1. Introduction
At the University Hospital in Bern (Inselspital), Switzerland, patients aged 16 years and older are treated at the adult emergency department (ED), whereas younger patients are referred to paediatric emergency services. Therefore, adolescents aged sixteen to eighteen years are a transitional age group, interposed between paediatric and adult ED services. In a study at our tertiary ED at the Inselspital, we have shown that these adolescents present significantly more often with trauma and psychiatric problems than adults [
1]. The study at hand aimed to gather more detailed information about the adolescents aged 16 to 18 years presenting with psychiatric problems to an adult Swiss ED, in order to characterise this particular group of patients more clearly.
It is known that mental health disorders in children and adolescents are becoming more frequent worldwide, particularly in developed countries [
2]. Lo et al. showed that over a ten-year study period (2007 to 2016) in the United States, paediatric ED visits due to mental health disorders rose by 60%, whereas the overall paediatric ED visits were stable [
3]. The greatest increase (of 68%) was observed among adolescents aged 15 to 18 years. According to the World Health Organization (WHO), approximately 10% to 20% of adolescents globally experience mental health problems, although a considerable number remain underdiagnosed and undertreated [
4]. In addition, they stated that 16% of the global burden of disease in teenagers aged 10–19 years is due to mental health conditions.
In Switzerland, three of the top 10 causes of death in adolescents aged 15–19 years are associated with mental health problems, namely self-harm, drug use disorders and interpersonal violence [
5]. If the top ten causes of disability-adjusted life years (DALYs) are scrutinised, the importance of mental illness in adolescents becomes even clearer: six of the top 10 causes of DALYs for Swiss adolescents aged 15–19 years are psychiatric problems, with anxiety and depressive disorders being the top two [
6]. Further mental-health related problems causing the loss of healthy life-years are self-harm, drug use disorders, childhood behavioural disorders and bipolar disorder.
Adolescence is a vulnerable phase, in which many biological, cognitive, emotional, and social changes occur [
7]. Essential developmental tasks include shaping one’s identity, detachment from home and obtaining independence, career entry as well as building one’s social network. As many mental disorders emerge during adolescence, they continue to have substantial effects on life into adulthood [
8]. It is known that mental disorders are associated with educational underachievement, substance abuse, violence, and increased health-care costs. In addition to this, they pose a major risk factor for self-harm and suicide, which is the most common cause of death in Swiss adolescents aged 15 to 19 years [
5,
9]. The ages of 15–18 years mark a period of transition, including changes in health care systems. As mentioned before, in our ED, patients from the age of 16 years are treated by the adult emergency services. However, for adolescents up to 18 years, psychiatric care is guaranteed by child psychiatrists. The transitional phase of adolescents consequently poses a central challenge in psychiatric care [
7].
As important and challenging as mental health in young adults is, few data exist on the characteristics of adolescent ED users presenting with psychiatric problems. The study at hand will address important questions such as: What are the differences among adolescent ED users in terms of current and past psychiatric diagnoses, social setting and use of drugs and alcohol? Furthermore, the goal was to distinguish sex differences in presentation with problems related to mental health, since a previous study on the whole Swiss population suggested that males more often present with externalised diseases such as hyperkinetic disorders, substance abuse, and antisocial behaviour, whereas females more frequently suffer from depressive and anxiety disorders, as well as eating and psychosomatic disorders [
9]. This unique retrospective study of young ED users will fill a gap in our current knowledge of the patterns of psychiatric problems suffered by adolescents utilising our University Emergency Department. The data may lay the foundation for further inquiries and help to guide public health measures.
4. Discussion
To our knowledge, this is the first Swiss study to characterise adolescents aged 16 to 18 years presenting to general adult emergency services due to mental health problems. Overall, one tenth of cases of adolescents presenting to our ED were triaged as having a psychiatric problem [
1]. This shows the importance of understanding mental health conditions among adolescents, especially since these years are crucial in development and maintenance of social and emotional behaviour, which are in turn important for mental well-being [
4]. Furthermore, there are few studies from any country that focus on this particular transitional age group. Our present study at hand presents a good clinical characterisation of a subgroup of patients presenting to adult ED that has hardly ever been investigated.
It is interesting that we found a female/male ratio of 1.6:1 in adolescents presenting with mental-health-related problems, whereas in the original overview, the overall sex distribution for adolescents presenting to our ED for any reason was almost balanced [
1]. The finding that mental health conditions in female adolescents are more common is in line with several studies that found similar values of 62–65% females in their cohort [
2,
11]. However, this ratio may be distorted by repeated presentations, which are higher for both problems related to mental health and for females [
12]. In 65 of the 612 included cases, patients had presented to our ED at least twice for psychiatric problems. Of these, 40 were only treated twice, but some individual patients were treated five to seven times, or in one case even 23 times. Data of previous studies show that repeated visits by the same patient usually account for a substantial portion of mental health-related ED-presentations (approximately 20–40%) [
2,
12,
13,
14].
Since the first onset of three quarters of mental health disorders is before the age of 18 years, it does not come as a surprise that 54% of our cohort had received psychiatric care prior to ED presentation [
15].
Not only did we see fewer male adolescents in the ED, but they were also significantly less likely than females to have sought previous psychiatric assistance. The conclusion that more females than males seek psychiatric assistance is supported by a Swiss overview of psychiatric health care that focused on adolescents in their transitional years [
7]. This may be the reason that males were significantly less likely to be admitted to our ED by healthcare professionals than were females.
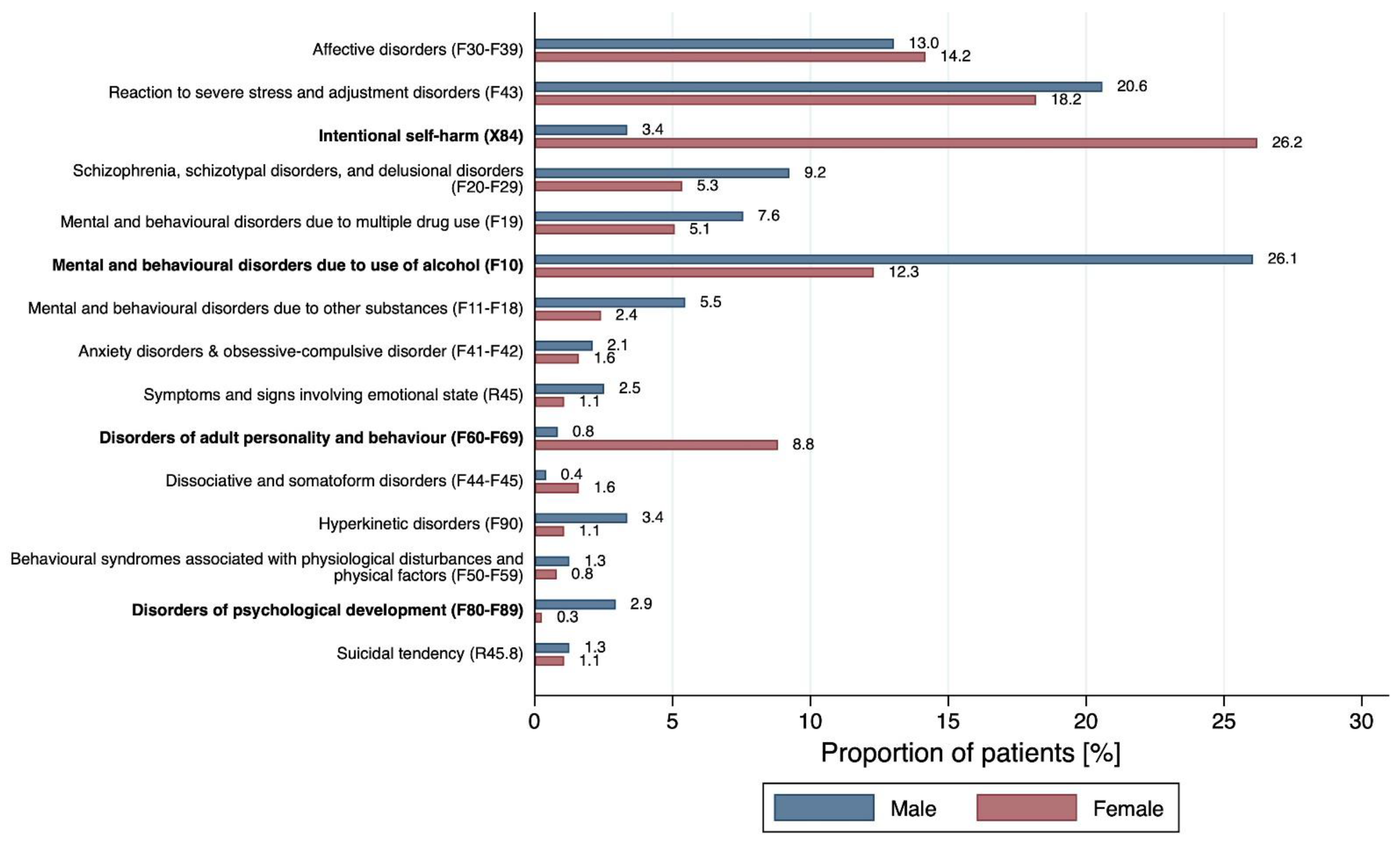
The most frequent diagnoses among our cohort were reactions to severe stress and adjustment disorders, followed by disorders due to use of alcohol, intentional self-harm, and affective disorders. Nearly one fifth of the cohort presented with reactions to severe stress, and adjustment disorders which might be correlated with the pressure adolescents are under in their transitional life years. There is a difference to adulthood, since the most frequent mental health-related diagnosis in Swiss adults is depression, hence affective disorders [
16]. Males were significantly more likely to present with disorders due to use of alcohol, which is in line with several Swiss observational studies [
9,
17,
18]. A Swiss overview of psychiatric health in 2020 showed that the most frequent diagnoses in children and adolescents who were admitted to inpatient psychiatric care are depressive episodes (F32), followed by reactions to severe stress, and adjustment disorders (F43) [
16]. Especially when it comes to acute alcohol intoxication, patients often stay at the ED for detoxication and go home as soon as they feel better, but they are rarely admitted to inpatient care.
Pre-existing disorders of adult personality and behaviour (F60–F69) were significantly less likely in males. However, it is controversial to make a diagnosis of these disorders at such a young age, since it must be based on a specific pattern of symptoms and behaviour throughout adolescence and adulthood. This emphasises the transitional age of adolescents, so that it is unusual to make a diagnosis at the age of 16 to 18 years. In this study, 17.3% of presentations of adolescents to the ED were for deliberate self-harm and males were significantly less likely to be affected. Lo et al. support this high prevalence, and even showed a threefold increase in intentional self-harm in American children aged 5 to 17 years over a study period of ten years (2007–2016) [
3]. Male adolescents in our cohort less often reported previous self-harm, previous suicidal intentions, or previous suicide attempts. In addition, males had almost four times lower odds of presenting with previous suicide attempts compared to females, and this is similar to results of a Turkish study about non-suicidal self-harm, suicidal ideation and suicide attempts (SA) in children and adolescents (female/male ratio for SA = 4.83:1) [
19]. It is crucial to identify and deal with non-suicidal self-harm and suicidal ideation, since they are known to be strong predictors for suicide. A study on suicide in England and Wales showed that 52% of children and adolescents who committed suicide had a history of self-harm [
20].
Overall, approximately one fifth of our cohort reported attempted suicide prior to ED presentation. According to the WHO, self-harm is the leading cause of death in Swiss adolescents aged fifteen to nineteen years—so that it is essential to recognise self-harming behaviour [
5]. This is of the greatest importance, as EDs are frequently the first point of contact with the health care system for many children and adolescents who self-harm. Therefore, we highlight the importance of establishing specific post-ED care for patients with self-harming behaviour.
The incidence of suicidal tendencies as the main reason for presentation to the ED (1.1%) was much less than the incidence of acute suicidal ideation in a specific assessment during their stay at the ED (31.7%). One explanation for the rather low percentage of acute suicidal tendency in our cohort might be a bias in triage categorisation, so that suicide attempts might not have been categorised as a primary mental health problem, but for example as trauma or as a neurological problem (e.g., self-poisoning). Otherwise, suicidal ideation is mostly associated with other problems, be they mental, social, or physical, and are therefore not necessarily the chief complaint. In addition, patients might not mention suicidal tendencies on their own due to shame or fear of stigmatisation. However, the high percentage of patients reporting acute suicidal ideation shows the importance of a thorough assessment in the emergency department, and this indicates that every patient presenting with mental health problems should be explicitly asked about suicidal thoughts and intentions.
Whereas young girls tended more to self-harming behaviour, 14.3% of males in our cohort stated that they represented a danger for fellow men and this was associated with threefold higher odds of external aggression in boys. Our data are therefore consistent with the view that females more often present with internalising diagnoses, whereas males have a higher rate of externalizing diagnoses [
9]. This is in line with the aforementioned Turkish study which also showed the prominence of aggressive symptoms in males [
19]. It is known that not only mental health issues and younger age per se, yet also male sex, ED admission in police custody as well as active substance use, are associated with a greater risk of violent events in the emergency department [
21]. Possible parallels can be drawn, since our cohort showed that males were roughly two times more likely to be admitted by police. Furthermore, boys were significantly more likely to report consumption of alcohol and cannabis.
Not only were disorders due to use of alcohol the second most frequent reason for referral to the ED (17.6%), but overall, 43.3% of the cohort affirmed regular alcohol use. We were not able to draw a distinction between acute alcohol intoxication and harmful alcohol use or even alcohol dependence. Alcohol misuse was globally the highest risk factor for death among adolescents aged fifteen to nineteen years in 2013, similar to our results predominantly in males [
22]. Furthermore, alcohol consumption poses a risk for suicide and is strongly associated with mental health disorders [
4,
8]. In addition to this, excessive alcohol consumption leads to an increase in violence and aggressiveness, trauma, and social marginalisation [
17]. A Swiss report on addiction monitoring stated that adolescents mainly drink alcohol during the weekends, but when they drink they tend to consume large amounts [
17,
18]. This leads to binge drinking, particularly for adolescents or young adults aged 15 to 24 years.
More than a fifth (21.2%) of all cases reported smoking tobacco; however, from our data it was unclear whether the adolescents were smoking it daily or just on occasion. This percentage is in line with the prevalence of smoking tobacco in Swiss adolescents aged fifteen to nineteen years (21.1%) [
18]. There was no significant difference in likelihood according to sex.
Overall, 26.3% of our cohort reported the use of cannabis, with males having double the odds for this. This percentage is similar to the lifetime prevalence of cannabis consumption in Swiss adolescents aged 15 to 19 years [
18]. As the twelve month prevalence (20.8%) and the 30 day prevalence (9.4%) in the same subgroup are considerably lower, it suggests that many adolescents consume cannabis only on occasion, maybe even only to try it on a few opportunities. It would be interesting to see whether the twelve month and 30 day prevalence in our cohort were higher, but it was not possible to deduce this from our results. It may be relevant that adolescents who consume cannabis regularly, also tend to drink more alcohol, smoke regularly and use more other drugs [
18].
3.3% to 4.7% of patients reported that they consumed either amphetamine, LSD, cocaine, or Ecstasy/MDMA. It is possible that the respective subgroups overlap, but this is only an assumption. Apart from LSD consumption, which was more likely for males than females, there was no significant sex difference to discern. The percentages in our cohort were noticeably higher than published values for the overall twelve month prevalence of drug use by Swiss adolescents (0.3% to 0.5%) [
18]. This might be because our numbers represent the lifetime prevalence—which is supposedly higher. In general, it is presumed that the use of illegal drugs is underestimated in health surveys due to stigmatization and social undesirability, whereas this effect might be less marked during history taking by the ED doctor [
18]. However, it would not come as a surprise that drug use among mentally ill adolescents is more likely than in the overall population, as this might be an expression of psychological distress, dysfunctional coping-strategies, or an attempt at self-healing.
A quarter of adolescents in our cohort were admitted to the ED by family members. A previous study also found that the family was the most common source of referral to the ED for children and adolescents, but with a higher percentage (49%) [
23]. However, this study included children from the age of five years and it seems likely that the younger patients are, the more often they are admitted by family members. As mentioned before, males were significantly less likely to be admitted to the ED by health care professionals, suggesting that they are less likely to seek help earlier. They were, however, more likely to be escorted to the ED by police, in line with their higher likelihood of external aggressive behaviour.
According to a Swiss study, low educational attainment, migration background, loneliness, as well as unemployment mark risk factors for psychiatric diseases [
16]. In total, 14% of adolescents in our study reported a migration background, with a significantly higher likelihood in males (OR 2.58, 1.61–4.11). A study in Vienna, Austria—a larger city but with a similar culture—found that 53.4% of minors presenting to the psychiatric emergency department had a migration background—which is clearly more than in our study [
24]. They commented that emergency presentations from patients with migration background happen more often when the problems become overwhelming, rather than that they sought psychological help at an earlier point. Additionally, and contrary to our findings, even in patients with migration background, females presented significantly more often to the ED. Young adults with migration background presenting to the ED for mental health-related problems surely pose an interesting population and further characterisation is needed to understand this population more clearly.
A large portion of young adults mentioned familial problems, significantly less often in boys. Since adolescence is an important period for establishing social and emotional behaviour, conflicts might have crucial consequences [
4]. In a Turkish study, relational problems were indeed the strongest predictor of suicide attempts in children [
19]. The importance of a functional familial setting in adolescents and young adults is furthermore highlighted by Radde et al., who stated that dysfunctional communication with parents was a risk for suicidal tendencies [
25]. In addition to familial problems, educational issues were frequent as well, although with a higher likelihood in males. Interestingly, studies showed that ED presentation in adolescents occurs more commonly during school months, which might be a result of increased stress levels [
23].
More than half of our population were discharged home, which suggests that the clinical presentations in these patients were not as severe as to need further hospital or psychiatry treatment as an inpatient. The likelihood of males being able to return home was significantly higher—suggesting that disease patterns were more severe in girls. Additionally, males significantly more often presented with alcohol use disorders, but this less often resulted in inpatient admission.
This study has several strengths: It was conducted in an interdisciplinary ED and had broad inclusion criteria. Selection bias was minimised by careful screening and individual scrutiny of each report. In addition, there are hardly any previous data for this particular age-group focusing on mental-health-related ED visits. However, there are some limitations: Since the study was conducted as a retrospective analysis, there were no standardised questionnaires. Furthermore, for the statistical analysis we set ‘no information’ as being equivalent to a negation, as we assumed that only existing characteristics would be documented in the ED reports. However, the first assessment is usually performed by a general clinician rather than a psychiatrist, so there might be an information bias as not everyone inquired about all the parameters we analysed.
Additionally, data collection was based on diagnosis at triage, resulting not only in potential wrongful classification, yet also in possible underestimation of secondary diagnoses of mental health problems. Furthermore, data were gathered from one emergency department only, so data from similar clinics should be analysed too, in order to gather more information about adolescents with mental health-related problems. It should also be borne in mind that many adolescents hesitate to seek psychiatric assistance, so many cases are unreported.
As adolescents aged sixteen to eighteen years mark a transitional age group when it comes to health care services, we aimed to distinguish this specific subpopulation. Since presentation to our emergency department due to psychiatric problems was more frequent in younger than in older adults, and adolescence is known to be a vulnerable phase in which many mental health illnesses arise, it is important to understand this population [
1]. Additionally, there is the problem in Switzerland that the responsibilities in health care for adolescents change with age. As mentioned before, in our health system child psychiatrists are responsible for patients up to their eighteenth birthday. In contrast, for emergency services, adolescents in our hospital already change to adult care at the age of sixteen, i.e., two years earlier. At our ED, adolescents are assessed by adult psychiatrists. If it is necessary for them to be admitted to inpatient care, however, they enter a child psychiatry unit. Therefore, it is of crucial importance that not only child psychiatrists, but also adult psychiatrists focus specifically on adolescents, as mental health illnesses tend to persist into adulthood. A change in care services at some point is inevitable. Additionally, since there is a different spectrum of psychiatric diseases in adolescents, explicit work up and collaboration of child and adult psychiatrists is of great importance.