Association of the “Weekend Warrior” and Other Physical Activity Patterns with Metabolic Syndrome in the South Korean Population
Abstract
1. Introduction
2. Methods
2.1. Data
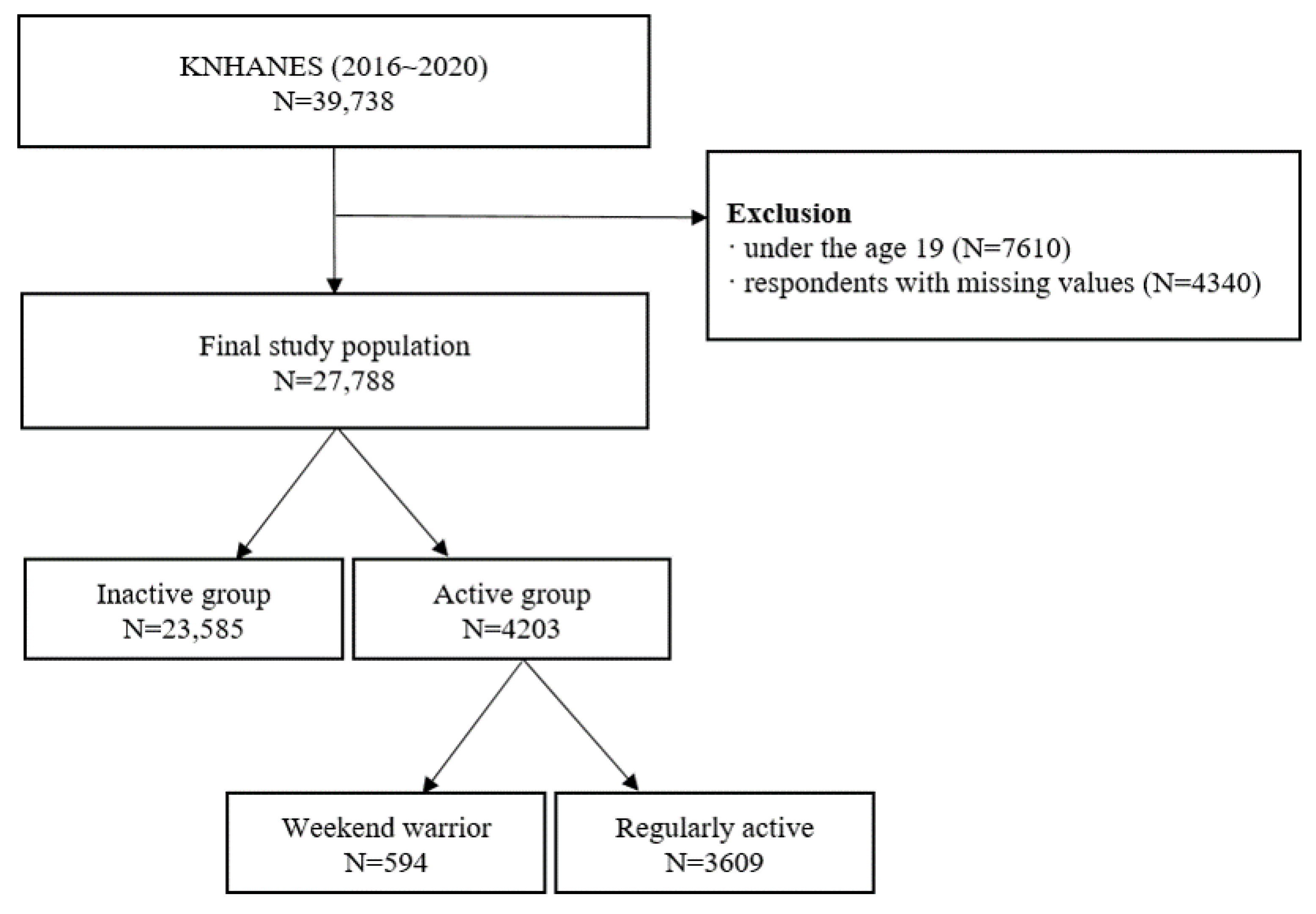
2.2. Participants
2.3. Variables
2.4. Statistical Analysis
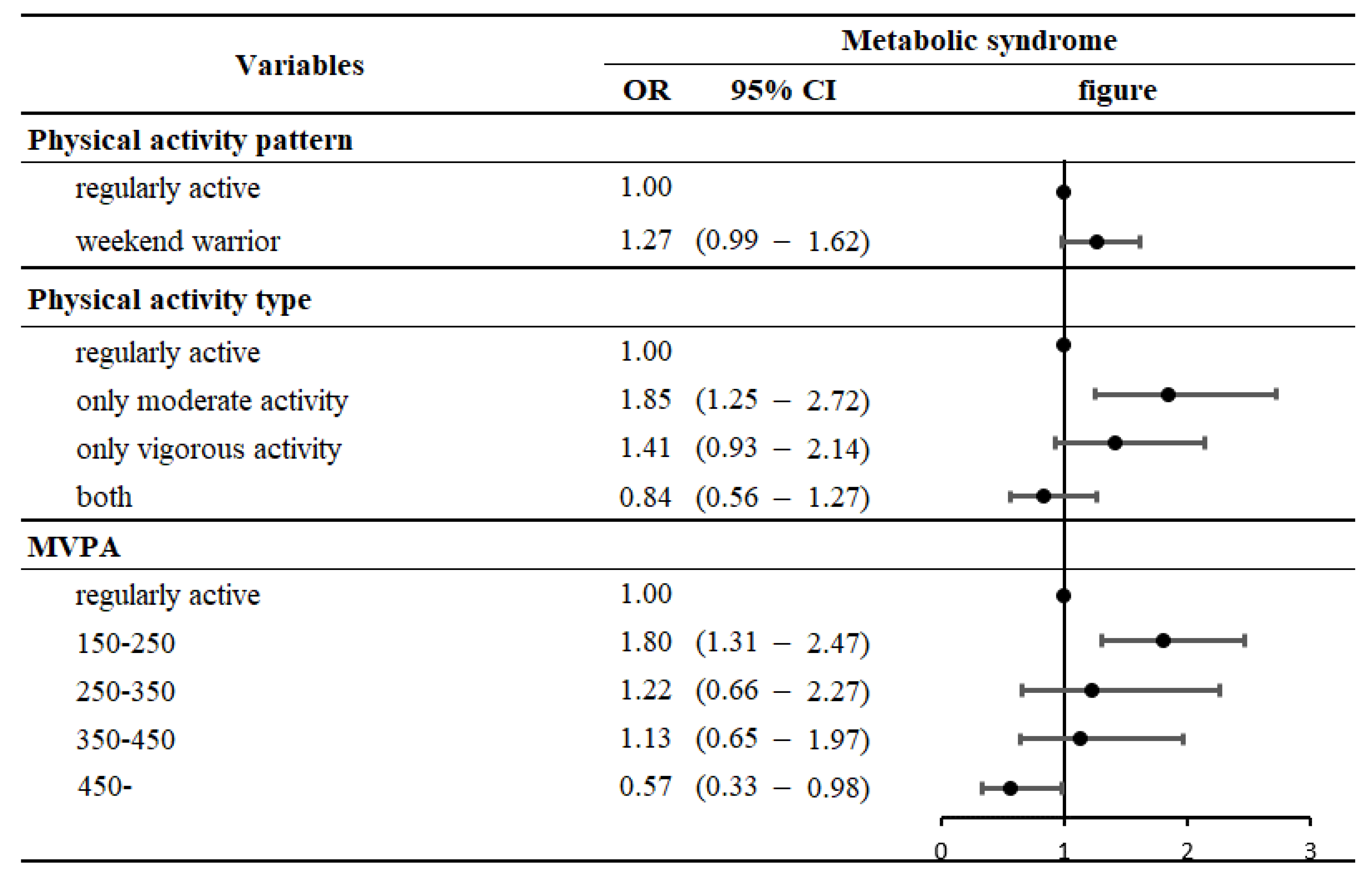
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lakka, T.A.; Bouchard, C. Physical activity, obesity and cardiovascular diseases. Handb. Exp. Pharmacol. 2005, 170, 137–163. [Google Scholar] [CrossRef]
- McTiernan, A.; Friedenreich, C.M.; Katzmarzyk, P.T.; Powell, K.E.; Macko, R.; Buchner, D.; Pescatello, L.S.; Bloodgood, B.; Tennant, B.; Vaux-Bjerke, A.; et al. Physical Activity in Cancer Prevention and Survival: A Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1252–1261. [Google Scholar] [CrossRef] [PubMed]
- Cleven, L.; Krell-Roesch, J.; Nigg, C.R.; Woll, A. The association between physical activity with incident obesity, coronary heart disease, diabetes and hypertension in adults: A systematic review of longitudinal studies published after 2012. BMC Public Health 2020, 20, 726. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Veeranki, S.P.; Magnussen, C.G.; Xi, B. Recommended physical activity and all cause and cause specific mortality in US adults: Prospective cohort study. BMJ 2020, 370, m2031. [Google Scholar] [CrossRef]
- Tomayko, E.J.; Tovar, A.; Fitzgerald, N.; Howe, C.L.; Hingle, M.D.; Murphy, M.P.; Muzaffar, H.; Going, S.B.; Hubbs-Tait, L. Parent Involvement in Diet or Physical Activity Interventions to Treat or Prevent Childhood Obesity: An Umbrella Review. Nutrients 2021, 13, 3227. [Google Scholar] [CrossRef]
- Vandercappellen, E.J.; Koster, A.; Savelberg, H.; Eussen, S.; Dagnelie, P.C.; Schaper, N.C.; Schram, M.T.; van der Kallen, C.J.H.; van Greevenbroek, M.M.J.; Wesselius, A.; et al. Sedentary behaviour and physical activity are associated with biomarkers of endothelial dysfunction and low-grade inflammation-relevance for (pre)diabetes: The Maastricht Study. Diabetologia 2022, 65, 777–789. [Google Scholar] [CrossRef]
- Calabrese, F.M.; Disciglio, V.; Franco, I.; Sorino, P.; Bonfiglio, C.; Bianco, A.; Campanella, A.; Lippolis, T.; Pesole, P.L.; Polignano, M.; et al. A Low Glycemic Index Mediterranean Diet Combined with Aerobic Physical Activity Rearranges the Gut Microbiota Signature in NAFLD Patients. Nutrients 2022, 14, 1773. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S. Reflections on Physical Activity and Health: What Should We Recommend? Can. J. Cardiol. 2016, 32, 495–504. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- O’Donovan, G.; Sarmiento, O.L.; Hamer, M. The Rise of the “Weekend Warrior”. J. Orthop. Sports Phys. Ther. 2018, 48, 604–606. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.H.; Lee, J.H.; Moon, J.S.; Sung, K.C.; Kim, J.Y.; Kang, D.R. Metabolic Syndrome Severity Score in Korean Adults: Analysis of the 2010-2015 Korea National Health and Nutrition Examination Survey. J. Korean Med. Sci. 2019, 34, e48. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Zimmet, P.; Shaw, J. The metabolic syndrome--a new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Roberts, C.K.; Hevener, A.L.; Barnard, R.J. Metabolic syndrome and insulin resistance: Underlying causes and modification by exercise training. Compr. Physiol. 2013, 3, 1–58. [Google Scholar] [CrossRef]
- Engin, A. The Definition and Prevalence of Obesity and Metabolic Syndrome. Adv. Exp. Med. Biol. 2017, 960, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Tadic, M.; Cuspidi, C.; Vasic, D.; Kerkhof, P.L.M. Cardiovascular Implications of Diabetes, Metabolic Syndrome, Thyroid Disease, and Cardio-Oncology in Women. Adv. Exp. Med. Biol. 2018, 1065, 471–488. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- He, D.; Xi, B.; Xue, J.; Huai, P.; Zhang, M.; Li, J. Association between leisure time physical activity and metabolic syndrome: A meta-analysis of prospective cohort studies. Endocrine 2014, 46, 231–240. [Google Scholar] [CrossRef]
- Zhang, D.; Liu, X.; Liu, Y.; Sun, X.; Wang, B.; Ren, Y.; Zhao, Y.; Zhou, J.; Han, C.; Yin, L.; et al. Leisure-time physical activity and incident metabolic syndrome: A systematic review and dose-response meta-analysis of cohort studies. Metabolism 2017, 75, 36–44. [Google Scholar] [CrossRef]
- Dos Santos, M.; Ferrari, G.; Lee, D.H.; Rey-López, J.P.; Aune, D.; Liao, B.; Huang, W.; Nie, J.; Wang, Y.; Giovannucci, E.; et al. Association of the “Weekend Warrior” and Other Leisure-time Physical Activity Patterns With All-Cause and Cause-Specific Mortality: A Nationwide Cohort Study. JAMA Intern. Med. 2022, 182, 840–848. [Google Scholar] [CrossRef]
- O’Donovan, G.; Lee, I.M.; Hamer, M.; Stamatakis, E. Association of “Weekend Warrior” and Other Leisure Time Physical Activity Patterns With Risks for All-Cause, Cardiovascular Disease, and Cancer Mortality. JAMA Intern. Med. 2017, 177, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.; An, J. Sex Differences in Risk Factors for Metabolic Syndrome in the Korean Population. Int. J. Environ. Res. Public Health 2020, 17, 9513. [Google Scholar] [CrossRef]
- Park, H.S.; Park, C.Y.; Oh, S.W.; Yoo, H.J. Prevalence of obesity and metabolic syndrome in Korean adults. Obes. Rev. 2008, 9, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, N.; Gyntelberg, F.; Faber, J. The appraisal of chronic stress and the development of the metabolic syndrome: A systematic review of prospective cohort studies. Endocr. Connect. 2014, 3, R55–R80. [Google Scholar] [CrossRef]
- Reis, J.P.; Loria, C.M.; Lewis, C.E.; Powell-Wiley, T.M.; Wei, G.S.; Carr, J.J.; Terry, J.G.; Liu, K. Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA 2013, 310, 280–288. [Google Scholar] [CrossRef]
- Bonomini, F.; Rodella, L.F.; Rezzani, R. Metabolic syndrome, aging and involvement of oxidative stress. Aging Dis. 2015, 6, 109–120. [Google Scholar] [CrossRef]
- Hwang, W.J.; Lee, C.Y. Effect of psychosocial factors on metabolic syndrome in male and female blue-collar workers. Jpn. J. Nurs. Sci. 2014, 11, 23–34. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines Approved by the Guidelines Review Committee. In Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- White, D.A.; Oh, Y.; Willis, E.A. The Effect of Physical Activity Bout Patterns on Metabolic Syndrome Risk Factors in Youth: National Health and Nutrition Examination Survey 2003–2006. J. Phys. Act. Health 2019, 16, 12–21. [Google Scholar] [CrossRef]
- Glazer, N.L.; Lyass, A.; Esliger, D.W.; Blease, S.J.; Freedson, P.S.; Massaro, J.M.; Murabito, J.M.; Vasan, R.S. Sustained and shorter bouts of physical activity are related to cardiovascular health. Med. Sci. Sports Exerc. 2013, 45, 109–115. [Google Scholar] [CrossRef]
- Metzger, J.S.; Catellier, D.J.; Evenson, K.R.; Treuth, M.S.; Rosamond, W.D.; Siega-Riz, A.M. Associations between patterns of objectively measured physical activity and risk factors for the metabolic syndrome. Am. J. Health Promot. 2010, 24, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.; Janssen, I. Is the frequency of weekly moderate-to-vigorous physical activity associated with the metabolic syndrome in Canadian adults? Appl. Physiol. Nutr. Metab. 2013, 38, 773–778. [Google Scholar] [CrossRef][Green Version]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C.; et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995, 273, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Sesso, H.D.; Oguma, Y.; Paffenbarger, R.S., Jr. The “weekend warrior” and risk of mortality. Am. J. Epidemiol. 2004, 160, 636–641. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Chu, M.; Shen, H.; Ren, W.; Li, Z.; Hua, T.; Xu, H.; Liang, Y.; Gao, Y.; Zhuang, X. Relationship of “weekend warrior” and regular physical activity patterns with metabolic syndrome and its associated diseases among Chinese rural adults. J. Sports Sci. 2018, 36, 1963–1971. [Google Scholar] [CrossRef]
- Alaca, N.; Uslu, S.; Gulec Suyen, G.; Ince, U.; Serteser, M.; Kurtel, H. Effects of different aerobic exercise frequencies on streptozotocin-nicotinamide-induced type 2 diabetic rats: Continuous versus short bouts and weekend warrior exercises. J. Diabetes 2018, 10, 73–84. [Google Scholar] [CrossRef]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef]
- Thompson, P.D.; Crouse, S.F.; Goodpaster, B.; Kelley, D.; Moyna, N.; Pescatello, L. The acute versus the chronic response to exercise. Med. Sci. Sports Exerc. 2001, 33, S438–S445. [Google Scholar] [CrossRef]
- Gill, J.M.; Hardman, A.E. Exercise and postprandial lipid metabolism: An update on potential mechanisms and interactions with high-carbohydrate diets (review). J. Nutr. Biochem. 2003, 14, 122–132. [Google Scholar] [CrossRef]
- Tsetsonis, N.V.; Hardman, A.E.; Mastana, S.S. Acute effects of exercise on postprandial lipemia: A comparative study in trained and untrained middle-aged women. Am. J. Clin. Nutr. 1997, 65, 525–533. [Google Scholar] [CrossRef]
- Pay, H.E.; Hardman, A.E.; Jones, G.J.; Hudson, A. The acute effects of low-intensity exercise on plasma lipids in endurance-trained and untrained young adults. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 64, 182–186. [Google Scholar] [CrossRef] [PubMed]
| Variables | Metabolic Syndrome | |||||||
|---|---|---|---|---|---|---|---|---|
| Total | Yes | No | p–Value | |||||
| N | % | N | % | N | % | |||
| Total | 27,788 | 100.0 | 7837 | 28.2 | 19,951 | 71.8 | ||
| Physical activity patterns | <0.0001 | |||||||
| Regularly active | 3609 | 13.0 | 715 | 19.8 | 2894 | 80.2 | ||
| Weekend warrior | 594 | 2.1 | 155 | 26.1 | 439 | 73.9 | ||
| Inactive | 23,585 | 84.9 | 6967 | 29.5 | 16,618 | 70.5 | ||
| Sex | <0.0001 | |||||||
| Male | 12,302 | 44.3 | 4008 | 32.6 | 8294 | 67.4 | ||
| Female | 15,486 | 55.7 | 3829 | 24.7 | 11,657 | 75.3 | ||
| Age | <0.0001 | |||||||
| 19–29 | 3504 | 12.6 | 289 | 8.2 | 3215 | 91.8 | ||
| 30–39 | 4240 | 15.3 | 750 | 17.7 | 3490 | 82.3 | ||
| 40–49 | 5089 | 18.3 | 1256 | 24.7 | 3833 | 75.3 | ||
| 50–59 | 5313 | 19.1 | 1622 | 30.5 | 3691 | 69.5 | ||
| 60–69 | 5001 | 18.0 | 1914 | 38.3 | 3087 | 61.7 | ||
| 70– | 4641 | 16.7 | 2006 | 43.2 | 2635 | 56.8 | ||
| Marital status | <0.0001 | |||||||
| Married | 19,029 | 68.5 | 5602 | 29.4 | 13,427 | 70.6 | ||
| Single, widow | 7311 | 26.3 | 1762 | 24.1 | 5549 | 75.9 | ||
| Divorced, Separated | 1448 | 5.2 | 473 | 32.7 | 975 | 67.3 | ||
| Educational level | <0.0001 | |||||||
| Middle school or below | 8038 | 28.9 | 3335 | 41.5 | 4703 | 58.5 | ||
| High school | 9186 | 33.1 | 2325 | 25.3 | 6861 | 74.7 | ||
| College or over | 10,564 | 38.0 | 2177 | 20.6 | 8387 | 79.4 | ||
| Household income | <0.0001 | |||||||
| Low | 5105 | 18.4 | 1995 | 39.1 | 3110 | 60.9 | ||
| Mid–low | 6750 | 24.3 | 2023 | 30.0 | 4727 | 70.0 | ||
| Mid–high | 7633 | 27.5 | 1943 | 25.5 | 5690 | 74.5 | ||
| High | 8300 | 29.9 | 1876 | 22.6 | 6424 | 77.4 | ||
| Region | <0.0001 | |||||||
| Metropolitan | 12,275 | 44.2 | 3228 | 26.3 | 9047 | 73.7 | ||
| Urban | 10,294 | 37.0 | 2828 | 27.5 | 7466 | 72.5 | ||
| Rural | 5219 | 18.8 | 1781 | 34.1 | 3438 | 65.9 | ||
| Occupational categories | <0.0001 | |||||||
| White | 7027 | 25.3 | 1515 | 21.6 | 5512 | 78.4 | ||
| Pink | 3637 | 13.1 | 927 | 25.5 | 2710 | 74.5 | ||
| Blue | 6333 | 22.8 | 2106 | 33.3 | 4227 | 66.7 | ||
| Inoccupation | 10,791 | 38.8 | 3289 | 30.5 | 7502 | 69.5 | ||
| Current smoking status | <0.0001 | |||||||
| Non–smoker | 16,676 | 60.0 | 4208 | 25.2 | 12,468 | 74.8 | ||
| Ex–smoker | 6163 | 22.2 | 2002 | 32.5 | 4161 | 67.5 | ||
| Current–smoker | 4949 | 17.8 | 1627 | 32.9 | 3322 | 67.1 | ||
| Current drinking status | <0.0001 | |||||||
| Never or occasionally | 7621 | 27.4 | 2532 | 33.2 | 5089 | 66.8 | ||
| 2~4 times/month | 14,105 | 50.8 | 3371 | 23.9 | 10,734 | 76.1 | ||
| 2~4 times/week | 6062 | 21.8 | 1934 | 31.9 | 4128 | 68.1 | ||
| Year | 0.0055 | |||||||
| 2016 | 5558 | 20.0 | 1571 | 28.3 | 3987 | 71.7 | ||
| 2017 | 5549 | 20.0 | 1474 | 26.6 | 4075 | 73.4 | ||
| 2018 | 5724 | 20.6 | 1594 | 27.8 | 4130 | 72.2 | ||
| 2019 | 5740 | 20.7 | 1645 | 28.7 | 4095 | 71.3 | ||
| 2020 | 5217 | 18.8 | 1553 | 29.8 | 3664 | 70.2 | ||
| Variables | Metabolic Syndrome | ||||
|---|---|---|---|---|---|
| OR | 95% CI | ||||
| Physical activity patterns | |||||
| Regularly active | 1.00 | ||||
| Weekend warrior | 1.29 | (1.02 | – | 1.65) | |
| Inactive | 1.38 | (1.25 | – | 1.53) | |
| Sex | |||||
| male | 1.90 | (1.73 | – | 2.08) | |
| female | 1.00 | ||||
| Age | |||||
| 19–29 | 1.00 | ||||
| 30–39 | 2.88 | (2.40 | – | 3.45) | |
| 40–49 | 4.37 | (3.64 | – | 5.25) | |
| 50–59 | 5.60 | (4.65 | – | 6.74) | |
| 60–69 | 6.19 | (5.11 | – | 7.49) | |
| 70– | 6.81 | (5.62 | – | 8.25) | |
| Marital status | |||||
| Married | 1.00 | ||||
| Single, widow | 1.21 | (1.10 | – | 1.33) | |
| Divorced, Separated | 1.00 | (0.87 | – | 1.15) | |
| Educational level | |||||
| Middle school or below | 1.62 | (1.45 | – | 1.81) | |
| High school | 1.19 | (1.08 | – | 1.30) | |
| College or over | 1.00 | ||||
| Household income | |||||
| Low | 1.00 | ||||
| Mid–low | 0.91 | (0.82 | – | 1.01) | |
| Mid–high | 0.86 | (0.77 | – | 0.96) | |
| High | 0.81 | (0.72 | – | 0.91) | |
| Region | |||||
| Metropolitan | 1.00 | ||||
| Urban | 1.06 | (0.98 | – | 1.14) | |
| Rural | 1.12 | (1.02 | – | 1.24) | |
| Occupational categories | |||||
| White | 1.00 | (0.91 | – | 1.11) | |
| Pink | 1.00 | (0.90 | – | 1.12) | |
| Blue | 0.85 | (0.77 | – | 0.93) | |
| Inoccupation | 1.00 | ||||
| Current smoking status | |||||
| Non–smoker | 1.00 | ||||
| Ex–smoker | 0.99 | (0.89 | – | 1.09) | |
| Current–smoker | 1.21 | (1.09 | – | 1.35) | |
| Current drinking status | |||||
| Never or occasionally | 1.00 | ||||
| 2~4 times/month | 0.89 | (0.82 | – | 0.97) | |
| 2~4 times/week | 1.06 | (0.95 | – | 1.17) | |
| Year | |||||
| 2016 | 1.00 | ||||
| 2017 | 0.89 | (0.79 | – | 1.00) | |
| 2018 | 0.98 | (0.87 | – | 1.09) | |
| 2019 | 1.06 | (0.95 | – | 1.19) | |
| 2020 | 1.09 | (0.98 | – | 1.22) | |
| Metabolic Syndrome | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Regularly Active | Weekend Warrior | Inactive | ||||||||
| OR | OR | 95% CI | OR | 95% CI | ||||||
| Sex | ||||||||||
| male | 1.00 | 1.14 | (0.87 | – | 1.50) | 1.41 | (1.24 | – | 1.60) | |
| female | 1.00 | 1.70 | (1.00 | – | 2.89) | 1.43 | (1.20 | – | 1.70) | |
| Age | ||||||||||
| 19–29 | 1.00 | 1.29 | (0.62 | – | 2.70) | 1.38 | (0.97 | – | 1.96) | |
| 30–39 | 1.00 | 1.14 | (0.64 | – | 2.02) | 1.07 | (0.81 | – | 1.41) | |
| 40–49 | 1.00 | 1.11 | (0.62 | – | 1.98) | 1.81 | (1.41 | – | 2.32) | |
| 50–59 | 1.00 | 1.49 | (0.94 | – | 2.36) | 1.58 | (1.26 | – | 1.98) | |
| 60–69 | 1.00 | 1.45 | (0.81 | – | 2.58) | 1.33 | (1.08 | – | 1.64) | |
| 70 – | 1.00 | 0.99 | (0.32 | – | 3.03) | 1.00 | (0.73 | – | 1.35) | |
| Marital status | ||||||||||
| Married | 1.00 | 1.35 | (1.02 | – | 1.79) | 1.38 | (1.22 | – | 1.56) | |
| Single, widow | 1.00 | 1.10 | (0.64 | – | 1.89) | 1.31 | (1.04 | – | 1.67) | |
| Divorced, Separated | 1.00 | 1.19 | (0.37 | – | 3.86) | 1.96 | (1.14 | – | 3.36) | |
| Household income | ||||||||||
| Low | 1.00 | 3.78 | (1.24 | – | 11.52) | 1.40 | (1.03 | – | 1.91) | |
| Mid–low | 1.00 | 0.77 | (0.45 | – | 1.30) | 1.25 | (1.00 | – | 1.56) | |
| Mid–high | 1.00 | 1.45 | (0.92 | – | 2.27) | 1.23 | (1.01 | – | 1.49) | |
| High | 1.00 | 1.27 | (0.89 | – | 1.82) | 1.63 | (1.38 | – | 1.93) | |
| Occupational categories | ||||||||||
| White | 1.00 | 1.24 | (0.83 | – | 1.87) | 1.46 | (1.20 | – | 1.76) | |
| Pink | 1.00 | 1.29 | (0.66 | – | 2.51) | 1.30 | (0.97 | – | 1.75) | |
| Blue | 1.00 | 1.52 | (0.94 | – | 2.45) | 1.44 | (1.13 | – | 1.85) | |
| Inoccupation | 1.00 | 1.07 | (0.61 | – | 1.87) | 1.38 | (1.16 | – | 1.63) | |
| Physical Activity Patterns | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Regularly Active | Weekend Warrior | Inactive | ||||||||
| OR | OR | 95% CI | OR | 95% CI | ||||||
| Metabolic syndrome components | Abdominal obesity | 1.00 | 0.96 | (0.76 | – | 1.21) | 1.21 | (1.10 | – | 1.34) |
| High BP | 1.00 | 0.99 | (0.79 | – | 1.23) | 0.99 | (0.90 | – | 1.09) | |
| Low HDL | 1.00 | 1.24 | (0.99 | – | 1.55) | 1.36 | (1.23 | – | 1.49) | |
| High TG | 1.00 | 1.26 | (1.01 | – | 1.58) | 1.24 | (1.13 | – | 1.37) | |
| High Glucose | 1.00 | 1.06 | (0.85 | – | 1.32) | 1.18 | (1.08 | – | 1.30) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, Y.S.; Joo, H.J.; Jung, Y.H.; Park, E.-C.; Jang, S.-Y. Association of the “Weekend Warrior” and Other Physical Activity Patterns with Metabolic Syndrome in the South Korean Population. Int. J. Environ. Res. Public Health 2022, 19, 13434. https://doi.org/10.3390/ijerph192013434
Jang YS, Joo HJ, Jung YH, Park E-C, Jang S-Y. Association of the “Weekend Warrior” and Other Physical Activity Patterns with Metabolic Syndrome in the South Korean Population. International Journal of Environmental Research and Public Health. 2022; 19(20):13434. https://doi.org/10.3390/ijerph192013434
Chicago/Turabian StyleJang, Yun Seo, Hye Jin Joo, Yun Hwa Jung, Eun-Cheol Park, and Suk-Yong Jang. 2022. "Association of the “Weekend Warrior” and Other Physical Activity Patterns with Metabolic Syndrome in the South Korean Population" International Journal of Environmental Research and Public Health 19, no. 20: 13434. https://doi.org/10.3390/ijerph192013434
APA StyleJang, Y. S., Joo, H. J., Jung, Y. H., Park, E.-C., & Jang, S.-Y. (2022). Association of the “Weekend Warrior” and Other Physical Activity Patterns with Metabolic Syndrome in the South Korean Population. International Journal of Environmental Research and Public Health, 19(20), 13434. https://doi.org/10.3390/ijerph192013434








