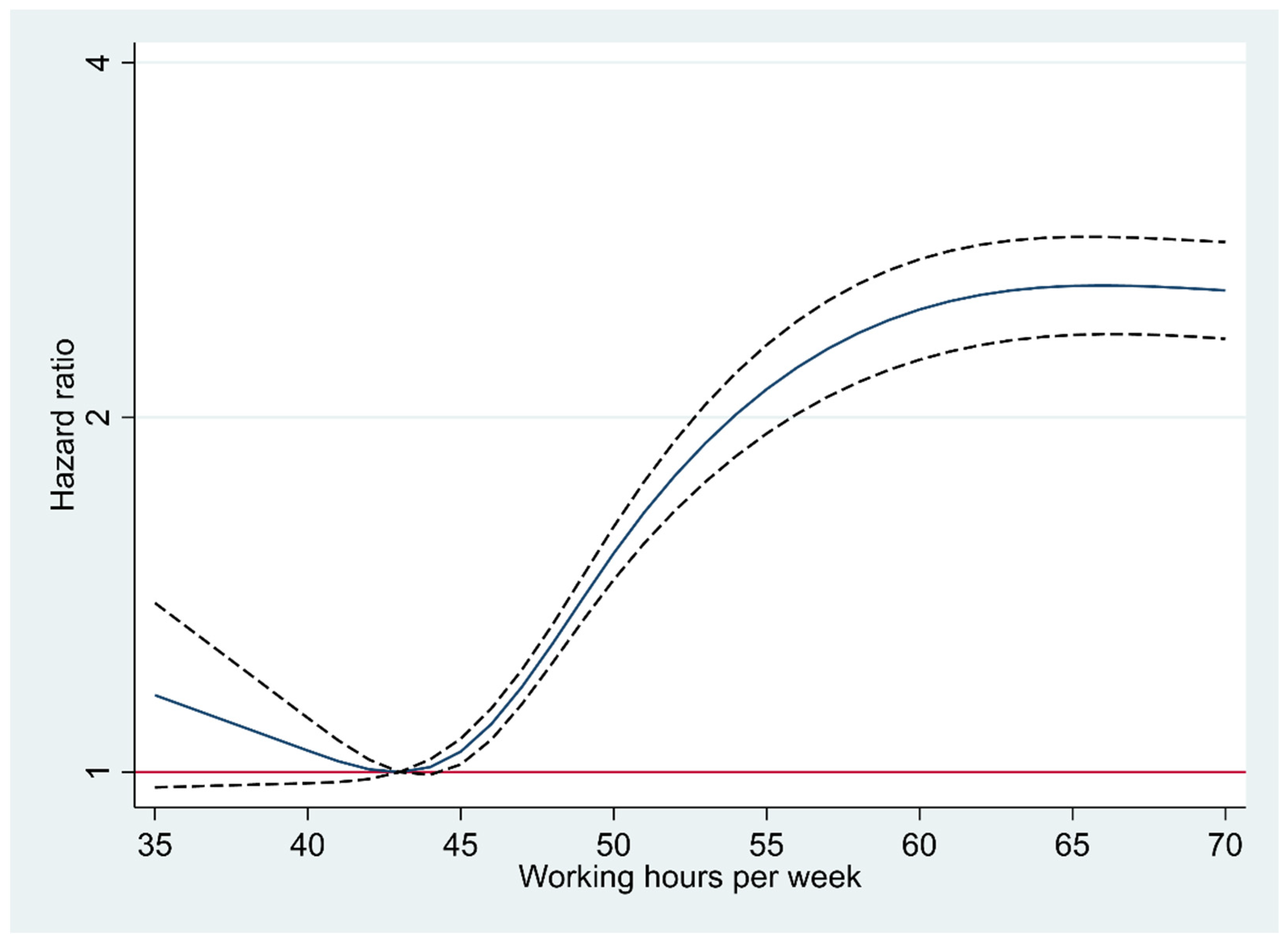
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, S.H.; McCann, D.M.; Messenger, J.C. Working Time Around the World: Trends in Working Hours, Laws and Policies in a Global Comparative Perspective; Routledge: London, UK, 2007; Volume 1, pp. 1–220. [Google Scholar]
- Pega, F.; Náfrádi, B.; Momen, N.C.; Ujita, Y.; Streicher, K.N.; Prüss-Üstün, A.M.; Descatha, A.; Driscoll, T.; Fischer, F.M.; Godderis, L.; et al. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000–2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 154, 106595. [Google Scholar] [CrossRef] [PubMed]
- Pega, F.; Hamzaoui, H.; Náfrádi, B.; Momen, N.C. Global, regional and national burden of disease attributable to 19 selected occupational risk factors for 183 countries, 2000–2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Scand. J. Work Environ. Health 2022, 48, 158–168. [Google Scholar] [CrossRef] [PubMed]
- OECD. Hours Worked (Indicator). Available online: https://data.oecd.org/emp/hours-worked.htm (accessed on 2 August 2022).
- ILO. How Did COVID-19 Impact Working Hours in Asia-Pacific Economies in 2020? Available online: https://www.ilo.org/asia/publications/WCMS_779273/lang--en/index.htm (accessed on 16 September 2022).
- Lee, D.W.; Lee, J.; Kim, H.R.; Kang, M.Y. Association of long working hours and health-related productivity loss, and its differential impact by income level: A cross-sectional study of the Korean workers. J. Occup. Health 2020, 62, e12190. [Google Scholar] [CrossRef]
- Kivimäki, M.; Jokela, M.; Nyberg, S.T.; Singh-Manoux, A.; Fransson, E.I.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A.; et al. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015, 386, 1739–1746. [Google Scholar] [CrossRef]
- Trudel, X.; Brisson, C.; Gilbert-Ouimet, M.; Vézina, M.; Talbot, D.; Milot, A. Long Working Hours and the Prevalence of Masked and Sustained Hypertension. Hypertension 2020, 75, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Ruan, W.; Chen, Z.; Yi, G.; Lu, Z.; Wang, D. A meta-analysis of observational studies including dose-response relationship between long working hours and risk of obesity. Rev. Endocr. Metab. Disord. 2021, 22, 837–845. [Google Scholar] [CrossRef]
- Virtanen, M.; Jokela, M.; Madsen, I.E.; Magnusson Hanson, L.L.; Lallukka, T.; Nyberg, S.T.; Alfredsson, L.; Batty, G.D.; Bjorner, J.B.; Borritz, M.; et al. Long working hours and depressive symptoms: Systematic review and meta-analysis of published studies and unpublished individual participant data. Scand. J. Work Environ. Health 2018, 44, 239–250. [Google Scholar] [CrossRef]
- Lin, X.; Xu, Y.; Pan, X.; Xu, J.; Ding, Y.; Sun, X.; Song, X.; Ren, Y.; Shan, P.F. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 2020, 10, 14790. [Google Scholar] [CrossRef]
- Kivimäki, M.; Virtanen, M.; Kawachi, I.; Nyberg, S.T.; Alfredsson, L.; Batty, G.D.; Bjorner, J.B.; Borritz, M.; Brunner, E.J.; Burr, H.; et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: A meta-analysis of published and unpublished data from 222,120 individuals. Lancet Diabetes Endocrinol. 2015, 3, 27–34. [Google Scholar] [CrossRef]
- Kuwahara, K.; Miyamoto, T.; Yamamoto, S.; Honda, T.; Nakagawa, T.; Mizoue, T. Japan Epidemiology Collaboration on Occupational Health Study, G. Patterns of changes in overtime working hours over 3years and the risk for progression to type 2 diabetes in adults with pre-diabetes. Prev. Med. 2019, 121, 18–23. [Google Scholar] [CrossRef]
- Rossnagel, K.; Jankowiak, S.; Liebers, F.; Schulz, A.; Wild, P.; Arnold, N.; Seidler, A.; Hegewald, J.; Romero Starke, K.; Letzel, S.; et al. Long working hours and risk of cardiovascular outcomes and diabetes type II: Five-year follow-up of the Gutenberg Health Study (GHS). Int. Arch. Occup. Environ. Health 2022, 95, 303–312. [Google Scholar] [CrossRef]
- Tayama, J.; Li, J.; Munakata, M. Working Long Hours is Associated with Higher Prevalence of Diabetes in Urban Male Chinese Workers: The Rosai Karoshi Study. Stress Health 2016, 32, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Gilbert-Ouimet, M.; Ma, H.; Glazier, R.; Brisson, C.; Mustard, C.; Smith, P.M. Adverse effect of long work hours on incident diabetes in 7065 Ontario workers followed for 12 years. BMJ Open Diabetes Res. Care 2018, 6, e000496. [Google Scholar] [CrossRef] [PubMed]
- Bannai, A.; Yoshioka, E.; Saijo, Y.; Sasaki, S.; Kishi, R.; Tamakoshi, A. The Risk of Developing Diabetes in Association with Long Working Hours Differs by Shift Work Schedules. J. Epidemiol. 2016, 26, 481–487. [Google Scholar] [CrossRef]
- Baek, Y.; Kim, M.; Kim, G.R.; Park, E.C. Cross-sectional study of the association between long working hours and pre-diabetes: 2010–2017 Korea national health and nutrition examination survey. BMJ Open 2019, 9, e033579. [Google Scholar] [CrossRef]
- Kim, D.J. The epidemiology of diabetes in Korea. Diabetes Metab. J. 2011, 35, 303–308. [Google Scholar] [CrossRef]
- Kim, J.H.; Lim, J.S. Trends of Diabetes and Prediabetes Prevalence among Korean Adolescents From 2007 to 2018. J. Korean Med. Sci. 2021, 36, e112. [Google Scholar] [CrossRef]
- Chang, Y.; Jung, H.S.; Cho, J.; Zhang, Y.; Yun, K.E.; Lazo, M.; Pastor-Barriuso, R.; Ahn, J.; Kim, C.W.; Rampal, S.; et al. Metabolically Healthy Obesity and the Development of Nonalcoholic Fatty Liver Disease. Am. J. Gastroenterol. 2016, 111, 1133–1140. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Association, A.D. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care 2021, 44, S15–S33. [Google Scholar] [CrossRef]
- Artazcoz, L.; Cortès, I.; Escribà-Agüir, V.; Cascant, L.; Villegas, R. Understanding the relationship of long working hours with health status and health-related behaviours. J. Epidemiol. Community Health 2009, 63, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Jang, T.W.; Kim, H.R.; Kang, M.Y. The relationship between working hours and lifestyle behaviors: Evidence from a population-based panel study in Korea. J. Occup. Health 2021, 63, e12280. [Google Scholar] [CrossRef] [PubMed]
- Akter, S.; Goto, A.; Mizoue, T. Smoking and the risk of type 2 diabetes in Japan: A systematic review and meta-analysis. J. Epidemiol. 2017, 27, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Śliwińska-Mossoń, M.; Milnerowicz, H. The impact of smoking on the development of diabetes and its complications. Diab. Vasc. Dis. Res. 2017, 14, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Polsky, S.; Akturk, H.K. Alcohol Consumption, Diabetes Risk, and Cardiovascular Disease within Diabetes. Curr. Diab. Rep. 2017, 17, 136. [Google Scholar] [CrossRef]
- Thorp, A.A.; Healy, G.N.; Winkler, E.; Clark, B.K.; Gardiner, P.A.; Owen, N.; Dunstan, D.W. Prolonged sedentary time and physical activity in workplace and non-work contexts: A cross-sectional study of office, customer service and call centre employees. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 128. [Google Scholar] [CrossRef]
- Qin, L.; Knol, M.J.; Corpeleijn, E.; Stolk, R.P. Does physical activity modify the risk of obesity for type 2 diabetes: A review of epidemiological data. Eur. J. Epidemiol. 2010, 25, 5–12. [Google Scholar] [CrossRef]
- Antza, C.; Kostopoulos, G.; Mostafa, S.; Nirantharakumar, K.; Tahrani, A. The links between sleep duration, obesity and type 2 diabetes mellitus. J. Endocrinol. 2021, 252, 125–141. [Google Scholar] [CrossRef]
- Min, J.; Lee, D.W.; Kang, M.Y.; Myong, J.P.; Kim, H.R.; Lee, J. Working for Long Hours Is Associated with Dietary Fiber Insufficiency. Front. Nutr. 2022, 9, 786569. [Google Scholar] [CrossRef]
- Weickert, M.O.; Pfeiffer, A.F.H. Impact of Dietary Fiber Consumption on Insulin Resistance and the Prevention of Type 2 Diabetes. J. Nutr. 2018, 148, 7–12. [Google Scholar] [CrossRef]
- Lee, K.; Suh, C.; Kim, J.E.; Park, J.O. The impact of long working hours on psychosocial stress response among white-collar workers. Ind. Health 2017, 55, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Hackett, R.A.; Steptoe, A. Type 2 diabetes mellitus and psychological stress—A modifiable risk factor. Nat. Rev. Endocrinol. 2017, 13, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Di Dalmazi, G.; Pagotto, U.; Pasquali, R.; Vicennati, V. Glucocorticoids and type 2 diabetes: From physiology to pathology. J. Nutr. Metab. 2012, 2012, 525093. [Google Scholar] [CrossRef] [PubMed]
- Clore, J.N.; Thurby-Hay, L. Glucocorticoid-induced hyperglycemia. Endocr. Pract. 2009, 15, 469–474. [Google Scholar] [CrossRef]
- Hackett, R.A.; Kivimäki, M.; Kumari, M.; Steptoe, A. Diurnal Cortisol Patterns, Future Diabetes, and Impaired Glucose Metabolism in the Whitehall II Cohort Study. J. Clin. Endocrinol. Metab. 2016, 101, 619–625. [Google Scholar] [CrossRef]
- Tsigos, C.; Chrousos, G.P. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J. Psychosom. Res. 2002, 53, 865–871. [Google Scholar] [CrossRef]
- Almadi, T.; Cathers, I.; Chow, C.M. Associations among work-related stress, cortisol, inflammation, and metabolic syndrome. Psychophysiology 2013, 50, 821–830. [Google Scholar] [CrossRef]
- Chia, C.W.; Egan, J.M.; Ferrucci, L. Age-Related Changes in Glucose Metabolism, Hyperglycemia, and Cardiovascular Risk. Circ. Res. 2018, 123, 886–904. [Google Scholar] [CrossRef]
- Lee, M.K.; Han, K.; Kwon, H.S. Age-specific diabetes risk by the number of metabolic syndrome components: A Korean nationwide cohort study. Diabetol. Metab. Syndr. 2019, 11, 112. [Google Scholar] [CrossRef]
- Wang, Y.; Yu, L.; Gao, Y.; Jiang, L.; Yuan, L.; Wang, P.; Cao, Y.; Song, X.; Ge, L.; Ding, G. Association between shift work or long working hours with metabolic syndrome: A systematic review and dose-response meta-analysis of observational studies. Chronobiol. Int. 2021, 38, 318–333. [Google Scholar] [CrossRef]
- Sawang, S.; Newton, C.J. Defining Work Stress in Young People. J. Employ. Couns. 2018, 55, 72–83. [Google Scholar] [CrossRef]
- Reviriego, J.; Vázquez, L.A.; Goday, A.; Cabrera, M.; García-Margallo, M.T.; Calvo, E. Prevalence of impaired fasting glucose and type 1 and 2 diabetes mellitus in a large nationwide working population in Spain. Endocrinol. Nutr. 2016, 63, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Hedén Stahl, C.; Novak, M.; Hansson, P.O.; Lappas, G.; Wilhelmsen, L.; Rosengren, A. Incidence of Type 2 diabetes among occupational classes in Sweden: A 35-year follow-up cohort study in middle-aged men. Diabet. Med. 2014, 31, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, S.; Andersson, T.; Talbäck, M.; Feychting, M. Incidence and prevalence of type 2 diabetes by occupation: Results from all Swedish employees. Diabetologia 2020, 63, 95–103. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef]
- Mathur, M.B.; Ding, P.; Riddell, C.A.; VanderWeele, T.J. Web Site and R Package for Computing E-values. Epidemiology 2018, 29, e45–e47. [Google Scholar] [CrossRef]
| Weekly Working Hours | p for Trend | ||||
|---|---|---|---|---|---|
| Characteristics | Overall | 35–40 | 41–52 | >52 | |
| Number | 25,803 | 5171 | 16,316 | 4316 | |
| Age (years) * | 36.6 (7.6) | 40.4 (9.3) | 35.3 (6.6) | 36.7 (7.1) | <0.001 |
| Current smoker (%) | 30.0 | 33.0 | 26.8 | 38.2 | 0.002 |
| Heavy Alcohol intake (%) a | 18.8 | 23.8 | 16.5 | 21.3 | <0.001 |
| Regular exercise (%) b | 14.8 | 18.0 | 14.6 | 11.5 | <0.001 |
| High education level (%) c | 89.9 | 83.2 | 92.5 | 88.0 | <0.001 |
| Marital status—married (%) | 69.6 | 78.7 | 66.0 | 72.0 | <0.001 |
| High household income (%) d | 30.4 | 32.6 | 28.2 | 35.8 | 0.223 |
| Medication for hypertension (%) | 3.27 | 5.67 | 2.45 | 3.54 | <0.001 |
| Medication for dyslipidemia (%) | 1.76 | 2.61 | 1.40 | 2.13 | 0.029 |
| Obesity (%) e | 34.1 | 34.2 | 33.3 | 36.9 | 0.011 |
| BMI (kg/m2) * | 24.1 (2.8) | 24.1 (2.7) | 24.1 (2.8) | 24.4 (2.9) | <0.001 |
| Systolic BP (mmHg) * | 112.5 (10.7) | 113.0 (11.1) | 112.4 (10.6) | 112.0 (10.6) | <0.001 |
| Diastolic BP (mmHg) * | 72.2 (8.8) | 73.3 (9.1) | 71.8 (8.7) | 72.2 (8.9) | <0.001 |
| Glucose (mg/dL) * | 91.1 (5.5) | 91.5 (5.4) | 90.9 (5.5) | 91.1 (5.6) | <0.001 |
| Hemoglobin A1c (%) * | 5.39 (0.19) | 5.39 (0.19) | 5.38 (0.19) | 5.41 (0.18) | <0.001 |
| HOMA-IR # | 1.22 (0.82–1.76) | 1.19 (0.80–1.72) | 1.22 (0.83–1.77) | 1.23 (0.83–1.78) | 0.021 |
| Total cholesterol (mg/dL) * | 194.5 (32.8) | 196.0 (33.7) | 193.6 (32.5) | 195.8 (32.8) | 0.498 |
| LDL-C (mg/dL) * | 126.2 (30.6) | 127.7 (30.9) | 125.6 (30.5) | 126.6 (30.5) | 0.032 |
| HDL-C (mg/dL) * | 54.6 (13.3) | 54.5 (13.4) | 54.9 (13.3) | 54.0 (13.2) | 0.161 |
| Triglycerides (mg/dL) # | 100 (72–144) | 103 (74–149) | 99 (71–142) | 101 (74–145) | 0.102 |
| hsCRP (mg/L) # | 0.05 (0.03–0.09) | 0.05 (0.03–0.09) | 0.05 (0.03–0.09) | 0.05 (0.03–0.09) | 0.06 |
| Daytime work (%) f | 89.8 | 90.8 | 90.6 | 85.5 | <0.001 |
| Weekly Working Hours | Person-Years (PY) | Incident Cases | Incidence Density (per 100 PY) (95% CI) | Age-Adjusted HR (95% CI) | Multivariable-Adjusted HR (95% CI) a | ||
|---|---|---|---|---|---|---|---|
| Model 1 * | Model 2 ** | Model 3 *** | |||||
| 35–40 | 15,646.9 | 1194 | 7.63 (7.21–8.08) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 41–52 | 51,421.0 | 3858 | 7.50 (7.27–7.74) | 1.32 (1.23–1.41) | 1.33 (1.23–1.44) | 1.29 (1.18–1.41) | 1.28 (1.17–1.40) |
| >52 | 10,537.1 | 1689 | 16.03 (15.28–16.81) | 2.65 (2.46–2.86) | 2.72 (2.50–2.97) | 2.79 (2.53–3.08) | 2.80 (2.54–3.09) |
| per 1 h | 1.02 (1.02–1.03) | 1.02 (1.02–1.03) | 1.03 (1.02–1.03) | 1.03 (1.02–1.03) | |||
| p for trend | <0.001 | <0.001 | <0.001 | <0.001 | |||
| Subgroup | Weekly Working Hours | p for Trend | p for Interaction | ||
|---|---|---|---|---|---|
| 35–40 | 41–52 | >52 | |||
| Age | <0.001 | ||||
| <40 years (n = 18,041) | 1.00 (reference) | 1.10 (0.97–1.24) | 2.72 (2.38–3.10) | <0.001 | |
| ≥40 years (n = 7762) | 1.00 (reference) | 1.32 (1.16–1.50) | 2.27 (1.96–2.63) | <0.001 | |
| BMI | 0.317 | ||||
| <25 kg/m2 (n = 16,996) | 1.00 (reference) | 1.28 (1.14–1.44) | 2.91 (2.56–3.31) | <0.001 | |
| ≥25 kg/m2 (n = 8800) | 1.00 (reference) | 1.28 (1.12–1.48) | 2.67 (2.28–3.11) | <0.001 | |
| HOMA-IR | 0.557 | ||||
| <2.5 (n = 23,419) | 1.00 (reference) | 1.29 (1.18–1.42) | 2.80 (2.52–3.11) | <0.001 | |
| ≥2.5 (n = 2310) | 1.00 (reference) | 1.20 (0.92–1.56) | 2.84 (2.13–3.79) | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.; Seo, E.; Lee, W. Long Working Hours and the Risk of Glucose Intolerance: A Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 11831. https://doi.org/10.3390/ijerph191811831
Lee Y, Seo E, Lee W. Long Working Hours and the Risk of Glucose Intolerance: A Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(18):11831. https://doi.org/10.3390/ijerph191811831
Chicago/Turabian StyleLee, Yesung, Eunhye Seo, and Woncheol Lee. 2022. "Long Working Hours and the Risk of Glucose Intolerance: A Cohort Study" International Journal of Environmental Research and Public Health 19, no. 18: 11831. https://doi.org/10.3390/ijerph191811831
APA StyleLee, Y., Seo, E., & Lee, W. (2022). Long Working Hours and the Risk of Glucose Intolerance: A Cohort Study. International Journal of Environmental Research and Public Health, 19(18), 11831. https://doi.org/10.3390/ijerph191811831






