Physical Activity, Sedentary Behaviour, Weight Status, and Body Composition among South African Primary Schoolchildren
Abstract
:1. Introduction
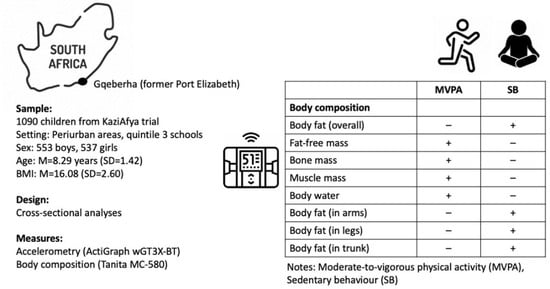
2. Materials and Methods
2.1. Design
2.2. Setting
2.3. Participants and Procedures
2.4. Ethical Considerations
2.5. Measures
2.6. Statistical Analyses
3. Results
3.1. Sample Characteristics and Between-Sex Differences
3.2. Relationship between Sedentary Behaviour, MVPA, Weight Status, and Body Composition
3.3. Differences between Children Who Meet vs. Do Not Meet Recommended MVPA Levels
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dietz, W.H. Critical periods in childhood for the development of obesity. Am. J. Clin. Nutr. 1994, 59, 955–959. [Google Scholar] [CrossRef] [PubMed]
- Kemper, H.C.G.; Post, G.B.; Twisk, J.W.R.; Van Mechelen, W. Lifestyle and obesity in adolescence and young adulthood: Results from the Amsterdam Growth and Health Longitudinal Study (AGAHLS). Int. J. Obes. Relat. Med. Disord. 1999, 23, S34–S40. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Lobstein, T. Worldwide trends in childhood overweight and obesity. Int. J. Pediatr. Obes. 2006, 1, 11–25. [Google Scholar] [CrossRef]
- De Onis, M.; Blossner, M.; Borghi, E. Global prevalence and trends of overweight and obesity among preschool children. Am. J. Clin. Nutr. 2010, 92, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- World Obesity Federation. Atlas of Childhood Obesity; London. 2019. Available online: https://www.worldobesity.org/nlsegmentation/global-atlas-on-childhood-obesity (accessed on 12 September 2022).
- Moschonis, G.; Siopis, G.; Anastasiou, C.; Iotova, V.; Stefanova, T.; Dimova, R.; Rurik, I.; Radó, A.S.; Cardon, G.; De Craemer, M.; et al. Prevalence of childhood obesity by country, family socio-demographics, and parental obesity in Europe: The Feel4Diabetes study. Nutrients 2022, 14, 1830. [Google Scholar] [CrossRef]
- Liu, W.N.; He, M.Z.; Dambach, P.; Schwertz, R.; Chen, S.; Yu, F.; Marx, M. Trends of overweight and obesity among preschool children from 2013 to 2018: A cross-sectional study in Rhine-Neckar County and the City of Heidelberg, Germany. BMC Public Health 2022, 22, 941. [Google Scholar] [CrossRef]
- Shekar, M.; Popkin, B.M. (Eds.) Prevalence and trends. In Obesity: Health and Economic Consequences of an Impending Global Challenge; World Bank: Washington, DC, USA, 2022; pp. 29–70. [Google Scholar]
- Gonzalez-Alvarez, M.A.; Lazaro-Alquezar, A.; Simon-Fernandez, M.B. Global trends in child obesity: Are figures converging? Int. J. Environ. Res. Public Health 2020, 17, 9252. [Google Scholar] [CrossRef]
- Danquah, F.I.; Ansu-Mensah, M.; Bawontuo, V.; Yeboah, M.; Kuupiel, D. Prevalence, incidence, and trends of childhood overweight/obesity in sub-Saharan Africa: A systematic scoping review. Arch. Public Health 2020, 78, 109. [Google Scholar] [CrossRef]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Mokabane, M.N.; Mashao, M.M.; van Staden, M.; Potgieter, M.J.; Potgieter, A. Low levels of physical activity in female adolescents cause overweight and obesity: Are our schools failing our children? S. Afr. Med. J. 2014, 104, 665–667. [Google Scholar] [CrossRef]
- Reddy, S.P.; Resnicow, K.; James, S.; Funani, I.N.; Kambaran, N.S.; Omardien, R.G.; Masuka, P.; Sewpaul, R.; Vaughan, R.D.; Mbewu, A. Rapid increases in overweight and obesity among South African adolescents: Comparison of data from the South African National Youth Risk Behaviour Survey in 2002 and 2008. Am. J. Public Health 2012, 102, 262–268. [Google Scholar] [CrossRef]
- Shisana, O.; Labadarios, D.; Rehle, T.A. South African National Health and Nutrition Examination Survey (SANHANES-1); HSRC Press: Cape Town, South Africa, 2013. [Google Scholar]
- Armstrong, M.E.G.; Lambert, M.I.; Lambert, E.V. Relationship between different nutritional anthropometric statuses and health-related fitness of South African primary school children. Ann. Hum. Biol. 2017, 44, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Goon, D.T.; Toriola, A.L.; Shaw, B.S.; Amusa, L.; Khoza, L.; Shaw, I. Body fat percentage of urban South African children: Implications for health and fitness. West Indian Med. J. 2014, 62, 582–588. [Google Scholar] [CrossRef]
- Negash, S.; Agyemang, C.; Matsha, T.E.; Peer, N.; Erasmus, R.T.; Kengne, A.P. Differential prevalence and associations of overweight and obesity by gender and population group among school learners in South Africa: A cross-sectional study. BMC Obes. 2017, 4, 29. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, S.S.; Neophytou, N.; Watson, E.D. Anthropometric profiles of 8–11 year old children from a low-income setting in South Africa. BMC Public Health 2019, 19, 314. [Google Scholar] [CrossRef]
- Otitoola, O.; Oldewage-Theron, W.; Egal, A. Prevalence of overweight and obesity among selected schoolchildren and adolescents in Cofimvaba, South Africa. S. Afr. J. Clin. Nutr. 2021, 34, 97–102. [Google Scholar] [CrossRef]
- Nomatshila, S.C.; Mabunda, S.A.; Puoane, T.; Apalata, T.R. Prevalence of obesity and associated risk factors among children and adolescents in the Eastern Cape Province. Int. J. Environ. Res. Public Health 2022, 19, 2946. [Google Scholar] [CrossRef]
- Lesiapeto, M.; Smuts, C.; Hanekom, S. Risk factors of poor anthropometric status in children under five years of age living in rural districts of the Eastern Cape and KwaZulu-Natal provinces, South Africa. S. Afr. J. Clin. Nutr. 2016, 23, 202–207. [Google Scholar] [CrossRef]
- Debeila, S.; Modjadji, P.; Madiba, S. High prevalence of overall overweight/obesity and abdominal obesity amongst adolescents: An emerging nutritional problem in rural high schools in Limpopo Province, South Africa. Afr. J. Prim. Health Care Fam. Med. 2021, 13, e1–e9. [Google Scholar] [CrossRef]
- McVeigh, J.A.; Norris, S.A.; de Wet, T. The relationship between socio-economic status and physical activity patterns in South African children. Acta Paediatr. 2004, 93, 982–988. [Google Scholar] [CrossRef]
- Tathiah, N.; Moodley, I.; Mubaiwa, V.; Denny, L.; Taylor, M. South Africa’s nutritional transition: Overweight, obesity, underweight and stunting in female primary school learners in rural KwaZulu-Natal, South Africa. S. Afr. Med. J. 2013, 103, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Olshansky, S.J.; Passaro, D.J.; Hershow, R.C.; Layden, J.; Carnes, B.A.; Brody, J.; Ludwig, D.S. A potential decline in life expectancy in the United States in the 21st century. N. Engl. J. Med. 2005, 352, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J. Physical activity, sedentary behaviour and energy balance in the preschool child: Opportunities for early obesity prevention. Proc. Nutr. Soc. 2008, 67, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Wilks, D.C.; Sharp, S.J.; Ekelund, U.; Thompson, S.G.; Mander, A.P.; Turner, R.M.; Jebb, S.A.; Lindroos, A.K. Objectively measured physical activity and fat mass in children: A bias-adjusted meta-analysis of prospective studies. PLoS ONE 2011, 6, e17205. [Google Scholar] [CrossRef]
- Martinez-Gomez, D.; Eisenmann, J.C.; Tucker, J.; Heelan, K.A.; Welk, G.J. Associations between moderate-to-vigorous physical activity and central body fat in 3–8-year-old children. Int. J. Pediatr. Obes. 2011, 6, e611–e614. [Google Scholar] [CrossRef]
- Ekelund, U.; Luan, J.A.; Sherar, L.B.; Esliger, D.W.; Griew, P.; Cooper, A. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA 2012, 307, 704–712. [Google Scholar] [CrossRef]
- Jiménez-Pavón, D.; Kelly, J.; Reilly, J.J. Associations between objectively measured habitual physical activity and adiposity in children and adolescents: Systematic review. Int. J. Pediatr. Obes. 2010, 5, 3–18. [Google Scholar] [CrossRef]
- Bahia, L.; Schaan, C.W.; Sparrenberger, K.; Abreu, G.D.A.; Barufaldi, L.A.; Coutinho, W.; Schaan, B.D. Overview of meta-analysis on prevention and treatment of childhood obesity. J. Pediatr. 2019, 95, 385–400. [Google Scholar] [CrossRef]
- Cesa, C.C.; Molino, G.O.G.; Lima, J.; Pereira, R.B.; Eibel, B.; Barbiero, S.M.; Schaan, B.D.; Pellanda, L.C. Physical activity and cardiovascular risk factors in children: A meta-analysis update. Int. J. Cardiovasc. Sci. 2022, 35, 304–315. [Google Scholar] [CrossRef]
- Mamabolo, R.L.; Kruger, H.S.; Lennox, A.; Monyeki, M.; Pienaar, A.; Underhay, C.; Czlapka-Matyasik, M. Habitual physical activity and body composition of black township adolescents residing in the North West Province, South Africa. Public Health Nutr. 2007, 10, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Kruger, H.S.; Venter, C.S.; Vorster, H.H.; Margetts, B.M. Physical inactivity is the major determinant of obesity in black women in the North West province, South Africa: The THUSA study. Transition and health during urbanisation of South Africa. Nutrition 2002, 18, 422–427. [Google Scholar] [CrossRef]
- Wong, M.L.; Shiau, S.; Yin, M.T.; Strehlau, R.; Patel, F.; Coovadia, A.; Micklesfield, L.; Kuhn, L.; Arpadi, S.M. Decreased vigorous physical activity in school-aged children with human immunodeficiency virus in Johannesburg, South Africa. J. Pediatr. 2016, 172, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Truter, L.; Pienaar, A.E.; Du Toit, D. The relationship of overweight and obesity to the motor performance of children living in South Africa. S. Afr. Fam. Pract. 2012, 54, 429–435. [Google Scholar] [CrossRef]
- Zeng, Q.; Dong, S.Y.; Sun, X.N.; Xie, J.; Cui, Y. Percentage body fat is a better predictor of cardiovascular risk factors than body mass index. Braz. J. Med. Biol. Res. 2012, 45, 591–600. [Google Scholar] [CrossRef]
- Fritz, J.; Cöster, M.E.; Stenevi-Lundgren, S.; Nilsson, J.; Dencker, M.; Rosengren, B.E.; Karlsson, M.K. A 5-year exercise program in children improves muscle strength without affecting fracture risk. Eur. J. Appl. Physiol. 2016, 116, 707–715. [Google Scholar] [CrossRef]
- Tan, V.P.S.; Macdonald, H.M.; Kim, S.; Nettlefold, L.; Gabel, L.; Ashe, M.C.; McKay, H.A. Influence of physical activity on bone strength in children and adolescents: A systematic review and narrative synthesis. J. Bone Miner. Res. 2014, 29, 2161–2181. [Google Scholar] [CrossRef]
- Gerber, M.; Ayekoé, S.A.; Beckmann, J.; Bonfoh, B.; Coulibaly, J.T.; Daouda, D.; du Randt, R.; Finda, L.; Gall, S.; Mollel, G.J.; et al. Effects of school-based physical activity and multi-micronutrient supplementation intervention on growth, health and wellbeing of schoolchildren in three African countries: The KaziAfya cluster randomised controlled trial protocol using a 2 × 2 factorial design. Trials 2020, 21, 22. [Google Scholar] [CrossRef]
- Beckmann, J.; Lang, C.; du Randt, R.; Gresse, A.; Long, K.Z.; Ludyga, S.; Müller, I.; Nqweniso, S.; Pühse, U.; Utzinger, J.; et al. Prevalence of stunting and relationship between stunting and associated risk factors with academic achievement and cognitive function: A cross-sectional study with South African primary school children. Int. J. Environ. Res. Public Health 2021, 18, 4218. [Google Scholar] [CrossRef]
- Gerber, M.; Ayekoé, S.A.; Beckmann, J.; Bonfoh, B.; Kouassi, B.; Gba, B.C.; Traoré, S.G.; Coulibaly, J.T.; Daouda, D.; du Randt, R.; et al. Moderate-to-vigorous physical activity is associated with cardiorespiratory fitness among primary schoolchildren living in Côte d’Ivoire, South Africa, and Tanzania. Front. Public Health 2021, 9, 671782. [Google Scholar] [CrossRef]
- Gerber, M.; Ayekoé, S.A.; Bonfoh, B.; Coulibaly, J.T.; Daouda, D.; Gba, B.C.; Kouassi, B.; Traoré, S.G.; du Randt, R.; Nqweniso, S.; et al. Is grip strength linked to body composition and cardiovascular risk markers in primary schoolchildren? Cross-sectional data from three African countries. BMJ Open 2022, 12, e052326. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Lang, C.; Beckmann, J.; Degen, J.; du Randt, R.; Gall, S.; Long, K.Z.; Müller, I.; Nienaber, M.; Steinmann, P.; et al. Associations between household socioeconomic status, car ownership, physical activity, and cardiorespiratory fitness in South African primary schoolchildren living in marginalized communities. J. Phys. Act. Health 2021, 18, 883–894. [Google Scholar] [CrossRef] [PubMed]
- Long, K.Z.; Beckmann, J.; Lang, C.; Seelig, H.; Nqweniso, S.; Probst-Hensch, N.; Müller, I.; Pühse, U.; Steinmann, P.; du Randt, R.; et al. Associations of growth impairment and body composition among South African school-aged children enrolled in the KaziAfya project. Nutrients 2021, 13, 2735. [Google Scholar] [CrossRef]
- Long, K.Z.; Beckmann, J.; Lang, C.; Seelig, H.; Nqweniso, S.; Probst-Hensch, N.; Müller, I.; Pühse, U.; Steinmann, P.; du Randt, R.; et al. Impact of a school-based health intervention program on body composition among South African primary schoolchildren: Results from the KaziAfya cluster-randomized controlled trial. BMC Med. 2022, 20, 27. [Google Scholar] [CrossRef]
- Nqweniso, S.; Walter, C.; du Randt, R.; Adams, L.; Beckmann, J.; Degen, J.; Gall, S.; Joubert, N.; Lang, C.; Long, K.Z.; et al. Physical activity, cardiorespiratory fitness and clustered cardio-vascular risk in South African primary schoolchildren from disadvantaged communities: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 2080. [Google Scholar] [CrossRef] [PubMed]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; Mcdowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Clemente, F.M.; Nikolaidis, P.T.; Martins, F.M.; Mendes, R.S. Physical activity patterns in university students: Do they follow the public health guidelines? PLoS ONE 2016, 11, e0152516. [Google Scholar] [CrossRef]
- Aadland, E.; Andersen, L.B.; Skrede, T.; Ekelund, U.; Anderssen, S.A.; Resaland, G.K. Reproducibility of objectively measured physical activity and sedentary time over two seasons in children; comparing a day-by-day and a week-by-week approach. PLoS ONE 2017, 12, e0189304. [Google Scholar] [CrossRef]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef]
- De Onis, M. Development of a who growth reference for school-aged children and adolescents. Bull. World Health Org. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Weststrate, J.A.; Deurenberg, P. Body composition in children: Proposal for a method for calculating body fat percentage from total body density or skinfold-thickness measurements. Am. J. Clin. Nutr. 1989, 50, 1104–1115. [Google Scholar] [CrossRef] [PubMed]
- West, S.G.; Finch, J.F.; Curran, P.J. Structural equation models with nonnormal variables: Problems and remedies. In Structural Equation Modeling Concepts, Issues, and Applications; Hoyle, R.H., Ed.; Sage: Thousand Oakes, CA, USA, 1995; pp. 56–75. [Google Scholar]
- Nyati, L.H.; Pettifor, J.M.; Norris, S.A. The prevalence of malnutrition and growth percentiles for urban South African children. BMC Public Health 2019, 19, 492. [Google Scholar] [CrossRef] [PubMed]
- Hallal, P.C.; Reichert, F.F.; Ekelund, U.; Dumith, S.C.; Menezes, A.M.; Victora, C.; Wells, J. Bidirectional cross-sectional and prospective associations between physical activity and body composition in adolescence: Birth cohort study. J. Sports Sci. 2012, 30, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Lundeen, E.A.; Norris, S.A.; Adair, L.S.; Richter, L.M.; Stein, A.D. Sex differences in obesity incidence: 20-year prospective cohort in South Africa. Pediatr. Obes. 2016, 11, 75–80. [Google Scholar] [CrossRef]
- Nyberg, G.; Ekelund, U.; Yucel-Lindberg, T.L.; Modeér, T.; Marcus, C. Differences in metabolic risk factors between normal weight and overweight children. Int. J. Pediatr. Obes. 2011, 6, 244–252. [Google Scholar] [CrossRef]
- Juonala, M.; Magnussen, C.G.; Berenson, G.S.; Venn, A.; Burns, T.L.; Sabin, M.A.; Raitakari, O.T. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N. Engl. J. Med. 2011, 365, 1876–1885. [Google Scholar] [CrossRef]
- Muller, D.C.; Murphy, N.; Johansson, M.; Ferrari, P.; Tsilidis, K.K.; Boutron-Ruault, M.C.; Brennan, P. Modifiable causes of premature death in middle-age in Western Europe: Results from the EPIC cohort study. BMC Med. 2016, 14, 87. [Google Scholar] [CrossRef]
- Uys, M.; Bassett, S.; Draper, C.E.; Micklesfield, L.; Monyeki, M.A.; De Villiers, A.; Lambert, E.V. Results from South Africa’s 2016 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Health 2016, 13, S265–S273. [Google Scholar] [CrossRef]
- Nqweniso, S.; Walter, C.; du Randt, R.; Aerts, A.; Adams, L.; Degen, J.; Gerber, M. Prevention of overweight and hypertension through cardiorespiratory fitness and extracurricular sport participation among South African schoolchildren. Sustainability 2020, 12, 6581. [Google Scholar] [CrossRef]
- Riddoch, C.J.; Leary, S.D.; Ness, A.R.; Blair, S.N.; Deere, K.; Mattocks, C.; Griffiths, A.; Smith, G.D.; Tilling, K. Prospective associations between objective measures of physical activity and fat mass in 12-14 year old children: The Avon Longitudinal Study of Parents and Children (ALSPAC). BMJ 2009, 339, b4544. [Google Scholar] [CrossRef] [Green Version]
- Metcalf, B.S.; Hosking, J.; Jeffery, A.N.; Voss, L.D.; Henley, W.; Wilkin, T.J. Fatness leads to inactivity, but inactivity does not lead to fatness: A longitudinal study with children. Arch. Dis. Child. 2010, 96, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Morano, M.; Colella, D.; Robazza, C.; Bortoli, L.; Capranica, L. Physical self-perception and motor performance in normal-weight, overweight and obese children. Scand. J. Med. Sci. Sports 2011, 21, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Raustorp, A.; Archer, T.; Svensson, K.; Perlinger, T.; Alricsson, M. Physical self-esteem, a five year follow-up study on Swedish adolescents. Int. J. Adolesc. Med. Health 2009, 21, 497–508. [Google Scholar] [CrossRef] [PubMed]
- Webster-Gandy, J.; Warren, J.; Henry, C.J.K. Sexual dimorphism in fat patterning in a sample of 5 to 7-year old children in Oxford. Int. J. Obes. 2003, 54, 467–471. [Google Scholar] [CrossRef]
- WHO. Obesity: Preventing and Managing the Global Epidemic; Technical Report Series No. 894; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Martorell, R.; Khan, L.K.; Hughes, M.; Grummer-Strawn, L. Obesity in women from developing countries. Eur. J. Clin. Nutr. 2000, 54, 247–252. [Google Scholar] [CrossRef]
- Armstrong, N.; Welsman, J. Youth cardiorespiratory fitness: Evidence, myths and misconceptions. Bull. World Health Organ. 2019, 97, 777–782. [Google Scholar] [CrossRef]
- Mamabolo, R.L.; Alberts, M.; Steyn, N.P.; Waal, H.A.D.-V.D.; Levitt, N.S. Prevalence and determinants of stunting and overweight in 3-year-old black South African children residing in the Central Region of Limpopo Province, South Africa. Public Health Nutr. 2005, 8, 501–508. [Google Scholar] [CrossRef]
- Boeke, C.E.; Oken, E.; Kleinman, K.P.; Rifas-Shiman, S.L.; Taveras, E.M.; Gillman, M.W. Correlations among adiposity measures in school-aged children. BMC Pediatr. 2013, 13, 99. [Google Scholar] [CrossRef]
- Cheng, M.-F.; Chen, Y.-Y.; Jang, T.-R.; Lin, W.-L.; Chen, J.; Hsieh, K.-C. Total body composition estimated by standing-posture 8-electrode bioelectrical impedance analysis in male wrestlers. Biol. Sport 2016, 33, 399–405. [Google Scholar] [CrossRef]
- Hallal, P.C.; Reichert, F.F.; Clark, V.L.; Cordeira, K.L.; Menezes, A.M.B.; Eaton, S.; Ekelund, U.; Wells, J.C. Energy expenditure compared to physical activity measured by accelerometry and self-report in adolescents: A validation study. PLoS ONE 2013, 8, e77036. [Google Scholar] [CrossRef]
- Rowlands, A.V. Accelerometer assessment of physical activity in children: An update. Pediatr. Exerc. Sci. 2007, 19, 252–266. [Google Scholar] [CrossRef] [PubMed]
- Lynch, B.A.; Kaufman, T.K.; Rajjo, T.I.; Mohammed, K.; Kumar, S.; Murad, M.H.; Gentile, N.E.; Koepp, G.A.; McCrady-Spitzer, S.K.; Levine, J.A. Accuracy of accelerometers for measuring physical activity and levels of sedentary behavior in children: A systematic review. J. Prim. Care Community Health 2019, 10, 2150132719874252. [Google Scholar] [CrossRef] [PubMed]



| Metric Variable | M | SD | Min | Max | Skew | Kurt |
|---|---|---|---|---|---|---|
| Accelerometry | ||||||
| Sedentary behaviour (min/day) | 609.0 | 69.1 | 339.8 | 852.3 | −0.17 | 0.22 |
| MVPA (min/day) | 82.2 | 27.7 | 15.7 | 211.9 | 0.61 | 0.58 |
| Body composition: overall | ||||||
| Body fat (in kg) | 5.9 | 3.1 | 1.7 | 25.1 | 3.00 | 11.42 |
| Body fat (in %) | 22.6 | 5.3 | 9.3 | 48.8 | 1.45 | 3.38 |
| Fat-free mass (in kg) | 19.4 | 4.2 | 10.6 | 38.1 | 0.92 | 1.31 |
| Fat-free mass (in %) | 77.4 | 5.6 | 51.1 | 90.6 | −1.45 | 3.36 |
| Bone mass (in kg) | 1.1 | 0.2 | 0.6 | 2.0 | 0.69 | 0.90 |
| Bone mass (in %) | 4.4 | 0.5 | 2.7 | 5.6 | −0.30 | 0.16 |
| Muscle mass (in kg) | 18.3 | 4.0 | 10.0 | 36.2 | 0.93 | 1.33 |
| Muscle mass (in %) | 73.1 | 4.9 | 48.7 | 85.3 | −1.48 | 3.54 |
| Body water (in kg) | 14.2 | 3.1 | 7.8 | 27.9 | 0.92 | 1.30 |
| Body water (in %) | 56.7 | 3.9 | 37.5 | 68.4 | −1.40 | 3.35 |
| Body composition: arms | ||||||
| Body fat (in kg) | 0.7 | 0.4 | 0.2 | 3.9 | 3.23 | 14.33 |
| Body fat (in %) | 33.5 | 5.7 | 16.7 | 61.9 | 0.91 | 2.07 |
| Fat-free mass (in kg) | 1.4 | 0.5 | 0.3 | 3.5 | 0.93 | 1.37 |
| Fat-free mass (in %) | 66.5 | 5.7 | 38.1 | 83.3 | −0.91 | 2.07 |
| Body composition: legs | ||||||
| Body fat (in kg) | 2.4 | 1.3 | 0.4 | 10.8 | 2.93 | 11.38 |
| Body fat (in %) | 5.2 | 0.8 | 9.8 | 51.8 | 0.76 | 1.88 |
| Fat-free mass (in kg) | 5.6 | 1.8 | 1.6 | 14.5 | 1.10 | 2.23 |
| Fat-free mass (in %) | 70.7 | 5.2 | 48.2 | 90.2 | −0.76 | 1.88 |
| Body composition: trunk | ||||||
| Body fat (in kg) | 2.8 | 1.5 | 0.3 | 11.4 | 2.81 | 10.19 |
| Body fat (in %) | 17.8 | 5.3 | 3.0 | 44.1 | 1.48 | 3.61 |
| Fat-free mass (in kg) | 12.4 | 2.0 | 7.6 | 21.1 | 0.71 | 0.82 |
| Fat-free mass (in %) | 82.2 | 5.3 | 55.8 | 97.2 | −1.47 | 3.61 |
| Age and anthropometric measures | ||||||
| Age (in years) | 8.3 | 1.4 | 5.7 | 13.2 | 0.28 | −0.72 |
| Height (in cm) | 124.6 | 9.1 | 102.0 | 152.0 | 0.21 | −0.34 |
| Weight (in kg) | 25.3 | 6.7 | 13.5 | 61.2 | 1.74 | 4.64 |
| BMI (in kg/m2) | 16.1 | 2.6 | 10.5 | 29.9 | 2.11 | 6.14 |
| Categorical variables | N | % | ||||
| Sex | ||||||
| Boys | 553 | 50.7 | ||||
| Girls | 537 | 49.3 | ||||
| Weight status | ||||||
| Underweight | 49 | 4.5 | ||||
| Normal weight | 862 | 79.1 | ||||
| Overweight | 107 | 9.8 | ||||
| Obese | 72 | 6.6 | ||||
| High body fat | ||||||
| No | 1006 | 92.3 | ||||
| Yes | 84 | 7.7 |
| Sedentary Behaviour | MVPA | |||||
|---|---|---|---|---|---|---|
| Mixed Logistic Regression | B | SE | 95% CI | B | SE | 95% CI |
| Weight status | ||||||
| Normal weight (reference) | 0 | 0 | ||||
| Underweight | 0.005 | 0.003 | −0.001; 0.010 | 0.006 | 0.006 | −0.005; 0.019 |
| Overweight | 0.001 | 0.002 | −0.002; 0.005 | −0.016 ** | 0.005 | −0.025; −0.006 |
| Obesity | 0.005 * | 0.002 | 0.001; 0.010 | −0.037 *** | 0.007 | −0.051; −0.024 |
| High body fat a | ||||||
| No (reference) | 0 | 0 | ||||
| Yes | 0.006 ** | 0.002 | 0.002; 0.010 | −0.040 *** | 0.007 | −0.054; −0.027 |
| Mixed linear regression | ||||||
| Body composition: overall | ||||||
| Body fat (in %) | 0.009 *** | 0.003 | 0.004; 0.015 | −0.048 *** | 0.006 | −0.060; −0.037 |
| Fat-free mass (in %) | −0.010 *** | 0.003 | −0.015; −0.004 | 0.049 *** | 0.006 | 0.037; 0.060 |
| Bone mass (in %) | −0.001 ** | 0.000 | −0.001; 0.000 | 0.003 *** | 0.001 | 0.002; 0.004 |
| Muscle mass (in %) | −0.009 *** | 0.003 | −0.014; −0.004 | 0.046 *** | 0.006 | 0.035; 0.056 |
| Body water (in %) | −0.007 *** | 0.002 | −0.011; −0.003 | 0.036 *** | 0.004 | 0.027; 0.044 |
| Body fat in specific body parts | ||||||
| Body fat in arms (in %) | 0.014 *** | 0.003 | 0.008; 0.020 | −0.055 *** | 0.006 | −0.068; −0.043 |
| Body fat in legs (in %) | 0.007 ** | 0.003 | 0.002; 0.012 | −0.040 *** | 0.005 | −0.051; −0.029 |
| Body fat in the trunk (in %) | 0.011 *** | 0.003 | 0.006; 0.017 | −0.052 *** | 0.006 | −0.064; −0.040 |
| Not Meeting MVPA Standards (n = 250) | Meeting MVPA Standards (n = 840) | Main Effect: MVPA | Main Effect: Sex | Interaction Effect: MVPA by Sex | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Girls (n = 201) | Boys (n = 49) | Girls (n = 336) | Boys (n = 504) | |||||||||||
| M | SD | M | SD | M | SD | M | SD | F | η2 | F | η2 | F | η2 | |
| Body composition: overall | ||||||||||||||
| Body fat (in %) | 26.4 | 6.3 | 22.1 | 6.4 | 23.4 | 3.9 | 20.6 | 4.4 | 30.31 *** | 0.027 | 68.96 *** | 0.060 | 2.59 | 0.002 |
| Fat-free mass (in %) | 73.7 | 6.3 | 77.9 | 6.4 | 76.6 | 3.9 | 79.5 | 4.5 | 30.37 *** | 0.027 | 68.43 *** | 0.059 | 2.43 | 0.002 |
| Bone mass (in %) | 3.9 | 0.4 | 4.6 | 0.5 | 4.1 | 0.3 | 4.7 | 0.4 | 22.20 *** | 0.020 | 377.61 *** | 0.260 | 1.08 | 0.001 |
| Muscle mass (in %) | 69.7 | 6.0 | 73.4 | 5.9 | 72.5 | 3.7 | 74.8 | 4.2 | 29.88 *** | 0.027 | 54.46 *** | 0.048 | 2.71 | 0.002 |
| Body water (in %) | 53.9 | 4.6 | 57.1 | 4.8 | 56.1 | 2.9 | 58.2 | 3.3 | 28.45 *** | 0.026 | 70.90 *** | 0.061 | 3.05 | 0.003 |
| Body fat in specific body parts | ||||||||||||||
| Body fat in arms (in %) | 37.3 | 6.6 | 32.9 | 6.3 | 34.3 | 4.6 | 31.5 | 5.0 | 25.89 *** | 0.023 | 59.20 *** | 0.052 | 3.35 | 0.003 |
| Body fat in legs (in %) | 33.1 | 5.3 | 28.0 | 6.1 | 30.8 | 3.4 | 26.9 | 4.7 | 23.02 *** | 0.021 | 122.94 *** | 0.102 | 2.23 | 0.002 |
| Body fat in trunk (in %) | 21.2 | 6.7 | 17.9 | 6.4 | 18.1 | 4.2 | 16.1 | 4.5 | 32.08 *** | 0.029 | 36.12 *** | 0.032 | 2.37 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerber, M.; Lang, C.; Beckmann, J.; du Randt, R.; Long, K.Z.; Müller, I.; Nienaber, M.; Probst-Hensch, N.; Steinmann, P.; Pühse, U.; et al. Physical Activity, Sedentary Behaviour, Weight Status, and Body Composition among South African Primary Schoolchildren. Int. J. Environ. Res. Public Health 2022, 19, 11836. https://doi.org/10.3390/ijerph191811836
Gerber M, Lang C, Beckmann J, du Randt R, Long KZ, Müller I, Nienaber M, Probst-Hensch N, Steinmann P, Pühse U, et al. Physical Activity, Sedentary Behaviour, Weight Status, and Body Composition among South African Primary Schoolchildren. International Journal of Environmental Research and Public Health. 2022; 19(18):11836. https://doi.org/10.3390/ijerph191811836
Chicago/Turabian StyleGerber, Markus, Christin Lang, Johanna Beckmann, Rosa du Randt, Kurt Z. Long, Ivan Müller, Madeleine Nienaber, Nicole Probst-Hensch, Peter Steinmann, Uwe Pühse, and et al. 2022. "Physical Activity, Sedentary Behaviour, Weight Status, and Body Composition among South African Primary Schoolchildren" International Journal of Environmental Research and Public Health 19, no. 18: 11836. https://doi.org/10.3390/ijerph191811836
APA StyleGerber, M., Lang, C., Beckmann, J., du Randt, R., Long, K. Z., Müller, I., Nienaber, M., Probst-Hensch, N., Steinmann, P., Pühse, U., Utzinger, J., Nqweniso, S., & Walter, C. (2022). Physical Activity, Sedentary Behaviour, Weight Status, and Body Composition among South African Primary Schoolchildren. International Journal of Environmental Research and Public Health, 19(18), 11836. https://doi.org/10.3390/ijerph191811836