A Change Management Approach to Promoting and Endorsing Ergonomics within a Dental Setting
Abstract
1. Introduction
2. Materials and Methods
2.1. Embracing Ergonomic Interventions
- (i)
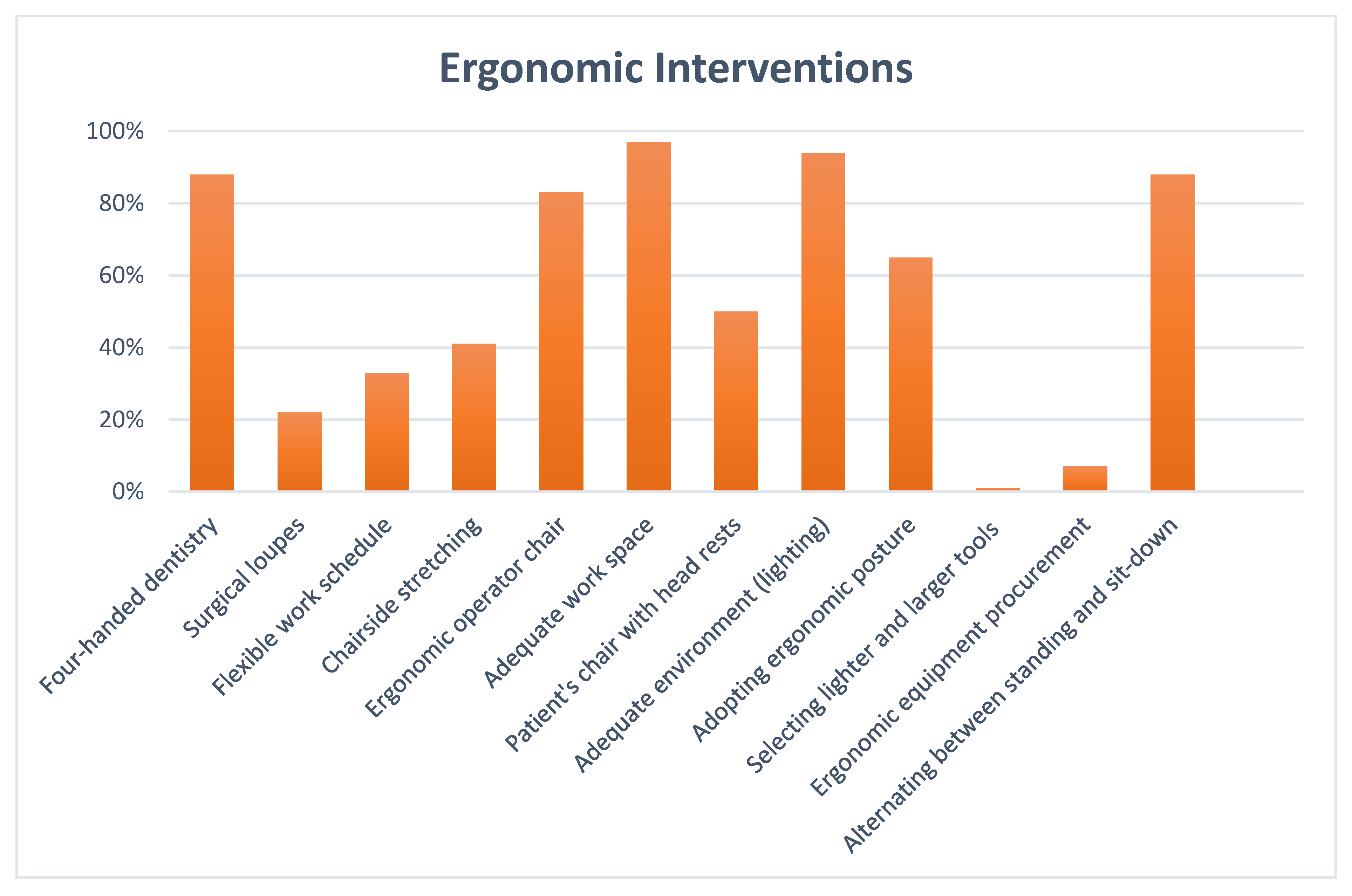
- A 12-item checklist was developed in the project’s first phase, based on evidence-based ergonomic interventions mentioned in the literature review [11]. The preliminary data from the checklists will serve as baseline information for capturing the ergonomic compliance witnessed. The participants responded to each item on the checklist with simple “yes/no” responses. The checklist is shown in Table 2.
- (ii)
- Comparing the number of sickness absence rates due to MSDs before and after implementing the ergonomic change was another evaluation method. Sick leave data were obtained from electronic medical records, and a prospective drop in sick leave rates due to MSDs was considered an ergonomic improvement [16].
2.1.1. Step 1. Create a Sense of Urgency
2.1.2. Step 2. Build an Ergonomic Coalition
2.1.3. Step 3. Form the Ergonomic Vision
2.1.4. Step 4. Communicate the Vision and the Initiatives
- Develop a user-friendly information brochure entitled “MSDs Prevention among Dental Personnel”. (See Appendix A).
- Identify available educational resources and construct training materials, such as videos, posters, and lectures.
- Take advantage of periodic staff meetings and education sessions, such as the dental journal club, to identify ergonomic behaviours.
- Design a fishbone diagram to help dental personnel understand the causes of musculoskeletal problems. (See Figure 1).
- Review various strategies or recommendations advocated to reduce ergonomic problems.
- Conduct research on ergonomic dental equipment to assist in the funding decisions required. Managers have a crucial role in supporting and enabling the adoption of ergonomic technologies.
- Look to others who have led similar ergonomic projects. For instance, the team reviewed a comparable ergonomic program proposed by the Occupational Safety and Health Administration (OSHA). The program included the following six elements: management leadership, hazard information and reporting, job hazard analysis and control, ergonomic awareness training, MSD management, and program evaluation [24].
- Encourage and involve others to suggest and discuss ergonomic improvement ideas.
- Create a Gantt chart to monitor project progress and document ergonomic progress and obstacles.
2.1.5. Step 5. Empower Staff to Act on the Vision and Remove Obstacles
2.1.6. Step 6. Create Quick Ergonomic Wins
2.1.7. Step 7. Build on the Ergonomic Change
2.1.8. Step 8. Anchor the Ergonomic Culture
3. Project Outcomes and Discussion
4. Conclusions
4.1. Research Limitations/Implications
4.2. Practical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef] [PubMed]
- Alzayani, M.K.; Salama, K.F.; Zafar, M. Work-related musculoskeletal disorders among dental staff in Armed Force Hospital in Dhahran, Saudi Arabia. Int. J. Prev. Med. 2021, 12, 119. [Google Scholar]
- Centers for Disease Control and Prevention. Work-Related Musculoskeletal Disorders & Ergonomics; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020. [Google Scholar]
- ZakerJafari, H.R.; YektaKooshali, M.H. Work-related musculoskeletal disorders in Iranian dentists: A systematic review and meta-analysis. Saf. Health Work. 2018, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Haas, Y.; Naser, A.; Haenel, J.; Maltry, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brüggmann, D.; et al. Prevalence of muscular skeletal disorders among qualified dental assistants. Int. J. Environ. Res. Public Health 2020, 17, 3490. [Google Scholar] [CrossRef] [PubMed]
- Geethika, S.; Sharada, N. Prevalence of musculoskeletal disorders among dental students: A questionnaire survey. Int. J. Soc. Rehabil. 2021, 6, 50. [Google Scholar]
- Gandham, A.; Boppana, N.K.; Vinnakota, N.R.; Burri, K.K.; Th, U.K.; Pallepati, A. Assessment of musculoskeletal disorders and associated risk factors among dentists in Rajahmundry City: A cross-sectional study. J. Indian Assoc. Public Health Dent. 2019, 17, 114. [Google Scholar] [CrossRef]
- Lietz, J.; Ulusoy, N.; Nienhaus, A. Prevention of musculoskeletal diseases and pain among dental professionals through ergonomic interventions: A systematic literature review. Int. J. Environ. Res. Public Health 2020, 17, 3482. [Google Scholar] [CrossRef]
- Deshmuk, R.C.; Gomes, S.R.; Acharya, S.S.; Khanapure, S.C. An overview of ergonomics in dentistry. Indian J. Oral Health Res. 2019, 5, 40. [Google Scholar]
- Tanzila, R.A.; Prameswarie, T.; Hartanti, M.D.; Denaneer, T. The Correlation between Position and Duration Use of Laptops with Musculoskeletal Disorders (MSDs). Mutiara Med. J. Kedokt. Dan Kesehat. 2021, 21, 79–85. [Google Scholar] [CrossRef]
- Roll, S.C.; Tung, K.D.; Chang, H.; Sehremelis, T.A.; Fukumura, Y.E.; Randolph, S.; Forrest, J.L. Prevention and rehabilitation of musculoskeletal disorders in oral health care professionals: A systematic review. J. Am. Dent. Assoc. 2019, 150, 489–502. [Google Scholar] [CrossRef] [PubMed]
- Schlussel, A.T.; Maykel, J.A. Ergonomics and musculoskeletal health of the surgeon. Clin. Colon Rectal Surg. 2019, 32, 424–434. [Google Scholar] [CrossRef]
- Emran, M. Ergonomics-follow and keep well. KYAMC J. 2020, 11, 57–58. [Google Scholar] [CrossRef]
- Doppalapudi, N.; Burugapalli, R.K. Benefits of utilization of magnification in dentistry: A review. Dent. Res. Oral Health 2020, 3, 121–128. [Google Scholar] [CrossRef]
- Anu, V.; Babu, A.S.; Kumar, P.M. Insights about dental ergonomics among dental students: The need of the hour to recommend dental ergonomics in academic curriculum. J. Adv. Oral Res. 2018, 9, 49–54. [Google Scholar] [CrossRef]
- Russo, F.; Papalia, G.F.; Vadalà, G.; Fontana, L.; Iavicoli, S.; Papalia, R.; Denaro, V. The effects of workplace interventions on low back pain in workers: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 12614. [Google Scholar] [CrossRef] [PubMed]
- Halkai, K.R.; Halkai, R.S.; Sulgante, S.; Sanadi, R.M.; Ara, S.A.; Zainab, H.; Kuriadom, S.T.; Munaga, S.; Chitumalla, R. Work-related musculoskeletal disorders among dentists and their prevention through ergonomic interventions-A systematic review. Int. J. Occup. Saf. Health 2022, 12, 125–139. [Google Scholar] [CrossRef]
- DM, E.H.; MA, M.; GO, W. Work Related Musculoskeletal Disorders among Egyptian Dentists Working at Faculty of Dentistry-Ain Shams University. Egypt. J. Occup. Med. 2019, 43, 413–428. [Google Scholar] [CrossRef]
- Small, A.; Gist, D.; Souza, D.; Dalton, J.; Magny-Normilus, C.; David, D. Using Kotter’s change model for implementing bedside handoff: A quality improvement project. J. Nurs. Care Qual. 2016, 31, 304–309. [Google Scholar] [CrossRef]
- Kotter, J.P. Leading Change; Harvard Business Press: Boston, MA, USA, 2012. [Google Scholar]
- Burden, M. Using a change model to reduce the risk of surgical site infection. Br. J. Nurs. 2016, 25, 949–955. [Google Scholar] [CrossRef]
- Averweg, U.R.; Kroeze, J.H. Probing some theoretical aspects of practitioner-based inquiry research in Information Systems. In Proceedings of the 2010 Annual Research Conference of the South African Institute of Computer Scientists and Information Technologists, Bela Bela, South Africa, 11–13 October 2010. [Google Scholar]
- Koshy, E.; Koshy, V.; Waterman, H. Action Research in Healthcare; Sage: Newcastle upon Tyne, UK, 2010. [Google Scholar]
- Herr, K.; Anderson, G.L. The action Research Dissertation: A Guide for Students and Faculty; Sage Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Chevalier, J.M.; Buckles, D.J. Participatory Action Research: Theory and Methods for Engaged Inquiry; Routledge: London, UK, 2019. [Google Scholar]
- Wentworth, D.K.; Behson, S.J.; Kelley, C.L. Implementing a new student evaluation of teaching system using the Kotter change model. Stud. High. Educ. 2020, 45, 511–523. [Google Scholar] [CrossRef]
- Cohen, D.S. The Heart of Change Field Guide: Tools and Tactics for Leading Change in Your Organization; Harvard Business Press: Boston, MA, USA, 2005. [Google Scholar]
- OSHA. Ergonomic Program; Final Rule, 65 Federal Register 68293; OSHA: Washington, DC, USA, 2000. [Google Scholar]
- Goffee, R.; Jones, G. Why Should Anyone be Lead by You: What It Takes to be an Authentic Leader; Harvard Business School Press: Boston, MA, USA, 2006. [Google Scholar]
- Taylor-Bianco, A.; Schermerhorn, J. Self-regulation, strategic leadership and paradox in organizational change. J. Organ. Change Manag. 2006, 19, 4. [Google Scholar] [CrossRef]
- Gifford, J.; Boury, D.; Finney, L.; Garrow, V.; Hatcher, C.; Meredith, M.; Rann, R. What makes change successful in the NHS. In A Review of Change Programmes in NHS South of England; Roffey Park Institute: Horsham, UK, 2012. [Google Scholar]
- Aziz, A.-M. A change management approach to improving safety and preventing needle stick injuries. J. Infect. Prev. 2017, 18, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Dable, R.A.; Wasnik, P.B.; Yeshwante, B.J.; Musani, S.I.; Patil, A.K.; Nagmode, S.N. Postural assessment of students evaluating the need of ergonomic seat and magnification in dentistry. J. Indian Prosthodont. Soc. 2014, 14, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Hallaj, S.; Razi, S.S.M. Design and evaluation of an arm support for prevention of msds in dentists. In Advances in Ergonomics in Design; Springer: Berlin/Heidelberg, Germany, 2016; pp. 265–275. [Google Scholar]
- Hayes, M.J.; Osmotherly, P.G.; Taylor, J.A.; Smith, D.R.; Ho, A. The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. Int. J. Dent. Hyg. 2014, 12, 174–179. [Google Scholar] [CrossRef]
- Maillet, J.P.; Millar, A.M.; Burke, J.M.; Maillet, M.A.; Maillet, W.A.; Neish, N.R. Effect of magnification loupes on dental hygiene student posture. J. Dent. Educ. 2008, 72, 33–44. [Google Scholar] [CrossRef]
- Lindegård, A.; Gustafsson, M.; Hansson, G.-Å. Effects of prismatic glasses including optometric correction on head and neck kinematics, perceived exertion and comfort during dental work in the oral cavity—A randomised controlled intervention. Appl. Ergon. 2012, 43, 246–253. [Google Scholar] [CrossRef]
- Lindegård, A.; Nordander, C.; Jacobsson, H.; Arvidsson, I. Opting to wear prismatic spectacles was associated with reduced neck pain in dental personnel: A longitudinal cohort study. BMC Musculoskelet. Disord. 2016, 17, 1–10. [Google Scholar] [CrossRef]
- Rempel, D.; Lee, D.L.; Dawson, K.; Loomer, P. The effects of periodontal curette handle weight and diameter on arm pain: A four-month randomized controlled trial. J. Am. Dent. Assoc. 2012, 143, 1105–1113. [Google Scholar] [CrossRef]
- Sachdeva, A.; Bhateja, S.; Arora, G. Ergonomics in Dentistry. OHASAJOURNAL 2021. Available online: https://www.ohasa.co.za/journals/2021-22-4.pdf#page=7 (accessed on 4 October 2022).
- Dehghan, N.; Aghilinejad, M.; Nassiri-Kashani, M.H.; Amiri, Z.; Talebi, A. The effect of a multifaceted ergonomic intervention program on reducing musculoskeletal disorders in dentists. Med. J. Islam. Repub. Iran 2016, 30, 472. [Google Scholar]
- Farrokhnia, T.; Rezai, M.; Vaziri, M.H.; Vaziri, F. Investigating the effect of educational intervention on musculoskeletal disorders in dentists. Middle East J. Fam. Med. 2018, 7, 307. [Google Scholar] [CrossRef]
- Koni, A.; Kufersin, M.; Ronchese, F.; Travan, M.; Cadenaro, M.; Filon, F.L. Approach to prevention of musculoskeletal symptoms in dental students: An interventional study. la Med. del Lav. 2018, 109, 276. [Google Scholar]
- Patel, D.P.K. Ergonomics and dentistry: A Brief Review. MAR Dent. Sci. 2021. Available online: https://www.medicalandresearch.com/assets/articles/documents/DOCUMENT_20210219114002.pdf (accessed on 4 October 2022).
- Díaz Caballero, A.J.; Palencia, I.P.G.; Cárdenas, S.D. Ergonomic factors that cause the presence of pain muscle in students of dentistry. Med. Oral Patol. Oral Cir. Bucal. 2010, 15, e906-11. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=5900107 (accessed on 4 October 2022). [CrossRef]
- Uppada, U.K.; Susmitha, M.; Hussaini, S.W.U.; Virk, I.; Yadav, T.G.; Khader, M.A. Ergonomics among dentists in the states of Telangana and Andhra Pradesh. Natl. J. Maxillofac. Surg. 2020, 11, 253. [Google Scholar] [CrossRef]
- Valachi, B. Little things can make a big difference. Dent. Today 2010, 29, 142–143. [Google Scholar]
- Goodchild, J. Musculoskeletal Disorders in Clinical Dentistry. Dent. Today 2019, 2. Available online: https://www.premierdentalco.com/wp-content/uploads/2019/04/DentistryToday_DrGoodchild.pdf (accessed on 4 October 2022).
- Calley, K. and K. Hodges, Automate your probing process. Dimensions of Dental Hygiene 2011, 9, 44–47. [Google Scholar]
- Harris, M.L.; Sentner, S.M.; Doucette, H.J.; Brillant, M.G.S. Musculoskeletal disorders among dental hygienists in Canada. Can. J. Dent. Hyg. 2020, 54, 61. [Google Scholar]
- Kushwaha, A.; Shivalingesh, K.K.; Gautam, N.; Kumar, P. Assessment of Knowledge Regarding Equipment Ergonomics among Interns and Final Year Dental Students in Bareilly. Oral Rehabil. 2021, 12, 14. [Google Scholar]
- Careau, N. Design of a Dental Mirror Mechanism; Worcester Polytechnic Institute: Worcester, MA, USA, 2009. [Google Scholar]
- Santucci, N.; Santucci, E.; Geissberger, M. A Simplified Clinical Technique for a Routine Indirect Restoration Impression on a Challenging Patient Using a Dry Field Illuminator. Oper. Dent. 2014, 39, 15–21. [Google Scholar] [CrossRef][Green Version]
- SW, S.; KP, L. Uptake and experience of visual magnification and illumination aids by Otago University Bachelor of Dental Surgery students’. N. Z. Dent. J. 2020, 116, 129–139. [Google Scholar]
- Kotter, J.P.; Cohen, D.S. The Heart of Change: Real-Life Stories of How People Change Their Organizations; Harvard Business Press: Boston, MA, USA, 2012. [Google Scholar]
- Kumar, M.; Pai, K.M.; Vineetha, R. Occupation-related musculoskeletal disorders among dental professionals. Med. Pharm. Rep. 2020, 93, 405. [Google Scholar] [CrossRef]
- Alnaser, M.Z.; Almaqsied, A.M.; Alshatti, S.A. Risk factors for work-related musculoskeletal disorders of dentists in Kuwait and the impact on health and economic status. Work 2021, 68, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Samat, D.R.B.A. Prevalence of Back Pain and Its Associated Factors among Government Dental Personnel in Kelantan. Ph.D. Thesis, Universiti Sains Malaysia, Penang, Malaysia, 2011. [Google Scholar]
- Yasobant, S.; Mohanty, S. Musculoskeletal disorders as a public health concern in India: A call for action. Physiother.—J. Indian Assoc. Physiother. 2018, 12, 46. [Google Scholar] [CrossRef]
- Mulimani, P.; Hoe, V.C.; Hayes, M.J.; Idiculla, J.J.; Abas, A.B.; Karanth, L. Ergonomic interventions for preventing musculoskeletal disorders in dental care practitioners. Cochrane Database Syst. Rev. 2018, 10, CD011261. [Google Scholar] [CrossRef] [PubMed]
- Nye, W.H.; Partido, B.B.; DeWitt, J.; Kearney, R.C. Prevention and Reduction of Musculoskeletal Pain Through Chair-Side Stretching among Dental Hygiene Students. Am. Dent. Hyg. Assoc. 2021, 95, 84–91. [Google Scholar]
- Alhazzazi, T.Y.; Alzebiani, N.A.; Alotaibi, S.K.; Bogari, D.F.; Bakalka, G.T.; Hazzazi, L.W.; Jan, A.M.; McDonald, N.J. Awareness and attitude toward using dental magnification among dental students and residents at King Abdulaziz University, Faculty of Dentistry. BMC Oral Health 2017, 17, 1–7. [Google Scholar] [CrossRef]
- Plessas, A.; Delgado, M.B. The role of ergonomic saddle seats and magnification loupes in the prevention of musculoskeletal disorders. A systematic review. Int. J. Dent. Hyg. 2018, 16, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Aboalshamat, K.; Daoud, O.; Mahmoud, L.A.; Attal, S.; Alshehri, R.; Bin Othman, D.; Alzahrani, R. Practices and attitudes of dental loupes and their relationship to musculoskeletal disorders among dental practitioners. Int. J. Dent. 2020, 2020, 8828709. [Google Scholar] [CrossRef] [PubMed]
- Guignon, A.N. Seeing the Bigger View July 15, 2014 Only a Handful of Dentists Used Loupes Decades ago. At the Time, It Was Even More Rare for a Dental Hygienist to Use Magnification. Available online: https://www.rdhmag.com/career-profession/article/16404168/seeing-the-bigger-view (accessed on 4 October 2022).
- Valachi, B. Ergonomic guidelines for selecting patient chairs and delivery systems. Dent. Today 2009, 28, 130–133. [Google Scholar] [PubMed]
- Michalak-Turcotte, C.; Saunders, M.; Dussetschleger, J.; Ing, M. Selecting Equipment to Fit Your Ergonomic Needs. Woman Dent. J. 2006. Available online: https://www.google.com.hk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjqgcfNntz6AhVURd4KHSVBCM0QFnoECAcQAQ&url=https%3A%2F%2Fwww.dentistryiq.com%2Fpractice-management%2Findustry%2Farticle%2F16351006%2Fselecting-equipment-to-fit-your-ergonomic-needs&usg=AOvVaw02cbh76pvssUouusryompD (accessed on 4 October 2022).
- Nevala, N.; Sormunen, E.; Remes, J.; Suomalainen, K. Evaluation of ergonomics and efficacy of instruments in dentistry. Ergon. Open J. 2013, 6, 6–12. [Google Scholar] [CrossRef][Green Version]
- Freedman, G. Buyers’ guide to air-driven handpieces. Handpieces play an important role in practices. Dent. Today 2006, 25, 140–148. [Google Scholar] [PubMed]
- Sepah, Y.; Samad, L.; Altaf, A.; Halim, M.S.; Rajagopalan, N.; Khan, A.J. Aspiration in injections: Should we continue or abandon the practice? F1000Research 2014, 3, 157. [Google Scholar] [CrossRef] [PubMed]
- Kawaldeep, K.S.; Sakshi, G.; Puneet, S.; Deepak, B.K.; Madhu, G.B. Ergonomics in Dental Practice: An Update. Eur. J. Pharm. Med. Res. 2018, 5, 182–188. [Google Scholar]
- Kapitán, M.; Sustova, Z.; Ivancakova, R.; Suchánek, J. A comparison of different rubber dam systems on a dental simulator. Acta Med. 2014, 57, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Feng, B.; Liang, Q.; Wang, Y.; Andersen, L.L.; Szeto, G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open 2014, 4, e006451. [Google Scholar] [CrossRef]
- Marklund, S.; Huang, K.; Zohouri, D.; Wahlström, J. Dentists working conditions–factors associated with perceived workload. Acta Odontol. Scand. 2021, 79, 296–301. [Google Scholar] [CrossRef]
- Gupta, A.; Bhat, M.; Mohammed, T.; Bansal, N.; Gupta, G. Ergonomics in dentistry. Int. J. Clin. Pediatr. Dent. 2014, 7, 30. [Google Scholar] [CrossRef]
- Saleh, M.; Miko, H.; Triyanto, R.; Artawa, I.M.B. Musculoskeletal Disorders and Cumulative Trauma Disorders in Dental Practitioner (Review Article: Risk factor in dentist and dental hygienists). Actual Res. Sci. Acad. 2016, 1, 1–10. [Google Scholar]
- Bârlean, L.; Danila, I.; Sãveanu, I. Dentists ergonomic knowledge and attitudes in north-east region, Romania. Rom. J. Oral Rehabil. 2012, 4, 40–43. [Google Scholar]
- Jain, C.; Karibasappa, G.N.; Gautam, N.; Momin, S.; Nalawade, S.; Nandy, K.; Nagargoje, K. Assessment of attitude and perception of implementation of four handed dentistry among dental students-A Cross sectional study. Int. J. Dent. Res. 2022, 7, 4–8. [Google Scholar] [CrossRef]
- Preoteasa, C.T.; Pirvu, C.F.; Axante, A.; Enache, A.M.; Preoteasa, E. Four-handed dentistry-tasks of team members and general rules for instrument transfer. Rom. J. Oral Rehab. 2017, 9, 61–65. [Google Scholar]
- Pîrvu, C.; Pătraşcu, I.; Pîrvu, D.; Ionescu, C. The dentist’s operating posture–ergonomic aspects. J. Med. Life 2014, 7, 177. [Google Scholar]
- Bindra, P.; Ahluwalia, R.; Kumar, A.; Kumar, P.S.; Verma, D.; Mittal, M. Musculo skeletal disorders in dentistry. J. Orofac. Res. 2017, 6, 1–3. [Google Scholar]
- Garcia, P.P.N.S.; de Araujo Gottardello, A.C.; Presoto, C.D.; Campos, J.A.D.B. Ergonomic work posture in undergraduate dentistry students: Correlation between theory and practice. J. Educ. Ethics Dent. 2015, 5, 47. [Google Scholar] [CrossRef]
- Ramanigopal, C. The Factors that Affect the Work Environment of a Dentist inside the Dental Clinic* Vindha Paul. J. Exclus. Manag. Sci. 2015, 4, 2. [Google Scholar]
- Alamri, A.; El Sharkawy, M.F.; Alafandi, D. Occupational physical hazards and safety practices at dental clinics. Eur. J. Dent. 2022; Online ahead of print. [Google Scholar] [CrossRef]
- Shah, A.F.; Tangade, P.; Batra, M.; Kabasi, S. Ergonomics in dental practice. Int. J. Dent. Health Sci. 2014, 1, 68–78. [Google Scholar]
- Pejčić, N.; Đurić-Jovičić, M.; Miljković, N.; Popović, D.B.; Petrović, V. Posture in dentists: Sitting vs. standing positions during dentistry work: An EMG study. Srp. Arh. Za Celok. Lek. 2016, 144, 181–187. [Google Scholar] [CrossRef]
- Das, H.; Motghare, V.; Singh, M. Ergonomics in dentistry: Narrative review. Int. J. Appl. Dent. Sci. 2018, 4, 104–110. [Google Scholar]
- Ahearn, D.J.; Sanders, M.J.; Turcotte, C. Ergonomic design for dental offices. Work 2010, 35, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Suedbeck, J.R.; Tolle, S.L.; McCombs, G.; Walker, M.L.; Russell, D.M. Effects of instrument handle design on dental hygienists’ forearm muscle activity during scaling. Am. Dent. Hyg. Assoc. 2017, 91, 47–54. [Google Scholar]

| Kotter’s 8-Step Change Model | |
|---|---|
| Step 1: Urgency Step 2: Coalition Step 3: Vision | Creating a climate for change |
| Step 4: Communicate Step 5: Empower Step 6: Wins | Engaging the organisation |
| Step 7: Consolidate Step 8: Anchor | Implementing the change |
| Item | Ergonomic Feature | Yes | No |
|---|---|---|---|
| 1 | Breaks and chair side stretching exercises during the workday | ||
| 2 | Adequate work environment space | ||
| 3 | Inadequate environment (lighting, temperature, humidity) | ||
| 4 | Flexible work schedule | ||
| 5 | Ergonomic operator chair | ||
| 6 | Patient chair with adjustable headrests | ||
| 7 | Using surgical loupes | ||
| 8 | Practising four-handed dentistry | ||
| 9 | Changing postures frequently (alternating between standing and sit-down dentistry) | ||
| 10 | Selecting larger and lighter handles of dental instruments | ||
| 11 | Considering the purchase of ergonomic dental equipment | ||
| 12 | Adopting ergonomic posture |
| Ergonomic Checkpoint Applied | n */(%) | Brief Description of Intervention Effect |
|---|---|---|
| 18—(41%) | Reduces MSDs and has a positive effect on symptoms |
| 1—(3%) | Narrow workspaces are risk factors for MSDs |
| 2—(6%) | Good lighting increases the operator’s clarity and accessibility |
| 10—(22%) | Loupes influence the working posture |
| 30—(67%) | Flexible scheduling provides a sufficient recovery time |
| 7—(7%) | Enhances comfort and efficiency |
| 40—(88%) | Promotes efficiency and reduces stress |
| 29—(65%) | Proper posture maintains good health |
| 10—(16%) | Improves the working posture |
| 40—(88%) | An effective tool to prevent MSD injuries |
| 15—(50%) | Maximises patient access |
| 2—(2%) | Affects hand muscle load |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anshasi, R.J.; Alsyouf, A.; Alhazmi, F.N.; AbuZaitoun, A.T. A Change Management Approach to Promoting and Endorsing Ergonomics within a Dental Setting. Int. J. Environ. Res. Public Health 2022, 19, 13193. https://doi.org/10.3390/ijerph192013193
Anshasi RJ, Alsyouf A, Alhazmi FN, AbuZaitoun AT. A Change Management Approach to Promoting and Endorsing Ergonomics within a Dental Setting. International Journal of Environmental Research and Public Health. 2022; 19(20):13193. https://doi.org/10.3390/ijerph192013193
Chicago/Turabian StyleAnshasi, Rami J., Adi Alsyouf, Fahad Nasser Alhazmi, and Abeer Taha AbuZaitoun. 2022. "A Change Management Approach to Promoting and Endorsing Ergonomics within a Dental Setting" International Journal of Environmental Research and Public Health 19, no. 20: 13193. https://doi.org/10.3390/ijerph192013193
APA StyleAnshasi, R. J., Alsyouf, A., Alhazmi, F. N., & AbuZaitoun, A. T. (2022). A Change Management Approach to Promoting and Endorsing Ergonomics within a Dental Setting. International Journal of Environmental Research and Public Health, 19(20), 13193. https://doi.org/10.3390/ijerph192013193







