The Need for Trauma Management Training and Evaluation on a Prehospital Setting
Abstract
:1. Introduction
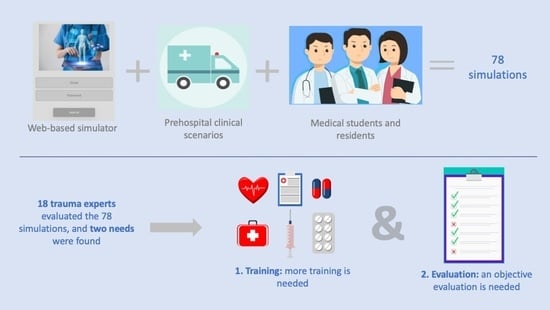
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Analysis
3. Results
4. Discussion
Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coalition for National Trauma Research. Trauma Statistics & Facts. 2021. Available online: https://www.nattrauma.org/trauma-statistics-facts/ (accessed on 18 October 2021).
- Trunkey, D.; Lim, R. Analysis of 425 consecutive trauma fatalities: An autopsy study. J. Am. Coll. Emerg. Physicians 1974, 3, 368–371. [Google Scholar] [CrossRef]
- Kleber, C.; Giesecke, M.; Tsokos, M.; Haas, N.; Schaser, K.; Stefan, P.; Buschmann, C. Overall distribution of trauma-related deaths in berlin 2010: Advancement or stagnation of german trauma management? World J. Surg. 2012, 36, 2125–2130. [Google Scholar] [CrossRef] [PubMed]
- Pang, J.; Civil, I.; Ng, A.; Adams, D.; Koelmeyer, T. Is the trimodal pattern of death after trauma a dated concept in the 21st century? Trauma deaths in auckland 2004. Injury 2008, 39, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Wessem, K.V.; McDougall, D.; Lee, K.; Lyons, T.; Balogh, Z. Epidemiology of traumatic deaths: Comprehensive population-based assessment. World J. Surg. 2009, 34, 158–163. [Google Scholar] [CrossRef]
- Rauf, R.; von Matthey, F.; Croenlein, M.; Zyskowski, M.; Griensven, M.V.; Biberthaler, P.; Lefering, R.; Huber-Wagner, S. Changes in the temporal distribution of in-hospital mortality in severely injured patients—An analysis of the traumaregister DGU. PLoS ONE 2019, 14, 20212095. [Google Scholar] [CrossRef] [Green Version]
- Lansink, K.; Gunning, A.; Leenen, L. Cause of death and time of death distribution of trauma patients in a level i trauma center in the Netherlands. Eur. J. Trauma Emerg. Surg. 2013, 39, 375–383. [Google Scholar] [CrossRef]
- American College of Surgeons. The Committee on Trauma. 2020. Available online: https://www.facs.org/Quality-Programs/Trauma (accessed on 1 December 2020).
- Mastoridis, S.; Shanmugaragah, K.; Kneebone, R. Undergraduate education in trauma medicine: The students’ verdict on current teaching. Med. Teach. 2011, 33, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Jouda, M.; Finn, Y. Training in polytrauma management in medical curricula: A scoping review. Med. Teach. 2020, 42, 1385–1393. [Google Scholar] [CrossRef]
- Long, A.; Lefebvre, C.; Masneri, D.; Mowery, N.; Chang, M.; Johnson, J.; Carter, J. The golden opportunity: Multidisciplinary simulation training improves trauma team effciency. J. Surg. Educ. 2019, 76, 1116–1121. [Google Scholar] [CrossRef] [PubMed]
- Minor, S.; Green, R.; Jessula, S. Crash testing the dummy: A review of in situ trauma simulation at a canadian tertiary centre. Can. J. Surg. 2019, 62, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Harrington, C.; Kavanagh, D.; Quinlan, J.; Ryan, D.; Dicker, P.; O’Keeffe, D.; Traynor, O.; Tierney, S. Development and evaluation of a trauma decision-making simulator in oculus virtual reality. Am. J. Surg. 2018, 215, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Wallin, C.; Meurling, L.; Hedman, L.; Hedegard, J.; Fellander-Tsai, L. Target-focused medical emergency team training using a human patient simulator: Effect on behaviour and attitude. Med. Educ. 2007, 41, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Mobrad, A.; Alnajjar, A.; Abuzeid, R.; Alhazmi, R.; Aldayes, A.; Villanueva, C. Evaluating the effect of the prehospital trauma life support (phtls) course on emergency medical services students’ knowledge. Biomed. Res. 2020, 31, 31–36. [Google Scholar]
- Häske, D.; Beckers, S.; Hofmann, M.; Lefering, R.; Gliwitzky, B.; Wölfl, C.; Grützner, P.; Stöckle, U.; Dieroff, M.; Münzberg, M. Quality of documentation as a surrogate marker for awareness and training effectiveness of phtls-courses. part of the prospective longitudinal mixed-methods epptc-trial. PLoS ONE 2017, 12, e0170004. [Google Scholar] [CrossRef]
- Ali, J.; Adam, R.; Josa, D.; Pierre, I.; Bedsaysie, H.; West, U.; Winn, J.; Ali, E.; Haynes, B. Effect of basic prehospital trauma life support program on cognitive and trauma management skills. World J. Surg. 1998, 22, 1192–1196. [Google Scholar] [CrossRef] [PubMed]
- Requena, A.; Jimenez, L.; Gomez, R.; del Arco, C. International trauma life support (itls) training through the spanish society of emergency medicines (semes): 10 years’ experience with the semes-itls program. Emergencias 2015, 27, 62–65. [Google Scholar]
- Campbell, J.; International Trauma Life Support (ITLS). International Trauma Life Support for Emergency Care Providers; Pearson Education: London, UK, 2013. [Google Scholar]
- PHTLS Courses. Naemt.org. Available online: https://www.naemt.org/education/phtls/phtls-courses (accessed on 30 August 2022).
- NAEMT—National Association of Emergency Medical Techinicians. PHTLS, Prehospital Trauma Life Support, 9th ed.; Jones & Barlett Learning: Burlington, MA, USA, 2018. [Google Scholar]
- Zonies, D.; Maier, R.; Civil, I.; Eid, A.; Geisler, B.; Guerrero, A.; Mock, C. Trauma and burn education: A global survey. World J. Surg. 2012, 36, 548–555. [Google Scholar] [CrossRef]
- Waterford, S.D.; Williams, M.; Siegert, C.J.; Fisichella, P.M.; Lebenthal, A. Trauma education in a state of emergency: A curriculum-based analysis. J. Surg. Res. 2015, 197, 236–239. [Google Scholar] [CrossRef]
- Hill, D.A. A model to teach trauma care to medical-students. Med. Teach. 1993, 15, 179–186. [Google Scholar] [CrossRef]
- Cuisinier, A.; Schilte, C.; Declety, P.; Picard, J.; Berger, K.; Bouzat, P.; Falcon, D.; Bosson, J.L.; Payen, J.F.; Albaladejo, P. A major trauma course based on posters, audio-guides and simulation improves the management skills of medical students: Evaluation via medical simulator. Anaesth. Crit. Care Pain Med. 2015, 34, 339–344. [Google Scholar] [CrossRef]
- Hill, K.A.; Johnson, E.D.; Lutomia, M.; Puyana, J.C.; Lee, K.K.; Oduor, P.R.; MacLeod, J.B. Implementing the Trauma Evaluation and Management (TEAM) Course in Kenya. J. Surg. Res. 2018, 232, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Borggreve, A.S.; Meijer, J.M.R.; Schreuder, H.W.R.; Ten Cate, O. Simulation-based trauma education for medical students: A review of literature. Med. Teach. 2017, 39, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Curtis, K.; Asha, S.; Unsworth, A.; Lam, M.; Goldsmith, H.; Langcake, M.; Dwyer, D. Chip: An early activation protocol for isolated blunt chest injury improves outcomes, a retrospective cohort study. Australas. Emerg. Nurs. J. 2016, 19, 127–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carrie, C.; Stecken, L.; Cayrol, E.; Cottenceau, V.; Petit, L.; Revel, P.; Biais, M.; Sztark, F. Bundle of care for blunt chest trauma patients improves analgesia but increases rates of intensive care unit admission: A retrospective case-control study. Anaesth. Crit. Care Pain Med. 2018, 37, 211–215. [Google Scholar] [CrossRef]
- Todd, S.; McNally, M.; Holcomb, J.; Kozar, R.; Kao, L.; Gonzalez, E.; Cocanour, C.; Vercruysse, G.; Lygas, M.; Brasseaux, B.; et al. A multidisciplinary clinical pathway decreases rib fracture-associated infectious morbidity and mortality in high-risk trauma patients. Am. J. Surg. 2006, 192, 806–811. [Google Scholar] [CrossRef]
- Nyland, B.; Spilman, S.; Halub, M.; Lamb, K.; Jackson, J.; Oetting, T.; Sahr, S. A preventative respiratory protocol to identify trauma subjects at risk for respiratory compromise on a general in-patient ward. Respir. Care 2016, 61, 1580–1587. [Google Scholar] [CrossRef]
- Sahr, S.; Webb, M.; Renner, C.; Sokol, R.; Swegle, J. Implementation of a rib fracture triage protocol in elderly trauma patients. J. Trauma Nurs. 2013, 20, 172–175. [Google Scholar] [CrossRef]
- Menditto, V.; Gabielli, B.; Marcosignori, M.; Screpante, F.; Pupita, G.; Polonara, S.; Salvi, A.; Raggettu, G.; Pomponio, G. A management of blunt thoracic trauma in an emergency department observation unit. J. Trauma Acute Care Surg. 2012, 72, 222–228. [Google Scholar] [CrossRef] [Green Version]
- Morrison, C.; Lee, T.; Wall, M.; Carrick, M. Use of a trauma service clinical pathway to improve patient outcomes for retained traumatic hemothorax. World J. Surg. 2009, 33, 1851–1856. [Google Scholar] [CrossRef]
- Frederickson, T.; Renner, C.; Swegle, J.; Sahr, S. The cumulative effect of multiple critical care protocols on length of stay in a geriatric trauma population. J. Intensive Care Med. 2012, 28, 58–66. [Google Scholar] [CrossRef]
- Dunham, C.; Bosse, M.; Clancy, T.; Cole, F.; Coles, M.; Knuth, T.; Luchette, F.; Ostrum, R.; Plaisier, B.; Poka, A.; et al. Practice management guidelines for the optimal timing of long-bone fracture stabilization in polytrauma patients: The east practice management guidelines work group. J. Trauma Inj. Infect. Crit. Care 2001, 50, 958–967. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobs, D.; Plaisier, B.; Barie, P.; Hammond, J.; Holevar, M.; Sinclair, K.; Scalea, T.; Wahl, W. Practice management guidelines for geriatric trauma: The east practice management guidelines work group. J. Trauma Inj. Infect. Crit. Care 2003, 54, 391–416. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.; Bin, J.; Sesperez, J.; Seger, M.; Sugrue, M. Clinical pathways—Can they be used in trauma care. An analysis of their ability to fit the patient. Injury 2001, 32, 525–532. [Google Scholar] [CrossRef]
- Baker, E.; Woolley, A.; Xyrichis, A.; Norton, C.; Hopkins, P.; Lee, G. How does the implementation of a patient pathway-based intervention in the acute care of blunt thoracic injury impact on patient outcomes? A systematic review of the literature. Injury 2020, 51, 1733–1743. [Google Scholar] [CrossRef]
- Unsworth, A.; Curtis, K.; Asha, S. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 17. [Google Scholar] [CrossRef] [Green Version]
- Kourouche, S.; Buckleya, T.; Munroe, B.; Curtis, K. Development of a blunt chest injury care bundle: An integrative review. Injury 2018, 49, 1008–1023. [Google Scholar] [CrossRef]
- Roberts, H. The effectiveness of implementing a care pathway for femoral neck fracture in older people: A prospective controlled before and after study. Age Ageing 2004, 33, 178–184. [Google Scholar] [CrossRef] [Green Version]
- Kwan, J. Effects of introducing an integrated care pathway in an acute stroke unit. Age Ageing 2004, 33, 362–367. [Google Scholar] [CrossRef] [Green Version]
- Vanhaecht, K.; de Witte, K.; Panella, M.; Sermeus, W. Do pathways lead to better organized care processes? J. Eval. Clin. Pract. 2009, 15, 782–788. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Jarrett, M.; McCrone, P.; Thornicroft, G. Facilitators and barriers to implementing clinical care pathways. BMC Health Serv. Res. 2010, 10, 182. [Google Scholar] [CrossRef] [Green Version]
- Hipp, R.; Abel, E.; Weber, R. A primer on clinical pathways. Hosp. Pharm. 2016, 51, 416–421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, J.; Howard, M.; Williams, J. Is attrition of advanced trauma life support acquired skills affected by trauma patient volume? Am. J. Surg. 2002, 183, 142–145. [Google Scholar] [CrossRef]
- Tsang, B.; McKee, J.; Engels, P.; Paton-gay, D.; Widder, S. Compliance to advanced trauma life support protocols in adult trauma patients in the acute setting. World J. Emerg. Surg. 2013, 8, 39–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santora, T.; Trooskin, S.; Blank, C.; Clarke, J.; Schinco, M. Video assessment of trauma response: Adherence to atls protocols. Am. J. Emerg. Med. 1996, 14, 564–569. [Google Scholar] [CrossRef]
- Spanjersberg, W.; Bergs, E.; Mushkudiani, N.; Klimek, M.; Schipper, I. Protocol compliance and time management in blunt trauma resuscitation. Emerg. Med. J. 2009, 26, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Rein, E.V.; der Sluijs, R.V.; Raaijmaakers, A.; Leenen, L.; Jeijl, M.V. Compliance to prehospital trauma triage protocols worldwide: A systematic review. Injury 2018, 49, 1373–1388. [Google Scholar] [CrossRef]
- Knudson, M.; Khaw, L.; Bullard, M.; Dicker, R.; Cohen, M.J.; Staudenmayer, K.; Sadjadi, J.; Howard, S.; Gaba, D.; Krummel, T. Trauma Training in Simulation: Translating Skills From SIM Time to Real Time. J. Trauma Inj. Infect. Amp Crit. Care 2008, 64, 255–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruesseler, M.; Weinlich, M.; Muller, M.; Byhahn, C.; Marzi, I.; Walcher, F. Simulation training improves ability to manage medical emergencies. Emerg. Med. J. 2010, 27, 734–738. [Google Scholar] [CrossRef]
- Cohen, D.; Sevdalis, N.; Taylor, D.; Kerr, K.; Heys, M.; Willett, K.; Batrick, N.; Darzi, A. Emergency preparedness in the 21st century: Training and preparation modules in virtual environments. Resuscitation 2013, 84, 78–84. [Google Scholar] [CrossRef]
- Cecilio-Fernandes, D.; Brandao, C.; de Oliveira, D.; Fernandez, G.; Tio, R. Additional simulation training: Does it affect students’ knowledge acquisition and retention? BMJ Simul. Technol. Enhanc. Learn. 2018, 5, 140–143. [Google Scholar] [CrossRef]
- Larraga-García, B.; Quintana-Díaz, M.; Guitérrez, Á. Simulation-Based Education in Trauma Management: A Scoping Review; Technical Report; UPM: Madrid, Spain, 2022. [Google Scholar]
- Abelsson, A.; Rystedt, I.; Suserud, B.; Lindwall, L. Mapping the use of simulation in prehospital care—A literature review. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 22. [Google Scholar] [CrossRef] [PubMed]





| Trauma Scenario 1 | Trauma Scenario 3 |
|---|---|
| 6.12 ± 1.93 | 6.25 ± 1.55 |
| 6.00 ± 2.01 | 7.06 ± 1.54 |
| 5.87 ± 2.15 | 5.75 ± 2.10 |
| 5.44 ± 1.64 | 5.75 ± 1.37 |
| 5.69 ± 1.94 | 5.81 ± 2.01 |
| 4.81 ± 1.18 | 4.25 ± 1.46 |
| 4.31 ± 1.18 | 3.56 ± 1.48 |
| 3.62 ± 1.59 | 4.31 ± 1.96 |
| 4.19 ± 1.63 | 4.44 ± 1.18 |
| 5.37 ± 1.55 | 5.19 ± 1.16 |
| 5.81 ± 1.44 | 4.31 ± 1.24 |
| 5.44 ± 1.22 | 0.81 ± 0.63 |
| 4.87 ± 1.69 | 2.50 ± 1.17 |
| 5.12 ± 1.43 | 2.56 ± 1.17 |
| 4.06 ± 1.59 | 2.67 ± 1.49 |
| 2.00 ± 0.91 | 3.80 ± 1.72 |
| 4.40 ± 2.24 | 4.30 ± 2.29 |
| 4.27 ± 1.72 | 4.47 ± 1.93 |
| 3.60 ± 2.12 | 4.60 ± 1.02 |
| 4.13 ± 1.77 | 4.37 ± 2.17 |
| 4.20 ± 1.55 | 3.47 ± 2.12 |
| 3.47 ± 1.93 | 4.13 ± 1.75 |
| 4.93 ± 1.65 | 4.80 ± 1.79 |
| 5.07 ± 1.92 | 3.67 ± 1.84 |
| 5.25 ± 2.11 | 3.30 ± 2.37 |
| 5.10 ± 1.86 | 4.83 ± 1.50 |
| 3.87 ± 1.77 | 4.17 ± 2.00 |
| 3.10 ± 1.53 | 3.80 ± 2.45 |
| 4.13 ± 1.66 | 3.73 ± 1.56 |
| 4.67 ± 1.81 | 3.53 ± 2.12 |
| 4.33 ± 1.92 | |
| 4.47 ± 1.83 | |
| 3.73 ± 1.69 | |
| 4.20 ± 1.87 | |
| 4.13 ± 1.99 | |
| 5.17 ± 1.58 | |
| 4.58± 1.71 | 4.21± 1.67 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Larraga-García, B.; Quintana-Díaz, M.; Gutiérrez, Á. The Need for Trauma Management Training and Evaluation on a Prehospital Setting. Int. J. Environ. Res. Public Health 2022, 19, 13188. https://doi.org/10.3390/ijerph192013188
Larraga-García B, Quintana-Díaz M, Gutiérrez Á. The Need for Trauma Management Training and Evaluation on a Prehospital Setting. International Journal of Environmental Research and Public Health. 2022; 19(20):13188. https://doi.org/10.3390/ijerph192013188
Chicago/Turabian StyleLarraga-García, Blanca, Manuel Quintana-Díaz, and Álvaro Gutiérrez. 2022. "The Need for Trauma Management Training and Evaluation on a Prehospital Setting" International Journal of Environmental Research and Public Health 19, no. 20: 13188. https://doi.org/10.3390/ijerph192013188