Holistic Assessment of Factors Associated with Exhaustion, the Main Symptom of Burnout: A Meta-Analysis of Longitudinal Studies
Abstract
1. Introduction
Aims of the Study
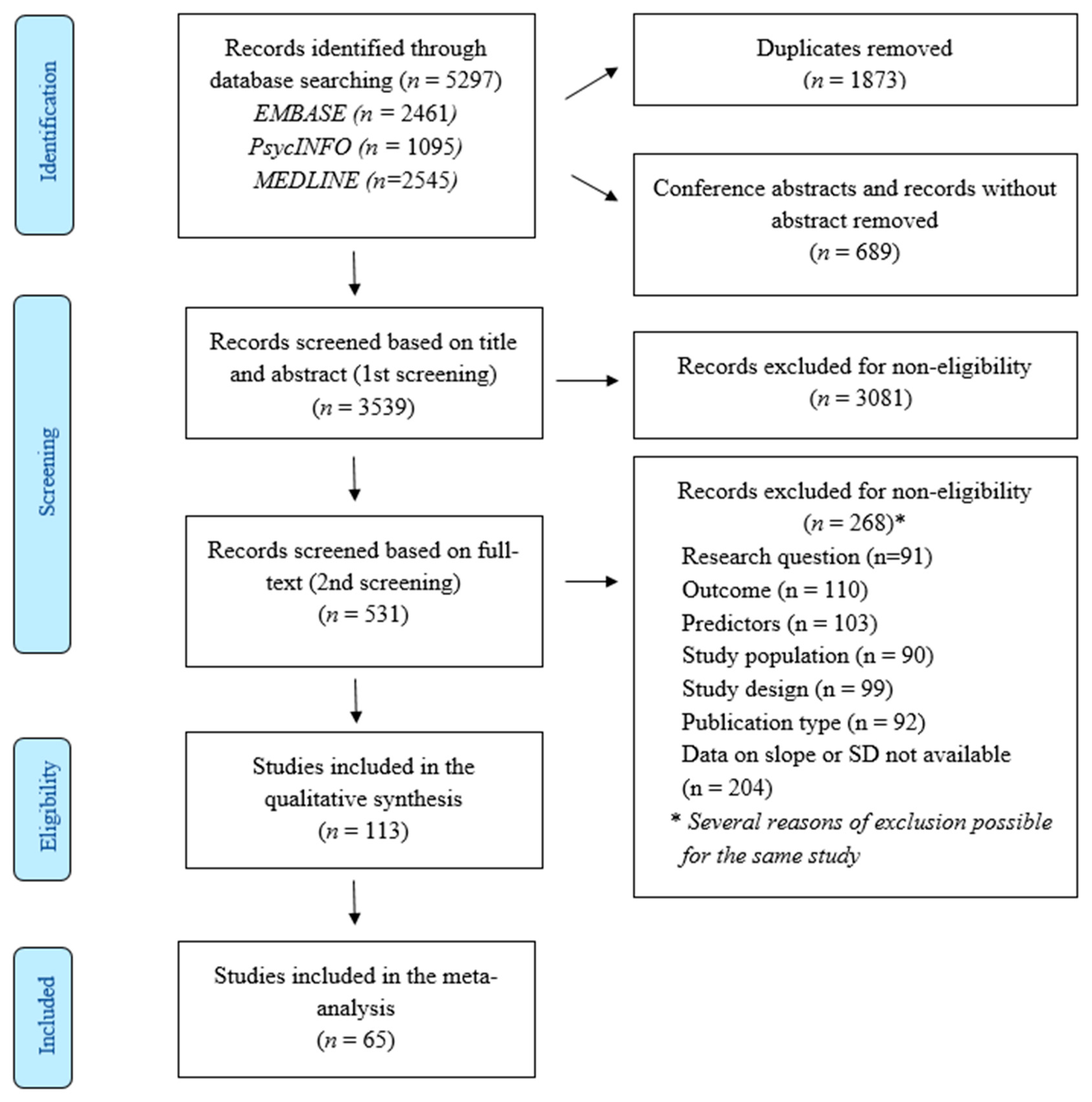
2. Materials and Methods
2.1. Protocol and Registration
2.2. Literature Search
2.3. Data Extraction
2.4. Meta-Analysis
2.5. Risk of Bias and Overall Quality of Evidence
3. Results
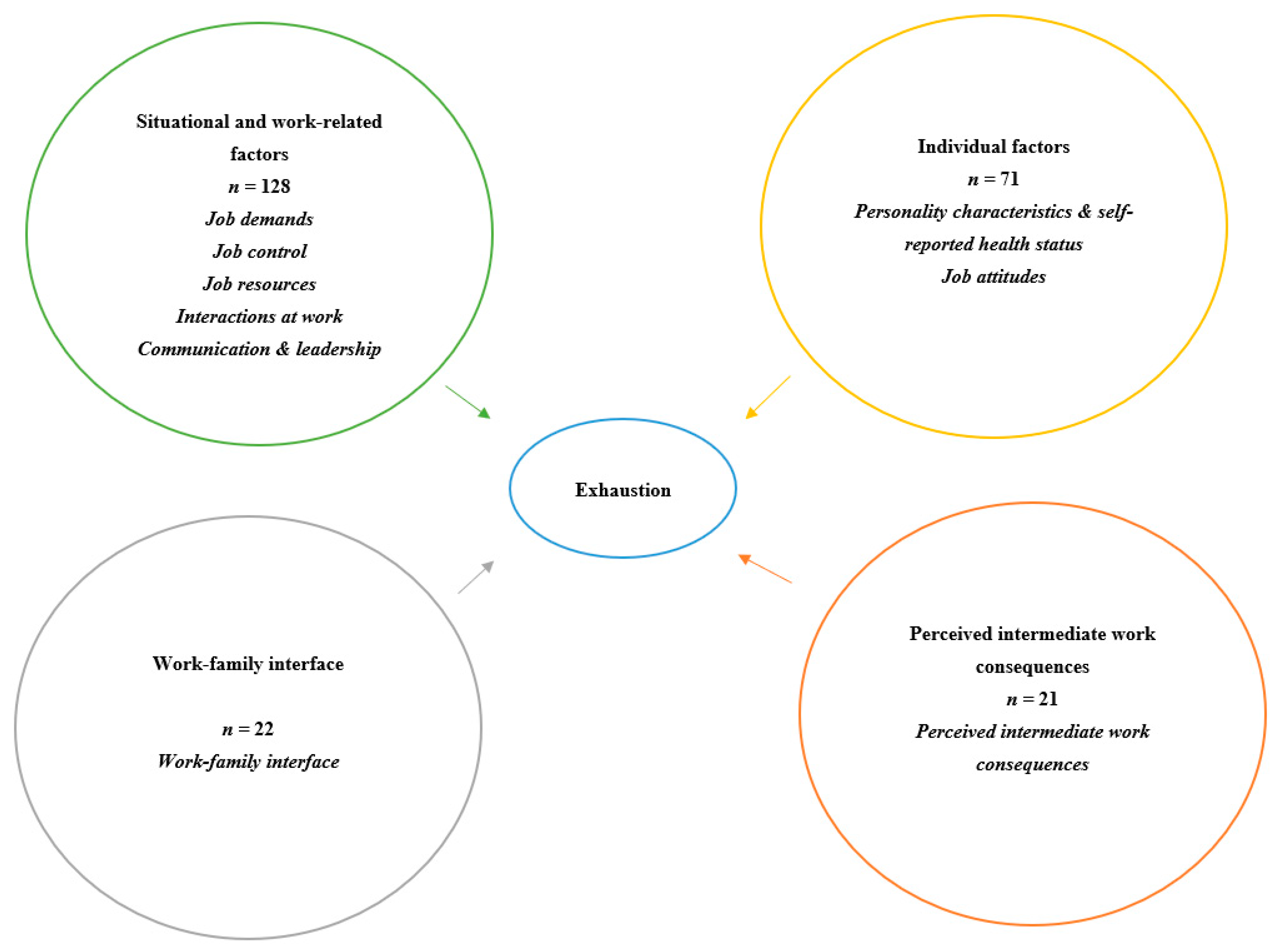
3.1. Included Studies
3.2. Meta-Analysis
3.3. Effect of the Follow-Up Length on the Observed Associations
3.4. Sensitivity Analysis and Additional Analyses
3.5. Publication Bias
4. Discussion
4.1. Main Findings
4.2. Defining and Measuring Exhaustion
4.3. Defining and Measuring Predictors of Occupational Burnout
4.4. The Latency of Occupational Burnout
4.5. Implications of the Findings
4.6. Conclusive Remarks
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Word Health Organization. Burn-Out an “Occupational Phenomenon”: International Classification of Diseases. Available online: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed on 28 May 2019).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Guseva Canu, I.; Marca, S.C.; Dell’Oro, F.; Balázs, Á.; Bergamaschi, E.; Besse, C.; Bianchi, R.; Bislimovska, J.; Koscec Bjelajac, A.; Bugge, M.; et al. Harmonized definition of occupational burnout: A systematic review, semantic analysis, and Delphi consensus in 29 countries. Scand. J. Work. Environ. Health 2021, 47, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Shirom, A.; Melamed, S. A comparison of the construct validity of two burnout measures in two groups of professionals. Int. J. Stress Manag. 2006, 13, 176–200. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Shoman, Y.; Marca, S.C.; Bianchi, R.; Godderis, L.; van der Molen, H.F.; Guseva Canu, I. Psychometric properties of burnout measures: A systematic review. Epidemiol. Psychiatry Sci. 2021, 30, e8. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E. The Measurement of Experienced Burnout. J. Occup. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Demerouti, E.; Demerouti, E.; Bakker, A.B.; Vardakou, I.; Kantas, A. The Convergent Validity of Two Burnout Instruments. Eur. J. Psychol. Assess. 2003, 19, 12–23. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef]
- Kisling, L.; Das, J.P. Prevention Strategies; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- West, C.P.; Dyrbye, L.N.; Erwin, P.J.; Shanafelt, T.D. Interventions to Prevent and Reduce Physician Burnout: A Systematic Review and Meta-analysis. Obstet. Gynecol. Surv. 2017, 72, 147–149. [Google Scholar] [CrossRef]
- Vargas, C.; Canadas, G.A.; Aguayo, R.; Fernandez, R.; de la Fuente, E.I. Which occupational risk factors are associated with burnout in nursing? A meta-analytic study. Int. J. Clin. Health Psychol. 2014, 14, 28–38. [Google Scholar] [CrossRef]
- Pradas-Hernandez, L.; Ariza, T.; Gomez-Urquiza, J.L.; Albendin-Garcia, L.; De la Fuente, E.I.; Canadas-De la Fuente, G.A. Prevalence of burnout in paediatric nurses: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0195039. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, K.; Neff, D.M.; Pitman, S. Burnout in mental health professionals: A systematic review and meta-analysis of prevalence and determinants. Eur. Psychiatry 2018, 53, 74–99. [Google Scholar] [CrossRef] [PubMed]
- Aronsson, G.; Theorell, T.; Grape, T.; Hammarstrom, A.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Traskman-Bendz, L.; Hall, C. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health 2017, 17, 264. [Google Scholar] [CrossRef] [PubMed]
- Alarcon, G.M. A meta-analysis of burnout with job demands, resources, and attitudes. J. Vocat. Behav. 2011, 79, 549–562. [Google Scholar] [CrossRef]
- Guthier, C.; Dormann, C.; Voelkle, M.C. Reciprocal Effects Between Job Stressors and Burnout: A Continuous Time Meta-Analysis of Longitudinal Studies. Psychol. Bull. 2020, 146, 1146–1173. [Google Scholar] [CrossRef]
- Chirico, F. Job stress models for burnout syndrome: A review. Ann. Istituto Super. Sanita 2016, 52, 443–456. [Google Scholar]
- Shoman, Y.; El May, E.; Marca, S.; Wild, P.; Bianchi, R.; Bugge, M.; Caglayan, C.; Cheptea, D.; Gnesi, M.; Godderis, L.; et al. Predictors of Occupational Burnout: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9188. [Google Scholar] [CrossRef]
- Seidler, A.; Thinschmidt, M.; Deckert, S.; Then, F.; Hegewald, J.; Nieuwenhuijsen, K.; Riedel-Heller, S.G. The role of psychosocial working conditions on burnout and its core component emotional exhaustion—A systematic review. J. Occup. Med. Toxicol. 2014, 9, 10. [Google Scholar] [CrossRef]
- Wang, M.; Liao, X.; Laden, F.; Spiegelman, D. Quantifying risk over the life course—Latency, age-related susceptibility, and other time-varying exposure metrics. Stat. Med. 2016, 35, 2283–2295. [Google Scholar] [CrossRef]
- Kuh, D.; Ben-Shlomo, Y.; Lynch, J.; Hallqvist, J.; Power, C. Life course epidemiology. J. Epidemiol. Community Health 2003, 57, 778–783. [Google Scholar] [CrossRef]
- Rothman, K. Epidemiology: An Introduction; Oxford University Press: Oxford, UK, 2002. [Google Scholar]
- Schaufeli, W.B.; Vandierendonck, D. A Cautionary Note About the Cross-National and Clinical Validity of Cutoff Points for the Maslach Burnout Inventory. Psychol. Rep. 1995, 76, 1083–1090. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef] [PubMed]
- White, F. Application of Disease Etiology and Natural History to Prevention in Primary Health Care: A Discourse. Med. Princ. Pract. 2020, 29, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Ahola, K.; Gould, R.; Virtanen, M.; Honkonen, T.; Aromaa, A.; Lonnqvist, J. Occupational burnout as a predictor of disability pension: A population-based cohort study. Occup. Environ. Med. 2009, 66, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Toppinen-Tanner, S.; Ojajarvi, A.; Vaananen, A.; Kalimo, R.; Jappinen, P. Burnout as a predictor of medically certified sick-leave absences and their diagnosed causes. Behav. Med. 2005, 31, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Borritz, M.; Rugulies, R.; Christensen, K.B.; Villadsen, E.; Kristensen, T.S. Burnout as a predictor of self-reported sickness absence among human service workers: Prospective findings from three year follow up of the PUMA study. Occup. Environ. Med. 2006, 63, 98–106. [Google Scholar] [CrossRef]
- Dekkers, O.M.; Vandenbroucke, J.P.; Cevallos, M.; Renehan, A.G.; Altman, D.G.; Egger, M. COSMOS-E: Guidance on conducting systematic reviews and meta-analyses of observational studies of etiology. PLoS Med. 2019, 16, e1002742. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Karasek, R. Control in the workplace and its health-related aspect. In Job Control and Worker Health; Sauter, S.L., Hurrell, J.J., Cooper, C.L., Eds.; Wiley: Chichester, UK, 1989; pp. 129–160. [Google Scholar]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Welz, T.; Doebler, P.; Pauly, M. Fisher transformation based confidence intervals of correlations in fixed- and random-effects meta-analysis. Br. J. Math. Stat. Psychol. 2021, 75, 12224. [Google Scholar] [CrossRef] [PubMed]
- Bishara, A.J.; Hittner, J.B. Confidence intervals for correlations when data are not normal. Behav. Res. Methods 2017, 49, 294–309. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Dancey, C.; Reidy, J. Statistics without Maths for Psychology; Pearson Education: London, UK, 2007. [Google Scholar]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M. Quantifying the risk of error when interpreting funnel plots. Syst. Rev. 2015, 4, 24. [Google Scholar] [CrossRef]
- Light, R.; Pillemer, D. Summing Up: The Science of Reviewing Research; Harvard University Press: Cambridge, UK, 1984. [Google Scholar]
- Pustejovsky, J.E.; Rodgers, M.A. Testing for funnel plot asymmetry of standardized mean differences. Res. Synth. Methods 2019, 10, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Sutton, A.; Abrams, K.; Jones, D.; Sheldon, T.; Song, F. Methods for Meta-Analysis in Medical Research; Wiley: Chichester, UK, 2000. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Shamliyan, T.; Kane, R.L.; Dickinson, S. A systematic review of tools used to assess the quality of observational studies that examine incidence or prevalence and risk factors for diseases. J. Clin. Epidemiol. 2010, 63, 1061–1070. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schunemann, H.J.; Group, G.W. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Westman, M.; Etzion, D.; Gattenio, E. International business travels and the work-family interface: A longitudinal study. J. Occup. Organ. Psychol. 2008, 81, 459–480. [Google Scholar] [CrossRef]
- Fritz, C.; Sonnentag, S. Recovery, well-being, and performance-related outcomes: The role of workload and vacation experiences. J. Appl. Psychol. 2006, 91, 936–945. [Google Scholar] [CrossRef]
- Fritz, C.; Sonnentag, S. Recovery, health, and job performance: Effects of weekend experiences. J. Occup. Health Psychol. 2005, 10, 187–199. [Google Scholar] [CrossRef]
- Spence Laschinger, H.K.; Finegan, J. Situational and dispositional predictors of nurse manager burnout: A time-lagged analysis. J. Nurs. Manag. 2008, 16, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Gelsema, T.I.; van der Doef, M.; Maes, S.; Janssen, M.; Akerboom, S.; Verhoeven, C. A longitudinal study of job stress in the nursing profession: Causes and consequences. J. Nurs. Manag. 2006, 14, 289–299. [Google Scholar] [CrossRef][Green Version]
- Travis, D.; Lizano, E.; Mor Barak, M. ‘I’m So Stressed!’: A Longitudinal Model of Stress, Burnout and Engagement among Social Workers in Child Welfare Settings. Br. J. Soc. Work 2015, 46, 1076–1095. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.; Osca, A.; Recio, P.; Urien, B.; Peiro, J.M. Work-family conflict, self-efficacy, and emotional exhaustion: A test of longitudinal effects. J. Work Organ. Psychol. 2015, 31, 147–154. [Google Scholar] [CrossRef]
- Lizano, E.L.; Barak, M.E.M. Workplace demands and resources as antecedents of job burnout among public child welfare workers: A longitudinal study. Child Youth Serv. Rev. 2012, 34, 1769–1776. [Google Scholar] [CrossRef]
- Langballe, E.; Innstrand, S.T.; Aasland, O.; Falkum, E. The Predictive Value of Individual Factors, Work-Related Factors, and Work-Home Interaction on Burnout in Female and Male Physicians: A Longitudinal Study. Stress Health 2011, 27, 73–87. [Google Scholar] [CrossRef]
- Sabitova, A.; McGranahan, R.; Altamore, F.; Jovanovic, N.; Windle, E.; Priebe, S. Indicators Associated with Job Morale among Physicians and Dentists in Low-Income and Middle-Income Countries: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e1913202. [Google Scholar] [CrossRef]
- Koutsimani, P.; Montgomery, A.; Georganta, K. The Relationship between Burnout, Depression, and Anxiety: A Systematic Review and Meta-Analysis. Front. Psychol. 2019, 10, 284. [Google Scholar] [CrossRef]
- Bianchi, R.; Verkuilen, J.; Schonfeld, I.S.; Hakanen, J.J.; Jansson-Frojmark, M.; Manzano-Garcia, G.; Laurent, E.; Meier, L.L. Is Burnout a Depressive Condition? A 14-Sample Meta-Analytic and Bifactor Analytic Study. Clin. Psychol. Sci. 2021, 9, 579–597. [Google Scholar] [CrossRef]
- Hillert, A.; Albrecht, A.; Voderholzer, U. The Burnout Phenomenon: A Résumé after More than 15,000 Scientific Publications. Front. Psychiatry 2020, 11, 519237. [Google Scholar] [CrossRef]
- Eurofound. Burnout in the Workplace: A Review of Data and Policy Responses in the EU; Publicatios Office of the European Union: Luxembourg, 2018. [Google Scholar]
- Bianchi, R.; Schonfeld, I.S.; Laurent, E. Is it Time to Consider the “Burnout Syndrome” A Distinct Illness? Front. Public Health 2015, 3, 158. [Google Scholar] [CrossRef] [PubMed]
- Engebretsen, K.M. Suffering without a medical diagnosis. A critical view on the biomedical attitudes towards persons suffering from burnout and the implications for medical care. J. Eval. Clin. Pract. 2018, 24, 1150–1157. [Google Scholar] [CrossRef] [PubMed]
- Danhof-Pont, M.B.; van Veen, T.; Zitman, F.G. Biomarkers in burnout: A systematic review. J. Psychosom. Res. 2011, 70, 505–524. [Google Scholar] [CrossRef] [PubMed]
- Bakusic, J.; Schaufeli, W.; Claes, S.; Godderis, L. 1496 Epigenetic perspective of burnout. BMJ 2018, 75, A574. [Google Scholar]
- Bakusic, J.; Schaufeli, W.; Claes, S.; Godderis, L. Stress, burnout and depression: A systematic review on DNA methylation mechanisms. J. Psychosom. Res. 2017, 92, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, S.; Patras, J.; Adolfsen, F.; Richardsen, A.M.; Martinussen, M. Using the Job Demands-Resources Model to Evaluate Work-Related Outcomes Among Norwegian Health Care Workers. Sage Open 2020, 10, 2158244020947436. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job Demands-Resources Theory: Taking Stock and Looking Forward. J. Occup. Health Psychol. 2017, 22, 273–285. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Taris, T.W. A critical review of the job demands-resources model: Implications for improving work and health. In Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach; Springer Science + Business Media: New York, NY, USA, 2014; pp. 43–68. [Google Scholar]
- Chen, W.; Zhang, G.; Tian, X.; Wang, L.; Luo, J. Rasch Analysis of Work-Family Conflict Scale Among Chinese Prison Police. Front. Psychol. 2021, 12, 37005. [Google Scholar] [CrossRef]
- Schaufeli, W.; Enzmann, D. The Burnout Companion to Study and Practice: A Critical Analysis; Taylor & Francis: London, UK, 1998. [Google Scholar]
- Guedes, D.; Gaspar, E. Burnout in a sample of Brazilian Physical Education professional. Rev. Bras. Educ. Fís. Esporte 2016, 30, 1011–1022. [Google Scholar]
- Arrighi, H.M.; Hertz-Picciotto, I. The evolving concept of the healthy worker survivor effect. Epidemiology 1994, 5, 189–196. [Google Scholar] [CrossRef]
- Zhang, X.J.; Song, Y.; Jiang, T.; Ding, N.; Shi, T.Y. Interventions to reduce burnout of physicians and nurses: An overview of systematic reviews and meta-analyses. Medicine 2020, 99, e20992. [Google Scholar] [CrossRef]
- Romppanen, J.; Haggman-Laitila, A. Interventions for nurses’ well-being at work: A quantitative systematic review. J. Adv. Nurs. 2017, 73, 1555–1569. [Google Scholar] [CrossRef]
- McDonald, G.; Jackson, D.; Wilkes, L.; Vickers, M.H. Personal resilience in nurses and midwives: Effects of a work-based educational intervention. Contemp. Nurse 2013, 45, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.F.; Luo, Y.H.; Lam, L.; Cross, W.; Plummer, V.; Zhang, J.P. Burnout and its association with resilience in nurses: A cross-sectional study. J. Clin. Nurs. 2018, 27, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Hawken, T.; Turner-Cobb, J.; Barnett, J. Coping and adjustment in caregivers: A systematic review. Health Psychol. Open 2018, 5, 055102918810659. [Google Scholar] [CrossRef] [PubMed]
- Karkkainen, R.; Saaranen, T.; Hiltunen, S.; Ryynanen, O.P.; Rasanen, K. Systematic review: Factors associated with return to work in burnout. Occup. Med. 2017, 67, 461–468. [Google Scholar] [CrossRef]
- Ahola, K.; Toppinen-Tanner, S.; Seppänen, J. Interventions to alleviate burnout symptoms and to support return to work among employees with burnout: Systematic review and meta-analysis. Burn. Res. 2017, 4, 1–11. [Google Scholar] [CrossRef]
- Deligkaris, P.; Panagopoulou, E.; Montgomery, A.J.; Masoura, E. Job burnout and cognitive functioning: A systematic review. Work Stress 2014, 28, 107–123. [Google Scholar]
- Van Dijk, D.M.; van Rhenen, W.; Murre, J.M.J.; Verwijk, E. Cognitive functioning, sleep quality, and work performance in non-clinical burnout: The role of working memory. PLoS ONE 2020, 15, e0231906. [Google Scholar] [CrossRef]
- Karasek, R.A. Job Demands, Job Decision Latitude, and Mental Strain—Implications for Job Redesign. Admin. Sci. Quart. 1979, 24, 285–308. [Google Scholar] [CrossRef]
- Karasek, R.; Theorell, T. Healthy Work, Stress, Productivity, and the Reconstruction of Working Life; Basic Books: New York, NY, USA, 1990. [Google Scholar]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef]
- Zwingmann, I.; Wolf, S.; Richter, P. Every light has its shadow: A longitudinal study of transformational leadership and leaders’ emotional exhaustion. J. Appl. Soc. Psychol. 2016, 46, 19–33. [Google Scholar] [CrossRef]
- Wirtz, N.; Rigotti, T.; Otto, K.; Loeb, C. What about the Leader? Crossover of Emotional Exhaustion and Work Engagement from Followers to Leaders. J. Occup. Health Psychol. 2017, 22, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Welp, A.; Meier, L.; Manser, T. The interplay between teamwork, clinicians’ emotional exhaustion, and clinician-rated patient safety: A longitudinal study. Crit. Care 2016, 20, 110. [Google Scholar] [CrossRef] [PubMed]
- Vegchel, N.v.; Jonge, J.d.; Söderfeldt, M.; Dormann, C.; Schaufeli, W. Quantitative Versus Emotional Demands Among Swedish Human Service Employees: Moderating Effects of Job Control and Social Support. Int. J. Stress Manag. 2004, 11, 21–40. [Google Scholar] [CrossRef]
- van der Ploeg, E.; Kleber, R.J. Acute and chronic job stressors among ambulance personnel: Predictors of health symptoms. Occup. Environ. Med. 2003, 60, 40–46. [Google Scholar] [CrossRef]
- Van de Ven, B.; van den Tooren, M.; Vlerick, P. Emotional Job Resources and Emotional Support Seeking as Moderators of the Relation Between Emotional Job Demands and Emotional Exhaustion: A Two-Wave Panel Study. J. Occup. Health Psychol. 2013, 18, 1–8. [Google Scholar] [CrossRef]
- Turgut, S.; Michel, A.; Rothenhofer, L.M.; Sonntag, K. Dispositional resistance to change and emotional exhaustion: Moderating effects at the work-unit level. Eur. J. Work Organ. Psychol. 2016, 25, 735–750. [Google Scholar] [CrossRef]
- Tonjes, B.; Dickhauser, O. Longitudinal effects of goal orientation on factors of occupational burden in the teacher profession. Z. Entwickl. Padagog. Psychol. 2009, 41, 79–86. [Google Scholar]
- Thompson, M.J.; Carlson, D.S.; Kacmar, K.M.; Vogel, R.M. The Cost of Being Ignored: Emotional Exhaustion in the Work and Family Domains. J. Appl. Psychol. 2020, 105, 186–195. [Google Scholar] [CrossRef]
- Taris, T.W.; Peeters, M.C.; Le Blanc, P.M.; Schreurs, P.J.; Schaufeli, W.B. From inequity to burnout: The role of job stress. J. Occup. Health Psychol. 2001, 6, 303–323. [Google Scholar] [CrossRef]
- Taris, T.W.; Kompier, M.A.J.; Geurts, S.A.E.; Houtman, I.L.D.; van den Heuvel, F.F.M. Professional efficacy, exhaustion, and work characteristics among police officers: A longitudinal test of the learning-related predictions of the demand-control model. J. Occup. Organ. Psychol. 2010, 83, 455–474. [Google Scholar] [CrossRef]
- Salanova, M.; Schaufeli, W.; Martínez, I.; Bresó, E. How obstacles and facilitators predict academic performance: The mediating role of study burnout and engagement. Anxiety Stress Coping 2009, 23, 53–70. [Google Scholar] [CrossRef] [PubMed]
- Richter, A.; Schraml, K.; Leineweber, C. Work-family conflict, emotional exhaustion and performance-based self-esteem: Reciprocal relationships. Int. Arch. Occup. Environ. Health 2015, 88, 103–112. [Google Scholar] [CrossRef]
- Ramarajan, L.; Barsade, S.; Burack, O. The influence of organizational respect on emotional exhaustion in the human services. J. Posit. Psychol. 2008, 3, 4–18. [Google Scholar] [CrossRef]
- Raimo, J.; LaVine, S.; Spielmann, K.; Akerman, M.; Friedman, K.A.; Katona, K.; Chaudhry, S. The Correlation of Stress in Residency with Future Stress and Burnout: A 10-Year Prospective Cohort Study. J. Grad. Med. Educ. 2018, 10, 524–531. [Google Scholar] [CrossRef]
- Pomaki, G.; Karoly, P.; Maes, S. Linking Goal Progress to Subjective Well-Being at Work: The Moderating Role of Goal-Related Self-Efficacy and Attainability. J. Occup. Health Psychol. 2009, 14, 206–218. [Google Scholar] [CrossRef]
- Pisanti, R.; van der Doef, M.; Maes, S.; Meier, L.L.; Lazzari, D.; Violani, C. How Changes in Psychosocial Job Characteristics Impact Burnout in Nurses: A Longitudinal Analysis. Front. Psychol. 2016, 7, 1082. [Google Scholar] [CrossRef]
- Philipp, A.; Schupbach, H. Longitudinal effects of emotional labour on emotional exhaustion and dedication of teachers. J. Occup. Health Psychol. 2010, 15, 494–504. [Google Scholar] [CrossRef]
- Petrou, P.; Demerouti, E.; Schaufeli, W.B. Job crafting in changing organizations: Antecedents and implications for exhaustion and performance. J. Occup. Health Psychol. 2015, 20, 470–480. [Google Scholar] [CrossRef]
- McManus, I.C.; Winder, B.C.; Gordon, D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet 2002, 359, 2089–2090. [Google Scholar] [CrossRef]
- Martinez-Inigo, D.; Totterdell, P. The mediating role of distributive justice perceptions in the relationship between emotion regulation and emotional exhaustion in healthcare workers. Work Stress 2016, 30, 26–45. [Google Scholar] [CrossRef]
- Makikangas, A.; Kinnunen, U. Psychosocial work stressors and well-being: Self-esteem and optimism as moderators in a one-year longitudinal sample. Pers. Indiv. Differ. 2003, 35, 537–557. [Google Scholar] [CrossRef]
- Lu, L.; Lin, H.Y.; Cooper, C.L. Unhealthy and present: Motives and consequences of the act of presenteeism among Taiwanese employees. J. Occup. Health Psychol. 2013, 18, 406–416. [Google Scholar] [CrossRef]
- Leiter, M.P.; Hakanen, J.J.; Ahola, K.; Toppinen-Tanner, S.; Koskinen, A.; Vaananen, A. Organizational predictors and health consequences of changes in burnout: A 12-year cohort study. J. Organ. Behav. 2013, 34, 959–973. [Google Scholar] [CrossRef]
- Lavigne, G.L.; Forest, J.; Crevier-Braud, L. Passion at work and burnout: A two-study test of the mediating role of flow experiences. Eur. J. Work Organ. Psychol. 2012, 21, 518–546. [Google Scholar] [CrossRef]
- Lapointe, É.; Vandenberghe, C.; Boudrias, J.-S. Psychological contract breach, affective commitment to organization and supervisor, and newcomer adjustment: A three-wave moderated mediation model. J. Vocat. Behav. 2013, 83, 528–538. [Google Scholar] [CrossRef]
- Kubicek, B.; Korunka, C.; Tement, S. Too much job control? Two studies on curvilinear relations between job control and eldercare workers’ well-being. Int. J. Nurs. Stud. 2014, 51, 1644–1653. [Google Scholar] [CrossRef]
- Kubicek, B.; Korunka, C. Does job complexity mitigate the negative effect of emotion-rule dissonance on employee burnout? Work Stress 2015, 29, 379–400. [Google Scholar] [CrossRef]
- Korunka, C.; Kubicek, B.; Paskvan, M.; Ulferts, H. Changes in work intensification and intensified learning: Challenge or hindrance demands? J. Manag. Psychol. 2015, 30, 786–800. [Google Scholar] [CrossRef]
- Konze, A.-K.; Rivkin, W.; Schmidt, K.-H. Is Job Control a Double-Edged Sword? A Cross-Lagged Panel Study on the Interplay of QuantitativeWorkload, Emotional Dissonance, and Job Control on Emotional Exhaustion. Int. J. Environ. Res. Public Health 2017, 14, 1608. [Google Scholar] [CrossRef] [PubMed]
- Koch, A.K.; Adler, M. Emotional exhaustion and innovation in the workplace-a longitudinal study. Ind. Health 2018, 56, 524–538. [Google Scholar] [CrossRef] [PubMed]
- Knoll, M.; Hall, R.J.; Weigelt, O. A Longitudinal Study of the Relationships Between Four Differentially Motivated Forms of Employee Silence and Burnout. J. Occup. Health Psychol. 2019, 24, 572–589. [Google Scholar] [CrossRef]
- Jimenez, P.; Dunkl, A. The Buffering Effect of Workplace Resources on the Relationship between the Areas of Worklife and Burnout. Front. Psychol. 2017, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.; Knudsen, K. A two-wave cross-lagged study of business travel, work–family conflict, emotional exhaustion, and psychological health complaints. Eur. J. Work Organ. Psychol. 2016, 26, 1–12. [Google Scholar] [CrossRef]
- Innstrand, S.T.; Langballe, E.; Falkum, E. The longitudinal effects of individual vulnerability, organisational factors, and work–home interaction on burnout among male church ministers in Norway. Ment. Health Relig. Cult. 2011, 14, 241–257. [Google Scholar] [CrossRef]
- Tone Innstrand, S.; Melbye Langballe, E.; Arild Espnes, G.; Falkum, E.; Gjerl⊘w Aasland, O. Positive and negative work-family interaction and burnout: A longitudinal study of reciprocal relations. Work Stress 2008, 22, 1–15. [Google Scholar] [CrossRef]
- Idris, M.A.; Dollard, M.F.; Yulita. Psychosocial safety climate, emotional demands, burnout, and depression: A longitudinal multilevel study in the Malaysian private sector. J. Occup. Health Psychol. 2014, 19, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Hudek-Knezevic, J.; Maglica, B.K.; Krapic, N. Personality, organizational stress, and attitudes toward work as prospective predictors of professional burnout in hospital nurses. Croat. Med. J. 2011, 52, 538–549. [Google Scholar] [CrossRef]
- Huang, Y.H.; Chen, C.H.; Du, P.L.; Huang, I.C. The causal relationships between job characteristics, burnout, and psychological health: A two-wave panel study. Int. J. Hum. Resour. Man 2012, 23, 2108–2125. [Google Scholar] [CrossRef]
- Hornung, S.; Weigl, M.; Glaser, J.; Angerer, P. Is It So Bad or Am I So Tired? Cross-Lagged Relationships Between Job Stressors and Emotional Exhaustion of Hospital Physicians. J. Pers. Psychol. 2013, 12, 124–131. [Google Scholar]
- Hochwalder, J. A longitudinal study of the relationship between empowerment and burnout among registered and assistant nurses. Work 2008, 30, 343–352. [Google Scholar] [PubMed]
- Gregersen, S.; Vincent-Höper, S.; Nienhaus, A. The Relation Between Leadership and Perceived Well-Being: What Role Does Occupational Self-Efficacy Play? J. Leadersh. Stud. 2014, 8, 6–18. [Google Scholar] [CrossRef]
- Gonzalez-Morales, M.G.; Rodriguez, I.; Peiro, J.M. A Longitudinal Study of Coping and Gender in a Female-Dominated Occupation: Predicting Teachers’ Burnout. J. Occup. Health Psychol. 2010, 15, 29–44. [Google Scholar] [CrossRef]
- Gonzalez-Morales, M.G.; Peiro, J.M.; Rodriguez, I.; Bliese, P.D. Perceived collective burnout: A multilevel explanation of burnout. Anxiety Stress Coping 2012, 25, 43–61. [Google Scholar] [CrossRef]
- Goddard, R.; O’Brien, P.; Goddard, M. Work environment predictors of beginning teacher burnout. Brit. Educ. Res. J. 2006, 32, 857–874. [Google Scholar] [CrossRef]
- Gil-Monte, P.R.; Garcia-Juesas, J.A. Effects of Work Overloading and Self-Efficacy over the Burnout Syndrome: A Longitudinal Survey about Nursing. Rev. Mex. Psicol. 2008, 25, 329–337. [Google Scholar]
- Firoozabadi, A.; Uitdewilligen, S.; Zijlstra, F.R.H. Should You Switch Off or Stay Engaged? The Consequences of Thinking About Work on the Trajectory of Psychological Well-Being Over Time. J. Occup. Health Psychol. 2018, 23, 278–288. [Google Scholar] [CrossRef]
- Figueiredo-Ferraz, H.; Grau-Alberola, E.; Gil-Monte, P.R.; Garcia-Juesas, J.A. Burnout and job satisfaction among nursing professionals. Psicothema 2012, 24, 271–276. [Google Scholar]
- Fida, R.; Laschinger, H.K.S.; Leiter, M.P. The protective role of self-efficacy against workplace incivility and burnout in nursing: A time-lagged study. Health Care Manag. Rev. 2018, 43, 21–29. [Google Scholar] [CrossRef]
- Feuerhahn, N.; Bellingrath, S.; Kudielka, B.M. The Interplay of Matching and Non-Matching Job Demands and Resources on Emotional Exhaustion among Teachers. Appl. Psychol. Health Well-Being 2013, 5, 171–192. [Google Scholar] [CrossRef] [PubMed]
- Fernet, C.; Lavigne, G.L.; Vallerand, R.J.; Austin, S. Fired up with passion: Investigating how job autonomy and passion predict burnout at career start in teachers. Work Stress 2014, 28, 270–288. [Google Scholar]
- Fernet, C.; Gagne, M.; Austin, S. When does quality of relationships with coworkers predict burnout over time? The moderating role of work motivation. J. Organ. Behav. 2010, 31, 1163–1180. [Google Scholar] [CrossRef]
- Dubois, C.A.; Bentein, K.; Ben Mansour, J.; Gilbert, F.; Bedard, J.L. Why Some Employees Adopt or Resist Reorganization of Work Practices in Health Care: Associations between Perceived Loss of Resources, Burnout, and Attitudes to Change. Int. J. Environ. Res. Public Health 2014, 11, 187–201. [Google Scholar] [CrossRef]
- Chrisopoulos, S.; Dollard, M.F.; Winefield, A.H.; Dormann, C. Increasing the probability of finding an interaction in work stress research: A two-wave longitudinal test of the triple-match principle. J. Occup. Organ. Psychol. 2010, 83, 17–37. [Google Scholar] [CrossRef]
- Childs, J.H.; Stoeber, J. Do you want me to be perfect? Two longitudinal studies on socially prescribed perfectionism, stress and burnout in the workplace. Work Stress 2012, 26, 347–364. [Google Scholar] [CrossRef]
- Boamah, S.A.; Read, E.A.; Laschinger, H.K.S. Factors influencing new graduate nurse burnout development, job satisfaction and patient care quality: A time-lagged study. J. Adv. Nurs. 2017, 73, 1182–1195. [Google Scholar] [CrossRef]
- Birkeland, I.K.; Richardsen, A.M.; Dysvik, A. The Role of Passion and Support Perceptions in Changing Burnout: A Johnson-Neyman Approach. Int. J. Stress Manag. 2018, 25, 163–180. [Google Scholar] [CrossRef]
- Basinska, B.A.; Gruszczynska, E. Job-Related Emotions and Job Burnout among Civil Servants: Examining the Shape of the Relationship in Cross-Sectional and Longitudinal Models. Med. Pr. 2019, 70, 201–211. [Google Scholar] [CrossRef]
- Angelo, R.P.; Chambel, M.J. The Reciprocal Relationship between Work Characteristics and Employee Burnout and Engagement: A Longitudinal Study of Firefighters. Stress Health 2015, 31, 106–114. [Google Scholar] [CrossRef]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Causes and consequences of occupational stress in emergency nurses, a longitudinal study. J. Nurs. Manag. 2015, 23, 346–358. [Google Scholar] [CrossRef] [PubMed]
| Studied Predictor-Variables Grouped Per (Sub)Family | Number of Studies | Heterogeneity “I2 Estimate” | Summary Estimate of the Association with Exhaustion | 95% Confidence Interval | Overall Risk of Bias Results | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Quality of Evidence 1 |
|---|---|---|---|---|---|---|---|---|---|---|
| Job demands | 27 | 89.25% | 0.33 | 0.28–0.38 | ||||||
| Work and time demands | 8 | 91.40% | 0.33 | 0.22–0.43 | Low | No | Yes | Yes | No | Low |
| Cognitive demands | 3 | 89.74% | 0.13 | −0.05, 0.31 | Moderate | Yes | No | Yes | No | Very low |
| Physical demands | 2 | 0.00% | 0.25 | 0.17, 0.34 | Low | No | No | Yes | No | Moderate |
| Workload | 6 | 18.69% | 0.38 | 0.34–0.43 | Moderate | No | No | No | No | Moderate |
| Time pressure | 5 | 92.34% | 0.35 | 0.17–0.53 | Low | No | No | Yes | No | Moderate |
| Job demands (overall) | 2 | 13.55% | 0.35 | 0.23–0.48 | Moderate | No | No | Yes | No | Low |
| Emotional demands | 8 | 31.69% | 0.34 | 0.30–0.39 | Moderate | No | Yes | Yes | No | Very Low |
| Job control | 20 | 94.14% | −0.15 | −0.21, −0.09 | ||||||
| Job control | 8 | 76.78% | −0.23 | −0.30, −0.16 | Low | No | Yes | Yes | No | Low |
| Skill discretion | 3 | 0.00% | −0.05 | −0.08, −0.02 | High | No | Yes | Yes | No | Very low |
| Autonomy | 6 | 77.82% | −0.21 | −0.21, −0.11 | Moderate | Yes | Yes | Yes | No | Very low |
| Decision authority | 5 | 81.59% | −0.06 | −0.19, 0.06 | High | Yes | Yes | Yes | No | Very low |
| Flow experiences | 1 | NA | −0.40 | −0.51, −0.29 | High | NA | NA | NA | No | Very low |
| Lack of control | 2 | 38.44% | 0.17 | 0.07, 0.28 | Low | No | No | Yes | No | Moderate |
| Job resources | 11 | 97.22% | −0.07 | −0.23, 0.08 | ||||||
| Job resources | 6 | 97.75% | −0.12 | −0.47, 0.22 | Low | No | No | Yes | No | Moderate |
| Lack of job resources | 4 | 73.40% | 0.12 | 0.02, 0.23 | Moderate | No | No | Yes | No | Low |
| Reward | 3 | 83.64% | −0.32 | −0.51, −0.12 | Low | No | No | No | No | High |
| Lack of reward/inequity | 2 | 96.27% | 0.35 | −0.12, 0.82 | Low | No | No | Yes | No | Moderate |
| Material resources | 3 | 72.77% | −0.27 | −0.42, −0.13 | Low | No | No | Yes | No | Moderate |
| Interactions at work | 23 | 96.57% | −0.02 | −0.10, 0.07 | ||||||
| Social support | 12 | 89.24% | −0.18 | −0.27, −0.08 | Moderate | No | No | Yes | No | Low |
| Poor social climate | 5 | 79.37% | 0.24 | 0.12, 0.35 | Low | No | No | Yes | No | Moderate |
| Support from supervisor | 3 | 91.71% | −0.16 | −0.29, −0.03 | Low | No | Yes | Yes | No | Very low |
| Support from colleagues | 3 | 0.01% | −0.16 | −0.21, −0,12 | Low | No | Yes | Yes | No | Very low |
| Fairness/justice | 2 | 0.00% | −0.35 | −0.45, −0.25 | High | No | No | Yes | No | Very low |
| Lack of support from supervisor | 2 | 85.25% | 0.27 | 0.01, 0.52 | Low | No | No | Yes | No | Moderate |
| Lack of support from coworkers | 2 | 0.01% | 0.27 | 0.20, 0.35 | Low | No | No | Yes | No | Moderate |
| Conflict & interpersonal problems | 3 | 92.19% | 0.30 | 0.05, 0.55 | Moderate | No | No | No | No | Moderate |
| Communication & leadership | 12 | 93.09% | −0.13 | −0.24, −0.03 | ||||||
| Work agreements | 2 | 0.00% | −0.25 | −0.33, −0.16 | Low | No | No | Yes | No | Moderate |
| Communication/information flow | 4 | 94.05% | −0.09 | −0.30, 0.12 | Moderate | No | Yes | Yes | No | Low |
| Quality of social interactions at work | 3 | 20.20% | −0.27 | −0.34, −0.19 | Moderate | No | No | No | No | Low |
| Leadership | 3 | 90.31% | −0.07 | −0.31, 0.17 | Low | Yes | Yes | Yes | No | Very low |
| Role conflict | 1 | NA | 0.19 | 0.09, 0.29 | Moderate | NA | NA | Yes | No | Low |
| Personality characteristics & self-reported health status | 26 | 96.60% | −0.02 | −0.11, 0.07 | ||||||
| Unvalued trait/ characteristics | 3 | 90.29% | 0.32 | 0.07, 0.57 | High | No | Yes | Yes | No | Very low |
| Valued trait/ characteristics | 5 | 88.15% | −0.24 | −0.39, −0.09 | Moderate | Yes | No | Yes | No | Very low |
| Extraversion | 1 | NA | 0.13 | −0.05, 0.31 | Moderate | NA | NA | Yes | NA | Low |
| Conscientiousness | 1 | NA | −0.01 | −0.19, 0.17 | Moderate | NA | NA | Yes | NA | Low |
| Openness | 1 | NA | 0.03 | −0.15, 0.21 | Moderate | NA | NA | Yes | NA | Low |
| Self-efficacy | 10 | 70.20% | −0.19 | −0.25, −0.12 | Moderate | No | Yes | Yes | No | Very low |
| Maladaptive coping | 3 | 0.00% | 0.33 | 0.24, 0.42 | Moderate | No | Yes | Yes | No | Very low |
| Adaptive coping | 4 | 73.55% | −0.02 | −0.16, 0.11 | Moderate | Yes | Yes | Yes | No | Very low |
| Emotion-focused coping | 2 | 87.42% | −0.02 | −0.18, 0.14 | Moderate | Yes | No | Yes | No | Very low |
| Self-esteem | 2 | 83.22% | −0.33 | −0.53, −0.13 | Low | No | No | Yes | No | Moderate |
| Performance-based self-esteem | 3 | 45.52% | 0.24 | 0.20, 0.28 | High | No | No | Yes | No | Low |
| Self-reported health status (harmful) | 2 | 92.14% | 0.34 | 0.13, 0.55 | Moderate | No | No | Yes | No | Very low |
| Self-reported health status (protective) | 1 | NA | −0.33 | −0.46, −0.20 | High | NA | NA | Yes | NA | Very low |
| Job attitudes | 18 | 95.73% | 0.05 | −0.04, 0.13 | ||||||
| Positive job attitudes | 7 | 79.71% | −0.24 | −0.33, −0.15 | Moderate | Yes | Yes | Yes | No | Very low |
| Negative job attitudes | 6 | 79.93% | 0.25 | 0.17, 0.33 | Moderate | Yes | Yes | Yes | No | Very low |
| Intrinsically motivated behavior | 8 | 86.28% | −0.07 | −0.17, 0.03 | High | Yes | Yes | Yes | No | Very low |
| Extrinsically motivated behavior | 4 | 83.30% | 0.28 | 0.05, 0.51 | Moderate | No | No | Yes | No | Low |
| Avoidance motives | 2 | 54.33% | 0.20 | 0.03, 0.37 | High | No | Yes | Yes | No | Very low |
| Acquiescent silence | 1 | NA | 0.22 | 0.14, 0.30 | High | NA | NA | Yes | NA | Very low |
| Quiescent silence | 1 | NA | 0.26 | 0.18, 0.34 | High | NA | NA | Yes | NA | Very low |
| Prosocial silence | 1 | NA | 0.01 | −0.07, 0.09 | High | NA | NA | Yes | NA | Very low |
| Opportunistic silence | 1 | NA | 0.13 | 0.05, 0.21 | High | NA | NA | Yes | NA | Very low |
| Work-family interface | 11 | 98.35% | 0.13 | 0.02, 0.23 | ||||||
| Work-family conflict | 10 | 49.36% | 0.36 | 0.33, 0.39 | Moderate | No | Yes | No | No | Low |
| Family-work conflict | 3 | 0.00% | 0.20 | 0.17, 0.24 | High | No | Yes | Yes | No | Very low |
| Work-family facilitation | 3 | 71.24% | −0.11 | −0.19, −0.02 | High | No | No | Yes | No | Low |
| Family-work facilitation | 3 | 57.95% | −0.05 | −0.11, 0.02 | High | Yes | No | Yes | No | Low |
| Value congruency | 3 | 54.12% | −0.27 | −0.34,−0.20 | Moderate | Yes | No | Yes | No | Very low |
| Perceived intermediate work consequences | 16 | 95.04% | 0.19 | 0.09, 0.29 | ||||||
| Work stressors | 4 | 80.55% | 0.24 | 0.13, 0.35 | Low | No | No | Yes | No | Moderate |
| Stressful interactions with patients/students | 2 | 0.00% | 0.22 | 0.16, 0.28 | Low | No | No | Yes | No | Moderate |
| Job insecurity | 2 | 56.18% | 0.16 | 0.03, 0.30 | Low | No | No | Yes | No | Moderate |
| Impact of change | 2 | 90.29% | 0.26 | 0.08, 0.44 | Moderate | No | No | Yes | No | Low |
| Psychological/physical toll | 2 | 33.39% | 0.44 | 0.31, 0.56 | Moderate | No | Yes | No | No | Low |
| Stress from work | 3 | 93.06% | 0.26 | 0.06, 0.46 | Moderate | No | No | Yes | No | Low |
| Satisfaction | 3 | 75.43% | −0.29 | −0.47, −0.11 | High | No | No | Yes | No | Very low |
| Colleagues/team exhaustion | 2 | 88.04% | 0.27 | −0.10, 0.64 | Moderate | No | No | Yes | No | Low |
| Subfamily | Change in the Associations between Predictors and Exhaustion | Change in Follow-Up Length (Months) |
|---|---|---|
| Job demands | No change | 3–48 |
| Job control | 2-fold decrease | 6–12 |
| Job resources | 2-fold decrease 6-fold decrease | 6–12 12–36 |
| Interactions at work and occupational burnout | 4-fold decrease 4-fold decrease | 6–12 12–24 |
| Communication and leadership | 2-fold decrease | 3–18 |
| Personality characteristics and self-reported health status | No change | 3–48 |
| Job attitudes | 2-fold decrease | 3–12 |
| Work-life interface | 3-fold decrease | 6–36 |
| Perceived intermediate work consequences | No change | 6–120 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shoman, Y.; Rousson, V.; Bianchi, R.; Guseva Canu, I. Holistic Assessment of Factors Associated with Exhaustion, the Main Symptom of Burnout: A Meta-Analysis of Longitudinal Studies. Int. J. Environ. Res. Public Health 2022, 19, 13037. https://doi.org/10.3390/ijerph192013037
Shoman Y, Rousson V, Bianchi R, Guseva Canu I. Holistic Assessment of Factors Associated with Exhaustion, the Main Symptom of Burnout: A Meta-Analysis of Longitudinal Studies. International Journal of Environmental Research and Public Health. 2022; 19(20):13037. https://doi.org/10.3390/ijerph192013037
Chicago/Turabian StyleShoman, Yara, Valentin Rousson, Renzo Bianchi, and Irina Guseva Canu. 2022. "Holistic Assessment of Factors Associated with Exhaustion, the Main Symptom of Burnout: A Meta-Analysis of Longitudinal Studies" International Journal of Environmental Research and Public Health 19, no. 20: 13037. https://doi.org/10.3390/ijerph192013037
APA StyleShoman, Y., Rousson, V., Bianchi, R., & Guseva Canu, I. (2022). Holistic Assessment of Factors Associated with Exhaustion, the Main Symptom of Burnout: A Meta-Analysis of Longitudinal Studies. International Journal of Environmental Research and Public Health, 19(20), 13037. https://doi.org/10.3390/ijerph192013037







