Barriers to Community-Based Primary Health Care Delivery in Urban China: A Systematic Mapping Review
Abstract
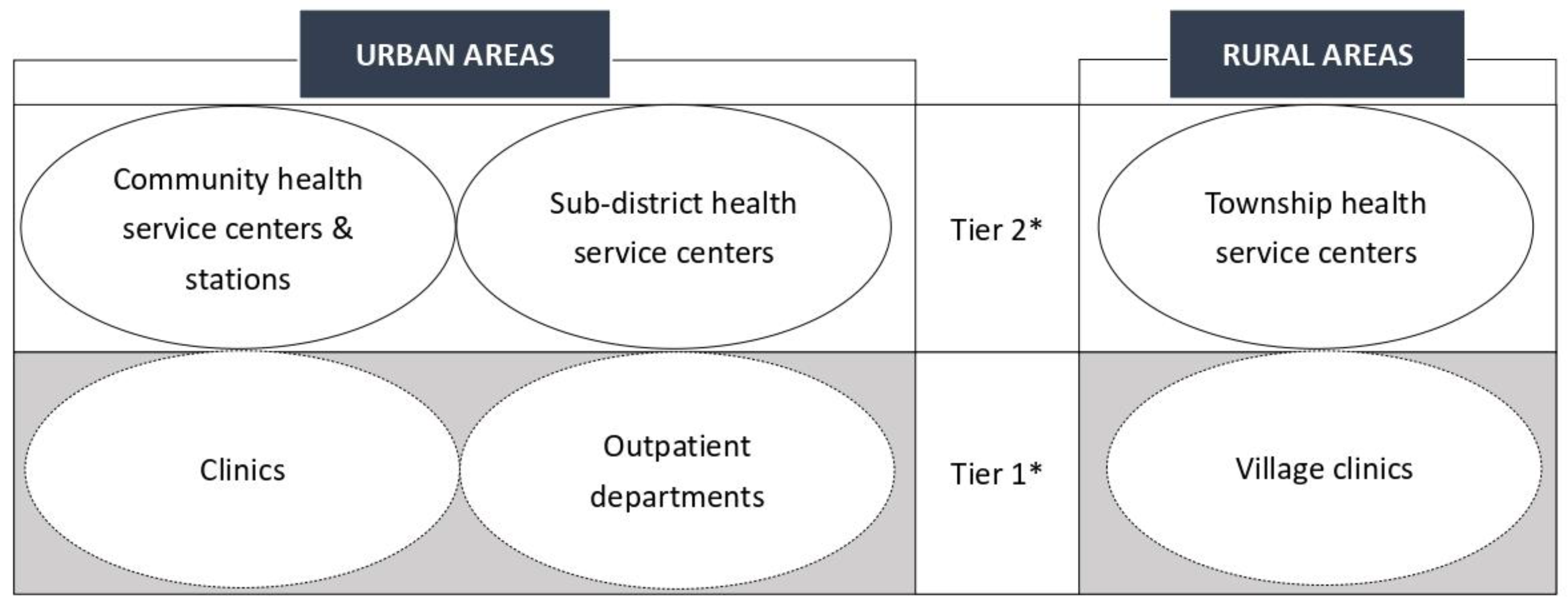
:1. Introduction
2. Materials and Methods
2.1. Framework of Searches and Syntheses
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Screening and Selection
2.5. Data Extraction and Syntheses
3. Results
3.1. Characteristics of the Included Studies
3.2. Access
3.2.1. Lack of Comprehensive Health Insurance Schemes
3.2.2. Lack of Public Awareness
3.3. People-Centered Care
3.3.1. Superficial Care Relationships
3.3.2. Gaps in Communication
3.4. Organization and Management
3.4.1. Staff Shortages and Poor Training
3.4.2. Second-Rate Equipment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Primary Health Care. Available online: https://www.who.int/health-topics/primary-health-care#tab=tab_1 (accessed on 1 January 2022).
- Sacks, E.; Schleiff, M.; Were, M.; Chowdhury, A.M.; Perry, H.B. Communities, universal health coverage and primary health care. Bull. World Health Organ. 2020, 98, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Bitton, A.; Fifield, J.; Ratcliffe, H.; Karlage, A.; Wang, H.; Veillard, J.H.; Schwarz, D.; Hirschhorn, L.R. Primary healthcare system performance in low-income and middle-income countries: A scoping review of the evidence from 2010 to 2017. BMJ Glob. Health 2019, 4, e001551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kruk, M.E.; Porignon, D.; Rockers, P.C.; Van Lerberghe, W. The contribution of primary care to health and health systems in low- and middle-income countries: A critical review of major primary care initiatives. Soc. Sci. Med. 2010, 70, 904–911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, K.; Li, Z.; Li, W.; Chen, L. China’s silk road and global health. Lancet 2017, 390, 2595–2601. [Google Scholar] [CrossRef]
- Li, B.; Chen, J. Equity in policy: An updated account of points systems for hukou conversion in Chinese megacities. J. Asian Public Policy 2022, 1–17. [Google Scholar] [CrossRef]
- National Bureau of Statistics. China Statistical Yearbook 2021. Available online: http://www.stats.gov.cn/tjsj/ndsj/2021/indexch.htm (accessed on 15 March 2022).
- Ramesh, M.; Wu, X.; He, A.J. Health governance and healthcare reforms in China. Health Policy Plan. 2014, 29, 663–672. [Google Scholar] [CrossRef] [Green Version]
- Bhattacharyya, O.; Delu, Y.; Wong, S.T.; Bowen, C. Evolution of primary care in China 1997–2009. Health Policy 2011, 100, 174–180. [Google Scholar] [CrossRef]
- Li, X.; Krumholz, H.M.; Yip, W.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Li, C.; Lu, J.; Su, M.; et al. Quality of primary health care in China: Challenges and recommendations. Lancet 2020, 395, 1802–1812. [Google Scholar] [CrossRef]
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 years of health-care reform in China: Progress and gaps in universal health coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]
- Li, L.; Fu, H. China’s health care system reform: Progress and prospects. Int. J. Health Plan. Manag. 2017, 32, 240–253. [Google Scholar] [CrossRef]
- Yao, J.; Wang, H.; Yin, J.; Shao, D.; Guo, X.; Sun, Q.; Yin, X. Factors associated with the utilization of community-based diabetes management care: A cross-sectional study in Shandong Province, China. BMC Health Serv. Res. 2020, 20, 407. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.H.; Wang, J.J.; Wong, S.; Wong, M.; Mercer, S.W.; Griffiths, S.M. The development of urban community health centres for strengthening primary care in China: A systematic literature review. Br. Med. Bull. 2015, 116, 139–153. [Google Scholar] [CrossRef] [Green Version]
- Huang, W.; Long, H.; Li, J.; Tao, S.; Zheng, P.; Tang, S.; Abdullah, A.S. Delivery of public health services by community health workers (CHWs) in primary health care settings in China: A systematic review (1996–2016). Glob. Health Res. Policy 2018, 3, 18. [Google Scholar] [CrossRef]
- Li, H.; Liu, K.; Gu, J.; Zhang, Y.; Qiao, Y.; Sun, X. The development and impact of primary health care in China from 1949 to 2015: A focused review. Int. J. Health Plan. Manag. 2017, 32, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lu, J.; Hu, S.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Xu, D.R.; Yip, W.; Zhang, H.; et al. The primary health-care system in China. Lancet 2017, 390, 2584–2594. [Google Scholar] [CrossRef]
- Booth, A. Formulating answerable questions. In Evidence Based Practice for Information Professionals: A Handbook; Booth, A., Brice, A., Eds.; Facet Publishing: London, UK, 2004; pp. 61–70. [Google Scholar]
- Briner, R.B.D.; Denyer, D. Systematic review and evidence synthesis as a practice and scholarship tool. In Handbook of Evidence-Based Management: Companies, Classrooms and Research; Rousseau, D.M., Ed.; Oxford University Press: Oxford, UK, 2012; pp. 112–129. [Google Scholar]
- James, K.L.; Randell, N.P.; Haddaway, N.R. A methodology for systematic mapping in environmental sciences. Environ. Evid. 2016, 5, 7. [Google Scholar] [CrossRef] [Green Version]
- Petersen, K.; Vakkalanka, S.; Kuzniarz, L. Guidelines for conducting systematic mapping studies in software engineering: An update. Inf. Softw. Technol. 2015, 64, 1–18. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A topology of reviews: An analysis of 14 review types and associated methodologies. Health Info. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Bitton, A.; Ratcliffe, H.L.; Veillard, J.H.; Kress, D.H.; Barkley, S.; Kimball, M.; Secci, F.; Wong, E.; Basu, L.; Taylor, C.; et al. Primary health care as a foundation for strengthening health systems in low-and middle-income countries. J. Gen. Intern. Med. 2017, 32, 566–571. [Google Scholar] [CrossRef] [Green Version]
- PHCPI. The PHCPI Conceptual Framework. Available online: https://improvingphc.org/phcpi-conceptual-framework (accessed on 7 May 2021).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CASP. CASP Qualitative Studies Checklist. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 7 December 2021).
- Hooper, P.; Jutai, J.W.; Strong, G.; Russell-Minda, E. Age-related macular degeneration and low-vision rehabilitation: A systematic review. Can. J. Ophthalmol. 2008, 43, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Saunders, L.D.; Soomro, G.M.; Buckingham, J.; Jamtvedt, G.; Raina, P. Assessing the methodological quality of nonrandomized intervention studies. West. J. Nurs. Res. 2003, 25, 223–237. [Google Scholar] [CrossRef]
- Jäkel, A.; von Hauenschild, P. Therapeutic effects of cranial osteopathic manipulative medicine: A systematic review. J. Osteopath. Med. 2011, 111, 685–693. [Google Scholar] [CrossRef]
- Nadelson, S.; Nadelson, L.S. Evidence-based practice article reviews using CASP tools: A method for teaching EBP. Worldviews Evid. Based Nurs. 2014, 11, 344–346. [Google Scholar] [CrossRef]
- Singh, J. Critical appraisal skills programme. J. Pharmacol. Pharmacother. 2013, 4, 76. [Google Scholar] [CrossRef] [Green Version]
- Gibbs, G.R. Analyzing Qualitative Data, 2nd ed.; Sage: London, UK, 2007; pp. 53–74. [Google Scholar]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Gan, Y.; Li, W.; Cao, S.; Dong, X.; Li, L.; Mkandawire, N.; Chen, Y.; Herath, C.; Song, X.; Yin, X.; et al. Patients’ willingness on community health centers as gatekeepers and associated factors in Shenzhen, China: A cross-sectional study. Medicine 2016, 95, e3261. [Google Scholar] [CrossRef]
- Li, H.; Zhu, W.; Xia, H.; Wang, X.; Mao, C. Cross-sectional study on the management and control of hypertension among migrants in primary care: What is the impact of segmented health insurance schemes? J. Am. Heart Assoc. 2019, 8, e012674. [Google Scholar] [CrossRef]
- Chung, V.C.; Wong, S.Y.; Wang, H.H.; Wong, M.C.; Wei, X.; Wang, J.; Liu, S.; Ho, R.S.; Ellen, L.M.; Griffiths, S.M. Use of traditional and complementary medicine as self-care strategies in community health centers: Cross-sectional study in urban Pearl River Delta Region of China. Medicine 2016, 95, e3761. [Google Scholar] [CrossRef]
- Yin, T.; Yin, D.L.; Xiao, F.; Xin, Q.Q.; Li, R.L.; Zheng, X.G.; Yang, H.M.; Wang, L.H.; Ding, X.Y.; Chen, B.W. Socioeconomic status moderates the association between patient satisfaction with community health service and self-management behaviors in patients with type 2 diabetes: A cross-sectional survey in China. Medicine 2019, 98, e15849. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Lee, D.C.; Liang, H.; Zhang, L.; Makinen, M.; Blanchet, N.; Kidane, R.; Lindelow, M.; Wang, H.; Wu, S. Community health centers and primary care access and quality for chronically-ill patients–a case-comparison study of urban Guangdong Province, China. Int. J. Equity Health 2015, 14, 90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, Z.; Liao, Y.; Chen, C.C.; Hao, Y.; Hu, R. Usual source of care and the quality of primary care: A survey of patients in Guangdong province, China. Int. J. Equity Health 2015, 14, 60. [Google Scholar] [CrossRef] [Green Version]
- Yue, P.; Xu, T.; Greene, B.; Wang, Y.; Wang, R.; Dai, G.; Xu, L. Caring in community nursing practice: Inductive content analysis reveals an inter-dynamic system between patients and nurses. J. Clin. Nurs. 2020, 29, 3025–3041. [Google Scholar] [CrossRef]
- Zhang, T.; Ren, J.; Zhang, X.; Max, W. Medical and socio-demographic characteristics associated with patient-perceived continuity of primary care: A cross-sectional survey in Hangzhou, China. Int. J. Health Plan. Manag. 2020, 35, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Kuang, L.; Liang, Y.; Mei, J.; Zhao, J.; Wang, Y.; Liang, H.; Shi, L. Family practice and the quality of primary care: A study of Chinese patients in Guangdong Province. Fam. Pract. 2015, 32, 557–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, W.; Huang, Y.; Zhou, H.; Lin, G.; Lu, M.; Xi, X. Associations between social capital and trust in general practitioners among the elderly people: Empirical evidence from China. Health Soc. Care Community 2020, 28, 1590–1602. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Zhang, T.; Wang, L.; Huang, J.; Liang, H.; Chen, G.; Liu, C.; Zhang, Y. The developing family doctor system: Evidence from the progress of the family doctor signing service from a longitudinal survey (2013–2016) in Pudong New Area, Shanghai. BMC Fam. Pract. 2021, 22, 11. [Google Scholar] [CrossRef]
- Li, H.; Sun, Y.; Qian, D. Can integrated health services delivery have an impact on hypertension management? A cross-sectional study in two cities of China. Int. J. Equity Health 2016, 15, 193. [Google Scholar] [CrossRef] [Green Version]
- Gu, T.; Yuan, J.; Li, L.; Shao, Q.; Zheng, C. Demand for community-based care services and its influencing factors among the elderly in affordable housing communities: A case study in Nanjing City. BMC Health Serv. Res. 2020, 20, 241. [Google Scholar] [CrossRef]
- Li, H.; Wei, X.; Wong, M.C.S.; Wong, S.Y.S.; Yang, N.; Griffiths, S.M. A cross-sectional comparison of perceived quality of primary care by hypertensive patients in Shanghai and Shenzhen, China. Medicine 2015, 94, e1388. [Google Scholar] [CrossRef]
- Wang, H.H.; Wang, J.J.; Wong, S.; Wong, M.; Li, F.J.; Wang, P.X.; Zhou, Z.H.; Zhu, C.Y.; Griffiths, S.M.; Mercer, S.W. Epidemiology of multimorbidity in China and implications for the healthcare system: Cross-sectional survey among 162,464 community household residents in southern China. BMC Med. 2014, 12, 188. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Wang, L.; Liu, S.; Zhang, T.; Liu, C.; Zhang, Y. The path analysis of family doctor’s gatekeeper role in Shanghai, China: A structural equation modeling (SEM) approach. Inquiry-J. Health Care Organ. Proviw. Financ. 2021, 58, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Searle, K.; Blashki, G.; Kakuma, R.; Yang, H.; Zhao, Y.; Minas, H. Current needs for the improved management of depressive disorder in community healthcare centres, Shenzhen, China: A view from primary care medical leaders. Int. J. Ment. Health Syst. 2019, 13, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, Y.; Zhao, X.; Liu, Y.; Wei, Y.; Jin, G.; Shao, S.; Lu, X. Perceptions, behaviours, barriers and needs of evidence-based medicine in primary care in Beijing: A qualitative study. BMC Fam. Pract. 2019, 20, 171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, T.; Liu, C.; Ren, J.; Wang, S.; Huang, X.; Guo, Q. Perceived impacts of the national essential medicines system: A cross-sectional survey of health workers in urban community health services in China. BMJ Open 2017, 7, e014621. [Google Scholar] [CrossRef] [Green Version]
- Xia, Z.; Gao, W.; Wei, X.; Peng, Y.; Ran, H.; Wu, H.; Liu, C. Perceived value of electronic medical records in community health services: A national cross-sectional survey of primary care workers in mainland China. Int. J. of Environ. Res. Public Health 2020, 17, 8510. [Google Scholar] [CrossRef]
- Wu, D.; Lam, T.P.; Lam, K.F.; Zhou, X.D.; Sun, K.S. Health reforms in China: The public’s choices for first-contact care in urban areas. Fam. Pract. 2017, 34, 194–200. [Google Scholar] [CrossRef] [Green Version]
- Edward, A.; Osei-Bonsu, K.; Branchini, C.; Arwal, S.H.; Naeem, A.J. Enhancing governance and health system accountability for people centered healthcare: An exploratory study of community scorecards in Afghanistan. BMC Health Serv. Res. 2015, 15, 299. [Google Scholar] [CrossRef]



| Key PHC Service Domains | CB-PHC Organizations | Non-CB-PHC Organizations | ||
|---|---|---|---|---|
| Community Health Service Centers and Stations | Sub-District Health Service Centers | Clinics | Outpatient Departments | |
| Prevention | √ | √ | X | √ |
| Treatment | √ | √ | √ | √ |
| Rehabilitation | √ | √ | X | √ |
| Palliative care | √ | X | X | X |
| Health education | √ | √ | X | X |
| Study | Methods | Sample | Sample Size | Research Sites |
|---|---|---|---|---|
| Theme one: Access | ||||
| Yin et al. (2019) | Cross-sectional | Patients (diabetes) | 1691 | Multi-provinces |
| Sun et al. (2019) | Cross-sectional | Residents (aged ≥18) | 915 | Sichuan |
| Li … & Mao. (2019) | Cross-sectional | Migrants (hypertension, aged >18) | 1046 | Shenzhen |
| Li … & Hu. (2019) | Cross-sectional | Patients (hypertension, aged ≥18) | 867 | Shenzhen |
| Zhong et al. (2018) | Cross-sectional | Patients (aged ≥18) | 1461 | Guangdong |
| Liu, D. et al. (2017) | Cross-sectional | Residents (aged ≥18) | 2247 | Chengdu |
| Li, W. et al. (2017) | Cross-sectional | Patients (aged ≥18) | 6887 | Shenzhen |
| Gan et al. (2016) | Cross-sectional | Patients (aged 18-90) | 7761 | Shenzhen |
| Chung et al. (2016) | Cross-sectional | Patients (aged ≥18) | 3360 | Guangdong * |
| Zeng et al. (2015) | Cross-sectional | Migrants (aged ≥18) | 736 | Guangzhou |
| Shi et al. (2015) | Cross-sectional | Patients (hypertension, diabetes, aged ≥50) | 560 | Guangdong |
| Chung et al. (2013) | Cross-sectional | Patients (aged ≥18) | 3356 | Guangdong * |
| Theme two: People-centered care | ||||
| Zhang, W. et al. (2020) | Cross-sectional | Residents (aged ≥60) | 2754 | Nationwide |
| Zhang, T. et al. (2020) | Cross-sectional | Patients (aged ≥18) | 624 | Hangzhou |
| Zhang, L. et al. (2020) | Cross-sectional | Patients (aged ≥18) | 515 | Changchun |
| Yue et al. (2020) | Interview | Patients (chronic disease) & nurses | 26 | Beijing |
| Gu et al. (2020) | Cross-sectional | Residents (aged ≥60) | 480 | Nanjing |
| Pu et al. (2019) | Cross-sectional | Patients (PTB, aged ≥15) | 638 | Guizhou |
| Huang et al. (2019) | Cross-sectional | Residents (aged ≥15) | 2919 | Shanghai |
| Su et al. (2017) | Cross-sectional | Residents (hypertension) | 1,092,031 | Nationwide |
| Qian et al. (2017) | Interview | Medical staff & patients | 50 | Hangzhou |
| Liu, C. et al. (2017) | Cross-sectional | Patients (aged ≥18) | 700 | Beijing |
| Li, H. et al. (2017) | Longitudinal | Patients (hypertension, aged ≥60) | 880 | Shanghai |
| Li, H. et al. (2016) | Cross-sectional | Patients (hypertension, aged 18-80) | 782 | Wuhan, Nanjing |
| Gu et al. (2016) | Cohort | Patients (heart disease, aged ≥55) | 329 | Beijing |
| Zhong et al. (2015) | Cross-sectional | Community inhabitants | 9067 | Anhui |
| Li … Yang et al. (2015) | Cross-sectional | Patients (hypertension, aged ≥18) | 696 | Shanghai, Shenzhen |
| Li … Lao et al. (2015) | Cohort | Patients (hypertension, aged ≥18) | 3196 | Shanghai, Shenzhen |
| Kuang et al. (2015) | Cross-sectional | Patients (aged ≥18) | 1645 | Guangdong |
| Du et al. (2015) | Cross-sectional | Patients | 864 | Guangdong |
| Yang et al. (2014) | Cross-sectional | Residents (NCD, aged ≥18) | 51,501 | Guangdong |
| Wang et al. (2014) | Cross-sectional | Residents | 162,464 | Guangdong |
| McCollum et al. (2014) | Cross-sectional & interview | Patients (aged ≥18) & health directors | 231 + 8 | Fuzhou |
| Chen et al. (2014) | Cross-sectional | Patients (hypertension, aged ≥35) | 3191 | Chengdu |
| Wang et al. (2013) | Cross-sectional | Patients (aged ≥18) | 1440 | Guangdong * |
| Shao et al. (2013) | Cross-sectional | Residents (aged ≥15) | 6592 | Beijing |
| Theme three: Organization and management | ||||
| Liu et al. (2021) | Longitudinal | Doctors | 8968 | Shanghai |
| Huang et al. (2021) | Longitudinal | Residents (aged ≥18) | 4749 | Shanghai |
| Zhang et al. (2020) | Cross-sectional & interview | Residents & health workers | 989 + 32 | Guizhou, Chongqing |
| Yao et al. (2020) | Cross-sectional | Patients (diabetes) & care providers | 2610 | Shandong |
| Xia et al. (2020) | Cross-sectional | Physicians & nurses | 2719 | Nationwide |
| Duan et al. (2020) | Cross-sectional | Patients (diabetes, aged ≥18) | 1972 | Yueqing |
| Zhu et al. (2019) | Cross-sectional | Patients (diabetes, common illness, aged ≥18) | 816 | Hangzhou |
| Zhao et al. (2019) | Interview | General practitioners | 32 | Beijing |
| Zhan et al. (2019) | Cross-sectional | Outpatient prescribers | 150 | Sichuan |
| Wang et al. (2019) | Cross-sectional | Patients (diabetes, aged ≥18) | 1598 | Shandong, Jiangsu |
| Searle et al. (2019) | Interview | Medical leaders | 17 | Shenzhen |
| Liang et al. (2019) | Cross-sectional & interview | Health workers & leaders | 198 + 70 | Guizhou, Chongqing |
| Huang et al. (2019) | Longitudinal | Patients (NCD, aged ≥18) | 4749 | Shanghai |
| Chen et al. (2019) | Cross-sectional | General practitioners & nurses | 172 | Shanghai |
| Zhu et al. (2018) | Interview | Managers & physicians | 15 | Wuhan |
| Mao et al. (2018) | Interview | Childcare providers | 22 | Hunan |
| Li, W. et al. (2018) | Cross-sectional | Patients (aged ≥18) | 1159 | Wuhan |
| Li, L. et al. (2018) | Cross-sectional | Patients (aged 18-89) | 698 | Guangzhou |
| Zhang et al. (2017) | Cross-sectional | Primary care workers | 791 | Multi-provinces |
| Wu et al. (2017) | Cross-sectional & interview | Residents | 1248 + 19 | Hangzhou |
| Wong et al. (2017) | Cross-sectional | Clinicians & primary care practitioners | 3738 | Nationwide |
| Wei et al. (2017) | Cross-sectional | Primary care users | 2924 | Multi-cities |
| Ong et al. (2017) | Cross-sectional | Primary care practitioners | 3580 | Nationwide |
| Wu et al. (2016) | Cross-sectional | Patients (aged ≥18) | 3848 | Shenzhen |
| Li, J. et al. (2016) | Cross-sectional | Patients (aged ≥15) | 1918 | Jilin |
| Chapman et al. (2016) | Interview | Doctors | 23 | Shenzhen |
| Wei et al. (2015) | Interview | Managerial & professional staff | 60 | Guangdong * |
| Jing et al. (2015) | Longitudinal | Residents (aged ≥18) | 1200 | Shanghai |
| Wang et al. (2014) | Interview | Primary family caregivers | 23 | Not specific |
| Li et al. (2014) | Cross-sectional | Patients (aged ≥18) | 787 | Shenzhen |
| Wong et al. (2012) | Cross-sectional | Patients (hypertension) | 1830 | Guangdong * |
| Barriers to CB-PHC Delivery | Impacts of the Barrier on Community-Based Health Care |
|---|---|
| PHCPI subdomain: Access | |
| Lack of comprehensive health insurance schemes |
|
| |
| |
| |
| |
| |
| Lack of public awareness |
|
| |
| |
| PHCPI subdomain: People-centered care | |
| Superficial care relationships |
|
| |
| |
| |
| |
| |
| |
| |
| |
| Gaps in communication |
|
| |
| |
| |
| |
| |
| |
| PHCPI subdomain: Organization and management | |
| Staff shortages and poor training |
|
| |
| |
| |
| |
| |
| |
| |
| |
| |
| Second-rate equipment |
|
| |
| |
| |
| |
| |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, B.; Chen, J. Barriers to Community-Based Primary Health Care Delivery in Urban China: A Systematic Mapping Review. Int. J. Environ. Res. Public Health 2022, 19, 12701. https://doi.org/10.3390/ijerph191912701
Li B, Chen J. Barriers to Community-Based Primary Health Care Delivery in Urban China: A Systematic Mapping Review. International Journal of Environmental Research and Public Health. 2022; 19(19):12701. https://doi.org/10.3390/ijerph191912701
Chicago/Turabian StyleLi, Bo, and Juan Chen. 2022. "Barriers to Community-Based Primary Health Care Delivery in Urban China: A Systematic Mapping Review" International Journal of Environmental Research and Public Health 19, no. 19: 12701. https://doi.org/10.3390/ijerph191912701
APA StyleLi, B., & Chen, J. (2022). Barriers to Community-Based Primary Health Care Delivery in Urban China: A Systematic Mapping Review. International Journal of Environmental Research and Public Health, 19(19), 12701. https://doi.org/10.3390/ijerph191912701





