Parenting Programs to Reduce Recurrence of Child Maltreatment in the Family Environment: A Systematic Review
Abstract
:1. Introduction
- Providing a summary of evidence on the effectiveness of behavioral/cognitive–behavioral PPs in preventing physical re-abuse in children (0–18);
- Extending previous reviews by including a reduction in recurrence as the main outcome measure but also focusing on the effect of PPs on secondary outcomes such as a reduction in maltreatment risk, a reduction in parental and child psychopathology, and an improvement in parent–child relationships;
- Overcoming prior reviews’ methodological limitations by including only randomized controlled trials (with at least one follow-up). Moreover, the present work provides a deep and focused look into the intervention programs, to point out what variables and treatment components support their effectiveness in reducing maltreatment recidivism.
2. Materials and Methods
2.1. Search Strategy
- Population: parents or other primary caregivers of children aged 0–18 years. Parents were eligible if they were referred for suspected or substantiated child physical maltreatment, supported by either an official report (police, child protection services or other official agency referral), parents’ or children’s self-reports, or an assessment through standardized instruments. Both suspected and substantiated cases were considered eligible, having the same recidivism risk [42].
- Intervention: behavioral or cognitive–behavioral parenting programs aimed at reducing the recurrence of child physical maltreatment within families (tertiary prevention).
- Comparison: the control group could be either an alternative intervention group, treatment as usual, waitlist, or no treatment.
- Outcome measures: a reduction in physical maltreatment recurrence according to official reports, according to parents’ or children’s self-reports, through standardized instruments, or through maltreatment-related indicators (such as physical punishment or harsh parenting). The following secondary outcomes were included in the present review: reduction in maltreatment risk, reduction in parental and child psychopathology, and improvement in parent–child relationship.
- Study design: randomized controlled trials with at least one follow-up.
- The sample did not include parents but other subjects (e.g., teachers).
- The parenting program was not behavioral or cognitive–behavioral in the approach or was used as a primary or secondary prevention intervention.
- Studies were not focused on the reduction in child physical maltreatment within families as the main indicator of a parenting program’s effectiveness.
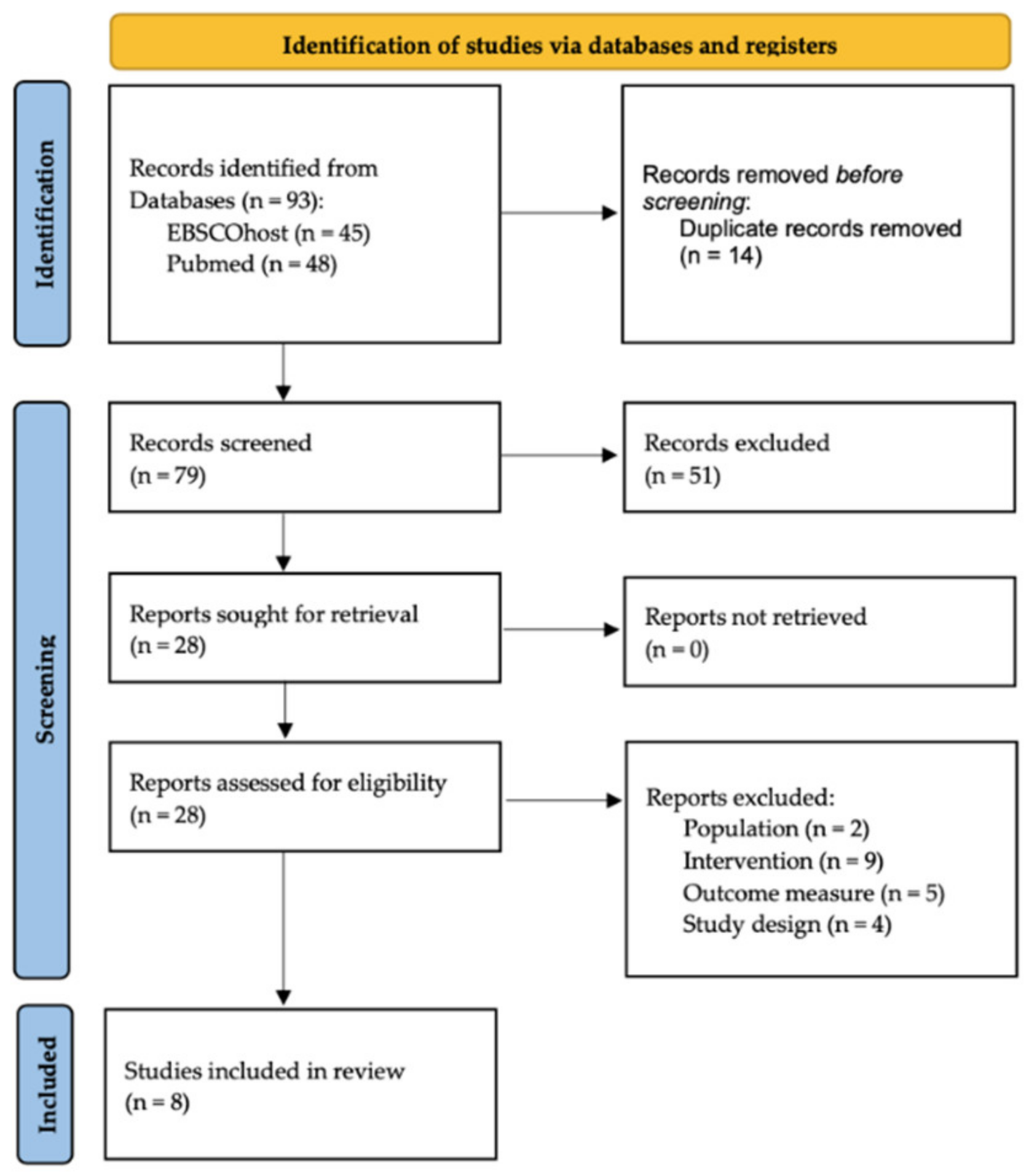
2.2. Selection Process and Data Extraction
3. Results
3.1. Study Selection
3.2. Characteristics of the Included Studies
3.2.1. Population
3.2.2. Interventions
3.2.3. Comparison Groups
3.2.4. Follow-Up
3.3. Primary Outcome Measure: Re-Abuse Reports
3.3.1. Within-Group Differences
3.3.2. Between-Group Differences
3.4. Secondary Outcomes (Proxies for Child Maltreatment)
3.4.1. Maltreatment Risk
3.4.2. Parent–Child Interactions, Parenting, and Family Functioning
3.4.3. Parental Psychopathology
3.4.4. Child Functioning
4. Discussion
4.1. Clinical Implications
4.2. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Preventing Child Maltreatment: A Guide to Taking Action and Generating Evidence; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- National Institute for Health and Care Excellence. Child Abuse and Neglect. NICE Guideline; NHS: London, UK, 2017.
- World Health Organization. Global Status Report on Violence Prevention 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Stoltenborgh, M.; Bakermans-Kranenburg, M.J.; Alink, L.R.A.; van IJzendoorn, M.H. The Prevalence of Child Maltreatment across the Globe: Review of a Series of Meta-Analyses: Prevalence of Child Maltreatment across the Globe. Child Abuse Rev. 2015, 24, 37–50. [Google Scholar] [CrossRef]
- Mehta, D.; Kelly, A.B.; Laurens, K.R.; Haslam, D.; Williams, K.E.; Walsh, K.; Baker, P.R.A.; Carter, H.E.; Khawaja, N.G.; Zelenko, O.; et al. Child Maltreatment and Long-Term Physical and Mental Health Outcomes: An Exploration of Biopsychosocial Determinants and Implications for Prevention. Child Psychiatry Hum. Dev. 2021, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Schilling, S.; Christian, C.W. Child Physical Abuse and Neglect. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Strathearn, L.; Giannotti, M.; Mills, R.; Kisely, S.; Najman, J.; Abajobir, A. Long-Term Cognitive, Psychological, and Health Outcomes Associated with Child Abuse and Neglect. Pediatrics 2020, 146, e20200438. [Google Scholar] [CrossRef] [PubMed]
- Kolko, D.J.; Berkout, O.V. Child Physical Abuse. In Handbook of Trauma Psychology; Gold, S., Cook, J., Dalenberg, C., Eds.; American Psychological Association: Washington, DC, USA, 2017; pp. 99–115. [Google Scholar]
- Maglione, D.; Caputi, M.; Moretti, B.; Scaini, S. Psychopathological Consequences of Maltreatment among Children and Adolescents: A Systematic Review of the GxE Literature. Res. Dev. Disabil. 2018, 82, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Perego, G.; Caputi, M.; Ogliari, A. Neurobiological Correlates of Psychosocial Deprivation in Children: A Systematic Review of Neuroscientific Contributions. Child Youth Care Forum 2016, 45, 329–352. [Google Scholar] [CrossRef]
- Teicher, M.H.; Samson, J.A. Annual Research Review: Enduring Neurobiological Effects of Childhood Abuse and Neglect. J. Child Psychol. Psychiatr. 2016, 57, 241–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Vecchio, T.; Erlanger, A.C.E.; Slep, A.M.S. Theories of Child Abuse. In Handbook of Family Theories; Fine, M.A., Fincham, F.D., Eds.; Taylor and Francis/Routledge: New York, NY, USA, 2014. [Google Scholar]
- Patterson, G.R. The aggressive child: Victim and architect of a coercive system. In Behavior Modification and Families; Mash, E.J., Hamerlynck, L.A., Handy, L.C., Eds.; Brunner/Mazel: New York, NY, USA, 1976; pp. 267–316. [Google Scholar]
- Patterson, G.R. Coercive Family Process; Castalia: Eugene, OR, USA, 1982. [Google Scholar]
- Bandura, A. Psychological Modeling: Conflicting Theories; Aldine: Chicago, IL, USA, 1971. [Google Scholar]
- Bandura, A. Self-Efficacy: Toward a Unifying Theory of Behavioral Change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Stith, S.M.; Liu, T.; Davies, L.C.; Boykin, E.L.; Alder, M.C.; Harris, J.M.; Som, A.; McPherson, M.; Dees, J.E.M.E.G. Risk Factors in Child Maltreatment: A Meta-Analytic Review of the Literature. Aggress. Violent Behav. 2009, 14, 13–29. [Google Scholar] [CrossRef] [Green Version]
- Azar, S.T.; Reitz, E.B.; Goslin, M.C. Mothering: Thinking Is Part of the Job Description: Application of Cognitive Views to Understanding Maladaptive Parenting and Doing Intervention and Prevention Work. J. Appl. Dev. Psychol. 2008, 29, 295–304. [Google Scholar] [CrossRef]
- Hakman, M.; Chaffin, M.; Funderburk, B.; Silovsky, J.F. Change Trajectories for Parent-Child Interaction Sequences during Parent-Child Interaction Therapy for Child Physical Abuse. Child Abuse Negl. 2009, 33, 461–470. [Google Scholar] [CrossRef]
- Bowlby, J. Attachment and Loss: Vol. 1. Attachment; Basic Books: New York, NY, USA, 1969. [Google Scholar]
- Pianta, R.; Egeland, B.; Erikson, M.F. The antecedents of maltreatment: Results of the Mother-Child Interaction Research Project. In Child Maltreatment: Theory and Research on the Causes and Consequences of Child Abuse and Neglect; Cicchetti, D., Carlson, V., Eds.; Cambridge University Press: New York, NY, USA, 1989; pp. 203–253. [Google Scholar]
- Belsky, J. Etiology of Child Maltreatment: A Developmental-Ecological Analysis. Psychol. Bull. 1993, 114, 413–434. [Google Scholar] [CrossRef]
- Dopke, C.A.; Milner, J.S. Impact of Child Noncompliance on Stress Appraisals, Attributions, and Disciplinary Choices in Mothers at High and Low Risk for Child Physical Abuse. Child Abuse Negl. 2000, 24, 493–504. [Google Scholar] [CrossRef]
- Gottman, J.M.; Katz, L.F.; Hooven, C. Parental Meta-Emotion Philosophy and the Emotional Life of Families: Theoretical Models and Preliminary Data. J. Fam. Psychol. 1996, 10, 243–268. [Google Scholar] [CrossRef]
- Chaffin, M.; Kelleher, K.; Hollenberg, J. Onset of Physical Abuse and Neglect: Psychiatric, Substance Abuse, and Social Risk Factors from Prospective Community Data. Child Abuse Negl. 1996, 20, 191–203. [Google Scholar] [CrossRef]
- Milner, J.S.; Chilamkurti, C. Physical Child Abuse Perpetrator Characteristics. A Review of the Literature. J. Interpers. Violence 1991, 6, 345–366. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Belsky, J. Child Maltreatment. An Ecological Integration. Am. Psychol. 1980, 35, 320–335. [Google Scholar]
- Black, D.A.; Heyman, R.E.; Smith Slep, A.M. Risk Factors for Child Physical Abuse. Aggress. Violent Behav. 2001, 6, 121–188. [Google Scholar] [CrossRef]
- DuMont, K.; Mitchell-Herzfeld, S.; Greene, R.; Lee, E.; Lowenfels, A.; Rodriguez, M.; Dorabawila, V. Healthy Families New York (HFNY) Randomized Trial: Effects on Early Child Abuse and Neglect. Child Abuse Negl. 2008, 32, 295–315. [Google Scholar] [CrossRef]
- Guterman, N.B.; Tabone, J.K.; Bryan, G.M.; Taylor, C.A.; Napoleon-Hanger, C.; Banman, A. Examining the Effectiveness of Home-Based Parent Aide Services to Reduce Risk for Physical Child Abuse and Neglect: Six-Month Findings from a Randomized Clinical Trial. Child Abuse Negl. 2013, 37, 566–577. [Google Scholar] [CrossRef]
- Lachman, J.M.; Alampay, L.P.; Jocson, R.M.; Alinea, C.; Madrid, B.; Ward, C.; Hutchings, J.; Mamauag, B.L.; Garilao, M.A.V.F.V.; Gardner, F. Effectiveness of a Parenting Programme to Reduce Violence in a Cash Transfer System in the Philippines: RCT with Follow-Up. Lancet Reg. Health West. Pac. 2021, 17, 100279. [Google Scholar] [CrossRef] [PubMed]
- Self-Brown, S.; Osborne, M.C.; Boyd, C.; DeVeausse Brown, N.; Rostad, W.; Patterson, A.; Baker, E.; Thomas, A.; McAdam, E.M.; Jackson, M.; et al. The Impact of SafeCare® Dads to Kids Program on Father Maltreatment Risk and Involvement: Outcomes and Lessons Learned from an Efficacy Trial. Child Abuse Negl. 2018, 83, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Mihalic, S.; Fagan, A.; Irwin, K.; Ballard, D.; Elliott, D. Blueprints for Violence Prevention; University of Colorado: Boulder, CO, USA, 2002. [Google Scholar]
- National Institute for Health and Clinical Excellence. Parent-Training/Education Programmes in the Management of Children with Conduct Disorders; NHS: London, UK, 2006.
- Vlahovicova, K.; Melendez-Torres, G.J.; Leijten, P.; Knerr, W.; Gardner, F. Parenting Programs for the Prevention of Child Physical Abuse Recurrence: A Systematic Review and Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2017, 20, 351–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barlow, J.; Johnston, I.; Kendrick, D.; Polnay, L.; Stewart-Brown, S. Individual and Group-Based Parenting Programmes for the Treatment of Physical Child Abuse and Neglect. Cochrane Database Syst. Rev. 2006. [Google Scholar] [CrossRef]
- Chen, M.; Chan, K.L. Effects of Parenting Programs on Child Maltreatment Prevention: A Meta-Analysis. Trauma Violence Abuse 2016, 17, 88–104. [Google Scholar] [CrossRef]
- Santini, P.M.; Williams, L.C. Parenting Programs to Prevent Corporal Punishment: A Systematic Review. Paidéia 2016, 26, 121–129. [Google Scholar] [CrossRef] [Green Version]
- Roth, A.; Fonagay, P. What Works for Whom? A Critical Review of Psychotherapy Research. Psychiatr. Serv. 1996, 48, 1596. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kohl, P.L.; Jonson-Reid, M.; Drake, B. Time to Leave Substantiation Behind: Findings From A National Probability Study. Child Maltreat. 2009, 14, 17–26. [Google Scholar] [CrossRef]
- Sanjeevi, J.; Houlihan, D.; Bergstrom, K.A.; Langley, M.M.; Judkins, J. A Review of Child Sexual Abuse: Impact, Risk, and Resilience in the Context of Culture. J. Child Sex. Abuse 2018, 27, 622–641. [Google Scholar] [CrossRef]
- MacMillan, H.L.; Thomas, B.H.; Jamieson, E.; Walsh, C.A.; Boyle, M.H.; Shannon, H.S.; Gafni, A. Effectiveness of Home Visitation by Public-Health Nurses in Prevention of the Recurrence of Child Physical Abuse and Neglect: A Randomised Controlled Trial. Lancet 2005, 365, 1786–1793. [Google Scholar] [CrossRef]
- Santini, P.M.; Williams, L.C.A. A Randomized Controlled Trial of an Intervention Program to Brazilian Mothers Who Use Corporal Punishment. Child Abuse Negl. 2017, 71, 80–91. [Google Scholar] [CrossRef]
- Chaffin, M.; Silovsky, J.F.; Funderburk, B.; Valle, L.A.; Brestan, E.V.; Balachova, T.; Jackson, S.; Lensgraf, J.; Bonner, B.L. Parent-Child Interaction Therapy With Physically Abusive Parents: Efficacy for Reducing Future Abuse Reports. J. Consult. Clin. Psychol. 2004, 72, 500–510. [Google Scholar] [CrossRef] [Green Version]
- Jouriles, E.N.; McDonald, R.; Rosenfield, D.; Norwood, W.D.; Spiller, L.; Stephens, N.; Corbitt-Shindler, D.; Ehrensaft, M. Improving Parenting in Families Referred for Child Maltreatment: A Randomized Controlled Trial Examining Effects of Project Support. J. Fam. Psychol. 2010, 24, 328–338. [Google Scholar] [CrossRef]
- Kolko, D.J. Clinical Monitoring of Treatment Course in Child Physical Abuse: Psychometric Characteristics and Treatment Comparisons. Child Abuse Negl. 1996, 20, 23–43. [Google Scholar] [CrossRef]
- Kolko, D.J.; Herschell, A.D.; Baumann, B.L.; Hart, J.A.; Wisniewski, S.R. AF-CBT for Families Experiencing Physical Aggression or Abuse Served by the Mental Health or Child Welfare System: An Effectiveness Trial. Child Maltreat. 2018, 23, 319–333. [Google Scholar] [CrossRef]
- Lee, E.; Kirkland, K.; Miranda-Julian, C.; Greene, R. Reducing Maltreatment Recurrence through Home Visitation: A Promising Intervention for Child Welfare Involved Families. Child Abuse Negl. 2018, 86, 55–66. [Google Scholar] [CrossRef]
- Runyon, M.K.; Deblinger, E.; Steer, R.A. Group Cognitive Behavioral Treatment for Parents and Children At-Risk for Physical Abuse: An Initial Study. Child Fam. Behav. Ther. 2010, 32, 196–218. [Google Scholar] [CrossRef]
- Chaffin, M.; Bard, D. Impact of Intervention Surveillance Bias on Analyses of Child Welfare Report Outcomes. Child Maltreat. 2006, 11, 301–312. [Google Scholar] [CrossRef]
- Milner, J.S. The Child Abuse Potential Inventory Manual, 2nd ed.; Psyctec: DeKalb, IL, USA, 1986. [Google Scholar]
- Ondersma, S.J.; Chaffin, M.J.; Mullins, S.M.; LeBreton, J.M. A Brief Form of the Child Abuse Potential Inventory: Development and Validation. J. Clin. Child Adolesc. Psychol. 2005, 34, 301–311. [Google Scholar] [CrossRef]
- Eyberg, S.M.; Bessmer, J.; Newcomb, K.; Edwards, D.; Robinson, E. Manual for the Dyadic Parent-Child Interaction Coding System-II; Social and Behavioral Sciences Documents (Ms. No. 2897); Research Connections: Washington, DC, USA, 1994. [Google Scholar]
- Straus, M.A.; Hamby, S.L.; Boney-McCoy, S.; Sugarman, D.B. The Revised Conflict Tactics Scales (CTS2). Development and Preliminary Psychometric Data. J. Fam. Issues 1996, 17, 283–316. [Google Scholar] [CrossRef]
- Straus, M.A. Measuring Intrafamily Conflict and Violence: The Conflict Tactics (CT) Scales. J. Marriage Fam. 1979, 41, 75. [Google Scholar] [CrossRef]
- Straus, M.A.; Hamby, S.L.; Finkelhor, D.; Moore, D.W.; Runyan, D. Identification of Child Maltreatment with the Parent-Child Conflict Tactics Scales: Development and Psychometric Data for a National Sample of American Parents. Child Abuse Negl. 1998, 22, 249–270. [Google Scholar] [CrossRef]
- Caldwell, B.M.; Bradley, R.H. Home Observation for Measurement of the Environment; University of Arkansas: Little Rock, AR, USA, 1984. [Google Scholar]
- Sanders, M.R.; Waugh, L.; Tully, L.; Hynes, K. The Revised Family Observation Schedule, 3rd ed.; Parenting and Family Support Centre: Brisbane, QLD, Australia, 1996. [Google Scholar]
- Campis, L.K.; Lyman, R.D.; Prentice-Dunn, S. The Parental Locus of Control Scale: Development and Validation. J. Clin. Child Psychol. 1986, 15, 260–267. [Google Scholar] [CrossRef]
- Arnold, D.S.; O’Leary, S.G.; Wolff, L.S.; Acker, M.M. The Parenting Scale: A Measure of Dysfunctional Parenting in Discipline Situations. Psychol. Assess. 1993, 5, 137–144. [Google Scholar] [CrossRef]
- Frick, P.J. Alabama Parenting Questionnaire (APQ); University of Alabama: Tuscaloosa, AL, USA, 1991. [Google Scholar] [CrossRef]
- Bavolek, S.J. Handbook for the Adult-Adolescent Parenting Inventory; Family Development Resources: Eau Claire, WI, USA, 1984. [Google Scholar]
- Moos, R.H.; Insel, P.M.; Humphrey, B. Family Work and Group Environment Scales; Consulting Psychologists Press: Palo Alto, CA, USA, 1974. [Google Scholar]
- Epstein, N.B.; Baldwin, L.M.; Bishop, D.S. The McMaster Family Assessment Device. J. Marital Fam. Ther. 1983, 9, 171–180. [Google Scholar] [CrossRef]
- Beck, A.T. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561. [Google Scholar] [CrossRef] [Green Version]
- Derogatis, L.R.; Rickels, K.; Rock, A.F. The SCL-90 and the MMPI: A Step in the Validation of a New Self-Report Scale. Br. J. Psychiatry 1976, 128, 280–289. [Google Scholar] [CrossRef]
- Reynolds, C.R.; Kamphaus, R.W. Manual for the Behavioral Assessment System for Children; American Guidance Service: Circle Pines, MN, USA, 1992. [Google Scholar]
- Wolraich, M.L. Psychometric Properties of the Vanderbilt ADHD Diagnostic Parent Rating Scale in a Referred Population. J. Pediatr. Psychol. 2003, 28, 559–568. [Google Scholar] [CrossRef] [Green Version]
- Foa, E.B.; Johnson, K.M.; Feeny, N.C.; Treadwell, K.R.H. The Child PTSD Symptom Scale: A Preliminary Examination of Its Psychometric Properties. J. Clin. Child Adolesc. Psychol. 2001, 30, 376–384. [Google Scholar] [CrossRef]
- Quay, H.C.; Peterson, D.R. The Revised Behavior Problem Checklist: Professional Manual; Psychological Assessment Resources: Odessa, FL, USA, 1987. [Google Scholar]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA School-Age Forms & Profiles; University of Vermont, Research Center for Children, Youth, and Families: Burlington, VT, USA, 2001. [Google Scholar]
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiat. 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- The National Child Traumatic Stress Network. Child Abuse Potential Inventory. 2014. Available online: https://www.nctsn.org/measures/child-abuse-potential-inventory (accessed on 5 July 2020).
- Urquiza, A.J.; McNeil, C.B. Parent-Child Interaction Therapy: An Intensive Dyadic Intervention for Physically Abusive Families. Child Maltreat. 1996, 1, 134–144. [Google Scholar] [CrossRef]
- Medley, A.; Sachs-Ericsson, N. Predictors of Parental Physical Abuse: The Contribution of Internalizing and Externalizing Disorders and Childhood Experiences of Abuse. J. Affect. Disord. 2009, 113, 244–254. [Google Scholar] [CrossRef] [Green Version]
- Runyon, M.K.; Deblinger, E.; Ryan, E.E.; Thakkar-Kolar, R. An Overview of Child Physical Abuse: Developing an Integrated Parent-Child Cognitive-Behavioral Treatment Approach. Trauma Violence Abus. 2004, 5, 65–85. [Google Scholar] [CrossRef] [Green Version]
- Children’s Hospital-San Diego; Chadwick Center for Children and Families; National Call to Action. Closing the Quality Chasm in Child Abuse Treatment: Identifying and Disseminating Best Practices. The Findings of the Kauffman Best Practices Project to Help Children Heal from Child Abuse; Children’s Hospital: San Diego, CA, USA, 2004. [Google Scholar]
- The California Evidence-Based Clearinghouse for Child Welfare. Alternatives for Families: A Cognitive-Behavioral Therapy (AF-CBT). 2021. Available online: https://www.cebc4cw.org/program/alternatives-for-families-a-cognitive-behavioral-therapy/detailed (accessed on 8 October 2022).
- Fernandez, M.A.; Eyberg, S.M. Predicting Treatment and Follow-up Attrition in Parent–Child Interaction Therapy. J. Abnorm. Child Psychol. 2009, 37, 431–441. [Google Scholar] [CrossRef]
- Harwood, M.D.; Eyberg, S.M. Therapist Verbal Behavior Early in Treatment: Relation to Successful Completion of Parent–Child Interaction Therapy. J. Clin. Child Adolesc. Psychol. 2004, 33, 601–612. [Google Scholar] [CrossRef]
- U.S. Department of Health & Human Services; Administration for Children and Families; Administration on Children, Youth and Families; Children’s Bureau. Child Maltreatment 2020. 2022. Available online: https://www.acf.hhs.gov/cb/data-research/child-maltreatment (accessed on 25 June 2022).
- Hegar, R.L.; Zuravin, S.J.; Orme, J.G. Factors predicting severity of physical child abuse injury: A review of the literature. J. Interpers. Violence 1994, 9, 170–183. [Google Scholar] [CrossRef]
| 1st Author and Year | Country | Population | Follow-Up (After Treatment) | ||||
|---|---|---|---|---|---|---|---|
| N | Parents | Children (Age Range) | |||||
| Chaffin et al. 2004 [46] | USA | 110 IG1: 42; IG2: 33; CG: 35 | 65% F; Mage = 32 | 4–12 | 2.3 years | ||
| Jouriles et al. 2010 [47] | USA | 35 IG: 17; CG: 18 | 100% F; Mage = 28.7 | 3–8 | 4, 8 months | ||
| Kolko, 1996 [48] | USA | 38 dyads IG: 21; CG: 17 | n/a | 6–13 | 1 year | ||
| Kolko et al. 2018 [49] | USA | 195 IG: 122; CG: 73 | n/a | 5–15 | 6, 12 months | ||
| Lee et al. 2018 [50] | USA | 104 IG: 52; CG: 52 | 100% F; Mage IG = 26.65; Mage CG = 26.96 | 0–7 | 2 years | ||
| MacMillan et al. 2005 [44] | Canada | 163 IG: 89; CG: 74 | 95% F; Mage = 29.2 | 0–13 | 1 year | ||
| Runyon et al. 2010 [51] | USA | 44 P + 60 C IG: 24 P + 34 C; CG: 20 P + 26 C | 86% F; Mage = 33.02 | 7–13 | 3 months | ||
| Santini et al. 2017 [45] | Brazil | 40 IG: 20; CG: 20 | 100% F; Mage = 32.85 | 4–14 | 4 months | ||
| Study | Intervention Group (IG) | Comparison Group (CG) | Dose | Setting | Recurrence Measure | Recurrence Reports | |
| Within Groups | Between Groups | ||||||
| Chaffin et al. 2004 [46] | IG1: PCIT; IG2: EPCIT | Standard community-based parenting group | IG1: 6 months (12–14 ses); IG2: 6 months (IG1 + individual services) | Clinic | CWS reports | n/a | Follow-up IG (19%) < CG (49%) (p < 0.02); IG1 (19%) < IG2 (36%), ns; IG2 = CG |
| Jouriles et al. 2010 [47] | Project support | TAU | 8 months: weekly ses (1–1.5 h) | Home | CPS records | n/a | Follow-up IG (5.9%) < CG (27.7%), ns |
| Kolko 1996 [48] | Individual child and parent CBT | Family Therapy | 4 months: 12 weekly ses (1 h) + 1 home ses every 2 clinic ses | Clinic and Home | Children/parents reports | - children reports: early IG/CG = late IG/CG - parents reports: early IG (45.5%) > late IG (9.1%) (p < 0.03); early CG = late CG | Late treatment - children rep: IG < CG (p < 0.007) - parents rep: IG < CG (p < 0.04) |
| Kolko et al. 2018 [49] | AF-CBT | TAU | 6 months | MHS or CWS | CWS reports | Pre IG (17%) > follow-up IG (5.3%) (p = 0.01); pre CG (13%) > follow-up CG (3%), ns | n/a |
| Lee et al. 2018 [50] | HFNY (Home visitation) | Other services | 5 years: from weekly ses, diminishing | Home | CPS records | n/a | Follow-up IG (3.3%) < CG (13.4%), ns |
| MacMillan et al. 2005 [44] | Home visitation by nurses | Standard services | 2 years: 1.5 h weekly ses for 6 months + every 2 weeks for 6 months + monthly for 12 months | Home | CPA reports | n/a | Follow-up IG (33%) < CG (43.1%), ns; hospital records: IG (23.6%) > CG (10.8%), sign |
| Runyon et al. 2010 [51] | CPC-CBT | Parent-only CBT | 4 months: 12 weekly ses (1 h), for 16 weeks | Clinic | CPA and parent/child reports | IG: 2 reports at follow-up Sign: n/a | n/a |
| Santini et al. 2017 [45] | Second unit of Projecto Parceria + coaching + VF | Wait-list parenting program 1 month after IG | 2.5 months: 8 weekly ses (50 min), 1 ses live coaching (50 min), 1 ses VF | Institution and house-lab | Observations of negative interactions | ns | n/a |
| Study | Maltreatment Risk | Parent–Child Relationship | Parental Psychopathology | Child Functioning | ||
|---|---|---|---|---|---|---|
| Parent–Child Interactions | Parenting | Family Functioning | ||||
| Chaffin et al. 2004 [46] | Child Abuse Potential Inventory (CAP) [53] | Dyadic Parent–Child Interaction Coding System (DPICS-II) [55] | Rigidity Subscale of the Child Abuse Potential Inventory (CAP) [53] | n/a | - Beck Depression Inventory (BDI) [67] - Distress and Loneliness Subscale of the Child Abuse Potential Inventory (CAP) [53] | Behavior Assessment System for Children (BASC) [69] |
| Jouriles et al. 2010 [47] | n/a | - Videotapes observations - Revised Conflict Tactics Scale (CTS-R) [56] | Parental Control of Child’s Behavior Subscales (PLOC) [61] | n/a | Symptoms Checklist-90-Revised (SCL-90-R) [68] | n/a |
| Kolko, 1996 [48] | - Child Abuse Potential Inventory (CAP) [53] - Weekly Report of Abuse Indicators (WRAI) [48] | - Conflict Tactics Scale (CTS) [57] | Parenting Scale (PS) [62] | - Cohesion Subscale of the Family Environment Scale (FES) [65] - General Functioning Subscale of the Family Assessment Device (FAD) [66] | Beck Depression Inventory (BDI) [67] | n/a |
| Kolko et al. 2018 [49] | - Weekly Report of Abuse Indicators (WRAI) [48] - Brief Child Abuse Potential Inventory (B-CAP) [54] | The Parent–Child Conflict Tactics Scale (CTS-PC) [58] | Alabama Parenting Questionnaire (APQ) [63] | - Family Conflict Subscale of the Brief Child Abuse Potential Inventory (B-CAP) [54] - General Functioning Subscale of the Family Assessment Device (FAD) [66] | n/a | - Vanderbilt ADHD Diagnostic Parent Rating Scale (VADPRS) [70] - Child PTSD Symptom Scale (CPSS) [71] |
| Lee et al. 2018 [50] | n/a | The Parent–Child Conflict Tactics Scale (CTS-PC) [58] | Adult- Adolescent Parenting Inventory (AAPI) [64] | n/a | n/a | n/a |
| MacMillan et al. 2005 [44] | Child Abuse Potential Inventory (CAP) [53] | Home Observation for Measurement of the Environment (HOME) [59] | Adult-Adolescent Parenting Inventory (AAPI) [65] | General Functioning Subscale of the Family Assessment Device (FAD) [66] | n/a | Revised Behavior Problem Checklist (RBPC) [72] |
| Runyon et al. 2010 [51] | n/a | n/a | Alabama Parenting Questionnaire (APQ) [66] | n/a | n/a | - PTSD section of the Schedule for Affective Disorders and Schizophrenia for School-Age Children- Present and Lifetime version (K-SADS-PL) [73] - Child Behavior Checklist (CBCL) [74] |
| Santini et al. 2017 [45] | n/a | Observational Protocol [60] | n/a | n/a | Beck Depression Inventory (BDI) [67] | Strengths and Difficulties Questionnaire SDQ [75] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morello, L.; Caputi, M.; Scaini, S.; Forresi, B. Parenting Programs to Reduce Recurrence of Child Maltreatment in the Family Environment: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 13283. https://doi.org/10.3390/ijerph192013283
Morello L, Caputi M, Scaini S, Forresi B. Parenting Programs to Reduce Recurrence of Child Maltreatment in the Family Environment: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(20):13283. https://doi.org/10.3390/ijerph192013283
Chicago/Turabian StyleMorello, Luisa, Marcella Caputi, Simona Scaini, and Barbara Forresi. 2022. "Parenting Programs to Reduce Recurrence of Child Maltreatment in the Family Environment: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 20: 13283. https://doi.org/10.3390/ijerph192013283





