Kinesiological Treatment of Early Spine Osteoarthritis in a Motorcyclist
Abstract
:1. Introduction
2. Case Report
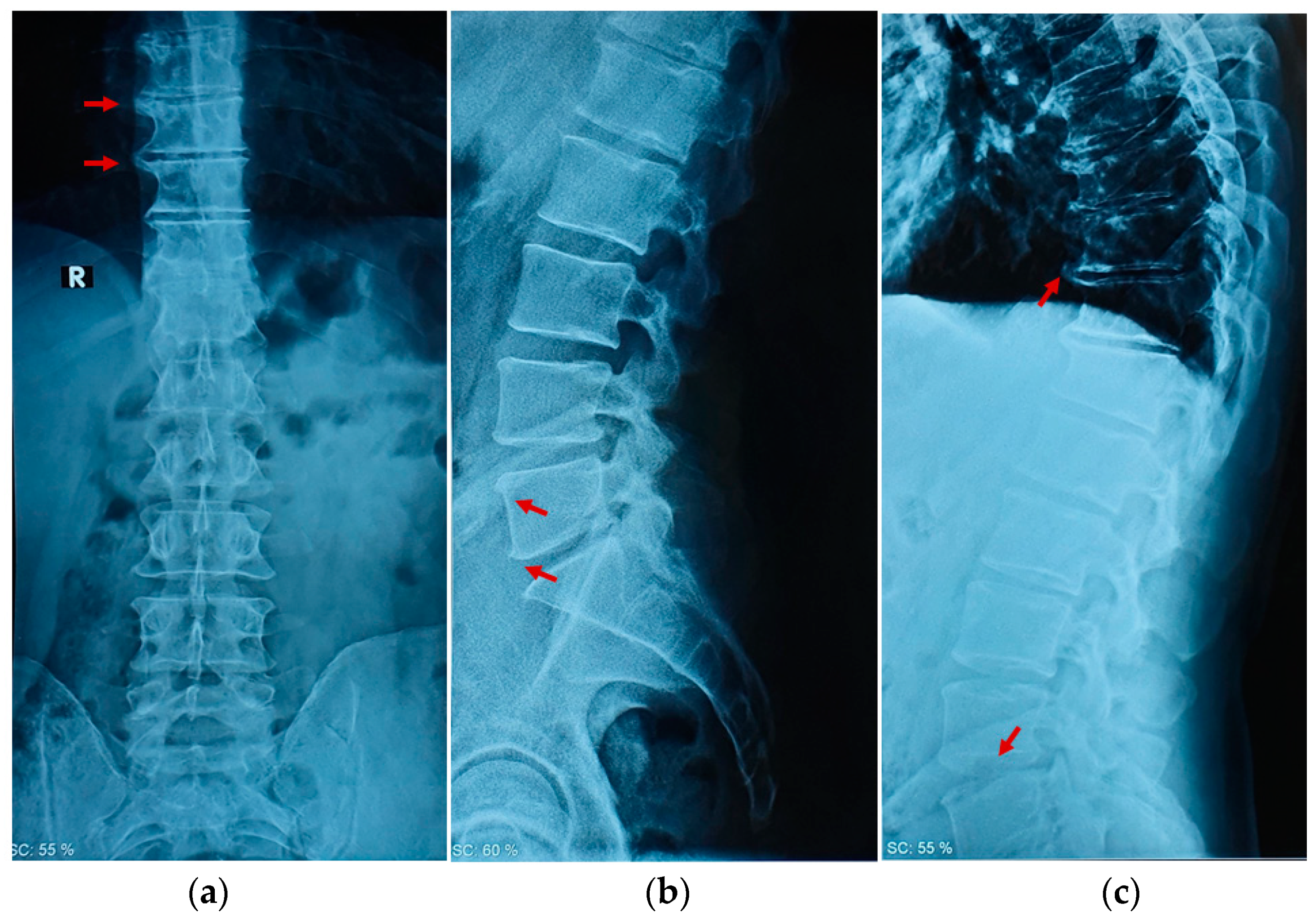
2.1. Clinical Examination
2.2. Physical Examination
2.3. Therapeutic Intervention
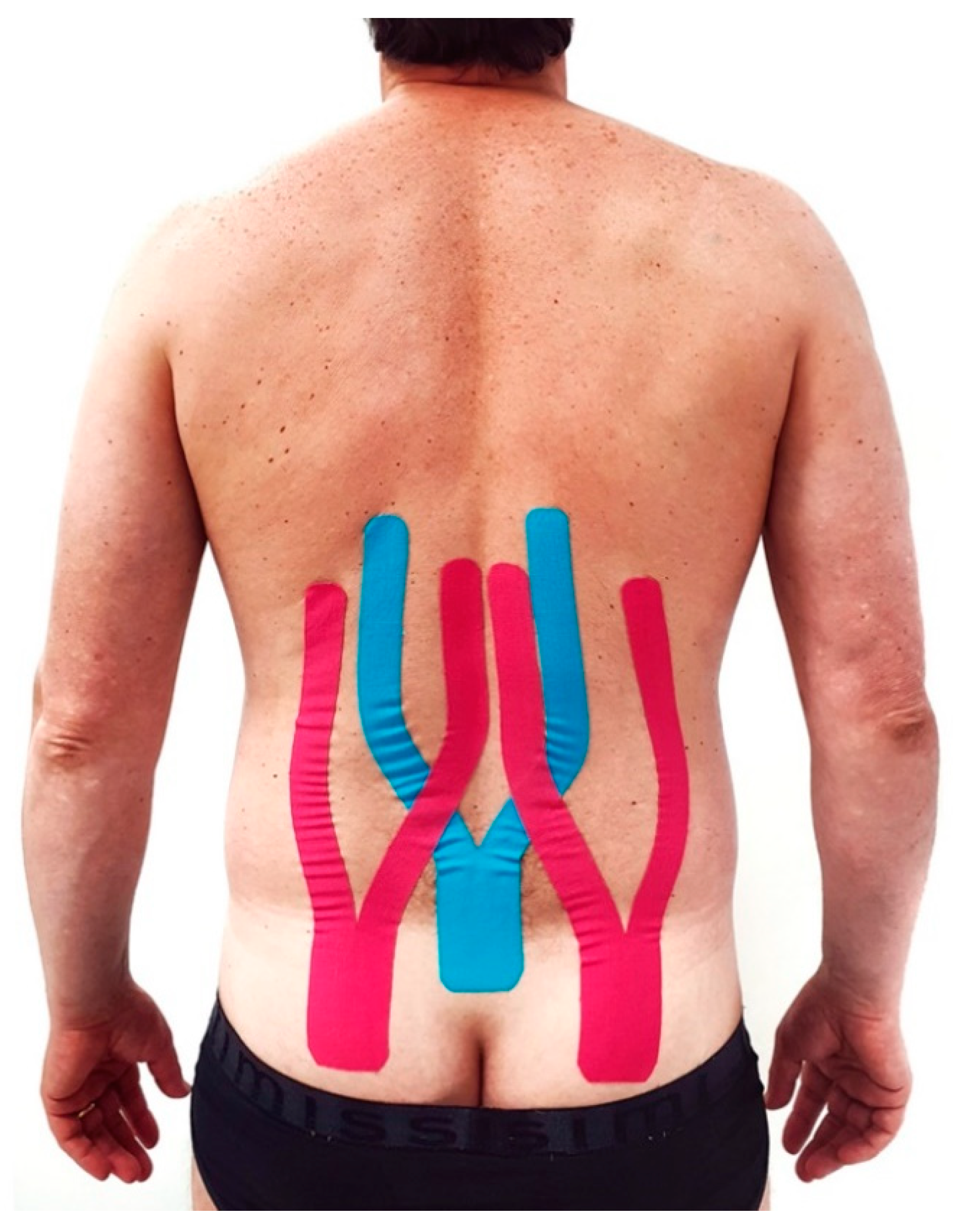
2.4. Kinesio Taping Application
2.5. Exercise Administration
- Upright position with the back leaning against a wall. Bend the knees and push the back against the wall while exhaling (Figure 5a);
- Sitting position with the back against a wall. Place a rolled-up cloth under the lower back and exert rhythmic pressure while exhaling (Figure 5b);
- Supine position. Breathe while inflating the belly and chest alternately. With each exhale, press the lower back to the ground (Figure 5c);
- Supine position. Place a rolled-up cloth in the lumbar area and exert rhythmic pressure while exhaling (Figure 5d);
- Supine position. Place a cloth under the painful part of the dorsal column and extend the arms while exhaling (Figure 5e);
- Supine position. Place a cloth in correspondence under the painful area and carry out torsion movements of the trunk while exhaling (Figure 5f);
- Supine position with legs flexed. Cross roll left and right with hands at the nape of the neck (Figure 5g);
- Supine position. Flexion of the hips and pull the knees to the chest. Gently swing the trunk left and right (Figure 5h).By week three, exercises 6, 7, and 8 were replaced with mobility exercises as follows:
- Sitting position. Lateral trunk translation in kyphosis with arm extended laterally (Figure 5i);
- Sitting position with a stick in the hands held high over the head. The lateral inclination of the trunk (Figure 5l);
- Upright position placed beside a wall with the hand resting and the arm outstretched. With the other hand, push the pelvis towards the wall (Figure 5m).
2.6. Changes in Therapeutic Intervention
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gellhorn, A.C.; Katz, J.N.; Suri, P. Osteoarthritis of the spine: The facet joints. Nat. Rev. Rheumatol. 2013, 9, 216–224. [Google Scholar] [CrossRef] [Green Version]
- Goode, A.P.; Cleveland, R.J.; Schwartz, T.A.; Nelson, A.E.; Kraus, V.B.; Hillstrom, H.J.; Hannan, M.T.; Flowers, P.; Renner, J.B.; Jordan, J.M.; et al. Relationship of joint hypermobility with low Back pain and lumbar spine osteoarthritis. BMC Musculoskelet. Disord. 2019, 20, 158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DePalma, M.J.; Ketchum, J.M.; Saullo, T. What is the source of chronic low back pain and does age play a role? Pain Med. 2011, 12, 224–233. [Google Scholar] [CrossRef] [Green Version]
- Laplante, B.L.; DePalma, M.J. Spine osteoarthritis. Pm & R 2012, 4 (Suppl. S5), S28–S36. [Google Scholar]
- Hoy, D.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Bain, C.; Williams, G.; Smith, E.; Vos, T.; Barendregt, J.; et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boussios, S.; Cooke, D.; Hayward, C.; Kanellos, F.S.; Tsiouris, A.K.; Chatziantoniou, A.A.; Zakynthinakis-Kyriakou, N.; Karathanasi, A. Metastatic Spinal Cord Compression: Unraveling the Diagnostic and Therapeutic Challenges. Anticancer Res. 2018, 38, 4987–4997. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leonardi, R.; Rusu, M.C.; Loreto, F.; Loreto, C.; Musumeci, G. Immunolocalization and expression of lubricin in the bilaminar zone of the human temporomandibular joint disc. Acta Histochem. 2012, 114, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Loreto, C.; Musumeci, G.; Leonardi, R. Chondrocyte-like apoptosis in temporomandibular joint disc internal derangement as a repair-limiting mechanism. An in vivo study. Histol. Histopathol. 2009, 24, 293–298. [Google Scholar]
- Kuisma, M.; Karppinen, J.; Haapea, M.; Niinimäki, J.; Ojala, R.; Heliövaara, M.; Korpelainen, R.; Kaikkonen, K.; Taimela, S.; Natri, A.; et al. Are the determinants of vertebral endplate changes and severe disc degeneration in the lumbar spine the same? A magnetic resonance imaging study in middle-aged male workers. BMC Musculoskelet. Disord. 2008, 9, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCann, M.R.; Veras, M.A.; Yeung, C.; Lalli, G.; Patel, P.; Leitch, K.M.; Holdsworth, D.W.; Dixon, S.J.; Séguin, C.A. Whole-body vibration of mice induces progressive degeneration of intervertebral discs associated with increased expression of Il-1β and multiple matrix degrading enzymes. Osteoarthr. Cartil. 2017, 25, 779–789. [Google Scholar] [CrossRef] [Green Version]
- Khanna, A.; Bagouri, E.O.; Gougoulias, N.; Maffulli, N. Sport injuries in enduro riders: A review of literature. Muscles Ligaments Tendons J. 2015, 5, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Colburn, N.T.; Meyer, R.D. Sports Injury or trauma? Injuries of the competition off-road motorcyclist. Injury 2003, 34, 207–214. [Google Scholar] [CrossRef]
- Sabeti-Aschraf, M.; Serek, M.; Pachtner, T.; Auner, K.; Machinek, M.; Geisler, M.; Goll, A. The Enduro motorcyclist's wrist and other overuse injuries in competitive Enduro motorcyclists: A prospective study. Scand. J. Med. Sci. Sports 2008, 18, 582–590. [Google Scholar] [CrossRef]
- Borzì, F.; Szychlinska, M.A.; Di Rosa, M.; Musumeci, G. A Short Overview of the Effects of Kinesio Taping for Postural Spine Curvature Disorders. J. Funct. Morphol. Kinesiol. 2018, 3, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castrogiovanni, P.; Di Giunta, A.; Guglielmino, C.; Roggio, F.; Romeo, D.; Fidone, F.; Imbesi, R.; Loreto, C.; Castorina, S.; Musumeci, G. The Effects of Exercise and Kinesio Tape on Physical Limitations in Patients with Knee Osteoarthritis. J. Funct. Morphol. Kinesiol. 2016, 1, 355–368. [Google Scholar] [CrossRef] [Green Version]
- Altman, R.D. Osteoarthritis in the Elderly Population. In Geriatric Rheumatology: A Comprehensive Approach; Nakasato, Y., Yung, R.L., Eds.; Springer: New York, NY, USA, 2011; pp. 187–196. [Google Scholar]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [Green Version]
- Andreoni, G.; Negrini, S.; Ciavarro, G.L.; Santambrogio, G.C. ZooMS: A non invasive analysis of global and metameric movement of the lumbar spine. Eur. Medicophys. 2005, 41, 7–16. [Google Scholar]
- Ségui, Y.; Ramírez-Moreno, J. Global physiotherapy approach to thoracolumbar junction syndrome. A case report. J. Bodyw. Mov. Ther. 2021, 25, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Don, R.; Capodaglio, P.; Cimolin, V.; Benedetti, M.G.; D'Osualdo, F.; Frigo, C.; Vismara, L.; Negrini, S. Instrumental measures of spinal function: Is it worth? A state-of-the art from a clinical perspective. Eur. J. Phys. Rehabil. Med. 2012, 48, 255–273. [Google Scholar] [PubMed]
- Oliveira, C.B.; Maher, C.G.; Pinto, R.Z.; Traeger, A.C.; Lin, C.C.; Chenot, J.F.; van Tulder, M.; Koes, B.W. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur. Spine J. 2018, 27, 2791–2803. [Google Scholar] [CrossRef] [Green Version]
- Negrini, S.; Fusco, C.; Zaina, F.; Negrini, A. Scoliosis manager for medical doctors: A new Internet free tool to enhance medical approach to scoliosis worldwide. Scoliosis 2010, 5, O42. [Google Scholar] [CrossRef] [Green Version]
- Scoliosis Manager. Available online: www.scoliosismanager.it (accessed on 24 May 2021).
- Heo, M.Y.; Kim, K.; Hur, B.Y.; Nam, C.W. The effect of lumbar stabilization exercises and thoracic mobilization and exercises on chronic low back pain patients. J. Phys. Ther. Sci. 2015, 27, 3843–3846. [Google Scholar] [CrossRef] [Green Version]
- Parveen, A.; Nuhmani, S.; Hussain, M.E.; Khan, M.H. Effect of lumbar stabilization exercises and thoracic mobilization with strengthening exercises on pain level, thoracic kyphosis, and functional disability in chronic low back pain. J. Complement. Integr. Med. 2020, 18, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Alfuth, M.; Cornely, D. Chronic low back pain: Comparison of mobilization and core stability exercises. Orthopade 2016, 45, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Goode, A.P.; Carey, T.S.; Jordan, J.M. Low back pain and lumbar spine osteoarthritis: How are they related? Curr. Rheumatol. Rep. 2013, 15, 305. [Google Scholar] [CrossRef] [Green Version]
- Spahn, G.; Lipfert, J.U.; Maurer, C.; Hartmann, B.; Schiele, R.; Klemm, H.T.; Grifka, J.; Hofmann, G.O. Risk factors for cartilage damage and osteoarthritis of the elbow joint: Case-control study and systematic literature review. Arch. Orthop. Trauma Surg. 2017, 137, 557–566. [Google Scholar] [CrossRef] [PubMed]
- McCann, M.R.; Yeung, C.; Pest, M.A.; Ratneswaran, A.; Pollmann, S.I.; Holdsworth, D.W.; Beier, F.; Dixon, S.J.; Séguin, C.A. Whole-body vibration of mice induces articular cartilage degeneration with minimal changes in subchondral bone. Osteoarthr. Cartil. 2017, 25, 770–778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musumeci, G. The Effect of Mechanical Loading on Articular Cartilage. J. Funct. Morphol. Kinesiol. 2016, 1, 154–161. [Google Scholar] [CrossRef] [Green Version]
- Musumeci, G. The Use of Vibration as Physical Exercise and Therapy. J. Funct. Morphol. Kinesiol. 2017, 2, 17. [Google Scholar] [CrossRef] [Green Version]
- Guglielmino, C.; Musumeci, G. Early elbow osteoarthritis in competitive enduro motorcyclist. Scand. J. Med. Sci. Sports 2020, 30, 1287–1290. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-C.; Chen, W.-C.; Liu, Y.-P.; Chen, C.-Y.; Pan, Y.-T. Whole-body vibration exposure experienced by motorcycle riders—An evaluation according to ISO 2631–1 and ISO 2631–5 standards. Int. J. Ind. Ergon. 2009, 39, 708–718. [Google Scholar] [CrossRef]
- Chen, H.-C.; Pan, Y.-T. Whole-Body Vibration Exposure in Urban Motorcycle Riders. In Proceedings of the Institute of Industrial Engineers Asian Conference Singapore; Springer: New York, NY, USA; Singapore; pp. 975–983.
- Shivakumara, B.S.; Sridhar, V. Study of vibration and its effect on health of the motorcycle rider. Online J. Health All. Sci. 2010, 9, 9. [Google Scholar]
- Tian, W.; Lv, Y.; Liu, Y.; Xiao, B.; Han, X. The high prevalence of symptomatic degenerative lumbar osteoarthritis in Chinese adults: A population-based study. Spine 2014, 39, 1301–1310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patterson, F.; Miralami, R.; Tansey, K.E.; Prabhu, R.K.; Priddy, L.B. Deleterious effects of whole-body vibration on the spine: A review of in vivo, ex vivo, and in vitro models. Anim. Models Experim. Med. 2021, 4, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Ayari, H.; Thomas, M.; Doré, S.; Serrus, O. Evaluation of lumbar vertebra injury risk to the seated human body when exposed to vertical vibration. J. Sound Vibrat. 2009, 321, 454–470. [Google Scholar] [CrossRef]
- Cerciello, S.; Rossi, S.; Visonà, E.; Corona, K.; Oliva, F. Clinical applications of vibration therapy in orthopaedic practice. Muscles Ligam. Tend. J. 2016, 6, 147–156. [Google Scholar] [CrossRef]
- Sanna, I.; Pinna, V.; Milia, R.; Roberto, S.; Olla, S.; Mulliri, G.; Crisafulli, A. Hemodynamic Responses during Enduro-Motorcycling Performance. Front. Physiol. 2017, 8, 1062. [Google Scholar] [CrossRef] [Green Version]
- Gobbi, A.W.; Francisco, R.A.; Tuy, B.; Kvitne, R.S. Physiological characteristics of top level off-road motorcyclists. Br. J. Sports Med. 2005, 39, 927–931. [Google Scholar] [CrossRef] [Green Version]
- Williams, S.; Whatman, C.; Hume, P.A.; Sheerin, K. Kinesio taping in treatment and prevention of sports injuries: A meta-analysis of the evidence for its effectiveness. Sports Med. 2012, 42, 153–164. [Google Scholar] [CrossRef] [Green Version]
- Mostafavifar, M.; Wertz, J.; Borchers, J. A systematic review of the effectiveness of kinesio taping for musculoskeletal injury. Phys. Sportsmed. 2012, 40, 33–40. [Google Scholar] [CrossRef] [Green Version]
- Parreira Pdo, C.; Costa Lda, C.; Hespanhol, L.C., Jr.; Lopes, A.D.; Costa, L.O. Current evidence does not support the use of Kinesio Taping in clinical practice: A systematic review. J. Physiother. 2014, 60, 31–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cai, C.; Au, I.P.; An, W.; Cheung, R.T. Facilitatory and inhibitory effects of Kinesio tape: Fact or fad? J. Sci. Med. Sport 2016, 19, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Lu, Z.; Li, X.; Chen, R.; Guo, C. Kinesio taping improves pain and function in patients with knee osteoarthritis: A meta-analysis of randomized controlled trials. Int. J. Surg. 2018, 59, 27–35. [Google Scholar] [CrossRef]
- Montalvo, A.M.; Cara, E.L.; Myer, G.D. Effect of kinesiology taping on pain in individuals with musculoskeletal injuries: Systematic review and meta-analysis. Phys. Sportsmed. 2014, 42, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Azab, A.R.; Elnaggar, R.K.; Diab, R.H.; Moawd, S.A. Therapeutic value of kinesio taping in reducing lower back pain and improving back muscle endurance in adolescents with hemophilia. J. Musculoskelet. Neuronal. Interact. 2020, 20, 256–264. [Google Scholar]
- Wang, D.; Wang, S.; Lu, K.; Sun, Y. Comparison of kinesio taping and sham taping in patients with chronic low back pain: A protocol of randomized controlled trial. Medicine 2020, 99, e23042. [Google Scholar] [CrossRef]
- Danazumi, M.S.; Ibrahim, S.U.; Yakasai, A.M.; Dermody, G.; Bello, B.; Kaka, B. A Comparison between the Effect of Combined Chain Exercises plus Kinesio Taping With Combined Chain Exercises Alone in Knee Osteoarthritis: A Randomized Clinical Trial. Am. J. Phys. Med. Rehabil. 2021, 100, 1070–1077. [Google Scholar] [CrossRef]
- Ghozy, S.; Dung, N.M.; Morra, M.E.; Morsy, S.; Elsayed, G.G.; Tran, L.; Minh, L.H.N.; Abbas, A.S.; Loc, T.T.H.; Hieu, T.H.; et al. Efficacy of kinesio taping in treatment of shoulder pain and disability: A systematic review and meta-analysis of randomised controlled trials. Physiotherapy 2020, 107, 176–188. [Google Scholar] [CrossRef]
- Toprak Celenay, S.; Mete, O.; Sari, A.; Ozer Kaya, D. A comparison of kinesio taping and classical massage in addition to cervical stabilization exercise in patients with chronic neck pain. Complement. Ther. Clin. Pract. 2021, 43, 101381. [Google Scholar] [CrossRef]
- Toprak Celenay, S.; Mete, O.; Akan, S.; Un Yildirim, N.; Erten, S. Comparison of the effects of stabilization exercise plus kinesio taping and stabilization exercise alone on pain and well-being in fibromyalgia. Complement. Ther. Clin. Pract. 2020, 38, 101076. [Google Scholar] [CrossRef]
- Ünlü Özkan, F.; Soylu Boy, F.N.; Erdem Kılıç, S.; Geler Külcü, D.; Biçer Özdemir, G.; Çağlıyan Hartevioğlu, H.; Akpınar, P.; Aktaş, İ. Clinical and radiological outcomes of kinesiotaping in patients with chronic neck pain: A double-blinded, randomized, placebo-controlled study. Turk. J. Phys. Med. Rehabil. 2020, 66, 459–467. [Google Scholar] [CrossRef]
- Luo, W.H.; Li, Y. Current Evidence Does Support the Use of KT to Treat Chronic Knee Pain in Short Term: A Systematic Review and Meta-Analysis. Pain Res. Manag. 2021, 2021, 5516389. [Google Scholar] [CrossRef]
- Hryvniak, D.; Frost, C.D. Spine Injury Prevention. Clin. Sports Med. 2021, 40, 429–444. [Google Scholar] [CrossRef]
- Peñalver-Barrios, M.L.; Lisón, J.F.; Ballester-Salvador, J.; Schmitt, J.; Ezzedinne-Angulo, A.; Arguisuelas, M.D.; Doménech, J. A novel (targeted) kinesio taping application on chronic low back pain: Randomized clinical trial. PLoS ONE 2021, 16, e0250686. [Google Scholar]
- Mengi, A.; Özdolap, Ş.; Köksal, T.; Köktürk, F.; Sarıkaya, S. Comparison of effectiveness of different kinesiological taping techniques in patients with chronic low back pain: A double-blind, randomized-controlled study. Turk. J. Phys. Med. Rehabil. 2020, 66, 252–261. [Google Scholar] [CrossRef]
- Paoloni, M.; Bernetti, A.; Fratocchi, G.; Mangone, M.; Parrinello, L.; Del Pilar Cooper, M.; Sesto, L.; Di Sante, L.; Santilli, V. Kinesio Taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. Eur. J. Phys. Rehabil. Med. 2011, 47, 237–244. [Google Scholar] [PubMed]
- Hayden, J.A.; van Tulder, M.W.; Malmivaara, A.; Koes, B.W. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst. Rev. 2005, 3, Cd000335. [Google Scholar] [CrossRef]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [Green Version]
- Vlaeyen, J.W.S.; Maher, C.G.; Wiech, K.; Van Zundert, J.; Meloto, C.B.; Diatchenko, L.; Battié, M.C.; Goossens, M.; Koes, B.; Linton, S.J. Low back pain. Nat. Rev. Dis. Primers 2018, 4, 52. [Google Scholar] [CrossRef] [PubMed]




| Week 1 | Week 2 | Week 3 | Week 4 | 3rd month | 6th month | |
|---|---|---|---|---|---|---|
| VAS scale | 8 | 6 | 4 | 2 | 1 | 1 |
| ROM flexion | 10° | 22° | 35° | 68° | 75° | 78° |
| ROM extension | 2° | 2° | 8° | 9° | 15° | 18° |
| ROM lateral inclination left | 17° | 20° | 36° | 55° | 63° | 67° |
| ROM lateral inclination right | 10° | 15° | 27° | 46° | 58° | 60° |
| Muscle force (kg) | 3.19 | 5.82 | 10.67 | 16.53 | 20.22 | 20.73 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roggio, F.; Trovato, B.; Ledda, C.; Rapisarda, V.; Musumeci, G. Kinesiological Treatment of Early Spine Osteoarthritis in a Motorcyclist. Int. J. Environ. Res. Public Health 2022, 19, 961. https://doi.org/10.3390/ijerph19020961
Roggio F, Trovato B, Ledda C, Rapisarda V, Musumeci G. Kinesiological Treatment of Early Spine Osteoarthritis in a Motorcyclist. International Journal of Environmental Research and Public Health. 2022; 19(2):961. https://doi.org/10.3390/ijerph19020961
Chicago/Turabian StyleRoggio, Federico, Bruno Trovato, Caterina Ledda, Venerando Rapisarda, and Giuseppe Musumeci. 2022. "Kinesiological Treatment of Early Spine Osteoarthritis in a Motorcyclist" International Journal of Environmental Research and Public Health 19, no. 2: 961. https://doi.org/10.3390/ijerph19020961










