Cranio-Mandibular Disorders after Whiplash Injury: A Mono-Institutional Clinical Study on 31 Patients
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
- (A)
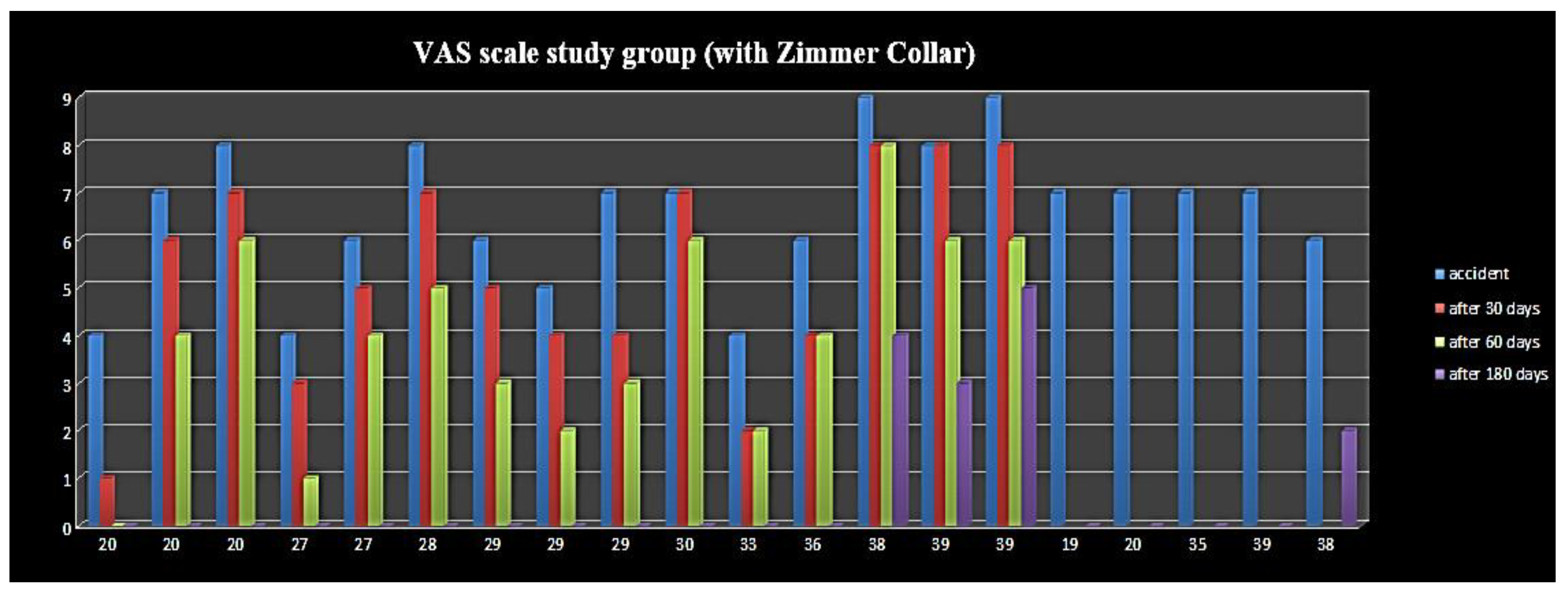
- Lesion severity: such as manifestation of a traumatic brain injury or craniocaudal joint dislocation. Indeed, a VAS of 4 remained in the patient that reported a traumatic brain injury and a VAS of 3 and 5 remained in those patients subject to very strong trauma.
- (B)
- Pre-existent craniomandibular dysfunction: Two patients out of three with a residual VAS higher than 3 showed signs of parafunction at the six-month follow-up period.
- (C)
- Patient age: three out of five patients with a residual VAS higher than 3 were older than 38 years; therefore, such patients were referred for longer therapy and gum shield use.
- (D)
- Control group: in the short term, Zimmer collar therapy promotes tendon myositis, with greater pain reported with respect to the control group (no Zimmer Collar); furthermore, chronic pain after six months was equal between the study and control group in terms of percentage, thus highlighting how pain persistence is due to a central sensitization phenomenon affecting the nervous system.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spitzer, W.O.; Skovron, M.L.; Salmi, L.R.; Cassidy, J.D.; Duranceau, J.; Suissa, S.; Zeiss, E. Scientific monograph of the Quebec Task Force on Whiplash-Associated disorders: Redefining “whiplash” and its management. Spine 1995, 20, 1S–73S. [Google Scholar] [PubMed]
- Sale, H.; Isberg, A. Delayed temporomandibular joint pain and dysfunction induced by whiplash trauma: A controlled prospective study. J. Am. Dent. Assoc. 2007, 138, 1084–1091. [Google Scholar] [CrossRef] [Green Version]
- Marini, I.; Paduano, S.; Bartolucci, M.L.; Bortolotti, F.; Bonetti, G.A. The prevalence of temporomandibular disorders in patients with late whiplash syndrome who experience orofacial pain: A case-control series study. J. Am. Dent. Assoc. 2013, 144, 486–490. [Google Scholar] [CrossRef]
- Salé, H.; Bryndahl, F.; Isberg, A. A 15-year follow-up of temporomandibular joint symptoms and magnetic resonance imaging findings in whiplash patients: A prospective, controlled study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 522–532. [Google Scholar] [CrossRef]
- Haggman-Henrikson, B.; Òsterlund, C.; Eriksson, P. Endurance during chewing in whiplash-associated disorders and TMD. J. Dent. Res. 2004, 83, 946–950. [Google Scholar] [CrossRef] [Green Version]
- Kasch, H.; Hjorth, T.; Svensson, P.; Nyhuus, L.; Jensen, T.S. Temporomandibular disorders after whiplash injury: A controlled, prospective study. J. Orofac. Pain. 2002, 16, 118–128. [Google Scholar]
- del Palomar, P.; Doblaré, M. Dynamic 3D FE modelling of the human temporomandibular joint during whiplash. Med. Eng. Phys. 2008, 30, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Abd-Ul-Salam, H.; Kryshtalskyj, B.; Weinberg, S. Temporomandibular joint arthroscopic findings in patients with cervical flexion-exstension Injury (Whiplash): A preliminary study of 30 patients. J. Can. Dent. Assoc. 2002, 68, 693–696. [Google Scholar]
- Ferrari, R.; Schrader, H.; Obelieniene, D. Prevalence of temporomandibular disorders associated with whiplash injury in Lithuania. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 87, 653–657. [Google Scholar] [CrossRef]
- Probert, T.C.; Wiesenfeld, D.; Reade, P.C. Temporomandibular pain dysfunction disorder resulting from road traffic accidents-An Australian study. Int. J. Oral Maxillofac. Surg. 1994, 23, 338–341. [Google Scholar] [CrossRef]
- Dalewski, B.; Kamińska, A.; Szydłowski, M.; Kozak, M.; Sobolewska, E. Comparison of Early Effectiveness of Three Different Intervention Methods in Patients with Chronic Orofacial Pain: A Randomized, Controlled Clinical Trial. Pain Res. Manag. 2019, 2019, 7954291. [Google Scholar] [CrossRef] [Green Version]
- Dworkin, S.F.; LeResche, L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J. Craniomandib. Disord. 1992, 6, 301–335. [Google Scholar] [PubMed]
- Weinberg, S.; Lapointe, H. Cervical extension-flexion injury (whiplash) and internal derangement of the temporomandibular joint. J. Oral Maxillofac Surg. 1987, 45, 653–656. [Google Scholar] [CrossRef]
- Lampa, E.; Wänman, A.; Nordh, E.; Häggman-Henrikson, B. Effects on jaw function shortly after whiplash trauma. J. Oral Rehabil. 2017, 44, 941–947. [Google Scholar] [CrossRef]
- Brault, J.R.; Wheeler, J.B.; Siegmund, G.P.; Brault, E.J. Clinical response of human subjects to rear-end automobile collisions. Arch. Phys. Med. Rehabil. 1998, 79, 72–80. [Google Scholar] [CrossRef]
- Garcia RJr Arrington, J.A. The relationship between cervical whiplash and temporomandibular joint injuries: An MRA study. Cranio 1996, 14, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Kolbinson, D.A.; Epstein, J.B.; Senthilselvan, A.; Burgess, J.A. A comparison of TMD patients with or without prior motor vehicle accident involvement: Initial signs, symptoms and diagnostic characteristics. J. Orofac. Pain 1997, 1, 206–214. [Google Scholar]
- Kolbinson, D.A.; Epstein, J.B.; Senthilselvan, A.; Burgess, J.A. Effect of impact and injury characteristics on post-motor vehicle accident temporomandibular disorders. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 665–673. [Google Scholar] [CrossRef]
- Kolbinson, D.A.; Epstein, J.B.; Senthilselvan, A.; Burgess, J.A. A comparison of TMD patients with or without prior motor vehicle accident involvement: Treatment and outcomes. J. Orofac. Pain 1997, 11, 337–345. [Google Scholar] [PubMed]
- Kolbinson, D.A.; Epstein, J.B.; Burgess, J.A.; Senthilselvan, A. Temporo-mandibular disorders, headaches, and neck pain after motor vehicle accidents: A pilot investigation of persistence and litigation effects. J. Prosthet Dent. 1997, 77, 46–53. [Google Scholar] [CrossRef]
- Corsalini, M.; Di Venere, D.; Rapone, B.; Stefanachi, G.; Laforgia, A.; Pettini, F. Evidence of signs and symptoms of Craniomandibular Disorders in Fibromyalgia patients. Open Dent. J. 2017, 11, 91–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krogstad, B.S.; Jokstad, A.; Dahi, B.L.; Soboleva, U. Somatic complaints, psychologic distress, and treatment outcome in two groups of TMD patients, one previously subjected to whiplash injury. J. Orofac. Pain 1998, 12, 136–144. [Google Scholar]
- de Boever, J.A.; Keersmaekers, K. Trauma in patients with temporo-mandibular disorders: Frequency and treatment outcome. J. Oral Rehabil. 1996, 23, 91–96. [Google Scholar] [CrossRef]
- Davis, C.G. Mechanisms of chronic pain from whiplash injury. J. Forensic Leg. Med. 2013, 20, 74–85. [Google Scholar] [CrossRef]
- Solarino, B.; Coppola, F.; Di Vella, G.; Corsalini, M.; Quaranta, N. Vestibular evoked myogenic potentials (VEMPs) in whiplash injury: A prospective study. Acta Otolaryngol. 2009, 129, 976–981. [Google Scholar] [CrossRef]
- Favia, G.; Corsalini, M.; Di Venere, D.; Pettini, F.; Favia, G.; Capodiferro, S.; Maiorano, E. Immunohistochemical evaluation of neuroreceptors in healthy and pathological temporo-mandibular joint. Int. J. Med. Sci. 2013, 10, 1698–1701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curatolo, M.; Bogduk, N.; Ivancic, P.C.; McLean, S.A.; Siegmund, G.P.; Winkelstein, B.A. The role of tissue damage in whiplash-associated disorders: Discussion paper 1. Spine 2011, 36, S309–S315. [Google Scholar] [CrossRef] [Green Version]
- McKee, A.C.; Daneshvar, D.H. The neuropathology of traumatic brain injury. Handb. Clin. Neurol. 2015, 127, 45–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sareen, J. Posttraumatic stress disorder in adults: Impact, comorbidity, risk factors, and treatment. Can. J. Psychiatry 2014, 59, 460–467. [Google Scholar] [CrossRef] [Green Version]





| Grade | Clinical Presentation * | Subgrade |
|---|---|---|
| 0 | No complaint, no physical signs | 2A: point tenderness. normal range of movement |
| 1 | Neck pain, stiffness, or tenderness | |
| 2 | Neck complaint and musculoskeletal signs: decreased range of movement and point tenderness | |
| 3 | Neck complaint and neurologic signs: decreased or absent deep tendon reflexes, weakness, or sensory deficits | 2B: point tenderness. abnormal range of movement |
| 4 | Neck complaint and fracture or dislocation |
| PT No. | AGE | SEX | VAS I Visit | VAS 6 Months | RDC I Visit | RDC 6 Months | Michigan Occlusal Splint | Zimmer Collar |
|---|---|---|---|---|---|---|---|---|
| 1 | 20 | F | 4 | 0 | 1B + 3A | 1A | NO | YES |
| 2 | 20 | M | 7 | 0 | 1B | 0 | NO | YES |
| 3 | 20 | F | 8 | 0 | 1B + 3A | 0 | YES | YES |
| 4 | 27 | M | 4 | 0 | 1B | 0 | NO | YES |
| 5 | 27 | F | 6 | 0 | 1B + 3A | 0 | NO | YES |
| 6 | 28 | F | 8 | 0 | 1B + 3A | 0 | NO | YES |
| 7 | 29 | F | 6 | 0 | 1B | 0 | NO | YES |
| 8 | 29 | F | 5 | 0 | 1B + 2A | 0 | NO | YES |
| 9 | 29 | F | 7 | 0 | 1A | 0 | NO | YES |
| 10 | 30 | F | 7 | 0 | 1B + 3A | 1A | YES | YES |
| 11 | 33 | F | 4 | 0 | 1B | 0 | NO | YES |
| 12 | 36 | F | 6 | 0 | 1B + 3A | 0 | NO | YES |
| 13 | 38 | F | 6 | 4 | 1B + 3A | 1A | YES | YES |
| 14 | 39 | F | 8 | 3 | 1B + SA | 1A | YES | YES |
| 15 | 39 | F | 9 | 5 | 1B + 3A | 1A | YES | YES |
| 16 | 19 | F | 7 | 0 | 1B | 0 | NO | YES |
| 17 | 20 | F | 7 | 0 | 1B | 0 | NO | YES |
| 18 | 35 | M | 7 | 0 | 1A + 1B | 0 | NO | YES |
| 19 | 39 | M | 7 | 0 | 1A + 1B | 0 | NO | YES |
| 20 | 38 | F | 6 | 2 | 1A | 0 | NO | YES |
| PT No. | AGE | SEX | VAS I Visit | VAS 6 Months | RDC I Visit | RDC 6 Months | Michigan Occlusal Splint | Zimmer Collar |
|---|---|---|---|---|---|---|---|---|
| 1 | 20 | F | 8 | 0 | 1B | 0 | NO | NO |
| 2 | 24 | M | 5 | 2 | 1B | 0 | YES | NO |
| 3 | 25 | M | 8 | 0 | 1B | 0 | NO | NO |
| 4 | 27 | M | 5 | 0 | 1A | 0 | NO | NO |
| 5 | 29 | F | 8 | 0 | 2A + 1B | 0 | NO | NO |
| 6 | 29 | F | 5 | 2 | 1A + 3A | 1A | YES | NO |
| 7 | 30 | F | 7 | 0 | 1A | 0 | NO | NO |
| 8 | 32 | F | 7 | 0 | 1A | 0 | NO | NO |
| 9 | 33 | M | 7 | 0 | 1B | 0 | NO | NO |
| 10 | 33 | M | 7 | 2 | 1B + 2A | 1A | YES | NO |
| 11 | 33 | F | 5 | 2 | 1B + 3A | 1A | YES | NO |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corsalini, M.; Capodiferro, S.; dell’Olio, F.; Albanese, G.; Quaranta, N.; Solarino, B.; Catapano, S.; Di Venere, D. Cranio-Mandibular Disorders after Whiplash Injury: A Mono-Institutional Clinical Study on 31 Patients. Int. J. Environ. Res. Public Health 2022, 19, 901. https://doi.org/10.3390/ijerph19020901
Corsalini M, Capodiferro S, dell’Olio F, Albanese G, Quaranta N, Solarino B, Catapano S, Di Venere D. Cranio-Mandibular Disorders after Whiplash Injury: A Mono-Institutional Clinical Study on 31 Patients. International Journal of Environmental Research and Public Health. 2022; 19(2):901. https://doi.org/10.3390/ijerph19020901
Chicago/Turabian StyleCorsalini, Massimo, Saverio Capodiferro, Fabio dell’Olio, Giovanni Albanese, Nicola Quaranta, Biagio Solarino, Santo Catapano, and Daniela Di Venere. 2022. "Cranio-Mandibular Disorders after Whiplash Injury: A Mono-Institutional Clinical Study on 31 Patients" International Journal of Environmental Research and Public Health 19, no. 2: 901. https://doi.org/10.3390/ijerph19020901








