A Community-Based Participatory Research Approach to Developing and Testing Social and Behavioural Interventions to Reduce the Spread of SARS-CoV-2: A Protocol for the ‘COPAR for COVID’ Programme of Research with Five Interconnected Studies in the Hong Kong Context
Abstract
:1. Introduction
2. Adoption of Self-Protecting Measures
3. Digital Health Literacy and COVID-19
4. Vaccine Hesitancy
5. Issues with Primary School Children
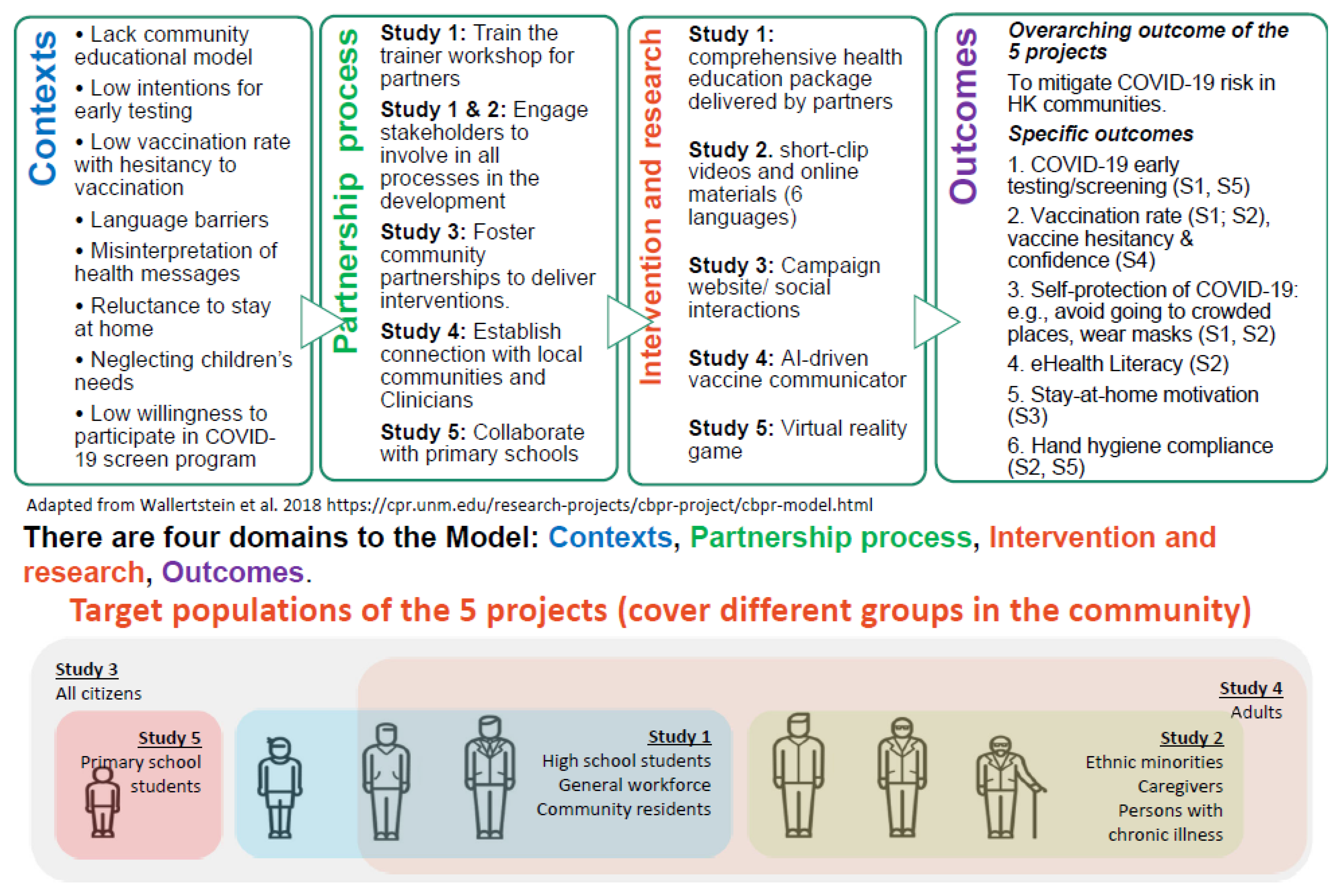
6. The Community-Based Participatory Research (CBPR) Approach
7. Study 1
7.1. Aims
7.2. Plan of Investigation
7.2.1. Subjects
7.2.2. Methods
Stage 1: Establishing the Collaboration Platform with Local Community Stakeholders
Stage 2: Pilot Study and Capacity Building for Research Partners: Train-the-Trainer (TTT) Workshops
Stage 3: Implementing the Community-Based Health Education Programmes
Stage 4: Health education model enhancement and promotion
7.2.3. Data Type, Data Processing and Analysis
8. Study 2
8.1. Aims
8.2. Plan of Investigation
8.2.1. Subjects
8.2.2. Methods
8.2.3. Study Design
8.2.4. Data Types and Data Analysis
9. Study 3
9.1. Aims
9.2. Plan of Investigation
9.2.1. Subjects
9.2.2. Methods
10. Study 4
10.1. Aims
10.2. Plan of Investigation
10.2.1. Subjects
10.2.2. Study Methods
10.2.3. Study design
10.2.4. Data Types, Processing, and Analysis
11. Study 5
11.1. Aims
- To assess the ability of a VRG-based educational intervention to enhance the knowledge and hygiene-practice compliance of primary schoolchildren in terms of the prevention of SARS-CoV-2 transmission, in comparison with a control group receiving usual community care, at 6 months after the intervention.
- To compare the bacterial loads on primary schoolchildren’s hands between the study group and the control group at 6 months after the intervention.
- To compare the detection rates of SARS-CoV-2 and other respiratory viruses in primary schoolchildren’s throat gargle samples between the study group and the control group at 6 months after the intervention.
- To compare the number of schoolchildren who participate in the community SARS-CoV-2 screening programme between the study group and the control group at 6 months after the intervention.
11.2. Plan of Investigation
11.2.1. Subjects
11.2.2. Methods
Phase 1: Pilot Study (8 Months)
Phase 2: Main Study (40 Months)
11.2.3. Study Design
11.2.4. Data Types
Hand-Hygiene Compliance (T1, T2, T3 and T4)
Awareness of Hand-Hygiene Practice (T1, T2, T3 and T4)
11.2.5. Data Analysis
12. Across All Studies, Other Common Elements Include
13. Ethics Considerations
14. Implications
15. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| CBPR | Community-based participatory research |
| CG | Professional and lay caregivers |
| COVID-19 | Coronavirus-19 |
| COPAR | Community Participatory Research |
| DHL | Digital Health Literacy |
| EM | Ethnic minority |
| GP | General practitioner |
| HK | Hong Kong |
| ITT | Intention to treat |
| KAP | Knowledge Attitude Practice |
| MI | Motivational interviewing |
| NGO | Non-governmental organisation |
| PMT | Protection Motivation Theory |
| PWCI | Patients with chronic illness |
| RAT | Rapid Antigen test |
| RCT | randomised controlled trial |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| TTT | Train-the-trainer |
| VRG | Virtual reality games |
References
- Lee, L.Y.K.; Lam, E.P.W.; Chan, C.K.; Chan, S.Y.; Chiu, M.K.; Chong, W.H.; Chu, K.W.; Hon, M.S.; Kwan, L.K.; Tsang, K.L.; et al. Practice and technique of using face mask amongst adults in the community: A cross-sectional descriptive study. BMC Public Health 2020, 20, 948. [Google Scholar] [CrossRef] [PubMed]
- Tam, V.C.; Tam, S.Y.; Poon, W.K.; Law, H.K.W.; Lee, S.W. A reality check on the use of face masks during the COVID-19 outbreak in Hong Kong. EClinicalMedicine 2020, 22, 100356. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [Green Version]
- Supporting Older People during the COVID-19 Pandemic is Everyone’s Business. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/4/supporting-older-people-during-the-covid-19-pandemic-is-everyones-business#:~:text=Support%20for%20older%20people%2C,they%20should%20fall%20il (accessed on 17 May 2021).
- GWI Coronavirus Research March 2020—Release 3: Multi-Market Research. Available online: https://www.gwi.com/hubfs/1.%20Coronavirus%20Research%20PDFs/GWI%20coronavirus%20findings%20March%202020%20-%20Multi-Market%20data%20(Release%203).pdf (accessed on 17 May 2021).
- Rathore, F.A.; Farooq, F. Information overload and infodemic in the COVID-19 pandemic. J. Pak. Med. Assoc. 2020, 70, S162–S165. [Google Scholar] [CrossRef]
- Yilmazkuday, H. Stay-at-home works to fight against COVID-19: International evidence from Google mobility data. J. Hum. Behav. Soc. Environ. 2021, 31, 210–220. [Google Scholar] [CrossRef]
- Zhao, S.Z.; Wong, J.Y.H.; Wu, Y.; Choi, E.P.H.; Wang, M.P.; Lam, T.H. Social distancing compliance under covid-19 pandemic and mental health impacts: A population-based study. Int. J. Environ. Res. Public Health 2020, 17, 6692. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef]
- Honein, M.A.; Christie, A.; Rose, D.A.; Brooks, J.T.; Meaney-Delman, D.; Cohn, A.; Sauber-Schatz, E.K.; Walker, A.; McDonald, L.C.; Liburd, L.C.; et al. Summary of guidance for public health strategies to address high levels of community transmission of sars-cov-2 and related deaths, december 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1860–1867. [Google Scholar] [CrossRef] [PubMed]
- Norman, C.D.; Skinner, H.A. eHEALS: The eHealth literacy scale. J. Med. Internet Res. 2006, 8, e507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, Y.Y.; Cheng, H.Y.; Chan, H.Y.L.; Chien, W.T.; Wong, S.Y.S. COVID-19 pandemic, infodemic and the role of eHealth literacy. Int. J. Nurs. Stud. 2020, 108, 103644. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.Y.M.; Parial, L.L.; Tolabing, M.C.; Sim, T.; Mo, P.; Okan, O.; Dadaczynski, K. Sense of coherence mediates the relationship between digital health literacy and anxiety about the future in aging population during the COVID-19 pandemic: A path analysis. Aging Ment. Health 2022, 26, 544–553. [Google Scholar] [CrossRef]
- Kor, P.P.K.; Leung, A.Y.M.; Parial, L.L.; Wong, E.M.L.; Dadaczynski, K.; Okan, O.; Amoah, P.A.; Wang, S.S.; Deng, R.; Cheung, T.C.C.; et al. Are People with Chronic Diseases Satisfied With the Online Health Information Related to COVID-19 during the Pandemic? J. Nurs. Scholarsh. 2021, 53, 75–86. [Google Scholar] [CrossRef]
- Wong, D.K.; Cheung, M.K. Online health information seeking and ehealth literacy among patients attending a primary care clinic in Hong Kong: A cross-sectional survey. J. Med. Internet Res. 2019, 21, e10831. [Google Scholar] [CrossRef] [Green Version]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Groenewoud, R.; Rachor, G.S.; Asmundson, G.J.G. A proactive approach for managing COVID-19: The importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front. Psychol. 2020, 11, 575950. [Google Scholar] [CrossRef]
- Gagneur, A.; Lemaître, T.; Gosselin, V.; Farrands, A.; Carrier, N.; Petit, G.; Valiquette, L.; De Wals, P. A postpartum vaccination promotion intervention using motivational interviewing techniques improves short-term vaccine coverage: PromoVac study. BMC Public Health 2018, 18, 811. [Google Scholar] [CrossRef]
- Leung, S.F.; Ma, J.; Russell, J. Enhancing motivation to change in eating disorders with an online self-help program. Int. J. Ment. Health Nurs. 2013, 22, 329–339. [Google Scholar] [CrossRef]
- Szablewski, C.M.; Chang, K.T.; Brown, M.M.; Chu, V.T.; Yousaf, A.R.; Anyalechi, N.; Aryee, P.A.; Kirking, H.L.; Lumsden, M.; Mayweather, E. SARS-CoV-2 transmission and infection among attendees of an overnight camp—Georgia, June 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1023. [Google Scholar] [CrossRef] [PubMed]
- Gurdasani, D.; Alwan, N.A.; Greenhalgh, T.; Hyde, Z.; Johnson, L.; McKee, M.; Michie, S.; Prather, K.A.; Rasmussen, S.D.; Reicher, S.; et al. School reopening without robust COVID-19 mitigation risks accelerating the pandemic. Lancet 2021, 397, 1177–1178. [Google Scholar] [CrossRef]
- Goldfarb, D.M.; Tilley, P.; Al-Rawahi, G.N.; Srigley, J.A.; Ford, G.; Pedersen, H.; Pabbi, A.; Hannam-Clark, S.; Charles, M.; Dittrick, M.; et al. Self-Collected Saline Gargle Samples as an Alternative to Health Care Worker-Collected Nasopharyngeal Swabs for COVID-19 Diagnosis in Outpatients. J. Clin. Microbiol. 2021, 59, e02427-20. [Google Scholar] [CrossRef] [PubMed]
- Parong, J.; Mayer, R.E. Learning science in immersive virtual reality. J. Educ. Psychol. 2018, 110, 785–797. [Google Scholar] [CrossRef]
- Chiviacowsky, S.; Wulf, G.; de Medeiros, F.L.; Kaefer, A.; Wally, R. Self-controlled feedback in 10-year-old children: Higher feedback frequencies enhance learning. Res. Q. Exerc. Sport 2008, 79, 122–127. [Google Scholar] [CrossRef]
- Clack, L.; Hirt, C.; Wenger, M.; Saleschus, D.; Kunz, A.; Sax, H. Virtue-a virtual reality trainer for hand hygiene. In Proceedings of the 2018 9th International Conference on Information, Intelligence, Systems and Applications (IISA), Zakynthos, Greece, 23–25 July 2018; pp. 1–2. [Google Scholar]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of community-based research: Assessing partnership approaches to improve public health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef] [Green Version]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B.; Allen, A.J.; Guzman, J.R.; Lichtenstein, R. Critical issues in developing and following CBPR principles. Community-Based Particip. Res. Health Adv. Soc. Health Equity 2017, 3, 32–35. [Google Scholar]
- Leung, M.W.; Yen, I.H.; Minkler, M. Community-based participatory research: A promising approach for increasing epidemiology’s relevance in the 21st century. Int. J. Epidemiol. 2004, 33, 499–506. [Google Scholar] [CrossRef] [Green Version]
- Ye, Y.; Zhang, Q.; Cao, Z.; Dajun Zeng, D. Optimal vaccination program for two infectious diseases with cross-immunity spreading on a network. Europhys. Lett. 2021, 133, 46001. [Google Scholar] [CrossRef]
- Muller, K.E.; Barón, A.E.; Kreidler, S.M.; Chi, Y.-Y.; Glueck, D.H. Easy Power and Sample Size for Most of the Mixed Models You Will Ever See; Association of Clinical and Translational Statisticians (ACTS): Kansas City, KS, USA, 2013. [Google Scholar]
- Bammann, K.; Recke, C.; Albrecht, B.M.; Stalling, I.; Doerwald, F. Promoting Physical activity among older adults using community-based participatory research with an adapted PRECEDE-PROCEED model approach: The AEQUIPA/OUTDOOR ACTIVE Project. Am. J. Health Promot. 2020, 35, 409–420. [Google Scholar] [CrossRef]
- Wong, C.L.; Chen, J.; Chow, K.M.; Law, B.M.H.; Chan, D.N.S.; So, W.K.W.; Leung, A.W.Y.; Chan, C.W.H. Knowledge, attitudes and practices towards covid-19 amongst ethnic minorities in Hong Kong. Int. J. Environ. Res. Public Health 2020, 17, 7878. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Zhang, Q.; Cao, Z.; Huang, H.; Zeng, D.D. Sustainable targeted interventions to mitigate the COVID-19 pandemic: A big data-driven modeling study in Hong Kong. Chaos 2021, 31, 101104. [Google Scholar] [CrossRef]
- Wallerstein, N.; Oetzel, J.G.; Duran, B.; Magarati, M.; Pearson, C.; Belone, L.; Davis, J.; DeWindt, L.; Kastelic, S.; Lucero, J.; et al. Culture-centeredness in community-based participatory research: Contributions to health education intervention research. Health Educ. Res. 2019, 34, 372–388. [Google Scholar] [CrossRef] [PubMed]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Pecorelli, S. Assessing COVID-19 vaccine literacy: A preliminary online survey. Hum. Vaccines Immunother. 2021, 17, 1304–1312. [Google Scholar] [CrossRef] [PubMed]
- Young, H.M.L.; Goodliffe, S.; Madhani, M.; Phelps, K.; Regen, E.; Locke, A.; Burton, J.O.; Singh, S.J.; Smith, A.C.; Conroy, S. Co-producing progression criteria for feasibility studies: A partnership between patient contributors, clinicians and researchers. Int. J. Environ. Res. Public Health 2019, 16, 3756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conard, S. Best practices in digital health literacy. Int. J. Cardiol. 2019, 292, 277–279. [Google Scholar] [CrossRef]
- Dodson, S.; Good, S.; Osborne, R. Health Literacy Toolkit for Low and Middle-Income Countries: A Series of Information Sheets to Empower Communities and Strengthen Health Systems; WHO: Geneva, Switzerland, 2015.
- HK Digital Marketing. Available online: https://www.asiapacdigital.com/digital-marketing-insight/hk-digital-marketing-2020 (accessed on 17 May 2021).
- Chan, W.S.; Leung, A.Y. Facebook as a novel tool for continuous professional education on dementia: Pilot randomized controlled trial. J. Med. Internet Res. 2020, 22, e16772. [Google Scholar] [CrossRef]
- Van Der Vaart, R.; Drossaert, C. Development of the digital health literacy instrument: Measuring a broad spectrum of health 1.0 and health 2.0 skills. J. Med. Internet Res. 2017, 19, e6709. [Google Scholar] [CrossRef] [Green Version]
- Bates, B.R.; Moncayo, A.L.; Costales, J.A.; Herrera-Cespedes, C.A.; Grijalva, M.J. Knowledge, attitudes, and practices towards COVID-19 among Ecuadorians during the outbreak: An online cross-sectional survey. J. Community Health 2020, 45, 1158–1167. [Google Scholar] [CrossRef]
- Zhong, B.-L.; Luo, W.; Li, H.-M.; Zhang, Q.-Q.; Liu, X.-G.; Li, W.-T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef] [Green Version]
- Research Office of the Legislative Council Secretariat. Social Media Usage in HK. In Statistical Highlights; Research Office of the Legislative Council Secretariat: Hongkong, China, 2019; ISSH15/19-20. [Google Scholar]
- Jin, S.V.; Phua, J.; Lee, K.M. Telling stories about breastfeeding through Facebook: The impact of user-generated content (UGC) on pro-breastfeeding attitudes. Comput. Hum. Behav. 2015, 46, 6–17. [Google Scholar] [CrossRef]
- Hether, H.J.; Calabrese, C. Beyond liking: Inspiring user-generated content for health promotion. In Technology and Health; Elsevier: Amsterdam, The Netherlands, 2020; pp. 291–312. [Google Scholar]
- Song, H.; Omori, K.; Kim, J.; Tenzek, K.E.; Hawkins, J.M.; Lin, W.Y.; Kim, Y.C.; Jung, J.Y. Trusting social media as a source of health information: Online surveys comparing the United States, Korea, and Hong Kong. J. Med. Internet Res. 2016, 18, e4193. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.-Y.; Zhang, X.; Song, H.; Omori, K. Health information seeking in the Web 2.0 age: Trust in social media, uncertainty reduction, and self-disclosure. Comput. Hum. Behav. 2016, 56, 289–294. [Google Scholar] [CrossRef]
- Rogers, R.W. Cognitive and psychological processes in fear appeals and attitude change: A revised theory of protection motivation. In Social Psychophysiology: A Sourcebook; Guilford Press: New York, NY, USA, 1983; pp. 153–176. [Google Scholar]
- Kowalski, R.M.; Black, K.J. Protection Motivation and the COVID-19 Virus. Health Commun. 2021, 36, 15–22. [Google Scholar] [CrossRef]
- Adunlin, G.; Adedoyin, A.C.A.; Adedoyin, O.O.; Njoku, A.; Bolade-Ogunfodun, Y.; Bolaji, B. Using the protection motivation theory to examine the effects of fear arousal on the practice of social distancing during the COVID-19 outbreak in rural areas. J. Hum. Behav. Soc. Environ. 2021, 31, 168–172. [Google Scholar] [CrossRef]
- World Health Organization. WHO Strategic Communications Framework; World Health Organization: Geneva, Switzerland, 2017.
- Syred, J.; Naidoo, C.; Woodhall, S.C.; Baraitser, P. Would you tell everyone this? Facebook conversations as health promotion interventions. J. Med. Internet Res. 2014, 16, e3231. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Donner, A.; Klar, N. Design and Analysis of Cluster Randomization Trials in Health Research; Wiley: Hoboken, NJ, USA, 2000. [Google Scholar]
- When and How to Wash Your Hands. Available online: https://www.cdc.gov/handwashing/when-how-handwashing.html (accessed on 17 May 2021).
- Or, P.P.-L.; Ching, P.T.-Y.; Chung, J.W.-Y. Can flu-like absenteeism in kindergartens be reduced through hand hygiene training for both parents and their kindergarteners? J. Prim. Care Community Health 2020, 11, 2150132719901209. [Google Scholar] [CrossRef] [Green Version]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Molassiotis, A.; Xie, Y.J.; Leung, A.Y.M.; Ho, G.W.K.; Li, Y.; Leung, P.H.-M.; Wang, H.L.; Chen, C.X.R.; Tong, D.W.K.; Siu, J.Y.-m.; et al. A Community-Based Participatory Research Approach to Developing and Testing Social and Behavioural Interventions to Reduce the Spread of SARS-CoV-2: A Protocol for the ‘COPAR for COVID’ Programme of Research with Five Interconnected Studies in the Hong Kong Context. Int. J. Environ. Res. Public Health 2022, 19, 13392. https://doi.org/10.3390/ijerph192013392
Molassiotis A, Xie YJ, Leung AYM, Ho GWK, Li Y, Leung PH-M, Wang HL, Chen CXR, Tong DWK, Siu JY-m, et al. A Community-Based Participatory Research Approach to Developing and Testing Social and Behavioural Interventions to Reduce the Spread of SARS-CoV-2: A Protocol for the ‘COPAR for COVID’ Programme of Research with Five Interconnected Studies in the Hong Kong Context. International Journal of Environmental Research and Public Health. 2022; 19(20):13392. https://doi.org/10.3390/ijerph192013392
Chicago/Turabian StyleMolassiotis, Alex, Yao Jie Xie, Angela Y. M. Leung, Grace W. K. Ho, Yan Li, Polly Hang-Mei Leung, Hua Li Wang, Catherine Xiao Rui Chen, Danny W. K. Tong, Judy Yuen-man Siu, and et al. 2022. "A Community-Based Participatory Research Approach to Developing and Testing Social and Behavioural Interventions to Reduce the Spread of SARS-CoV-2: A Protocol for the ‘COPAR for COVID’ Programme of Research with Five Interconnected Studies in the Hong Kong Context" International Journal of Environmental Research and Public Health 19, no. 20: 13392. https://doi.org/10.3390/ijerph192013392





