Management of Traumatic and Non-Traumatic Cerebrospinal Fluid Rhinorrhea—Experience from Three Southeast Asian Countries
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Characteristics
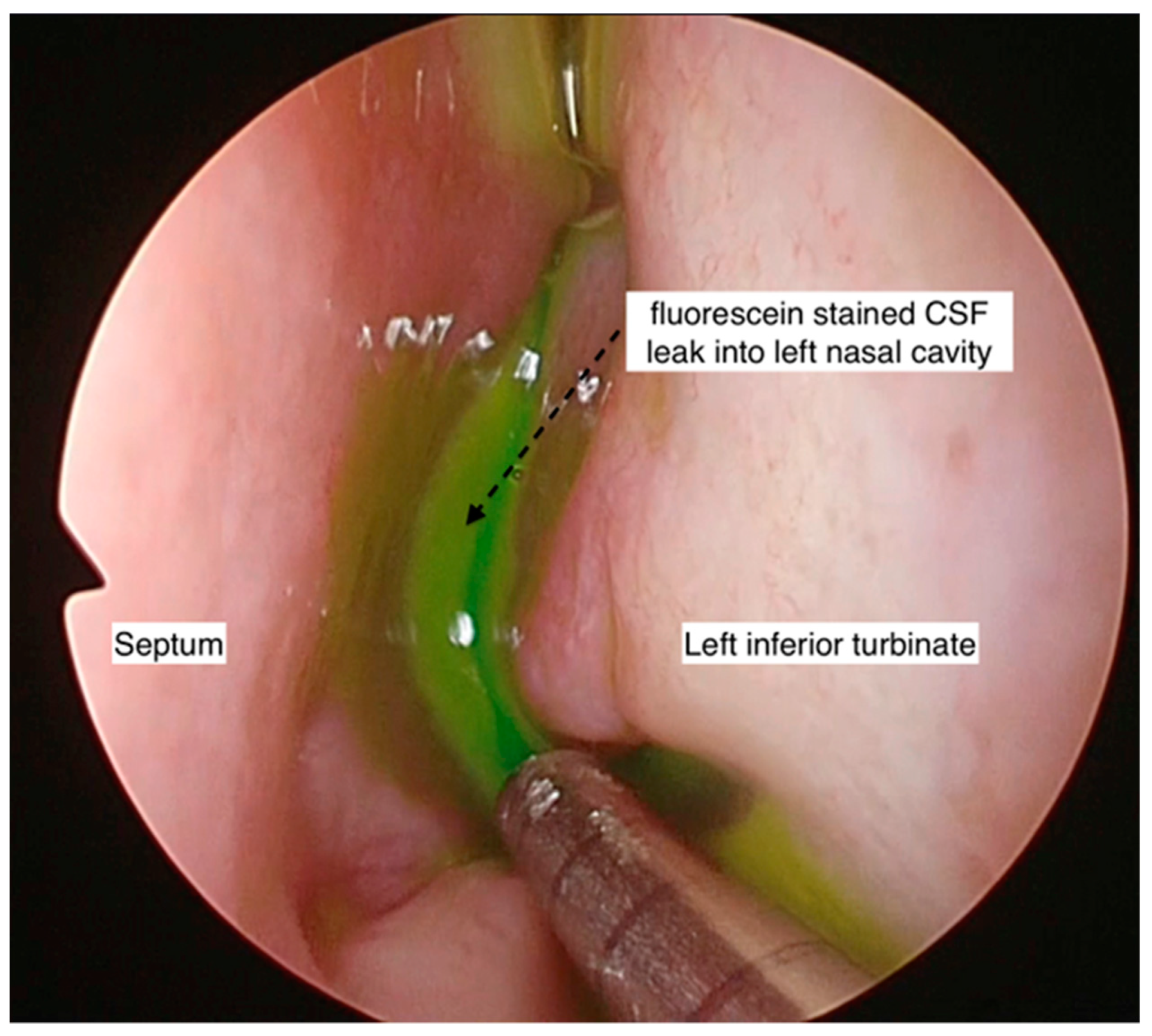
3.2. Methods in the Confirmation of Site of Leak
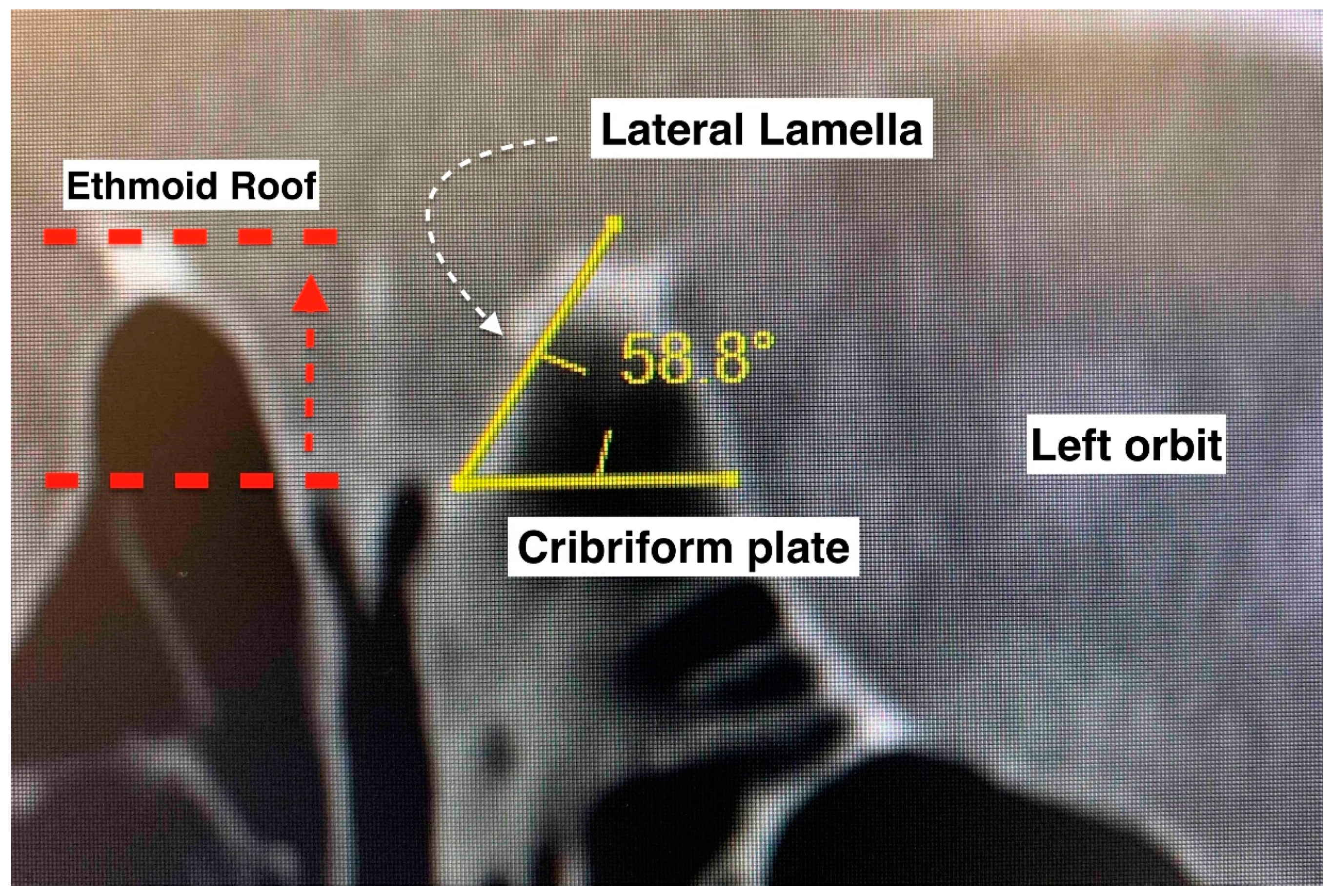
3.3. The Anterior Skull Base Configuration
3.4. Treatment and Outcomes
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ommaya, A.K.; Di Chiro, G.; Baldwin, M.; Pennybacker, J.B. Non-traumatic cerebrospinal fluid rhinorrhoea. J. Neurol. Neurosurg. Psychiatry 1968, 31, 214–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, M.; Zhou, K.; Kachra, S.; McHugh, T.; Sommer, D.D. Diagnosis and localization of cerebrospinal fluid rhinorrhea: A systematic review. Am. J. Rhinol. Allergy 2022, 36, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.L. Whence pseudotumor ceribri? J. Clin. Neuroophthalmol. 1985, 5, 55–56. [Google Scholar] [PubMed]
- Lobo, B.C.; Baumanis, M.M.; Nelson, R.F. Surgical repair of spontaneous cerebrospinal fluid (CSF) leaks: A systematic review. Laryngoscope Investig. Otolaryngol. 2017, 2, 215–224. [Google Scholar] [CrossRef]
- LeVay, A.J.; Kveton, J.F. Relationship between obesity, obstructive sleep apnea, and spontaneous cerebrospinal fluid otorrhea. Laryngoscope 2008, 118, 275–278. [Google Scholar] [CrossRef]
- Nelson, R.F.; Roche, J.P.; Gantz, B.J.; Hansen, M.R. Middle Cranial Fossa (MCF) approach without the use of lumbar drain for the management of spontaneous cerebral spinal Fluid (CSF) Leaks. Otol. Neurotol. 2016, 37, 1625–1629. [Google Scholar] [CrossRef] [Green Version]
- Kutz, J.W., Jr.; Husain, I.A.; Isaacson, B.; Roland, P.S. Management of spontaneous cerebrospinal fluid otorrhea. Laryngoscope 2008, 118, 2195–2199. [Google Scholar] [CrossRef]
- Jiang, Z.Y.; McLean, C.; Perez, C.; Barnett, S.; Friedman, D.; Batra, P.S. Surgical Outcomes and Postoperative Management in Spontaneous Cerebrospinal Fluid Rhinorrhea. J. Neurol. Surg. B Skull Base 2018, 79, 193–199. [Google Scholar] [CrossRef]
- Thapa, A.J.; Lei, B.X.; Zheng, M.G.; Li, Z.J.; Liu, Z.H.; Deng, Y.F. The Surgical Treatment of Posttraumatic Skull Base Defects with Cerebrospinal Fluid Leak. J. Neurol. Surg. B Skull Base 2018, 79, 205–216. [Google Scholar] [CrossRef]
- Keros, P. On the practical value of differences in the level of the lamina cribrosa of the ethmoid. Z. Laryngol. Rhinol. Otol. Ihre Grenzgeb 1962, 41, 808–813. [Google Scholar]
- Gera, R.; Mozzanica, F.; Karligkiotis, A.; Preti, A.; Bandi, F.; Gallo, S.; Schindler, A.; Bulgheroni, C.; Ottaviani, F.; Castelnuovo, P. Lateral lamella of the cribriform plate, a keystone landmark: Proposal for a novel classification system. Rhinology 2018, 56, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Preti, A.; Mozzanica, F.; Gera, R.; Gallo, S.; Zocchi, J.; Bandi, F.; Guidugli, G.; Ambrogi, F.; Yakirevitch, A.; Schindler, A.; et al. Horizontal lateral lamella as a risk factor for iatrogenic cerebrospinal fluid leak. Clinical retrospective evaluation of 24 cases. Rhinology 2018, 56, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Fadda, G.L.; Petrelli, A.; Martino, F.; Succo, G.; Castelnuovo, P.; Bignami, M.; Cavallo, G. Anatomic Variations of Ethmoid Roof and Risk of Skull Base Injury in Endoscopic Sinus Surgery: Statistical Correlations. Am. J. Rhinol. Allergy 2021, 35, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Heaton, C.M.; Goldberg, A.N.; Pletcher, S.D.; Glastonbury, C.M. Sinus anatomy associated with inadvertent cerebrospinal fluid leak during functional endoscopic sinus surgery. Laryngoscope 2012, 122, 1446–1449. [Google Scholar] [CrossRef] [PubMed]
- Prosser, J.D.; Vender, J.R.; Solares, C.A. Traumatic cerebrospinal fluid leaks. Otolaryngol. Clin. N. Am. 2011, 44, 857–873. [Google Scholar] [CrossRef]
- Sannareddy, R.R.; Rambabu, K.; Kumar, V.E.; Gnana, R.B.; Ranjan, A. Endoscopic management of CSF rhinorrhea. Neurol. India 2014, 62, 532–539. [Google Scholar] [CrossRef]
- Pérez, M.A.; Bialer, O.Y.; Bruce, B.B.; Newman, N.J.; Biousse, V. Primary spontaneous cerebrospinal fluid leaks and idiopathic intracranial hypertension. J. Neuroophthalmol. 2013, 33, 330–337. [Google Scholar] [CrossRef] [Green Version]
- Clark, D.; Bullock, P.; Hui, T.; Firth, J. Benign intracranial hypertension: A cause of CSF rhinorrhoea. J. Neurol. Neurosurg. Psychiatry 1994, 57, 847–849. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Wang, B.; Wang, C.; Liu, P. Primary spontaneous cerebrospinal fluid rhinorrhea: A symptom of idiopathic intracranial hypertension? J. Neurosurg. 2011, 115, 165–170. [Google Scholar] [CrossRef]
- Schlosser, R.J.; Woodworth, B.A.; Wilensky, E.M.; Grady, M.S.; Bolger, W.E. Spontaneous cerebrospinal fluid leaks: A variant of benign intracranial hypertension. Ann. Otol. Rhinol. Laryngol. 2006, 115, 495–500. [Google Scholar] [CrossRef]
- Sharma, S.D.; Kumar, G.; Bal, J.; Eweiss, A. Endoscopic repair of cerebrospinal fluid rhinorrhoea. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2016, 133, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Psaltis, A.J.; Schlosser, R.J.; Banks, C.A.; Yawn, J.; Soler, Z.M. A systematic review of the endoscopic repair of cerebrospinal fluid leaks. Otolaryngol. Head Neck Surg. 2012, 147, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Shetty, P.G.; Shroff, M.M.; Sahani, D.V.; Kirtane, M.V. Evaluation of high-resolution CT and MR cisternography in the diagnosis of cerebrospinal fluid fistula. AJNR Am. J. Neuroradiol. 1998, 19, 633–639. [Google Scholar] [PubMed]
- Oh, J.W.; Kim, S.H.; Whang, K. Traumatic cerebrospinal fluid leak: Diagnosis and management. Korean J. Neurotrauma 2017, 13, 63–67. [Google Scholar] [CrossRef] [Green Version]
- Vázquez, J.A.; Adducci, M.d.C.; Monzón, D.G.; Iserson, K.V. Lactic Dehydrogenase in Cerebrospinal Fluid May Differentiate between Structural and Non-Structural Central Nervous System Lesions in Patients with Diminished Levels of Consciousness. J. Emerg. Med. 2009, 37, 93–97. [Google Scholar] [CrossRef]
- Skorek, A.; Tretiakow, D.; Szmuda, T.; Przewozny, T. Is the Keros classification alone enough to identify patients with the ‘dangerous ethmoid’? An anatomical study. Acta Otolaryngol. 2017, 137, 196–201. [Google Scholar] [CrossRef]
- Phang, S.Y.; Whitehouse, K.; Lee, L.; Khalil, H.; McArdle, P.; Whitfield, P.C. Management of CSF Leak in Base of Skull Fractures in Adults. Br. J. Neurosurg. 2016, 30, 596–604. [Google Scholar] [CrossRef]
- Tilak, A.M.; Koehn, H.; Mattos, J.; Payne, S.C. Preoperative Management of Spontaneous Cerebrospinal Fluid Rhinorrhea with Acetazolamide. Int. Forum Allergy Rhinol. 2018, 9, 265–269. [Google Scholar] [CrossRef]
- Song, X.; Wang, D.; Sun, X.; Liu, Q.; Hu, L.; Gu, Y.; Zhang, H. Endoscopic repairs of sinonasal cerebrospinal leaks: Outcome and prognostic factors. J. Craniofac. Surg. 2018, 29, 182–187. [Google Scholar] [CrossRef]
- Jahanshahi, J.; Zeinalizadeh, M.; Reza Mohammadi, H.; Sadrehosseini, S.M. Endonasal endoscopic management of frontal sinus cerebrospinal fluid leak. Am. J. Rhinol. Allergy 2017, 31, 406–411. [Google Scholar] [CrossRef]
- Kreatsoulas, D.C.; Shah, V.S.; Otto, B.A.; Carrau, R.L.; Prevedello, D.M.; Hardesty, D.A. Surgical outcomes of the endonasal endoscopic approach within a standardized management protocol for repair of spontaneous cerebrospinal fluid rhinorrhea. J. Neurosurg. 2020, 134, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Sanghvi, S.; Sarna, B.; Alam, E.; Pasol, J.; Levine, C.; Casiano, R.R. Role of Adjunct Treatments for Idiopathic CSF Leaks After Endoscopic Repair. Laryngoscope 2021, 131, 41–47. [Google Scholar] [CrossRef]
- London, N.R., Jr.; Mohyeldin, A.; Montaser, A.S.; Tanjararak, K.; Prevedello, D.M.; Otto, B.A.; Carrau, R.L. Contributing factors for delayed postoperative cerebrospinal fluid leaks and suggested treatment algorithm. Int. Forum Allergy Rhinol. 2020, 10, 779–784. [Google Scholar] [CrossRef]
- Lam, K.; Luong, A.U.; Yao, W.C.; Citardi, M.J. Use of Autologous Fat Grafts for the Endoscopic Reconstruction of Skull Base Defects: Indications, Outcomes, and Complications. Am. J. Rhinol. Allergy 2018, 32, 310–317. [Google Scholar] [CrossRef] [PubMed]
- D’Anza, B.; Tien, D.; Stokken, J.K.; Recinos, P.F.; Woodard, T.R.; Sindwani, R. Role of lumbar drains in contemporary endonasal skull base surgery: Meta-analysis and systematic review. Am. J. Rhinol. Allergy 2016, 30, 430–435. [Google Scholar] [CrossRef]
- Zwagerman, N.T.; Wang, E.W.; Shin, S.S.; Chang, Y.F.; Fernandez-Miranda, J.C.; Snyderman, C.H.; Gardner, P.A. Does lumbar drainage reduce postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery? A prospective, randomized controlled trial. J. Neurosurg. 2018, 131, 1172–1178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCormack, B.; Cooper, P.R.; Persky, M.; Rothstein, S. Extracranial repair of cerebrospinal fluid fistulas: Technique and results in 37 patients. Neurosurgery 1990, 27, 412–417. [Google Scholar] [CrossRef]
- Alicandri-Ciufelli, M.; Fermi, M.; Rosa, M.S.; Garzaro, M.; Presutti, L. Spontaneous Nasal Cerebrospinal Fluid Leak Repaired with Single-Layer Mucoperichondrial Graft: Long-Term Results. Am. J. Rhinol. Allergy 2020, 34, 382–387. [Google Scholar] [CrossRef]
- Allensworth, J.J.; Rowan, N.R.; Storck, K.A.; Woodworth, B.A.; Schlosser, R.J. Endoscopic Repair of Spontaneous Skull Base Defects Decreases the Incidence Rate of Intracranial Complications. Int. Forum Allergy Rhinol. 2019, 9, 1089–1096. [Google Scholar] [CrossRef]
- Bubshait, R.F.; Moumen, A.A. The Endonasal Endoscopic Management of Cerebrospinal Fluid Rhinorrhea. Cureus 2021, 13, e13457. [Google Scholar] [CrossRef]
- Fiore, G.; Bertani, G.A.; Carrabba, G.G.; Guastella, C.; Marfia, G.; Tariciotti, L.; Gribaudi, G.L.; Mantovani, G.; Di Cristofori, A.; Locatelli, M. The “Parachute” Technique for the Endoscopic Repair of High-Flow Anterior Skull-Base CSF Leaks. World Neurosurg. 2021, 151, e880–e887. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Zhen, H.-T. Management of Cerebrospinal Fluid Rhinorrhea in the Sphenoid Sinus Lateral Recess through an Endoscopic Endonasal Transpterygoid Approach with Obliteration of the Lateral Recess. Ear Nose Throat J. 2020, 101, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Keshri, A.; Jain, R.; Manogaran, R.S.; Behari, S.; Khatri, D.; Mathialagan, A. Management of Spontaneous CSF Rhinorrhea: An Institutional Experience. J. Neurol. Surg. Part B Skull Base 2018, 80, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Kim-Orden, N.; Shen, J.; Or, M.; Hur, K.; Zada, G.; Wrobel, B. Endoscopic Endonasal Repair of Spontaneous Cerebrospinal Fluid Leaks Using Multilayer Composite Graft and Vascularized Pedicled Nasoseptal Flap Technique. Allergy Rhinol. 2019, 10, 215265671988862. [Google Scholar] [CrossRef]
- Poma, S.; Modica, D.M.; Mattina, G.; Gallina, S.; Azzolina, A.A.; Mario-Galfano, G. Skull Base Csf- Leak Closure with Autologous Fibrin Sealant. Iran J. Otorhinolaryngol. 2021, 33, 3–8. [Google Scholar]
- Rathod, R.; Virk, R.S.; Nayak, G. Plasma Ablation–Assisted Endoscopic Endonasal Transpterygoid Approach to Sphenoid Lateral Recess Cerebrospinal Fluid Leaks: Technique and Outcome. World Neurosurg. 2021, 149, e636–e645. [Google Scholar] [CrossRef]
- Workman, A.D.; Carey, R.M.; Parasher, A.K.; Kuan, E.C.; Godovchik, J.; Glicksman, J.T.; Kennedy, D.W.; Palmer, J.N.; Adappa, N.D. The Fate of the Bone Graft in Cerebrospinal Fluid Rhinorrhea Endoscopic Repair for Idiopathic Intracranial Hypertension: A Retrospective Case Series Analysis. Rhinol. J. 2017, 55, 376–381. [Google Scholar] [CrossRef]
- Xu, M.; Wang, J.; Chen, X.; Xue, T.; Chen, F. Comparison of Two Surgical Approaches in the Management of Cerebrospinal Fluid Rhinorrhea in the Lateral Recess of Sphenoid Sinus: A Retrospective Study. Ear Nose Throat J. 2022, 014556132211127. [Google Scholar] [CrossRef]
- Zhu, Z.J.; Cheng, L.; Yang, J. Transnasal Endoscopic Repair of Adult Spontaneous Cerebrospinal Fluid Rhinorrhea with Assistance of Computer-Assisted Navigation System: An Analysis of 21 Cases. Eur. Arch. Oto-Rhino-Laryngol. 2019, 276, 2835–2841. [Google Scholar] [CrossRef]
| Case | Age | Gender | Diagnosis | Cause of CSF Leak | Site of Leak | Pre-Op Imaging |
|---|---|---|---|---|---|---|
| 1 | 46 | F | IIH | Spontaneous | Cribriform plate defect | CT and MRI |
| 2 | 45 | M | Postcraniotomy leak | Iatrogenic Trauma | Posterior table of frontal sinus | CT |
| 3 | 33 | M | Previous trauma with meningitis | Non-Iatrogenic Trauma | Cribriform plate defect | CT |
| 4 | 29 | M | Industrial trauma | Non-Iatrogenic Trauma | Suprasellar/tuberculum sellae fracture line | CT |
| 5 | 40 | F | IIH | Spontaneous | Anterior cranial fossa defect (cribriform plate) | CT and MRI |
| 6 | 59 | M | Idiopathic | Spontaneous | Lt frontal sinus defect | CT and MRI |
| 7 | 66 | F | Idiopathic | Spontaneous | Rt anterior cranial fossa floor defect (cribriform plate) | CT and MRI |
| 8 | 61 | F | IIH | Spontaneous | Rt sella defect at the anterior wall | CT and MRI |
| 9 | 61 | F | IIH | Spontaneous | Sphenoid sinus defect | CT and MRI |
| 10 | 26 | M | Idiopathic | Spontaneous | Cribriform plate defect | CT and MRI |
| 11 | 81 | M | Inverted papilloma | Iatrogenic Trauma | Rt posterior table frontal sinus | CT and MRI |
| 12 | 77 | M | Nasal polyp | Iatrogenic Trauma | Rt cribriform plate | CT |
| 13 | 20 | M | RTA | Non-Iatrogenic Trauma | Rt cribriform plate | CT and MRI |
| 14 | 11 | M | Frontoethmoid mucocele | Spontaneous | Rt cribriform plate | CT and MRI |
| 15 | 16 | F | Epidural hematoma/Craniotomy | Iatrogenic Trauma | Lt cribriform plate | CT |
| Case | Keros Classification (mm) | L/R Difference (mm) | Gera Classification (Degrees) | L/R Difference (Degrees) | ||
|---|---|---|---|---|---|---|
| R | L | R | L | |||
| 1 | II (4.7) | II (4.1) | 0.5 | II (72.2) | II (78.7) | 6.5 |
| 2 | I (3.7) | II (4.3) | 0.6 | II (68.5) | II (73.5) | 5.0 |
| 3 | II (4.0) | I (3.2) | 0.8 | II (60.5) | II (68.4) | 7.9 |
| 4 | I (1.3) | I (1.2) | 0.1 | III (30.5) | III (35.0) | 4.5 |
| 5 | II (6.5) | II (4.8) | 1.7 | II (60.9) | II (76.7) | 15.8 |
| 6 | II (4.2) | I (1.7) | 2.5 | III (44.4) | III (42.8) | 1.6 |
| 7 | II (5.6) | II (5.8) | 0.2 | III (42.1) | II (66.8) | 24.7 |
| 8 | II (6.3) | II (6.2) | 0.1 | II (60.0) | II (73.1) | 13.1 |
| 9 | II (7.0) | II (6.2) | 0.8 | II (51.6) | II (63.0) | 11.4 |
| 10 | II (5.8) | II (6.8) | 1.0 | II (48.6) | II (76.1) | 27.5 |
| 11 | I (2.6) | I (3.0) | 0.4 | II (53) | II (59) | 6.0 |
| 12 | I (2.1) | I (2.8) | 0.7 | III (23) | II (56) | 33.0 |
| 13 | II (4.7) | I (3.7) | 1 | II (53) | II (61) | 8.0 |
| 14 | I (3.2) | I (3.0) | 0.2 | II (47) | II (54) | 7.0 |
| 15 | II (4.7) | II (6.3) | 1.6 | II (63) | II (69) | 6.0 |
| Type/Class | Keros n (%) | Gera n (%) |
|---|---|---|
| I | 12 (40) | 0 (0) |
| II | 18 (60) | 24 (80) |
| III | 0 (0) | 6 (20) |
| Total (sides) | 30 (100) | 30 (100) |
| Traumatic | Non-Traumatic | p Value * | |
|---|---|---|---|
| Site of leak | Cases (n = 7), n (%) | Cases (n = 8), n (%) | |
| Cribriform plate | 4 (57%) | 5 (63%) | |
| Frontal sinus | 2 (29%) | 1 (12%) | 0.64 |
| Sphenoid bone/sella/suprasellar defect | 1 (14%) | 2 (25%) | |
| Keros classification | Sides (n = 14), n (%) | Sides (n = 16), n (%) | |
| I | 9 (64%) | 3 (19%) | 0.02 |
| II | 5 (36%) | 13 (81%) | |
| III | 0 (0%) | 0 (0%) | |
| Gera classification | Sides (n = 14), n (%) | Sides (n = 16), n (%) | |
| I | 0 (0%) | 0 (0%) | 1.00 |
| II | 11 (79%) | 13 (81%) | |
| III | 3 (21%) | 3 (19%) |
| Technique of Repair | No. of Patients, n (%) | Requirement of Lumbar Drain, (n, %) | Use of Diuretics (n, %) | Duration of Hospital Stay Following Surgery (Days), Mean (SD) | Follow-up Duration (Months), Mean (SD) | Recurrent Leak, (n, %) | p Value * |
|---|---|---|---|---|---|---|---|
| Conservative management | 2 (13.3) | 0 (0) | 1 (50) | 20.5 ± 0.71 | 3.00 ± 0.00 | 0 (0) | 1.00 |
| Endoscopic multilayered closure | 13 (86.7) | 2 (15.4) | 1 (7.7) | 9.07 ± 6.17 | 5.15 ± 4.77 | 1 (7.7) ** |
| Author, Year (Country) | Study Design | No of Cases (n) | Etiology | Site of Leak (%) | Adjunct Treatment (%) | Duration of Hospital Stays (Day) | Success Rate of Primary Endoscopic Repair (%) | Immediate Postoperative Complications (%) | Recurrent Leak (%) |
|---|---|---|---|---|---|---|---|---|---|
| Alicandri-Ciufelli, 2020 (Italy) [38] | Retrospective | 29 | Spontaneous | Anterior ethmoid (79), sphenoid (14), frontal (7), posterior ethmoid (7) | None | 3–4 | 93 | Recurrent meningocele without CSF leak (3.4) | 7 |
| Allensworth, 2019 (USA) [39] | Retrospective | 222 | Spontaneous | Cribriform (25.6), lateral sphenoid (32.4), ethmoid roof (19.8), frontal (10.6) | Acetazolamide (74.3), VP shunt (19.8), Lumbar drain (82.8) | NA | 97.2 | Intracranial hematoma (1) Intracranial hemorrhage (0.45) Seizure (0.45) | 2.8 |
| Bubshait, 2021 (Saudi Arabia) [40] | Retrospective | 56 | Spontaneous 46%, Traumatic 54% | Frontal (14), ethmoid roof (25), cribriform (39), sphenoid (21), multiple (14) | Permanent VP shunt (2) | 6.5 | 93 | NA | 7 |
| Fiore, 2021 (Italy) [41] | Retrospective | 33 | Iatrogenic trauma 48.5%, non-iatrogenic trauma 15.2%, spontaneous 33.3%, tumor 3% | Sphenoid (60.6), cribriform (30.3), sphenoid/ethmoid (9.1) | Lumbar drain (100) | NA | 90.9 | NA | 9.1 |
| He, 2020 (China) [42] | Retrospective | 12 | Spontaneous | Sphenoid sinus lateral recess | 20% mannitol solution (100) | NA | 100 | None | 0 |
| Jahanshahi, 2017 (Iran) [30] | Retrospective | 24 | Traumatic 75%, spontaneous 25% | Frontal sinus | Acetazolamide (100) | NA | 95.8 | NA | 4.2 |
| Jiang, 2018 (USA) [8] | Retrospective | 48 | Spontaneous | Sphenoid (43.8), cribriform (33), ethmoid (17) | Lumbar drain (27), Acetazolamide (40) | NA | 93.8 | NA | 6.2 |
| Keshri, 2019 (India) [43] | Retrospective | 43 | Spontaneous | Sphenoid (6.9), cribriform (74.4), ethmoid (16.3), planum (2.3) | VP shunt/lumbar drain (53.4) | NA | 95.3 | Meningitis (4.7) | 4.7 |
| Kim-Orden, 2019 (USA) [44] | Retrospective | 20 | Spontaneous | Cribriform (44), ethmoid (32), lateral sphenoid (12), planum sphenoidale (12) | Lumbar drain (100),Acetazolamide (30) | 7 | 92 | None | 8 |
| Kreatsoulas, 2021 (USA) [31] | Retrospective | 46 | Spontaneous | Cribriform/ethmoid (56.6), lateral sphenoid (21.7) | permanent VP shunt (55.6), Acetazolamide (44.4) | NA | 95.7 | Seizures (2.2), Meningitis (4.4), Subdural hematoma (2.2) | 4.3 |
| Poma, 2021 (Italy) [45] | Retrospective | 20 | Traumatic | Ethmoid (65), sella (35) | NA | NA | 95 | None | 5 |
| Rathod, 2021 (India) [46] | Retrospective-prospective | 11 | Spontaneous | Sphenoid lateral recess (100) | Lumbar drain (9.1) | 4 | 90.9 | None | 9.1 |
| Sanghvi, 2020 (USA) [32] | Retrospective | 33 | Spontaneous | Cribriform (58), sphenoid lateral recess (30), multiple or bilateral (12) | Acetazolimide (9.1) Topiramate (3.0) VP shunt (9.1) | NA | 97 | None | 3 |
| Workman, 2017 (USA) [47] | Retrospective | 14 | Spontaneous | Cribriform (21.4), frontal (14.2), ethmoid roof (21.4), sphenoid (42.8), sphenoid/ethmoid (7.1) | Acetazolamide (92.9) Lumbar drain (100) VP shunt (21.4) | NA | 85.7 | NA | 14.3 |
| Xu, 2022 (China) [48] | Retrospective | 15 | NA | Lateral recess of sphenoid sinus (100) | 20% mannitol (100) | NA | 100 | Temporary numbness of upper lip or cheek (33.3) | 0 |
| Zhu, 2019 (China) [49] | Retrospective | 21 | Spontaneous | Ethmoid roof (57), cribriform (33), sphenoid (10) | 20% mannitol (100) | NA | 100 | Hyposmia (4.8) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zahedi, F.D.; Subramaniam, S.; Kasemsiri, P.; Periasamy, C.; Abdullah, B. Management of Traumatic and Non-Traumatic Cerebrospinal Fluid Rhinorrhea—Experience from Three Southeast Asian Countries. Int. J. Environ. Res. Public Health 2022, 19, 13847. https://doi.org/10.3390/ijerph192113847
Zahedi FD, Subramaniam S, Kasemsiri P, Periasamy C, Abdullah B. Management of Traumatic and Non-Traumatic Cerebrospinal Fluid Rhinorrhea—Experience from Three Southeast Asian Countries. International Journal of Environmental Research and Public Health. 2022; 19(21):13847. https://doi.org/10.3390/ijerph192113847
Chicago/Turabian StyleZahedi, Farah Dayana, Somasundaram Subramaniam, Pornthep Kasemsiri, Chenthilnathan Periasamy, and Baharudin Abdullah. 2022. "Management of Traumatic and Non-Traumatic Cerebrospinal Fluid Rhinorrhea—Experience from Three Southeast Asian Countries" International Journal of Environmental Research and Public Health 19, no. 21: 13847. https://doi.org/10.3390/ijerph192113847
APA StyleZahedi, F. D., Subramaniam, S., Kasemsiri, P., Periasamy, C., & Abdullah, B. (2022). Management of Traumatic and Non-Traumatic Cerebrospinal Fluid Rhinorrhea—Experience from Three Southeast Asian Countries. International Journal of Environmental Research and Public Health, 19(21), 13847. https://doi.org/10.3390/ijerph192113847









