Silver Diamine Fluoride (SDF) Efficacy in Arresting Cavitated Caries Lesions in Primary Molars: A Systematic Review and Metanalysis
Abstract
1. Introduction
2. Materials and Methods
- Population: children with active dentin cavitated lesions in primary molars;
- Intervention: silver diamine fluoride;
- Comparison: no treatment or any other type of non-invasive or minimally-invasive treatment;
- Outcome: caries arrest rate in different timeframes (primary outcome); patient’s discomfort during the treatment procedure (secondary outcome).
2.1. Eligibility Criteria
- Type of study: randomized (RCT) and non-randomized clinical studies (NRSI);
- Publication languages: papers published in English, Italian and French;
- Time of publication: no time restriction applied, last accessed on 10 January 2022;
- Type of intervention applied: SDF applied in active dentin cavitated lesions in primary molars (first and second molars);
- Follow up: longer than 6 months;
- Primary outcome: caries arrest rate, mean number of inactivated lesions, odds ratios;
- Secondary outcome: patient’s discomfort during the treatment procedure.
2.2. Information Sources and Search Strategy
- For PubMed, the string used was: (“dental caries” [MeSH Terms] OR “dentin caries” [Title/Abstract] OR “dental cavity” [Title/Abstract] OR “caries arrest rate” [Title/Abstract] OR “caries activity” [Title/Abstract] OR “caries progression” [Title/Abstract] OR “tooth, deciduous” [MeSH Terms] OR “carious lesion*” [Title/Abstract] OR “caries lesion*” [Title/Abstract] OR “deciduous dentition” [Title/Abstract] OR “primary dentition” [Title/Abstract] OR “primary teeth” [Title/Abstract] OR “primary tooth” [Title/Abstract]) AND (“silver fluoride”[Supplementary concept] OR “silver diamine fluoride”[Supplementary concept] OR SDF[Title/Abstract] OR “silver fluoride”[Title/Abstract] OR “diamine fluoride*”[Title/Abstract] OR “diammine”[Title/Abstract] OR “silver nitrate solutions”[Title/Abstract]).
- For Embase: (‘dental caries’/exp OR ‘dental caries’ OR ‘dentin’/exp OR ‘dentin’ OR ‘dental cavities’/exp OR ‘dental cavities’ OR ‘caries progression’ OR ‘caries arrest’ OR ‘deciduous tooth’/exp OR ‘deciduous tooth’ OR ‘primary dentition’/exp OR ‘primary dentition’) AND (‘silver fluoride’ OR ‘silver diamine fluoride’ OR ‘silver diammine’ OR ‘silver nitrate’) AND ‘article’/it AND ‘human’/de NOT ‘in vitro study’/de AND [child]/lim.
- For Scopus: (TITLE-ABS-KEY (dental AND caries) OR TITLE-ABS (dentin AND caries) OR TITLE-ABS (dental AND cavity) OR TITLE-ABS (caries AND arrest) OR TITLE-ABS (caries AND progression) OR TITLE-ABS (caries AND activity) OR TITLE-ABS-KEY (deciduous) OR TITLE-ABS-KEY (carious AND lesion) OR TITLE-ABS-KEY (caries) OR TITLE-ABS-KEY (primary AND dentition) OR TITLE-ABS-KEY (primary AND teeth) OR TITLE-ABS-KEY (primary AND tooth)) AND (TITLE-ABS-KEY (silver AND fluoride) OR TITLE-ABS-KEY (sdf) OR TITLE-ABS-KEY (silver AND diamine AND fluoride) OR TITLE-ABS-KEY (silver AND fluoride) OR TITLE-ABS-KEY (diamine AND fluoride) OR TITLE-ABS-KEY (diammine) OR TITLE-ABS (silver AND nitrate AND solution)) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (SUBJAREA, “DENT”)).
2.3. Study Selection
2.4. Data Collection
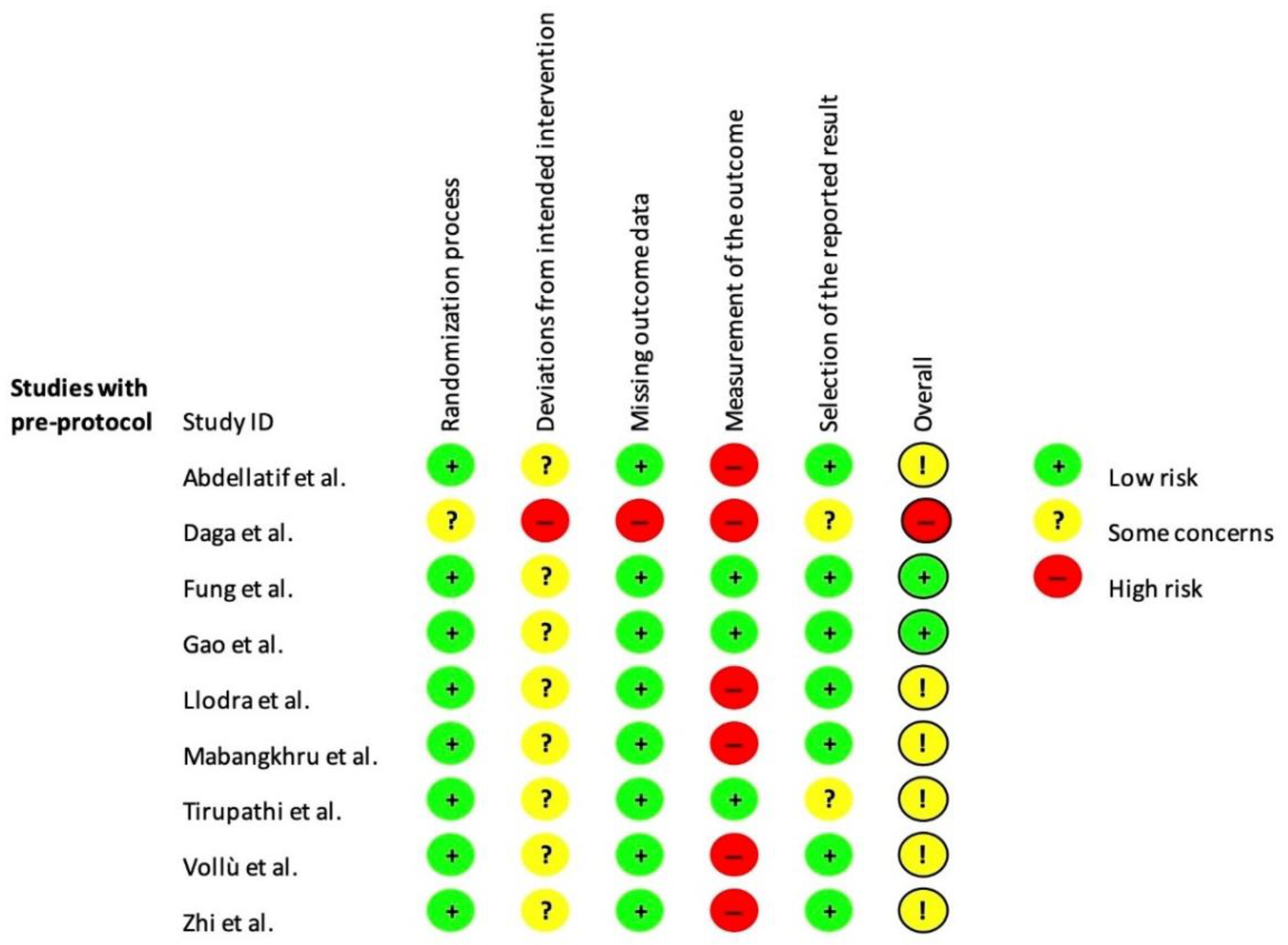
2.5. Risk of Bias
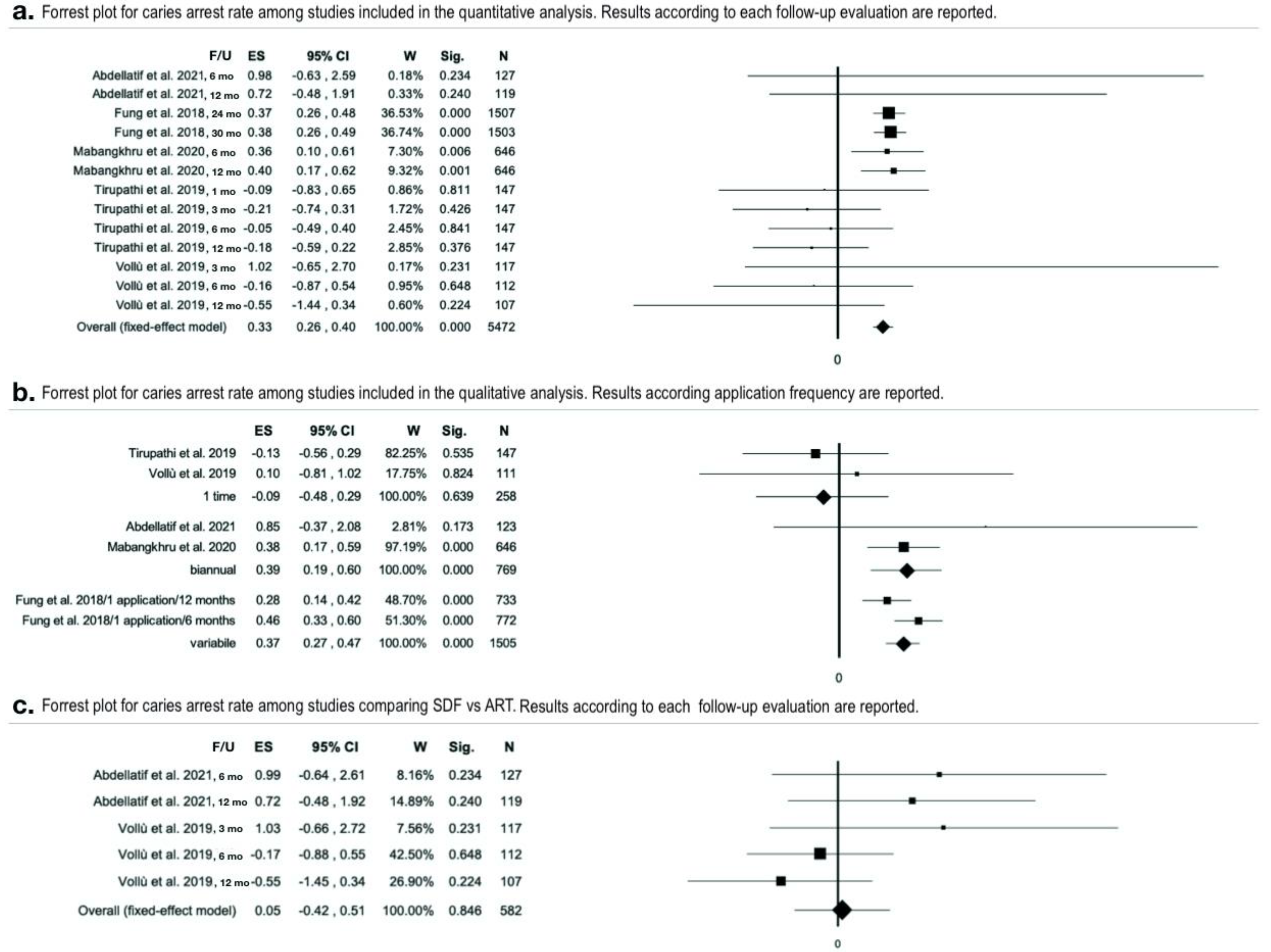
2.6. Statistical Analysis
3. Results
3.1. Study Selection
3.2. Subjects Involved
3.3. Study Characteristics
3.4. SDF Application Protocol
3.5. Risk of Bias Assessment
3.6. Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peres, M.A.; Macpherson, L.M.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Uribe, S.E.; Innes, N.; Maldupa, I. The global prevalence of early childhood caries: A systematic review with meta-analysis using the WHO diagnostic criteria. Int. J. Paediatr. Dent. 2021, 31, 817–830. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation. Global Health Data Exchange. (n.d.). Available online: https://www.healthdata.org (accessed on 12 September 2022).
- Tickotsky, N.; Petel, R.; Araki, R.; Moskovitz, M. Caries Progression Rate in Primary Teeth: A Retrospective Study. J. Clin. Pediatr. Dent. 2017, 41, 358–361. [Google Scholar] [CrossRef] [PubMed]
- Dawson, A.S.; Makinson, O.F. Dental treatment and dental health. Part 1. A review of studies in support of a philosophy of Minimum Intervention Dentistry. Aust. Dent. J. 1992, 37, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Tedesco, T.; Calvo, A.F.B.; Lenzi, T.L.; Hesse, D.; Guglielmi, C.A.B.; Camargo, L.B.; Gimenez, T.; Braga, M.M.; Raggio, D.P. ART is an alternative for restoring occlusoproximal cavities in primary teeth—Evidence from an updated systematic review and meta-analysis. Int. J. Paediatr. Dent. 2016, 27, 201–209. [Google Scholar] [CrossRef]
- Arrow, P.; Forrest, H.; Piggott, S. Minimally Invasive Dentistry: Parent/Carer Perspectives on Atraumatic Restorative Treatments and Dental General Anaesthesia to the Management of Early Childhood Caries. Front. Oral Health 2021, 2, 656530. [Google Scholar] [CrossRef]
- Cagetti, M.G.; Angelino, E. Could SARS-CoV-2 burst the use of Non-Invasive and Minimally Invasive treatments in paediatric dentistry? Int. J. Paediatr. Dent. 2020, 31, 27–30. [Google Scholar] [CrossRef]
- Ricketts, D.; Lamont, T.; Innes, N.P.; Kidd, E.; Clarkson, J.E. Operative caries management in adults and children. Cochrane Database Syst. Rev. 2019, 7, CD003808. [Google Scholar] [CrossRef]
- Schwendicke, F.; Frencken, J.; Bjørndal, L.; Maltz, M.; Manton, D.J.; Ricketts, D.; Van Landuyt, K.; Banerjee, A.; Campus, G.; Doméjean, S.; et al. Managing Carious Lesions: Consensus Recommendations on Carious Tissue Removal. Adv. Dent. Res. 2016, 28, 58–67. [Google Scholar] [CrossRef]
- Marinho, V. Evidence-based Effectiveness of Topical Fluorides. Adv. Dent. Res. 2008, 20, 3–7. [Google Scholar] [CrossRef]
- Corrêa-Faria, P.; Viana, K.A.; Raggio, D.P.; Hosey, M.T.; Costa, L.R. Recommended procedures for the management of early childhood caries lesions—A scoping review by the Children Experiencing Dental Anxiety: Collaboration on Research and Education (CEDACORE). BMC Oral Health 2020, 20, 75. [Google Scholar] [CrossRef] [PubMed]
- Urquhart, O.; Tampi, M.P.; Pilcher, L.; Slayton, R.L.; Araujo, M.; Fontana, M.; Guzmán-Armstrong, S.; Nascimento, M.M.; Nový, B.; Tinanoff, N.; et al. Nonrestorative Treatments for Caries: Systematic Review and Network Meta-analysis. J. Dent. Res. 2019, 98, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Richards, D. The effectiveness of silver diamine fluoride in arresting caries. Evidence-Based Dent. 2017, 18, 70. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.H.; Mei, L.; Seneviratne, C.J.; Lo, E.C.M. Effects of silver diamine fluoride on dentine carious lesions induced by Streptococcus mutans and Actinomyces naeslundii biofilms. Int. J. Paediatr. Dent. 2011, 22, 2–10. [Google Scholar] [CrossRef]
- Nishino, M.; Yoshida, S.; Sobue, S.; Kato, J.; Nishida, M. Effect of topically applied ammoniacal silver fluoride on dental caries in children. J. Osaka Univ. Dent. Sch. 1969, 9, 149–155. [Google Scholar]
- Lo, E.; Chu, C.; Lin, H. A community-based caries control program for pre-school children using topical fluorides: 18-month results. J. Dent. Res. 2001, 80, 2071–2074. [Google Scholar] [CrossRef]
- Bijella, M.F.T.B.; Bijella, V.T.; Silva, M.S.M.B.; Lopes, E.S. Avaliação clínica da aplicação de diamino-fluoreto de prata a 12% (Bioride) na dentição decídua e seu efeito na incidência de cárie em primeiros molares permanentes. Rev. Paul Odontol. 1991, 13, 28–35. [Google Scholar]
- Mauro, S.; García Robles, E.; Cinque, C.; Squassi, A.F.; Bordoni, N.E. Eficiencia de tres fluoruros concentrados para la estabilización de caries de esmalte. Bol. Asoc. Argent Odontol. Ninos. 2004, 33, 4–11. [Google Scholar]
- Mei, M.L.; Lo, E.C.M.; Chu, C.H. Clinical Use of Silver Diamine Fluoride in Dental Treatment. Compend. Contin. Educ. Dent. 2016, 37, 93–98. [Google Scholar]
- Horst, J.A.; Ellenikiotis, H.; UCSF Silver Caries Arrest Committee. USCF Protocol for Silver Diamine Fluoride: Rationale, Indications, and Consent. J. Calif. Dent. Assoc. 2016, 44, 16–28. [Google Scholar]
- Oliveira, B.H.; Rajendra, A.; Veitz-Keenan, A.; Niederman, R. The Effect of Silver Diamine Fluoride in Preventing Caries in the Primary Dentition: A Systematic Review and Meta-Analysis. Caries Res. 2018, 53, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Contreras, V.; Toro, M.J.; Elías-Boneta, A.R.; Encarnación-Burgos, M.A. Effectiveness of silver diamine fluoride in caries prevention and arrest: A systematic literature review. Gen. Dent. 2017, 65, 22–29. [Google Scholar] [PubMed]
- Chibinski, A.C.; Wambier, L.M.; Feltrin, J.; Loguercio, A.D.; Wambier, D.S.; Reis, A. Silver Diamine Fluoride Has Efficacy in Controlling Caries Progression in Primary Teeth: A Systematic Review and Meta-Analysis. Caries Res. 2017, 51, 527–541. [Google Scholar] [CrossRef] [PubMed]
- Trieu, A.; Mohamed, A.; Lynch, E. Silver diamine fluoride versus sodium fluoride for arresting dentine caries in children: A systematic review and meta-analysis. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Jabin, Z.; Vishnupriya, V.; Agarwal, N.; Nasim, I.; Sharma, A. Effect of 38% silver diamine fluoride on control of dental caries in primary dentition: A Systematic review. J. Fam. Med. Prim. Care 2020, 9, 1302–1307. [Google Scholar] [CrossRef]
- Duangthip, D.; Jiang, M.; Chu, C.H.; Lo, E.C.M. Non-surgical treatment of dentin caries in preschool children--systematic review. BMC Oral Health 2015, 15, 44. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLOS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Richardson, W.S.; Wilson, M.C.; Nishikawa, J.; Hayward, R.S. The well-built clinical question: A key to evidence-based decisions. ACP J. Club 1995, 123, A12–A13. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Higgins, J.P.T. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Fixed-Effect Model; John Wiley & Sons: Chichester, UK, 2009; Chapter 3; pp. 63–67. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Abdellatif, H.M.; Ali, A.M.; Baghdady, S.I.; ElKateb, M.A. Caries arrest effectiveness of silver diamine fluoride compared to alternative restorative technique: Randomized clinical trial. Eur. Arch. Paediatr. Dent. 2021, 22, 575–585. [Google Scholar] [CrossRef] [PubMed]
- Silver Diamine Fluoride in Arresting Dentinal Caries in School Children. Indian J. Public Health Res. Dev. 2020, 11, 530–535. [CrossRef]
- Fung, M.; Duangthip, D.; Wong, M.; Lo, E.; Chu, C. Randomized Clinical Trial of 12% and 38% Silver Diamine Fluoride Treatment. J. Dent. Res. 2017, 97, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Llodra, J.; Rodriguez, A.; Ferrer, B.; Menardia, V.; Ramos, T.; Morato, M. Efficacy of Silver Diamine Fluoride for Caries Reduction in Primary Teeth and First Permanent Molars of Schoolchildren: 36-month Clinical Trial. J. Dent. Res. 2005, 84, 721–724. [Google Scholar] [CrossRef]
- Mabangkhru, S.; Duangthip, D.; Chu, C.H.; Phonghanyudh, A.; Jirarattanasopha, V. A randomized clinical trial to arrest dentin caries in young children using silver diamine fluoride. J. Dent. 2020, 99, 103375. [Google Scholar] [CrossRef]
- Tirupathi, S.P.; Svsg, N.; Rajasekhar, S.; Nuvvula, S. Comparative cariostatic efficacy of a novel Nano-silver fluoride varnish with 38% silver diamine fluoride varnish a double-blind randomized clinical trial. J. Clin. Exp. Dent. 2019, 11, e105–e112. [Google Scholar] [CrossRef]
- Vollú, A.L.; Rodrigues, G.F.; Teixeira, R.V.R.; Cruz, L.R.; Massa, G.D.S.; Moreira, J.P.D.L.; Luiz, R.R.; Barja-Fidalgo, F.; Fonseca-Gonçalves, A. Efficacy of 30% silver diamine fluoride compared to atraumatic restorative treatment on dentine caries arrestment in primary molars of preschool children: A 12-months parallel randomized controlled clinical trial. J. Dent. 2019, 88, 103165. [Google Scholar] [CrossRef]
- Gao, S.S.; Chen, K.J.; Duangthip, D.; Wong, M.C.M.; Lo, E.C.M.; Chu, C.H. Arresting early childhood caries using silver and fluoride products—A randomised trial. J. Dent. 2020, 103, 103522. [Google Scholar] [CrossRef]
- Zhi, Q.H.; Lo, E.C.M.; Lin, H.C. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J. Dent. 2012, 40, 962–967. [Google Scholar] [CrossRef]
- Al-Nerabieah, Z.; Arrag, E.; Rajab, A. Cariostatic efficacy and children acceptance of nano-silver fluoride versus silver diamine fluoride: A randomized controlled clinical trial. J. Stomatol. 2020, 73, 100–106. [Google Scholar] [CrossRef]
- Saravanan, S.; Madivanan, I.; Subhashini, B.; Felix, J.W. Prevalence pattern of dental caries in the primary dentition among school children. Indian J. Dent. Res. 2005, 16, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Vaswani, S.; Sharma, D.S.; Mishra, S.; Sharma, S. Histologic validation of ICDAS-II and polarization sensitive optical coherence tomography to detect smooth surface early carious lesions. Int. J. Paediatr. Dent. 2018, 29, 193–202. [Google Scholar] [CrossRef] [PubMed]

| Authors (Year) | Sources | Location | Database | Type of Study |
|---|---|---|---|---|
| Abdellatif et al., 2021 [35] | Eur Arch Paed Dent | Saudi Arabia | Pubmed, Embase, Scopus | RCT |
| Zhi et al., 2021 [43] | J Dent | China | Pubmed, Embase, Scopus | RCT |
| Gao et al., 2020 [42] | J Dent | China | Pubmed, Embase, Scopus | RCT |
| Mabangkhru et al., 2020 [39] | J Dent | China | Pubmed, Embase, Scopus | RCT |
| Daga et al., 2020 [36] | Indian J Public Health Res Dev | India | Embase | RCT |
| Tirupathi et al., 2019 [40] | J Clin Exp Dent | India | Scopus | RCT |
| Vollú et al., 2019 [41] | J Dent | Brazil | Pubmed, Embase, Scopus | RCT |
| Fung et al., 2018 [37] | J Dent Res | China | Pubmed, Scopus | RCT |
| Llodra et al., 2005 [38] | J Dent Res | Spain | Pubmed, Embase, Scopus | RCT |
| RCT = Randomized Controlled Trial | ||||
| Authors (Year) | N-Participants (% Dropout) | Age-Range | M/F | Caries Prevalence at Baseline | Caries Lesions in Primary Molars at Baseline (n) | Intervention | Blinding | Findings (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Test | Control | Test | Control | Test | Control | Test | Control | ||||||
| Abdellatif et al. (2021) [35] | 40 † (32.50%) | 39 † (33.33%) | 3–8 yy † | 32/47 † | dmft = 4.13 † | 59 | 98 | 38% SDF at baseline and every 6 mo. | ART | No | 6 mo. | 100.00% (49/49) | 94.87% (74/78) |
| 12 mo. | 97.95% (48/49) | 92.86% (65/70) | |||||||||||
| ICDAS † | |||||||||||||
| 4 = 13.9% | |||||||||||||
| 5 = 62.4% | |||||||||||||
| 6 = 23.6% | |||||||||||||
| Mabangkhru et al. (2020) [39] | 153 † (15.03%) | 149 † (10.73%) | 1–5 yy † | 172/130 † | dmft = 5.27 † | 279 | 367 | 38% SDF at baseline repeated every 6 mo. | 5% NaF varnish at baseline repeated every 6 mo. | Participants and examiner | 6 mo. | 17.20% (48/279) | 9.81% (36/367) |
| 12 mo. | 23.65% (66/279) | 13.08% (48/367) | |||||||||||
| Tirupathi et al. (2019) [40] | 26 (7.69%) | 24 (4.16%) | 6–10 yy | 17/33 | dmft = 4.51 | 76* | 71* | 38% SDF at baseline (G-B) | 5% NSSF at baseline. (G-A) | Participants and examiner | 1 mo. | 93.42% (71/76) | 94.37% (67/71) |
| 3 mo. | 84.21% (64/76) | 88.73% (63/71) | |||||||||||
| 6 mo. | 78.95% (60/76) | 80.28% (57/71) | |||||||||||
| 12 mo. | 71.05% (54/76) | 77.46% (55/71) | |||||||||||
| Vollú et al. (2019) [41] | 34 (8.82%) | 33 (21.21%) | 2–5 yy | 41/26 | dmft = 6.72 | 65 | 53 | 30% SDF at baseline | ART | No | 3 mo. | 100.0% (65/65) | 96.15% (50/52) |
| 6 mo. | 89.06% (57/64) | 91.67% (44/48) | |||||||||||
| ICDAS | 12 mo. | 88.71% (55/62) | 95.56% (43/45) | ||||||||||
| 5 = 87.7% | |||||||||||||
| 6 = 12.3% | |||||||||||||
| Fung et al. (2018) [37] | 444 † (10.36%) | 444† (9.68%) | 3–4 yy † | 519/369 † | dmft = 3.85 † | 837 | 847 | 38% SDF at baseline and repeated every 12 mo. (G3) and every 6 mo. (G4) | 12% SDF at baseline repeated every 12 mo. (G1) and every 6 mo. (G2) | Participants and examiner | G3 | G1 | |
| 24 mo. | 46.36% (172/371) | 34.25% (124/362) | |||||||||||
| 30 mo. | 49.06% (182/371) | 36.74% (133/362) | |||||||||||
| G4 | G2 | ||||||||||||
| 24 mo. | 61.68% (227/368) | 41.38% (168/406) | |||||||||||
| 30 mo. | 60.65% (222/366) | 39.60% (160/404) | |||||||||||
| Author (Year) | N-Participants (% Dropout) | Age YY (Range or Mean) | M/F | Caries at Baseline (Mean) | Intervention | Blinding | Outcomes | Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Daga et al. (2020) [36] | G1 | G2 | G3 | 5–8 | No Data | No Data | G1 | G2 | G3 | No | Mean active caries (n) | G1 | G2 | G3 | |
| 16 (0.00%) | 16 (6.25%) | 16 (12.50%) | 38% SDF at baseline and at 1-2-3 mo. | 38% SDF at baseline and every 3 mo. | 38% SDF at baseline and every 6 mo. | 0 mo. | 2.56 | 2.25 | 2.12 | ||||||
| 6 mo. | 0.43 | 0.62 | 1.06 | ||||||||||||
| 12 mo. | 0.31 | 0.53 | 1.35 | ||||||||||||
| Significantly reduction on mean active caries in all groups (p = 0.01) and statistically significant differences at 12 mo. among G1 to G3 | |||||||||||||||
| Gao et al. (2020) [42] | G1 | G2 | 3–4 | No Data | dmft (5.91) | G1 | G2 | Participants and examiner | Caries arresting rate (%) | G1 | G2 | ||||
| 535 (16.45%) | 535 (19.06%) | 25 % AgNO3 followed by 5 % NaF varnish at baseline and every 6 mo. | 38% SDF followed by placebo varnish at baseline and every 6 mo. | 6 mo. | 41.3% | 38.7% | |||||||||
| 12 mo. | 62.4% | 60.0% | |||||||||||||
| 18 mo. | 64.1% | 62.4% | |||||||||||||
| 24 mo. | 68.6% | 66.5% | |||||||||||||
| 30 mo. | 70.6% | 68.9% | |||||||||||||
| Odds ratio (Ref.: lower posterior teeth) | |||||||||||||||
| Upper anterior teeth | 6.55 | ||||||||||||||
| Upper posterior teeth | 1.50 | ||||||||||||||
| Lower anterior teeth | 23.37 | ||||||||||||||
| Tooth location significantly related with caries arresting (p < 0.01): carious lesions in anterior teeth more likely to be arrested. | |||||||||||||||
| Zhi et al. (2012) [43] | G1 | G2 | G3 | 3.8 ± 0.6 | 82/79 | dmft (5.1) | G1 | G2 | G3 | No | Caries arresting rate (%) | G1 | G2 | G3 | |
| 71 (15.49%) | 69 (14.49%) | 72 (13.9%) | 38% SDF at baseline and every 12 mo. | 38% SDF at baseline and every 6 mo. | GI | 6 mo. | 31.5% | 43.3% | 31.3% | ||||||
| 12 mo. | 37.0% | 53.0% | 28.6% | ||||||||||||
| 18 mo. | 77.2% | 82.9% | 73.1% | ||||||||||||
| 24 mo. | 79.2% | 90.7% | 81.8% | ||||||||||||
| Odds Ratio (Ref.: posterior teeth) | |||||||||||||||
| Anterior 5.55 | |||||||||||||||
| Carious lesions in anterior teeth more likely to be arrested (p < 0.01) | |||||||||||||||
| Llodra et al. (2005) † [38] | G1 | G2 | 6.29 ± 0.48 | 229/223 | dmfs (3.55) | G1 | G2 | No | Caries arresting rate (%) | G1 | G2 | ||||
| Primary teeth | |||||||||||||||
| 225 (20.00%) | 227 (14.98%) | 38% SDF at baseline and every 6 mo. | No treatment | 36 mo. | 97% | 48% | |||||||||
| Significant differences between the groups in mean new decayed surfaces (p < 0.01). Significantly more surfaces with inactive caries in G1 (p < 0.05). | |||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaffarano, L.; Salerno, C.; Campus, G.; Cirio, S.; Balian, A.; Karanxha, L.; Cagetti, M.G. Silver Diamine Fluoride (SDF) Efficacy in Arresting Cavitated Caries Lesions in Primary Molars: A Systematic Review and Metanalysis. Int. J. Environ. Res. Public Health 2022, 19, 12917. https://doi.org/10.3390/ijerph191912917
Zaffarano L, Salerno C, Campus G, Cirio S, Balian A, Karanxha L, Cagetti MG. Silver Diamine Fluoride (SDF) Efficacy in Arresting Cavitated Caries Lesions in Primary Molars: A Systematic Review and Metanalysis. International Journal of Environmental Research and Public Health. 2022; 19(19):12917. https://doi.org/10.3390/ijerph191912917
Chicago/Turabian StyleZaffarano, Luciano, Claudia Salerno, Guglielmo Campus, Silvia Cirio, Araxi Balian, Lorena Karanxha, and Maria Grazia Cagetti. 2022. "Silver Diamine Fluoride (SDF) Efficacy in Arresting Cavitated Caries Lesions in Primary Molars: A Systematic Review and Metanalysis" International Journal of Environmental Research and Public Health 19, no. 19: 12917. https://doi.org/10.3390/ijerph191912917
APA StyleZaffarano, L., Salerno, C., Campus, G., Cirio, S., Balian, A., Karanxha, L., & Cagetti, M. G. (2022). Silver Diamine Fluoride (SDF) Efficacy in Arresting Cavitated Caries Lesions in Primary Molars: A Systematic Review and Metanalysis. International Journal of Environmental Research and Public Health, 19(19), 12917. https://doi.org/10.3390/ijerph191912917