Psychological Reactions of Hospital Workers to a Pandemic: A Comparison of SARS-CoV-2 in 2020 and SARS in 2003
Abstract
:1. Introduction
2. Materials and Methods
2.1. Background of the Study
2.2. Study Design and Measures
2.2.1. Exposure to SARS-CoV-2
2.2.2. Impact of Event Scale (IES)
2.2.3. Chinese-Version Health Questionnaire (CHQ)
2.2.4. Distress Thermometer (DT)
2.3. Statistical Analysis
3. Results
3.1. Characteristics of Respondents
3.2. Comparison of Clinical Characteristics of Hospital Workers during SARS-CoV-2 and SARS
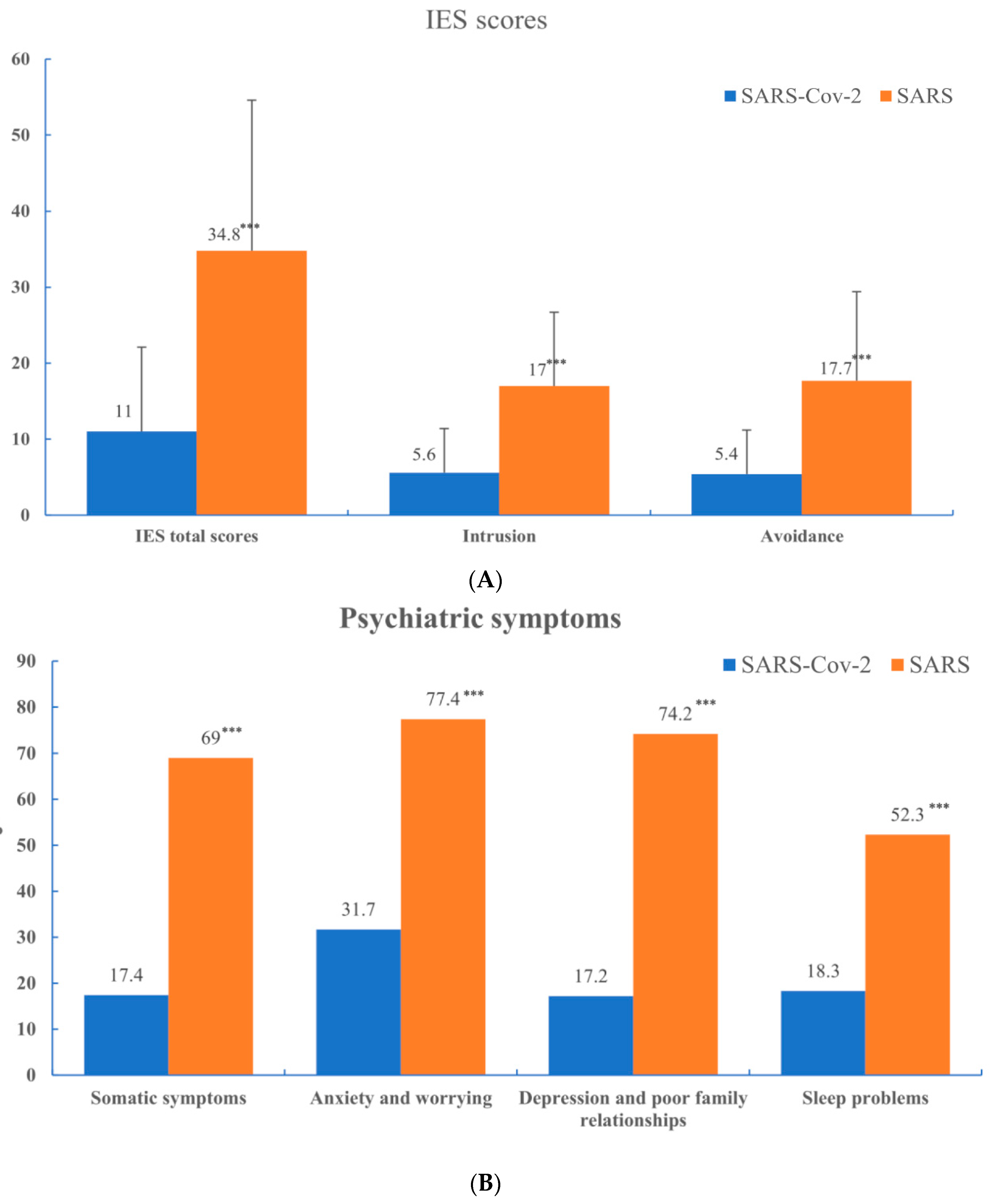
3.3. Impact of Events and Psychiatric Morbidity during SARS-CoV-2 and SARS
3.4. Comparison of Characteristics and Psychological Impact of Hospital Workers Who Have Had or Not Had Exposure to SARS
3.5. Perception of Threat
3.6. Risk of Psychiatric Morbidity in Hospital Workers Who Had Exposure to SARS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cartwright, F.F. Disease & History; Sutton Publishing Ltd.: Stroud, UK, 2004. [Google Scholar]
- Dawood, F.S.; Jain, S.; Finelli, L.; Shaw, M.W.; Lindstrom, S.; Garten, R.J.; Gubareva, L.V.; Xu, X.; Bridges, C.B.; Uyeki, T.M.; et al. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N. Engl. J. Med. 2009, 360, 2605–2615. [Google Scholar]
- Feldmann, H.; Jones, S.; Klenk, H.D.; Schnittler, H.J. Ebola virus: From discovery to vaccine. Nat. Rev. Immunol. 2003, 3, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Ashour, H.M.; Elkhatib, W.F.; Rahman, M.M.; Elshabrawy, H.A. Insights into the Recent 2019 Novel Coronavirus (SARS-CoV-2) in Light of Past Human Coronavirus Outbreaks. Pathogens 2020, 9, 186. [Google Scholar] [CrossRef] [Green Version]
- Kop, W.J. Biopsychosocial Processes of Health and Disease During the COVID-19 Pandemic. Psychosom. Med. 2021, 83, 304–308. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Pacitti, F.; Di Lorenzo, G.; Di Marco, A.; Siracusano, A.; Rossi, A. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw. Open 2020, 3, e2010185. [Google Scholar] [CrossRef] [PubMed]
- Gold, J.A. COVID-19: Adverse mental health outcomes for healthcare workers. BMJ 2020, 369, m1815. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Peng, T.; Hao, X.; Zou, C.; Lin, K.; Liao, X.; Chen, S.; Hayhoe, B. Psychological Distress Reported by Primary Care Physicians in China During the COVID-19 Pandemic. Psychosom. Med. 2021, 83, 380–386. [Google Scholar] [CrossRef]
- Ueda, M.; Stickley, A.; Sueki, H.; Matsubayashi, T. Mental health status of the general population in Japan during the COVID-19 pandemic. Psychiatry Clin. Neurosci. 2020, 74, 505–506. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef]
- Gorwood, P.; Fiorillo, A. One year after the COVID-19: What have we learnt, what shall we do next? Eur. Psychiatry 2021, 64, e15. [Google Scholar] [CrossRef]
- Ripp, J.; Peccoralo, L.; Charney, D. Attending to the Emotional Well-Being of the Health Care Workforce in a New York City Health System During the COVID-19 Pandemic. Acad. Med. 2020, 95, 1136–1139. [Google Scholar] [CrossRef]
- World Health Organization Geneva: 2003. Summary of severe acute respiratory syndrome (SARS) cases: International. 2015.
- Su, T.P.; Lien, T.C.; Yang, C.Y.; Su, Y.L.; Wang, J.H.; Tsai, S.L.; Yin, J.C. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007, 41, 119–130. [Google Scholar] [CrossRef]
- Chen, C.S.; Wu, H.Y.; Yang, P.; Yen, C.F. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr. Serv. 2005, 56, 76–79. [Google Scholar] [CrossRef]
- Chong, M.Y.; Wang, W.C.; Hsieh, W.C.; Lee, C.Y.; Chiu, N.M.; Yeh, W.C.; Huang, T.-L.; Wen, J.-K.; Chen, C.-L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry 2004, 185, 127–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lei, M.K.; Klopack, E.T. Social and psychological consequences of the COVID-19 outbreak: The experiences of Taiwan and Hong Kong. Psychol. Trauma 2020, 12, S35–S37. [Google Scholar] [CrossRef] [PubMed]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 9096. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.F. Grief: A Brief History of Research on How Body, Mind, and Brain Adapt. Psychosom. Med. 2019, 81, 731–738. [Google Scholar] [CrossRef]
- Horowitz, M.; Wilner, N.; Alvarez, W. Impact of Event Scale: A measure of subjective stress. Psychosom. Med. 1979, 41, 209–218. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.Y.; Yeh, W.Y.; Chen, C.W.; Wang, J.D. Prevalence and psychosocial risk factors of upper extremity musculoskeletal pain in industries of Taiwan: A nationwide study. J. Occup. Health 2005, 47, 311–318. [Google Scholar] [CrossRef]
- Hsu, C.C.; Chong, M.Y.; Yang, P.; Yen, C.F. Posttraumatic stress disorder among adolescent earthquake victims in Taiwan. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, T.A.; Williams, P. The design and development of a screening questionnaire (CHQ) for use in community studies of mental disorders in Taiwan. Psychol. Med. 1986, 16, 415–422. [Google Scholar] [CrossRef]
- Goldberg, D.P. The Detection of Psychiatric Illness by Questionnaire; Oxford University Press: London, UK, 1972. [Google Scholar]
- Chong, M.Y.; Wilkinson, G. Validation of 30- and 12-item versions of the Chinese Health Questionnaire (CHQ) in patients admitted for general health screening. Psychol. Med. 1989, 19, 495–505. [Google Scholar] [CrossRef]
- Cheng, T.A.; Wu, J.T.; Chong, M.Y.; Williams, P. Internal consistency and factor structure of the Chinese Health Questionnaire. Acta Psychiatr. Scand. 1990, 82, 304–308. [Google Scholar] [CrossRef]
- Schubart, J.R.; Emerich, M.; Farnan, M.; Stanley Smith, J.; Kauffman, G.L.; Kass, R.B. Screening for psychological distress in surgical breast cancer patients. Ann. Surg. Oncol. 2014, 21, 3348–3353. [Google Scholar] [CrossRef] [PubMed]
- Donovan, K.A.; Grassi, L.; McGinty, H.L.; Jacobsen, P.B. Validation of the distress thermometer worldwide: State of the science. Psychooncology 2014, 23, 241–250. [Google Scholar] [CrossRef]
- Diederen, K.; Haverman, L.; Grootenhuis, M.A.; Benninga, M.A.; Kindermann, A. Parental Distress and Quality of Life in Pediatric Inflammatory Bowel Disease: Implications for the Outpatient Clinic. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.K.; Wang, C.C.; Lin, M.C.; Kung, C.T.; Lan, K.C.; Lee, C.T. Effective strategies to prevent coronavirus disease-2019 (COVID-19) outbreak in hospital. J. Hosp. Infect. 2020, 105, 102–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cai, W.; Lian, B.; Song, X.; Hou, T.; Deng, G.; Li, H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J. Psychiatry 2020, 51, 102111. [Google Scholar] [CrossRef]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Khan, F.A.; Shanmugam, G.N.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef]
- Consolo, U.; Bellini, P.; Bencivenni, D.; Iani, C.; Checchi, V. Epidemiological Aspects and Psychological Reactions to COVID-19 of Dental Practitioners in the Northern Italy Districts of Modena and Reggio Emilia. Int. J. Environ. Res. Public Health 2020, 17, 3459. [Google Scholar] [CrossRef]
- Shacham, M.; Hamama-Raz, Y.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; Mijiritsky, E. COVID-19 Factors and Psychological Factors Associated with Elevated Psychological Distress among Dentists and Dental Hygienists in Israel. Int. J. Environ. Res. Public Health 2020, 17, 2900. [Google Scholar] [CrossRef] [Green Version]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.; Tian, Q.; Leng, H.; Du, J.; et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Lu, L.; Chen, T.; Ye, S.; Kelifa, M.O.; Cao, N.; Zhang, Q.; Liang, T.; Wang, W. Healthcare Worker’s Mental Health and Their Associated Predictors During the Epidemic Peak of COVID-19. Psychol. Res. Behav. Manag. 2021, 14, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.J.; Jin, Y.; Rao, W.W.; Li, W.; Zhao, N.; Cheung, T.; Chee, H.N.; Wang, Y.-Y.; Zhang, Q.-E.; Xiang, Y.-T. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: A systematic review and meta-analysis of observational studies. J. Affect. Disord. 2021, 287, 145–157. [Google Scholar] [CrossRef]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef]
- Johnson, H.; Thompson, A. The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clin. Psychol. Rev. 2008, 28, 36–47. [Google Scholar] [CrossRef]
- Wachinger, G.; Renn, O.; Begg, C.; Kuhlicke, C. The risk perception paradox--implications for governance and communication of natural hazards. Risk Anal. 2013, 33, 1049–1065. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Lu, H.; Cheung, E.F.; Neumann, D.L.; Shum, D.H.; Chan, R.C. “Female Preponderance” of Depression in Non-clinical Populations: A Meta-Analytic Study. Front. Psychol. 2016, 7, 1398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weisaeth, L. Importance of high response rates in traumatic stress research. Acta Psychiatr. Scand. Suppl. 1989, 355, 131–137. [Google Scholar] [CrossRef] [PubMed]
| Variable | SARS-CoV-2 n = 1816 | SARS n = 1257 |
|---|---|---|
| Gender: n (%) | ||
| Female | 1544 (85.0) | 1019 (81.1) |
| Male | 272 (15.0) | 238 (18.9) |
| Age, years: mean (s.d.) | 38.7 ± 10.2 | 31.8 ± 6.43 |
| Job title: n (%) | ||
| Doctor | 132 (7.3) | 139 (11.1) |
| Nurse | 1124 (61.9) | 676 (53.8) |
| Others * | 560 (30.8) | 442 (35.1) |
| Work experience, years: mean (s.d.) | 14.9 ± 10.2 | 8.5 ± 5.7 |
| Marital status: n (%) | ||
| Married | 1002 (55.2) | 621 (49.4) |
| Unmarried | 814 (44.8) | 636 (50.6) |
| Living condition: n (%) | ||
| With family | 1385 (76.3) | 825 (65.6) |
| Dormitory/Other | 431 (23.7) | 432 (34.4)) |
| Care of SARS-CoV-2 patients/SARS patients: n (%) | ||
| Yes | 78 (4.3) | 126 (9.9) |
| No | 1686 (92.8) | 1022 (81.3) |
| Not sure | 52 (2.9) | 122 (9.7) |
| Quarantine: n (%) | ||
| Yes | 74 (4.1) | 79 (6.3) |
| No | 1742 (95.9) | 1178 (93.7) |
| Variable | SARS Experience n = 696 | No SARS Experience n = 1120 | t/χ2 | p |
|---|---|---|---|---|
| Gender: n (%) | 7.88 | 0.005 | ||
| Female | 571 (82.0) | 973 (86.9) | ||
| Male | 125 (18.0) | 147 (13.1) | ||
| Age, years: mean (s.d.) | 48.4 ± 6.2 | 32.6 ± 6.9 | −50.80 | <0.001 |
| Job title: n (%) | 84.71 | <0.001 | ||
| Doctor | 42 (6.0) | 90 (8.0) | ||
| Nurse | 373 (53.6) | 751 (67.1) | ||
| Others * | 281 (40.4) | 279 (24.9) | ||
| Work experience, years: mean (s.d.) | 25.3 ± 6.1 | 8.3 ± 6.0 | −58.16 | <0.001 |
| Marital status: n (%) | 259.48 | <0.001 | ||
| Married | 550 (79.0) | 452 (40.4) | ||
| Unmarried | 146 (21.0) | 668 (59.6) | ||
| Living condition: n (%) | 70.83 | <0.001 | ||
| With family | 605 (86.9) | 780 (69.6) | ||
| Dormitory/Other | 91 (13.1) | 340 (30.4)) | ||
| Care of SARS-CoV-2 patients: n (%) | 1.24 | 0.54 | ||
| Yes | 27 (3.9) | 51 (4.6) | ||
| No | 652 (93.7) | 1034 (92.3) | ||
| Not sure | 17 (2.4) | 35 (3.1) | ||
| Quarantine: n (%) | 48.89 | <0.001 | ||
| Yes | 57 (4.1) | 17 (1.5) | ||
| No | 639 (91.8) | 1103 (98.5) |
| Yes n = 696 | No n = 1120 | B (95% C.I.) | p | |
|---|---|---|---|---|
| IES total scores | 11.6 | 10.7 | 0.82(−0.97, 2.60) | 0.37 |
| Intrusion | 6.0 | 5.4 | 0.33(−0.61, 1.27) | 0.49 |
| Avoidance | 5.6 | 5.3 | 0.49(−0.44, 1.41) | 0.30 |
| DT | 2.4 | 2.1 | 0.07(−0.24, 0.39) | 0.64 |
| CHQ | ||||
| CHQ scores | 1.69 | 1.44 | 0.06(−0.39, 0.51) | 0.70 |
| CHQ < 3 CHQ ≥ 3 | 538(77.3) 158(22.7) | 895(79.9) 225(20.1) | 1.01(0.65, 1.58) | 0.97 |
| Item | SARS Experience n = 696(%) | No SARS Experience n = 1120(%) | B (95% C.I.) | p |
|---|---|---|---|---|
| I might infect with SARS-CoV-2 because of taking care of SARS-CoV-2 patients. | 351 (50.1) | 449 (40.1) | 1.13 (0.80, 1.59) | 0.49 |
| I believe the hospital will take good care of me if I infect with SARS-CoV-2 because of my work. | 509 (73.1) | 626 (55.9) | 0.83 (0.59, 1.19) | 0.31 |
| I have little control over whether I get infected or not. | 203 (29.2) | 312 (27.9) | 1.45 (1.01, 2.08) | 0.043 |
| I accept the risk of caring for SARS-CoV-2 patients. | 256 (36.8) | 286 (25.5) | 0.48 (0.34, 0.70) | <0.001 |
| I think that it is my duty to take care of SARS-CoV-2 patients. | 428 (61.5) | 489 (43.7) | 0.71 (0.51, 0.99) | 0.041 |
| I think of resigning because of SARS-CoV-2. | 59 (8.5) | 153 (13.7) | 0.64 (0.38, 1.10) | 0.10 |
| People avoid my family because of my work. | 126 (18.1) | 155 (13.8) | 1.06 (0.68, 1.65) | 0.79 |
| My workplace had good morale before the SARS-CoV-2 pandemic. | 371 (53.3) | 541 (48.3) | 0.99 (0.72, 1.38) | 0.97 |
| My workload has increased a lot during SARS-CoV-2. | 385 (55.3) | 513 (45.8) | 1.11 (0.79, 1.55) | 0.55 |
| I feel more stress at work. | 376 (54.0) | 512 (45.7) | 0.92 (0.66, 1.28) | 0.61 |
| I think my hospital should provide staff with psychological counseling. | 533 (76.6) | 713 (63.7) | 0.75 (0.52, 1.08) | 0.12 |
| Item | β | S.E. | Wald | Odd Ratio | C.I. | p |
|---|---|---|---|---|---|---|
| DT | 0.56 | 0.06 | 82.76 | 1.76 | 1.56–1.98 | <0.001 |
| IES-Intrusion | 0.14 | 0.03 | 21.25 | 1.15 | 1.08–1.22 | <0.001 |
| IES-Avoidance | −0.02 | 0.03 | 0.38 | 0.98 | 0.92–1.04 | 0.54 |
| Female | 0.72 | 0.33 | 4.84 | 2.06 | 1.08–3.92 | 0.028 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.; Wang, L.-J.; Chou, W.-J.; Chiang, M.-C.; Huang, S.; Lin, Y.-C.; Lin, J.-Y.; Chiu, N.-M.; Chen, C.-H.; Lee, I.-K.; et al. Psychological Reactions of Hospital Workers to a Pandemic: A Comparison of SARS-CoV-2 in 2020 and SARS in 2003. Int. J. Environ. Res. Public Health 2022, 19, 833. https://doi.org/10.3390/ijerph19020833
Lee Y, Wang L-J, Chou W-J, Chiang M-C, Huang S, Lin Y-C, Lin J-Y, Chiu N-M, Chen C-H, Lee I-K, et al. Psychological Reactions of Hospital Workers to a Pandemic: A Comparison of SARS-CoV-2 in 2020 and SARS in 2003. International Journal of Environmental Research and Public Health. 2022; 19(2):833. https://doi.org/10.3390/ijerph19020833
Chicago/Turabian StyleLee, Yu, Liang-Jen Wang, Wen-Jiun Chou, Ming-Chu Chiang, Shan Huang, Yi-Chun Lin, Jie-Yi Lin, Nien-Mu Chiu, Chih-Hung Chen, Ing-Kit Lee, and et al. 2022. "Psychological Reactions of Hospital Workers to a Pandemic: A Comparison of SARS-CoV-2 in 2020 and SARS in 2003" International Journal of Environmental Research and Public Health 19, no. 2: 833. https://doi.org/10.3390/ijerph19020833
APA StyleLee, Y., Wang, L.-J., Chou, W.-J., Chiang, M.-C., Huang, S., Lin, Y.-C., Lin, J.-Y., Chiu, N.-M., Chen, C.-H., Lee, I.-K., Kung, C.-T., Wang, C.-C., & Chong, M.-Y. (2022). Psychological Reactions of Hospital Workers to a Pandemic: A Comparison of SARS-CoV-2 in 2020 and SARS in 2003. International Journal of Environmental Research and Public Health, 19(2), 833. https://doi.org/10.3390/ijerph19020833








