Family Structure and Family Climate in Relation to Health and Socioeconomic Status for Older Adults: A Longitudinal Moderated Mediation Analysis
Abstract
:1. Introduction
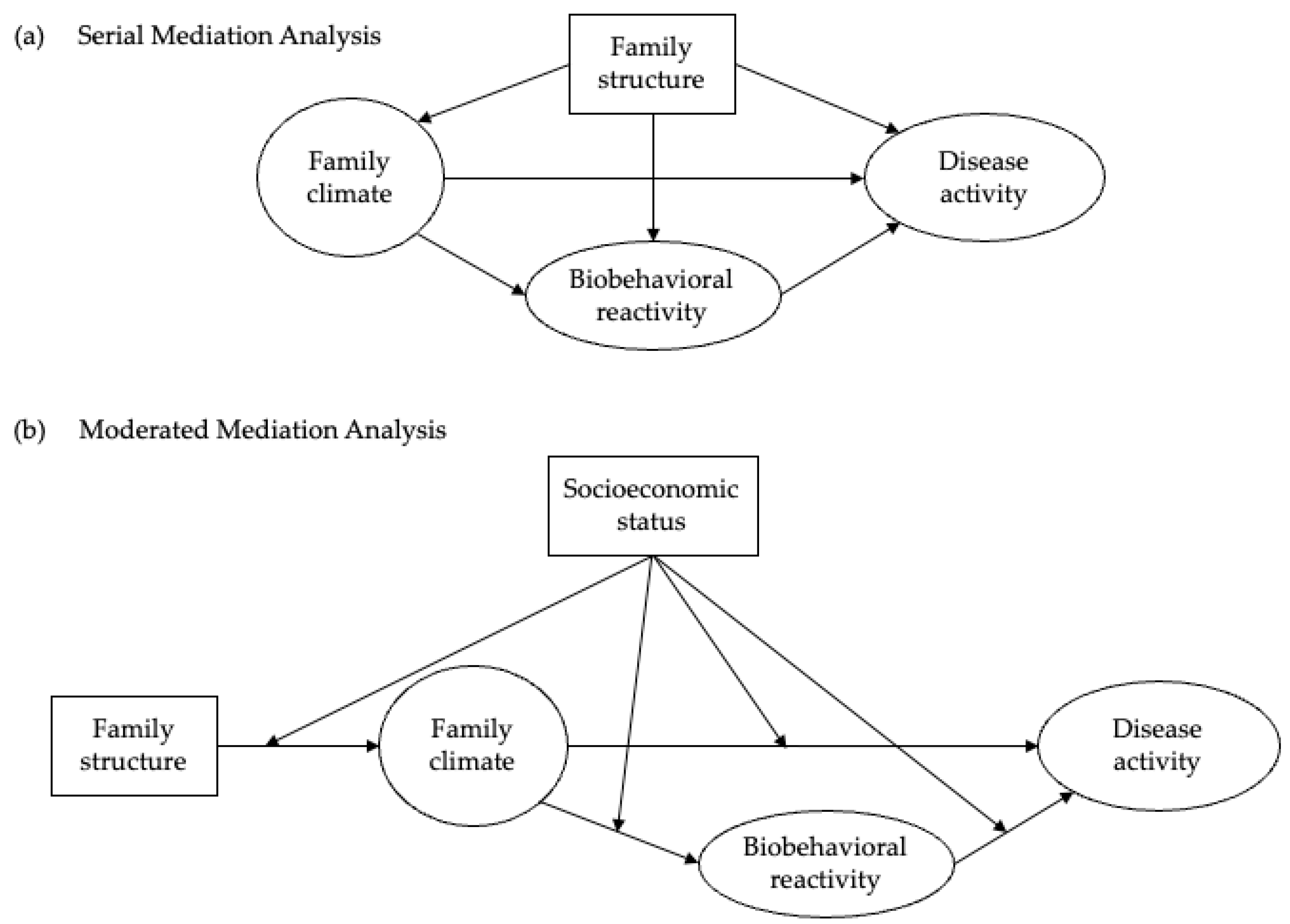
- (a)
- The longitudinal relationship between family structure (i.e., marital status) and later disease activity (i.e., physical health) is mediated by family climate and biobehavioral reactivity (i.e., mental health).
- (b)
- Socioeconomic differences alter the impact of family climate on health outcomes, with weaker health gains for those with lower SES.
2. Materials and Methods
2.1. Data and Sample
2.2. Measures
2.2.1. Family Structure
2.2.2. Family Climate
2.2.3. Biobehavioral Reactivity
2.2.4. Disease Activity
2.2.5. Socioeconomic Status
2.2.6. Potential Confounders
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Baseline Model
3.3. Structural Equation Modelling
4. Discussion
4.1. Contextualization of Findings
4.2. Strengths and Limitations of This Study
4.3. Perspectives and Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Winnicott, D.W. The Family and Individual Development; Routledge: London, UK, 2012. [Google Scholar]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P. Socioeconomic determinants of health: Health and social cohesion: Why care about income inequality? BMJ 1997, 314, 1037. [Google Scholar] [CrossRef] [PubMed]
- Lahelma, E.; Martikainen, P.; Laaksonen, M.; Aittomäki, A. Pathways between socioeconomic determinants of health. J. Epidemiol. Community Health 2004, 58, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, S.V.; Kim, D.J.; Kawachi, I. Social trust and self-rated health in US communities: A multilevel analysis. J. Urban. Health 2002, 79, S21–S34. [Google Scholar] [CrossRef]
- Ahnquist, J.; Wamala, S.P.; Lindstrom, M. Social determinants of health–a question of social or economic capital? Interaction effects of socioeconomic factors on health outcomes. Soc. Sci. Med. 2012, 74, 930–939. [Google Scholar] [CrossRef]
- Braveman, P.; Egerter, S.; Williams, D.R. The social determinants of health: Coming of age. Annu. Rev. Public Health 2011, 32, 381–398. [Google Scholar] [CrossRef]
- Berkman, L.F.; Kawachi, I.; Glymour, M.M. Social Epidemiology; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Tinker, A. The social implications of an ageing population. Mech. Ageing Dev. 2002, 123, 729–735. [Google Scholar] [CrossRef]
- Widmer, E.D. Family Configurations; Routledge: London, UK, 2016. [Google Scholar] [CrossRef]
- Michaelson, V.; Pilato, K.A.; Davison, C.M. Family as a health promotion setting: A scoping review of conceptual models of the health-promoting family. PLoS ONE 2021, 16, e0249707. [Google Scholar] [CrossRef]
- Woods, S.B.; Priest, J.B.; Roberson, P.N.E. Family versus intimate partners: Estimating who matters more for health in a 20-year longitudinal study. J. Fam. Psychol. 2020, 34, 247–256. [Google Scholar] [CrossRef]
- Conger, R.D.; Conger, K.J.; Martin, M.J. Socioeconomic status, family processes, and individual development. J. Marriage Fam. 2010, 72, 685–704. [Google Scholar] [CrossRef]
- Rosland, A.-M.; Heisler, M.; Piette, J.D. The impact of family behaviors and communication patterns on chronic illness outcomes: A systematic review. J. Behav. Med. 2012, 35, 221–239. [Google Scholar] [CrossRef] [PubMed]
- Carr, D.; Springer, K.W. Advances in Families and Health Research in the 21st Century. J. Marriage Fam. 2010, 72, 743–761. [Google Scholar] [CrossRef]
- Umberson, D.; Thomeer, M.B. Family Matters: Research on Family Ties and Health, 2010 to 2020. J. Marriage Fam. 2020, 82, 404–419. [Google Scholar] [CrossRef]
- Herke, M.; Knöchelmann, A.; Richter, M. Health and Well-Being of Adolescents in Different Family Structures in Germany and the Importance of Family Climate. Int. J. Environ. Res. Public Health 2020, 17, 6470. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.B.; Denton, W.H. The biobehavioral family model as a framework for examining the connections between family relationships, mental, and physical health for adult primary care patients. Fam. Syst. Health 2014, 32, 235–240. [Google Scholar] [CrossRef]
- Vanassche, S.; Swicegood, G.; Matthijs, K. Marriage and children as a key to happiness? Cross-national differences in the effects of marital status and children on well-being. J. Happiness Stud. 2013, 14, 501–524. [Google Scholar] [CrossRef]
- Wagner, K.D.; Ritt-Olson, A.; Chou, C.-P.; Pokhrel, P.; Duan, L.; Baezconde-Garbanati, L.; Soto, D.W.; Unger, J.B. Associations between family structure, family functioning, and substance use among Hispanic/Latino adolescents. Psychol. Addict. Behav. 2010, 24, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Zueras, P.; Rutigliano, R.; Trias-Llimós, S. Marital status, living arrangements, and mortality in middle and older age in Europe. Int. J. Public Health 2020, 65, 627–636. [Google Scholar] [CrossRef]
- Kapetanovic, S.; Skoog, T. The Role of the Family’s Emotional Climate in the Links between Parent-Adolescent Communication and Adolescent Psychosocial Functioning. Res. Child. Adolesc. Psychopathol. 2021, 49, 141–154. [Google Scholar] [CrossRef]
- Demo, D.H.; Aquilino, W.S.; Fine, M.A. Family Composition and Family Transitions. In Sourcebook of Family Theory and Research; SAGE Publications: London, UK, 2005; pp. 119–142. [Google Scholar]
- Hank, K.; Wagner, M. Parenthood, Marital Status, and Well-Being in Later Life: Evidence from SHARE. Soc. Indic. Res. 2013, 114, 639–653. [Google Scholar] [CrossRef]
- Hawkins, D.N.; Booth, A. Unhappily ever after: Effects of long-term, low-quality marriages on well-being. Soc. Forces 2005, 84, 451–471. [Google Scholar] [CrossRef]
- Carr, D.; Springer, K.W.; Williams, K. Health and Families. In The Wiley Blackwell Companion of to the Sociology of Families; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2014; pp. 255–276. [Google Scholar]
- Xu, M.; Thomas, P.A.; Umberson, D. Marital Quality and Cognitive Limitations in Late Life. J. Gerontol B. Psychol. Sci. Soc. Sci. 2016, 71, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.L. Beyond the “psychosomatic family”: A biobehavioral family model of pediatric illness. Fam. Process. 1993, 32, 261–278. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.B.; Priest, J.B.; Roush, T. The biobehavioral family model: Testing social support as an additional exogenous variable. Fam. Process. 2014, 53, 672–685. [Google Scholar] [CrossRef]
- Priest, J.B.; Woods, S.B.; Maier, C.A.; Parker, E.O.; Benoit, J.A.; Roush, T.R. The Biobehavioral Family Model: Close relationships and allostatic load. Soc. Sci. Med. 2015, 142, 232–240. [Google Scholar] [CrossRef]
- Park, J.-Y.; Baek, S.-Y.; Kim, H.-S.; Lim, J.-H.; Kim, T.-H. Testing the Biobehavioral Family Model in Understanding the Eating Problems of Adolescent Girls. Child. Health Nurs. Res. 2013, 19, 228. [Google Scholar] [CrossRef]
- Roberson, P.N.E.; Shorter, R.L.; Woods, S.; Priest, J. How health behaviors link romantic relationship dysfunction and physical health across 20 years for middle-aged and older adults. Soc. Sci. Med. 2018, 201, 18–26. [Google Scholar] [CrossRef]
- Priest, J.B.; McNeil Smith, S.; Woods, S.B.; Roberson, P.N.E. Discrimination, family emotional climate, and African American health: An application of the BBFM. J. Fam. Psychol. 2020, 34, 598–609. [Google Scholar] [CrossRef]
- Priest, J.B.; Woods, S.B. The Role of Close Relationships in the Mental and Physical Health of Latino Americans. Fam. Relat. 2015, 64, 319–331. [Google Scholar] [CrossRef]
- Stanton, S.C.E.; Selcuk, E.; Farrell, A.K.; Slatcher, R.B.; Ong, A.D. Perceived Partner Responsiveness, Daily Negative Affect Reactivity, and All-Cause Mortality: A 20-Year Longitudinal Study. Psychosom. Med. 2019, 81, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.B.; Priest, J.B.; Signs, T.L.; Maier, C.A. In sickness and in health: The longitudinal associations between marital dissatisfaction, depression and spousal health. J. Fam. Ther. 2019, 41, 102–125. [Google Scholar] [CrossRef]
- Woods, S.B.; Roberson, P.N.E.; Priest, J.B. Family emotional climate and health: Testing conveyance of effects via psychobiological mediators. Pers. Relatsh. 2020, 27, 674–707. [Google Scholar] [CrossRef]
- Adler, N.E.; Stewart, J. Preface to the biology of disadvantage: Socioeconomic status and health. Ann. N. Y. Acad. Sci. 2010, 1186, 1–4. [Google Scholar] [CrossRef]
- Cutler, D.M.; Lleras-Muney, A.; Vogl, T. Socioeconomic Status and Health: Dimensions and Mechanisms; National Bureau of Economic Research: Cambridge, MA, USA, 2008. [Google Scholar]
- Banovcinova, A.; Levicka, J.; Veres, M. The impact of poverty on the family system functioning. Procedia-Soc. Behav. Sci. 2014, 132, 148–153. [Google Scholar] [CrossRef]
- Botha, F.; Booysen, F.; Wouters, E. Family functioning and socioeconomic status in South African families: A test of the social causation hypothesis. Soc. Indic. Res. 2018, 137, 789–811. [Google Scholar] [CrossRef]
- Mansfield, A.K.; Dealy, J.A.; Keitner, G.I. Family functioning and income: Does low-income status impact family functioning? Fam. J. 2013, 21, 297–305. [Google Scholar] [CrossRef]
- Goldman, N. Social inequalities in health: Disentangling the underlying mechanisms. Ann. N. Y. Acad. Sci. 2001, 954, 118–139. [Google Scholar] [CrossRef] [PubMed]
- Fekete, C.; Reinhardt, J.D.; Arora, M.; Patrick Engkasan, J.; Gross-Hemmi, M.; Kyriakides, A.; Le Fort, M.; Tough, H. Socioeconomic status and social relationships in persons with spinal cord injury from 22 countries: Does the countries’ socioeconomic development moderate associations? PLoS ONE 2021, 16, e0255448. [Google Scholar] [CrossRef]
- Wu, Z.H.; Rudkin, L. Social Contact, Socioeconomic Status, and the Health Status of Older Malaysians. Gerontologist 2000, 40, 228–234. [Google Scholar] [CrossRef]
- Hostinar, C.E.; Ross, K.M.; Chen, E.; Miller, G.E. Modeling the association between lifecourse socioeconomic disadvantage and systemic inflammation in healthy adults: The role of self-control. Health Psychol. 2015, 34, 580–590. [Google Scholar] [CrossRef] [PubMed]
- Stringhini, S.; Berkman, L.; Dugravot, A.; Ferrie, J.E.; Marmot, M.; Kivimaki, M.; Singh-Manoux, A. Socioeconomic Status, Structural and Functional Measures of Social Support, and Mortality. Am. J. Epidemiol. 2012, 175, 1275–1283. [Google Scholar] [CrossRef]
- Robles, T.F.; Slatcher, R.B.; Trombello, J.M.; McGinn, M.M. Marital quality and health: A meta-analytic review. Psychol. Bull. 2014, 140, 140–187. [Google Scholar] [CrossRef]
- Booysen, F.; Botha, F.; Wouters, E. Conceptual causal models of socioeconomic status, family structure, family functioning and their role in public health. BMC Public Health 2021, 21, 191. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.E.; McLanahan, S.S.; Meadows, S.O.; Brooks-Gunn, J. Family structure transitions and maternal parenting stress. J. Marriage Fam. 2009, 71, 558–574. [Google Scholar] [CrossRef] [PubMed]
- Meadows, S.O. Family structure and fathers’ well-being: Trajectories of mental health and self-rated health. J. Health Soc. Behav. 2009, 50, 115–131. [Google Scholar] [CrossRef] [PubMed]
- Saladino, V.; Mosca, O.; Lauriola, M.; Hoelzlhammer, L.; Cabras, C.; Verrastro, V. Is Family Structure Associated with Deviance Propensity during Adolescence? The Role of Family Climate and Anger Dysregulation. Int. J. Environ. Res. Public Health 2020, 17, 9257. [Google Scholar] [CrossRef]
- Litwin, H.; Stoeckel, K.J.; Schwartz, E. Social networks and mental health among older Europeans: Are there age effects? Eur. J. Ageing 2015, 12, 299–309. [Google Scholar] [CrossRef]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S.; on behalf of the SHARE Central Coordination Team. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef]
- Malter, F.; Börsch-Supan, A. SHARE Wave 6: Panel Innovations and Collecting Dried Blood Spots; Munich Center for the Economics of Aging (MEA): Munich, Germany, 2017. [Google Scholar]
- Bergmann, M.; Kneip, T.; De Luca, G.; Scherpenzeel, A. Survey Participation in the Survey of Health, Ageing and Retirement in Europe (SHARE), Wave 1–6; Munich Center for the Economics of Aging: Munich, Germany, 2017. [Google Scholar]
- Wansbeek, T.; Meijer, E. Measurement Error and Latent Variables. In A Companion to Theoretical Econometrics; John Wiley & Sons: Hoboken, NJ, USA, 2001; pp. 162–179. [Google Scholar]
- Paiva, A.F.; Cunha, C.; Voss, G.; Delerue Matos, A. The interrelationship between social connectedness and social engagement and its relation with cognition: A study using SHARE data. Ageing Soc. 2021, 1–19. [Google Scholar] [CrossRef]
- Rattay, P.; Lampert, T.; Neuhauser, H.; Ellert, U. Bedeutung der familialen Lebenswelt für die Gesundheit von Kindern und Jugendlichen. Z. Für Erzieh. 2012, 15, 145–170. [Google Scholar] [CrossRef]
- Signs, T.L.; Woods, S.B. Linking family and intimate partner relationships to chronic pain: An application of the biobehavioral family model. Fam. Syst. Health 2020, 38, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Tetzner, J.; Schuth, M. Anxiety in late adulthood: Associations with gender, education, and physical and cognitive functioning. Psychol. Aging. 2016, 31, 532–544. [Google Scholar] [CrossRef] [PubMed]
- Lazarevič, P. Was Misst Self-Rated Health? Die Basis Subjektiver Gesundheit Und Unterschiede Nach Geschlecht, Alter Und Kohorte in Europa Und Kanada; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar] [CrossRef]
- Galobardes, B.; Lynch, J.; Smith, G.D. Measuring socioeconomic position in health research. Br. Med. Bull. 2007, 81, 21–37. [Google Scholar] [CrossRef]
- De Luca, G.; Rossetti, C.; Malter, F. Sample design and weighting strategies in SHARE Wave 5. Share Wave 2015, 5, 75–84. [Google Scholar]
- Himmelweit, S.; Santos, C.; Sevilla, A.; Sofer, C. Sharing of resources within the family and the economics of household decision making. J. Marriage Fam. 2013, 75, 625–639. [Google Scholar] [CrossRef]
- Darin-Mattsson, A.; Fors, S.; Kåreholt, I. Different indicators of socioeconomic status and their relative importance as determinants of health in old age. Int. J. Equity Health 2017, 16, 173. [Google Scholar] [CrossRef]
- Woody, E. An SEM Perspective on Evaluating Mediation: What Every Clinical Researcher Needs to Know. J. Exp. Psychopathol. 2011, 2, 210–251. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford publications: New York, NY, USA, 2015. [Google Scholar]
- Jose, P.E. The Merits of Using Longitudinal Mediation. Educ. Psychol. 2016, 51, 331–341. [Google Scholar] [CrossRef]
- Wooldridge, J.M. Econometric Analysis of Cross Section and Panel Data; MIT Press: Cambridge, MA, USA, 2010. [Google Scholar]
- Enders, C.K.; Bandalos, D.L. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct. Equ. Modeling 2001, 8, 430–457. [Google Scholar] [CrossRef]
- Hank, K.; Steinbach, A. Families and Health: A Review; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 23–39. [Google Scholar]
- Gellert, P.; Häusler, A.; Gholami, M.; Rapp, M.; Kuhlmey, A.; Nordheim, J. Own and partners’ dyadic coping and depressive symptoms in individuals with early-stage dementia and their caregiving partners. Aging Ment. Health 2018, 22, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Yun, Q.; Jiang, X.; Chang, C. Family SES, family social capital, and general health in Chinese adults: Exploring their relationships and the gender-based differences. BMC Public Health 2020, 20, 1401. [Google Scholar] [CrossRef] [PubMed]
- Lesthaeghe, R. The second demographic transition, 1986–2020: Sub-replacement fertility and rising cohabitation—a global update. Genus 2020, 76, 1–38. [Google Scholar] [CrossRef]
- Wood, B.L.; Woods, S.B.; Sengupta, S.; Nair, T. The Biobehavioral Family Model: An Evidence-Based Approach to Biopsychosocial Research, Residency Training, and Patient Care. Front. Psychiatry 2021, 12, 725045. [Google Scholar] [CrossRef]

| Variable | Category | Values | N (%) | |
|---|---|---|---|---|
| Time 1 | Age (mean, ±SD) | 50–101 | 65.44 (10.38) | |
| Sex | Female | 16,711 (56.73) | ||
| Male | 12,746 (43.27) | |||
| Migration background | Migrant | 2866 (9.73) | ||
| Non-migrant | 26,591 (90.27) | |||
| Education | Low | 12,275 (41.67) | ||
| Mid | 11,329 (38.46) | |||
| High | 5856 (19.88) | |||
| Household income | Low tertile | 9830 (33.37) | ||
| Mid tertile | 9786 (33.22) | |||
| High tertile | 9842 (33.41) | |||
| Socioeconomic status (SES) | Low SES | 11,061 (37.55) | ||
| Medium SES | 10,849 (36.83) | |||
| High SES | 7547 (25.62) | |||
| Family structure | Married | 20,867 (70.84) | ||
| Widowed | 4354 (14.78) | |||
| Divorced | 2577 (8.75) | |||
| Single/never married | 1658 (5.63) | |||
| Family climate (mean, ±SD) | Diversity of relations | 0–4 | 2.09 (1.12) | |
| Proximity | 0–4 | 1.75 (0.89) | ||
| Contact | 0–4 | 1.83 (0.88) | ||
| Emotional closeness | 0–4 | 1.77 (0.96) | ||
| Number of family members | 0–4 | 1.65 (0.90) | ||
| Family responsibilities (mean, ±SD) | 0.24 (0.56) | |||
| Family support (mean, ±SD) | 0.27 (0.66) | |||
| Children | One or more | 26,656 (90.49) | ||
| None | 2801 (9.51) | |||
| Living arrangement | Cohabiting with someone | 18,531 (62.91) | ||
| Living alone | 10,926 (37.09) | |||
| Biobehavioral reactivity (mean, ±SD) | EURO-D | 0–12 | 2.59 (2.30) | |
| BAI-5 | 0–20 | 6.21 (4.52) | ||
| Disease activity (mean, ±SD) | Self-rated health | 1–5 | 3.25 (1.08) | |
| Number chronic diseases | 0–11 | 1.74 (1.55) | ||
| Time 2 | Biobehavioral reactivity (mean, ±SD) | EURO-D | 0–12 | 2.43 (2.24) |
| BAI-5 | 0–20 | 5.91 (4.60) | ||
| Time 3 | Disease activity (mean, ±SD) | Self-rated health | 1–5 | 3.30 (1.05) |
| Number chronic diseases | 0–11 | 1.91 (1.64) |
| Variable | Direct Effect | Indirect Effect | Total Effect |
|---|---|---|---|
| Family climate | |||
| Family structure | |||
| Married | Reference | Reference | Reference |
| Widow | −0.098 *** (0.008) | −0.098 *** (0.008) | |
| Divorced | −0.011 *** (0.013) | −0.011 *** (0.013) | |
| Single/never married | −0.157 *** (−0.010) | −0.157 *** (−0.010) | |
| Support | 0.052 *** (0.004) | 0.052 *** (0.004) | |
| Responsibilities | 0.139 *** (0.005) | 0.139 *** (0.005) | |
| Presence of children | 0.101 *** (−0.004) | 0.101 *** (−0.004) | |
| Biobehavioral reactivity | |||
| Family climate | −0.095 *** (0.017) | −0.095 *** (0.017) | |
| Family structure | |||
| Married | Reference | Reference | Reference |
| Widowed | 0.213 (0.017) | 0.009 *** (0.002) | 0.222 (0.027) |
| Divorced/separated | −0.006 (0.016) | 0.010 *** (0.003) | 0.004 (0.032) |
| Single/never married | −0.056 (0.040) | 0.015 *** (0.002) | −0.041 (0.040) |
| Presence of children | −0.010 *** (0.002) | −0.010 *** (0.002) | |
| Family responsibilities | −0.013 *** (0.002) | −0.013 *** (0.002) | |
| Family support | −0.005 *** (0.001) | −0.005 *** (0.001) | |
| Depression T1 | 0.411 *** (0.005) | 0.411 *** (0.005) | |
| Anxiety T1 | 0.101 *** (0.002) | 0.101 *** (0.002) | |
| Disease activity | |||
| Family climate | −0.031 *** (0.007) | −0.010 *** (0.002) | −0.041 *** (0.007) |
| Biobehavioral reactivity | 0.102 *** (0.003) | 0.102 *** (0.003) | |
| Family structure | |||
| Married | Reference | Reference | Reference |
| Widowed | −0.023 (0.013) | 0.026 *** (0.003) | 0.003 (0.013) |
| Divorced/separated | 0.016 (0.014) | 0.003 ** (0.003) | 0.019 (0.014) |
| Single/never married | 0.010 (0.017) | 0.001 (0.004) | 0.011 (0.017) |
| Support | −0.002 *** (0.001) | −0.002 *** (0.001) | |
| Responsibilities | −0.006 *** (0.001) | −0.006 *** (0.001) | |
| Presence of children | −0.004 *** (0.001) | −0.004 *** (0.001) | |
| Female (Ref: Male) | −0.021 ** (0.001) | −0.021 ** (0.008) | |
| Age | 0.011 *** (0.001) | 0.011 *** (0.001) | |
| Socioeconomic status | −0.088 *** (0.005) | −0.088 *** (0.005) | |
| Migrant (Ref: Non-migrant) | 0.024 * (0.013) | 0.024 * (0.013) | |
| Cohabiting (Ref: Living alone) | −0.014 * (0.009) | −0.014 * (0.009) | |
| Depression T1 | 0.042 *** (0.001) | 0.042 *** (0.001) | |
| Anxiety T1 | 0.010 *** (0.001) | 0.010 *** (0.001) | |
| Self-rated health T1 | 0.331 *** (0.003) | 0.169 *** (0.003) | |
| Chronic diseases T1 | 0.169 *** (0.005) | 0.331 *** (0.005) |
| Variable | Low SES | Mid SES | High SES |
|---|---|---|---|
| Family climate | |||
| Family structure | |||
| Married | Reference | Reference | Reference |
| Widow | −0.114 *** (0.011) | −0.071 *** (0.014) | −0.048 * (0.012) |
| Divorced | −0.176 *** (0.017) | −0.086 *** (0.014) | −0.050 * (0.012) |
| Single/never married | −0.222 *** (0.020) | −0.163 *** (0.019) | −0.047 * (0.021) |
| Support | 0.073 *** (0.006) | 0.039 *** (0.006) | 0.052 *** (0.010) |
| Responsibilities | 0.125 *** (0.008) | 0.141 *** (0.007) | 0.138 *** (0.011) |
| Presence of children | −0.091 *** (0.005) | 0.103 *** (0.005) | 0.135 *** (0.005) |
| Biobehavioral reactivity | |||
| Family climate | −0.055 ** (0.028) | −0.077 *** (0.025) | −0.119 *** (0.029) |
| Biobehavioral reactivity | 0.416 *** (0.008) | 0.393 *** (0.007) | 0.406 *** (0.009) |
| Female (Ref: Male) | 0.122 *** (0.003) | 0.094 *** (0.003) | 0.071 *** (0.004) |
| Disease activity | |||
| Family climate | −0.014 ** (0.010) | −0.038 *** (0.010) | −0.057 *** (0.014) |
| Biobehavioral reactivity | 0.103 *** (0.004) | 0.104 *** (0.004) | 0.101 *** (0.007) |
| Female (Ref: Male) | 0.004 ** (0.012) | −0.036 ** (0.011) | −0.058 *** (0.016) |
| Age | 0.013 *** (0.000) | 0.011 *** (0.000) | 0.010 *** (0.001) |
| Migrant (Ref: Non-migrant) | 0.072 * (0.023) | 0.033 *** (0.019) | 0.029 * (0.023) |
| Cohabiting (Ref: Living alone) | 0.037 *** (0.012) | −0.003 * (0.011) | −0.036 * (0.016) |
| Self-rated health T1 | 0.316 *** (0.007) | 0.340 *** (0.007) | 0.341 *** (0.009) |
| Chronic diseases T1 | 0.152 *** (0.004) | 0.179 *** (0.004) | 0.198 *** (0.006) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alonso-Perez, E.; Gellert, P.; Kreyenfeld, M.; O’Sullivan, J.L., on behalf of the the Consortium for the Proposed Einstein Center for Population Diversity. Family Structure and Family Climate in Relation to Health and Socioeconomic Status for Older Adults: A Longitudinal Moderated Mediation Analysis. Int. J. Environ. Res. Public Health 2022, 19, 11840. https://doi.org/10.3390/ijerph191811840
Alonso-Perez E, Gellert P, Kreyenfeld M, O’Sullivan JL on behalf of the the Consortium for the Proposed Einstein Center for Population Diversity. Family Structure and Family Climate in Relation to Health and Socioeconomic Status for Older Adults: A Longitudinal Moderated Mediation Analysis. International Journal of Environmental Research and Public Health. 2022; 19(18):11840. https://doi.org/10.3390/ijerph191811840
Chicago/Turabian StyleAlonso-Perez, Enrique, Paul Gellert, Michaela Kreyenfeld, and Julie Lorraine O’Sullivan on behalf of the the Consortium for the Proposed Einstein Center for Population Diversity. 2022. "Family Structure and Family Climate in Relation to Health and Socioeconomic Status for Older Adults: A Longitudinal Moderated Mediation Analysis" International Journal of Environmental Research and Public Health 19, no. 18: 11840. https://doi.org/10.3390/ijerph191811840
APA StyleAlonso-Perez, E., Gellert, P., Kreyenfeld, M., & O’Sullivan, J. L., on behalf of the the Consortium for the Proposed Einstein Center for Population Diversity. (2022). Family Structure and Family Climate in Relation to Health and Socioeconomic Status for Older Adults: A Longitudinal Moderated Mediation Analysis. International Journal of Environmental Research and Public Health, 19(18), 11840. https://doi.org/10.3390/ijerph191811840






