Actionable Predictive Factors of Homelessness in a Psychiatric Population: Results from the REHABase Cohort Using a Machine Learning Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Database Evaluation
2.1.1. Population
2.1.2. Baseline Assessment
2.1.3. Clinical and Functioning Measures
2.2. Homelessness in the REHABase Database
2.3. Representativeness and Validation of the Database
2.4. Estimates of Homelessness Predictors’ Importance
2.4.1. Variable Selection
2.4.2. Machine Learning Model
2.4.3. Hyperparameter Tuning for Estimates of Predictors’ Importance
2.5. Post Hoc Analysis of Psychotropic Medications
2.6. Cognitive Factors Exploratory Analysis
3. Results
3.1. Representativeness and Validation of the Database
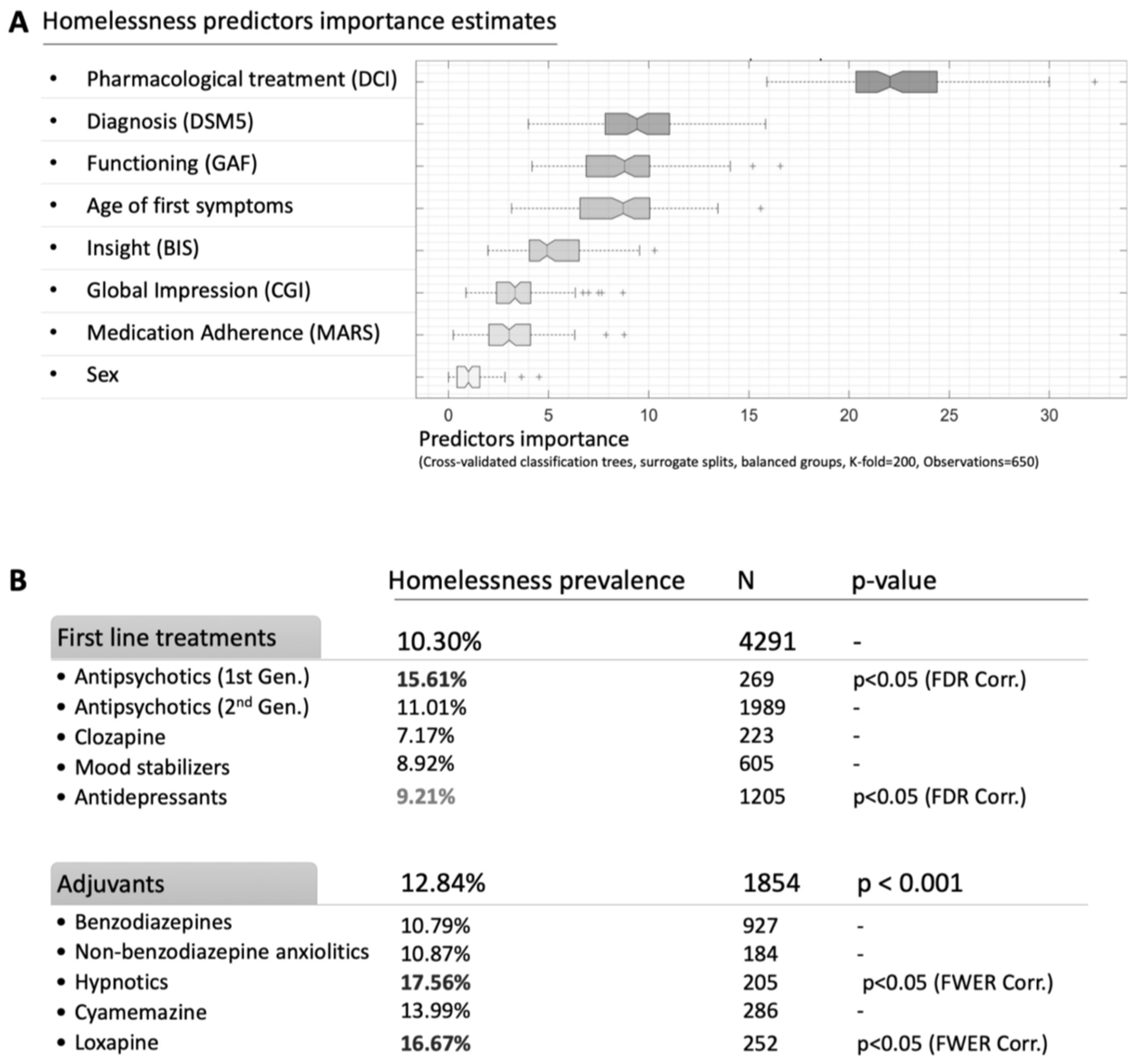
3.2. Estimates of Homelessness Predictors Importance
3.3. Post Hoc Analysis of the Psychotropic Medication
3.4. Exploratory Analysis of Cognitive Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Busch-Geertsema, V.; Edgar, W.; O’Sullivan, E.; Pleace, N. Homelessness and Homeless Policies in Europe: Lessons from Research. In Proceedings of the European Consensus Conference on Homelessness, Brussels, Belgium, 9–10 December 2010. [Google Scholar]
- Wagner, D.; Gilman, J.B. Confronting Homelessness: Poverty, Politics, and the Failure of Social Policy; Lynne Rienner: Boulder, CO, USA, 2012. [Google Scholar]
- Fazel, S.; Geddes, J.R.; Kushel, M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 2014, 384, 1529–1540. [Google Scholar] [CrossRef]
- European Commission. Directorate-General for Employment, Social Affaires and Equal Opportunities. In Joint Report on Social Protection and Social Inclusion 2008: Social Inclusion, Pensions, Healthcare and Long-Term Care; Office for Official Publications of the European Communities: Luxembourg, 2008. [Google Scholar]
- Furber, G.; Leach, M.; Guy, S.; Segal, L. Developing a broad categorisation scheme to describe risk factors for mental illness, for use in prevention policy and planning. Aust. N. Z. J. Psychiatry 2017, 51, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, S.F.; Nordentoft, M.; Hjorthøj, C. Individual-Level Predictors for Becoming Homeless and Exiting Homelessness: A Systematic Review and Meta-analysis. J. Urban Health 2019, 96, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, K.J.; Shelton, K.H.; van den Bree, M.B.M.; Los, F.J. Psychopathology in Young People Experiencing Homelessness: A Systematic Review. Am. J. Public Health 2013, 103, e24–e37. [Google Scholar] [CrossRef]
- Gutwinski, S.; Schreiter, S.; Deutscher, K.; Fazel, S. The prevalence of mental disorders among homeless people in high-income countries: An updated systematic review and meta-regression analysis. PLoS Med. 2021, 18, e1003750. [Google Scholar] [CrossRef]
- Franck, N.; Bon, L.; Dekerle, M.; Plasse, J.; Massoubre, C.; Pommier, R.; Legros-Lafarge, E.; Jaafari, N.; Guillard-Bouhet, N.; Quilès, C.; et al. Satisfaction and Needs in Serious Mental Illness and Autism Spectrum Disorder: The REHABase Psychosocial Rehabilitation Project. Psychiatr. Serv. 2019, 70, 316–323. [Google Scholar] [CrossRef]
- Folsom, D.P.; Hawthorne, W.; Lindamer, L.; Gilmer, T.; Bailey, A.; Golshan, S.; Garcia, P.; Unützer, J.; Hough, R.; Jeste, D.V. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am. J. Psychiatry 2005, 162, 370–376. [Google Scholar] [CrossRef]
- Churchard, A.; Ryder, M.; Greenhill, A.; Mandy, W. The prevalence of autistic traits in a homeless population. Autism 2019, 23, 665–676. [Google Scholar] [CrossRef]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees; Routledge: Oxfordshire, UK, 2017. [Google Scholar] [CrossRef]
- Stone, B.; Dowling, S.; Cameron, A. Cognitive impairment and homelessness: A scoping review. Health Soc. Care Community 2019, 27, e125–e142. [Google Scholar] [CrossRef] [Green Version]
- Aas, I.M. Global Assessment of Functioning (GAF): Properties and frontier of current knowledge. Ann. Gen. Psychiatry 2010, 9, 20. [Google Scholar] [CrossRef]
- Jääskeläinen, E.; Juola, P.; Hirvonen, N.; McGrath, J.J.; Saha, S.; Isohanni, M.; Veijola, J.; Miettunen, J. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr. Bull. 2013, 39, 1296–1306. [Google Scholar] [CrossRef] [PubMed]
- DSM5. Available online: https://www.elsevier-masson.fr/dsm5 (accessed on 1 June 2015).
- Baron-Cohen, S.; Wheelwright, S.; Robinson, J.; Woodbury-Smith, M. The Adult Asperger Assessment (AAA): A Diagnostic Method. J. Autism Dev. Disord. 2005, 35, 807. [Google Scholar] [CrossRef] [PubMed]
- Lord, C.; Rutter, M.; Le Couteur, A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J. Autism Dev. Disord. 1994, 24, 659–685. [Google Scholar] [CrossRef] [PubMed]
- Lord, C.; Risi, S.; Lambrecht, L.; Cook, E.H.; Leventhal, B.L.; DiLavore, P.C.; Pickles, A.; Rutter, M. The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. J. Autism Dev. Disord. 2000, 30, 205–223. [Google Scholar] [CrossRef]
- Guy: ECDEU Assessment Manual for Psychopharmacology. Available online: https://scholar.google.com/scholar_lookup?title=ECDEU+Assessment+Manual+for+Psychopharmacology&publication_year=1976& (accessed on 1 June 2014).
- Thompson, K.; Kulkarni, J.; Sergejew, A.A. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr. Res. 2000, 42, 241–247. [Google Scholar] [CrossRef]
- Birchwood, M.; Smith, J.; Drury, V.; Healy, J.; Macmillan, F.; Slade, M. A self-report Insight Scale for psychosis: Reliability, validity and sensitivity to change. Acta Psychiatr. Scand. 1994, 89, 62–67. [Google Scholar] [CrossRef]
- Coppersmith, D.; Hong, S.J.; Hosking, J.R.M. Partitioning Nominal Attributes in Decision Trees. Data Min. Knowl. Discov. 1999, 3, 197–217. [Google Scholar] [CrossRef]
- Feelders, A. Handling Missing Data in Trees: Surrogate Splits or Statistical Imputation? In Principles of Data Mining and Knowledge Discovery; Żytkow, J.M., Rauch, J., Eds.; Springer: Berlin/Heidelberg, Germany, 1999; Volume 1704, pp. 329–334. [Google Scholar]
- Loh, W.Y.; Shih, Y.S. Split Selection Methods for Classification Trees. Stat. Sin. 1997, 7, 815–840. [Google Scholar]
- Loh, W.Y. Regression Trees with Unbiased Variable Selection and Interaction Detection. Stat. Sin. 2002, 12, 361–386. [Google Scholar]
- Popovic, D.; Nuss, P.; Vieta, E. Revisiting loxapine: A systematic review. Ann. Gen. Psychiatry 2015, 14, 15. [Google Scholar] [CrossRef]
- Horn, M.; Vaiva, G.; Dumais, A. Prise en charge médicamenteuse des agitations aux urgences: Recommandations théoriques et études des pratiques. La Presse Méd. 2015, 44, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Bourdinaud, V.; Pochard, F. Survey of management methods for patients in a state of agitation at admission and emergency departments in France. Encephale 2003, 29, 89–98. [Google Scholar] [PubMed]
- Siskind, D.; McCartney, L.; Goldschlager, R.; Kisely, S. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: Systematic review and meta-analysis. Br. J. Psychiatry 2016, 209, 385–392. [Google Scholar] [CrossRef] [PubMed]
- WAIS-IV. In Encyclopedia of Clinical Neuropsychology; Kreutzer, J.S.; DeLuca, J.; Caplan, B. (Eds.) Springer: Berlin/Heidelberg, Germany, 2011; p. 2667. [Google Scholar] [CrossRef]
- Delis, D.C.; Freeland, J.; Kramer, J.H.; Kaplan, E. Integrating clinical assessment with cognitive neuroscience: Construct validation of the California Verbal Learning Test. J. Consult. Clin. Psychol. 1988, 56, 123–130. [Google Scholar] [CrossRef]
- Adam, S.; Van der Linden, M.; Poitrenaud, J.; Kalafat, M. L’épreuve de rappel indicé à 48 items (RI-48). In L’évaluation des Troubles de la Mémoire: Présentation de Quatre Tests de Mémoire Épisodique (Avec Leur Étalonnage); Van der Linden, M., Adam, S., Agniel, A., Baisset Mouly, C., membres du GREMEM, Eds.; Solal: Marseille, France, 2004; pp. 49–67. [Google Scholar]
- Bates, M.E.; Lemay, E.P. The d2 Test of attention: Construct validity and extensions in scoring techniques. J. Int. Neuropsychol. Soc. 2004, 10, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Hugonot-Diener, L.; Thomas-Antérion, C.; Sellal, F. Gremoire 2: Tests et Échelles des Maladies Neurologiques avec Symptomatologie Cognitive; De Boeck Superieur: Louvain-la-Neuve, Belgium, 2015. [Google Scholar]
- Shallice, T.; Burgess, P.W. Deficits in Strategy Application Following Frontal Lobe Damage in Man. Brain 1991, 114, 727–741. [Google Scholar] [CrossRef]
- Dziobek, I.; Fleck, S.; Kalbe, E.; Rogers, K.; Hassenstab, J.; Brand, M.; Kessler, J.; Woike, J.K.; Wolf, O.T.; Convit, A. Introducing MASC: A Movie for the Assessment of Social Cognition. J. Autism Dev. Disord. 2006, 36, 623–636. [Google Scholar] [CrossRef]
- Combs, D.R.; Penn, D.L.; Wicher, M.; Waldheter, E. The Ambiguous Intentions Hostility Questionnaire (AIHQ): A new measure for evaluating hostile social-cognitive biases in paranoia. Cogn. Neuropsychiatry 2007, 12, 128–143. [Google Scholar] [CrossRef]
- Foster, A.; Gable, J.; Buckley, J. Homelessness in Schizophrenia. Psychiatr. Clin. N. Am. 2012, 35, 717–734. [Google Scholar] [CrossRef]
- Aubry, T.; Nelson, G.; Tsemberis, S. Housing First for People with Severe Mental Illness Who are Homeless: A Review of the Research and Findings from the at Home—Chez soi Demonstration Project. Can. J. Psychiatry 2015, 60, 467–474. [Google Scholar] [CrossRef] [Green Version]
- Iwundu, C.N.; Chen, T.A.; Edereka-Great, K.; Businelle, M.S.; Kendzor, D.E.; Reitzel, L.R. Mental Illness and Youth-Onset Homelessness: A Retrospective Study among Adults Experiencing Homelessness. Int. J. Environ. Res. Public Health 2020, 17, 8295. [Google Scholar] [CrossRef] [PubMed]
- Weir, E.; Allison, C.; Baron-Cohen, S. Autistic adults have poorer quality healthcare and worse health based on self-report data. Mol. Autism 2022, 13, 23. [Google Scholar] [CrossRef] [PubMed]
- Santos, C.; Olmedo, R.E.; Kim, J. Sedative-hypnotic drug withdrawal syndrome: Recognition and treatment [digest]. Emerg. Med. Pract. 2017, 19, S1–S2. [Google Scholar] [PubMed]
- Toto, S.; Grohmann, R.; Bleich, S.; Frieling, H.; Maier, H.B.; Greil, W.; Cordes, J.; Schmidt-Kraepelin, C.; Kasper, S.; Stübner, S.; et al. Psychopharmacological Treatment of Schizophrenia Over Time in 30 908 Inpatients: Data from the AMSP Study. Int. J. Neuropsychopharmacol. 2019, 22, 560–573. [Google Scholar] [CrossRef]
- Yang, S.Y.; Chen, L.Y.; Najoan, E.; Kallivayalil, R.A.; Viboonma, K.; Jamaluddin, R.; Javed, A.; Hoa, D.T.Q.; Iida, H.; Sim, K.; et al. Polypharmacy and psychotropic drug loading in patients with schizophrenia in Asian countries: Fourth survey of Research on Asian Prescription Patterns on antipsychotics. Psychiatry Clin. Neurosci. 2018, 72, 572–579. [Google Scholar] [CrossRef]
- Gallego, J.A.; Bonetti, J.; Zhang, J.; Kane, J.M.; Correll, C.U. Prevalence and correlates of antipsychotic polypharmacy: A systematic review and meta-regression of global and regional trends from the 1970s to 2009. Schizophr. Res. 2012, 138, 18–28. [Google Scholar] [CrossRef]
- Baandrup, L. Polypharmacy in schizophrenia. Basic Clin. Pharmacol. Toxicol. 2020, 126, 183–192. [Google Scholar] [CrossRef]
- Barbui, C.; Biancosino, B.; Esposito, E.; Marmai, L.; Donà, S.; Grassi, L. Factors associated with antipsychotic dosing in psychiatric inpatients: A prospective study. Int. Clin. Psychopharmacol. 2007, 22, 221–225. [Google Scholar] [CrossRef]
- Centorrino, F.; Goren, J.L.; Hennen, J.; Salvatore, P.; Kelleher, J.P.; Baldessarini, R.J. Multiple Versus Single Antipsychotic Agents for Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus Benefits. Am. J. Psychiatry 2004, 161, 700–706. [Google Scholar] [CrossRef]
- Kreyenbuhl, J.A.; Valenstein, M.; McCarthy, J.F.; Ganoczy, D.; Blow, F.C. Long-Term Antipsychotic Polypharmacy in the VA Health System: Patient Characteristics and Treatment Patterns. Psychiatr. Serv. 2007, 58, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Koh, K.A.; Montgomery, A.E.; O’Brien, R.W.; Kennedy, C.J.; Luedtke, A.; Sampson, N.A.; Sarah, M.; Gildea, S.M.; Hwang, I.; King, A.J.; et al. Predicting Homelessness among, U.S. Army Soldiers No Longer on Active Duty. Am. J. Prev. Med. 2022, 63, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Barone, C.; Yamamoto, A.; Richardson, C.G.; Zivanovic, R.; Lin, D.; Mathias, S. Examining patterns of cognitive impairment among homeless and precariously housed urban youth. J. Adolesc. 2019, 72, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Carroll, Á.; O’Brien, S.; Harrington, D.; Cheallaigh, C.N.; Lawlee, A.M.; Sukumar, P. The Unmet Rehabilitation Needs in an Inclusion Health Integrated Care Programme for Homeless Adults in Dublin, Ireland. Int. J. Env. Res. Public Health 2021, 18, 7917. [Google Scholar] [CrossRef] [PubMed]
| Psychiatric Diagnoses (DSM-5 Criteria) | N | % |
|---|---|---|
| Schizophrenia spectrum disorders | 1598 | 45.70% |
| Neurodevelopmental disorders | 443 | 12.67% |
| Bipolar disorders | 407 | 11.64% |
| Personality disorders | 372 | 10.64% |
| Depressive disorders | 230 | 6.58% |
| Anxiety disorders | 200 | 5.72% |
| Addiction disorders | 58 | 1.66% |
| Post-traumatic stress disorders | 54 | 1.54% |
| Other diagnostic categories | 135 | 3.86% |
| Factor | Homelessnes Prevalence (%) | Mean Prevalence (%) | Difference with Mean Prevalence (%) | p (chi2) | |
|---|---|---|---|---|---|
| Gender | Female | 7.41 | 9.51 | −2.1 | p < 0.01 |
| Male | 10.71 | 9.51 | 1.2 | p < 0.01 | |
| Matrimonial status | Single | 10.16 | 9.49 | 0.67 | p < 0.05 |
| Divorced | 10.73 | 9.49 | 1.24 | ||
| Married | 4.18 | 9.49 | −5.31 | p < 0.01 | |
| Common-law marriage | 7.48 | 9.49 | −2.01 | ||
| Employment | Job | 4.40 | 9.77 | −5.37 | p < 0.001 |
| No employ | 10.35 | 9.77 | 0.58 | p < 0.001 | |
| Criminal History | Without | 7.55 | 9.54 | −1.99 | p < 0.001 |
| With | 24.38 | 9.54 | 14.84 | p < 0.001 | |
| Suicidal attempt history | No | 8.33 | 9.58 | −1.25 | p < 0.001 |
| Yes | 12.59 | 9.58 | 3.01 | p < 0.001 | |
| Substance abuse | No | 5.64 | 9.58 | −3.94 | p < 0.001 |
| Tabaco | 9.15 | 9.58 | −0.43 | ||
| Tabaco, alcohol | 11.73 | 9.58 | 2.15 | ||
| Tabaco, alcohol, cannabis | 21.65 | 9.58 | 12.07 | p < 0.001 | |
| Tabaco, cannabis | 18.92 | 9.58 | 9.34 | p < 0.001 | |
| Alcohol | 7.44 | 9.58 | −2.14 | ||
| Others | 15.74 | 9.58 | 6.16 | p < 0.001 |
| TEST (Z scores) | MATRICES | SIMILITUDES | RLRI16 | CVLT | MEM | d-2R | ACSo | MASC | AIHQ |
|---|---|---|---|---|---|---|---|---|---|
| Diff. Mean Scores | 0.07 | 0.14 | 0.11 | 0.24 | 0.04 | 0.30 | −0.02 | 0.17 | −0.14 |
| Diff. Median Scores | 0 | 0.15 | 0.14 | 0.40 | −0.01 | 0.25 | 0 | 0.16 | −0.19 |
| Pval (T test) | 0.56 | 0.27 | 0.19 | 0.12 | 0.62 | 0.0011 | 0.85 | 0.15 | 0.38 |
| FWER corr. | NS | NS | NS | NS | NS | p < 0.05 | NS | NS | NS |
| Pval (Wilcoxon) | 0.45 | 0.23 | 0.06 | 0.11 | 0.55 | 0.0017 | 0.73 | 0.14 | 0.41 |
| FWER CORR. | NS | NS | NS | NS | NS | p < 0.05 | NS | NS | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lio, G.; Ghazzai, M.; Haesebaert, F.; Dubreucq, J.; Verdoux, H.; Quiles, C.; Jaafari, N.; Chéreau-Boudet, I.; Legros-Lafarge, E.; Guillard-Bouhet, N.; et al. Actionable Predictive Factors of Homelessness in a Psychiatric Population: Results from the REHABase Cohort Using a Machine Learning Approach. Int. J. Environ. Res. Public Health 2022, 19, 12268. https://doi.org/10.3390/ijerph191912268
Lio G, Ghazzai M, Haesebaert F, Dubreucq J, Verdoux H, Quiles C, Jaafari N, Chéreau-Boudet I, Legros-Lafarge E, Guillard-Bouhet N, et al. Actionable Predictive Factors of Homelessness in a Psychiatric Population: Results from the REHABase Cohort Using a Machine Learning Approach. International Journal of Environmental Research and Public Health. 2022; 19(19):12268. https://doi.org/10.3390/ijerph191912268
Chicago/Turabian StyleLio, Guillaume, Malek Ghazzai, Frédéric Haesebaert, Julien Dubreucq, Hélène Verdoux, Clélia Quiles, Nemat Jaafari, Isabelle Chéreau-Boudet, Emilie Legros-Lafarge, Nathalie Guillard-Bouhet, and et al. 2022. "Actionable Predictive Factors of Homelessness in a Psychiatric Population: Results from the REHABase Cohort Using a Machine Learning Approach" International Journal of Environmental Research and Public Health 19, no. 19: 12268. https://doi.org/10.3390/ijerph191912268
APA StyleLio, G., Ghazzai, M., Haesebaert, F., Dubreucq, J., Verdoux, H., Quiles, C., Jaafari, N., Chéreau-Boudet, I., Legros-Lafarge, E., Guillard-Bouhet, N., Massoubre, C., Gouache, B., Plasse, J., Barbalat, G., Franck, N., & Demily, C. (2022). Actionable Predictive Factors of Homelessness in a Psychiatric Population: Results from the REHABase Cohort Using a Machine Learning Approach. International Journal of Environmental Research and Public Health, 19(19), 12268. https://doi.org/10.3390/ijerph191912268







