Guided Endodontics: A Literature Review
Abstract
:1. Introduction
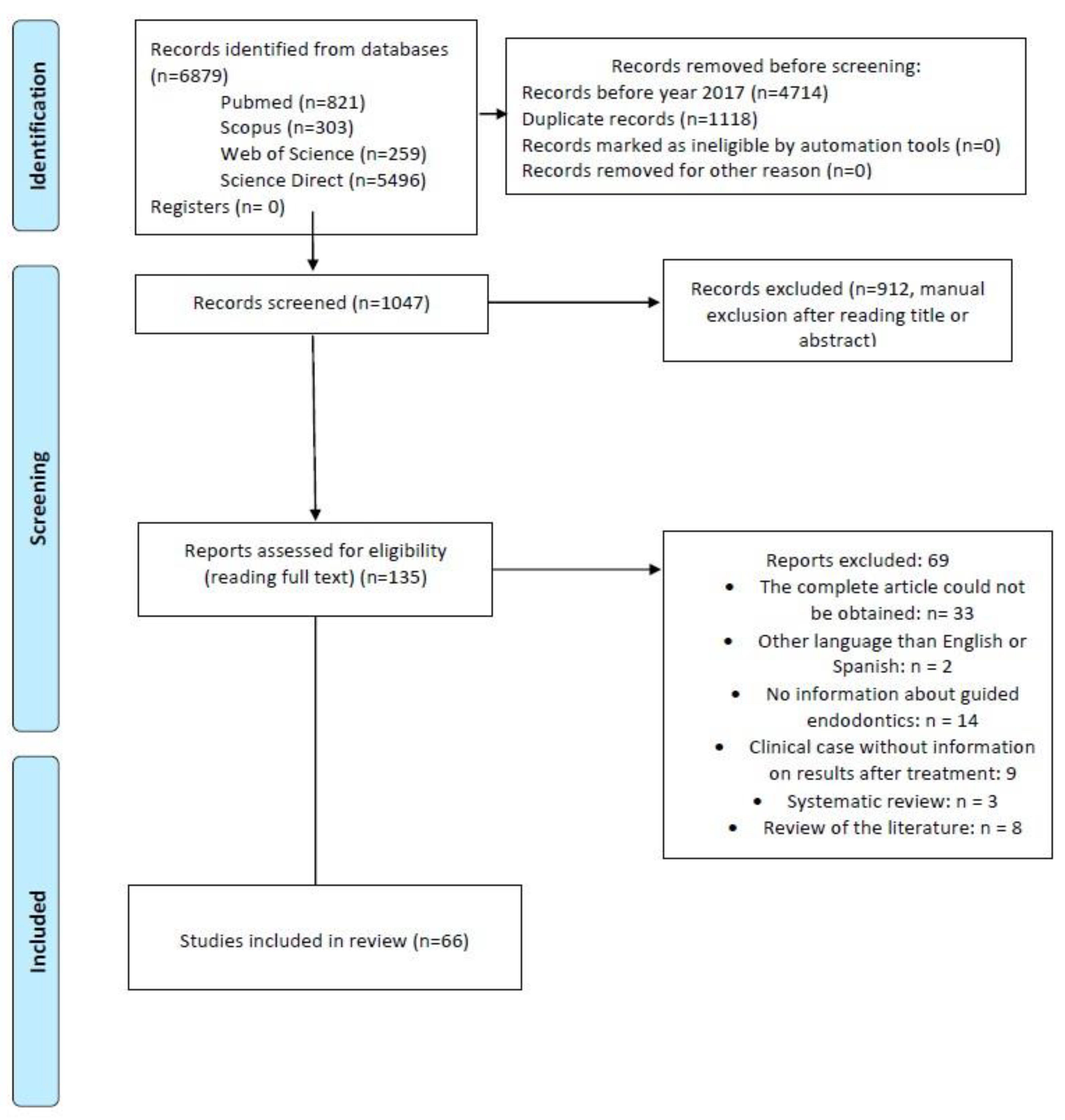
2. Materials and Methods
2.1. Inclusion Criteria
- Keywords: guided AND endodontics;
- Time period: last six years;
- Articles on guided endodontics: its types, uses, advantages, disadvantages, and/or outcomes of its use.
2.2. Exclusion Criteria
- Articles in languages other than English or Spanish;
- Animal studies;
- Reviews and systematic reviews;
- Articles that, after reading their title and abstract, did not fit in with the subject of interest of this paper.
3. Results
Studies Characteristics
| Authors | Object of Study and Type of EG | Nature of Teeth and Type | Operator and Practice | Conclusions |
|---|---|---|---|---|
| Gambarini G et al. 2020 [21] | Ultra-conservative AC precision (DGE vs. MAN) |
| operator with experience in both groups | DGE more precise, removes less tissue, reduces risk of iatrogenic coronary weakening |
| Connert T et al. 2017 [71] | SGE accuracy with miniaturized instruments |
| 2 operators | SGE is accurate, fast, and operator-independent in terms of preparing apically extensive access cavities in teeth with narrow roots. |
| Jain SD et al. 2020 [22] | Loss of tooth tissue in AC in teeth with OP (DGE vs. MAN) |
| 1 EST (with microscope for MAN access) | DGE removes less tissue and is more accurate in locating ducts with OP |
| Loureiro MAZ et al. 2020 [23] | Amount of tooth tissue removed in CA (SGE vs. MAN) |
| 1 ESP (with magnifying glasses) |
|
| Connert T et al. 2021 [24] | Time and tooth loss in AC (miniaturized DGE vs. MAN) |
| 1 operator with 12 years’ experience, 1 OP with 12 years’ experience, 1 OP with 12 years’ experience, 1 OP with 12 years’ experience. |
|
| Koch GK et al. 2022 [31] | Compare 3D printers (for SGE) |
| 1 EST |
|
| Buchgreitz J et al. 2019 [72] | SGE accuracy (in teeth with OP, apical periodontitis, and in need of post) |
| No data |
|
| Torres A et al. 2021 [32] | Accuracy and potential for use of DGE in AC teeth with simulated OP |
| 1 EST, 1 ESP Yes |
|
| Simon JC et al. 2021 [73] | Laser precision and predictability in minimally invasive CA (with DGE) |
| No data |
|
| Su Y et al. 2021 [74] | Accuracy in AC Linear and angular deviation during AC (with SGE) |
| No data |
|
| Krug R et al. 2020 [33] | Accuracy and effort of 2 AC software (with SGE) |
| 1 operator |
|
| Choi Y et al. 2021 [75] | Effectiveness in CA with guidelines to prevent excessive tooth loss (student-oriented) (with SGE) |
| 1 EST pre-doctoral |
|
| Ali A et al. 2021 [25] |
|
| Same operator (with magnifiers for MAN) |
|
| Dianat O et al. 2020 [26] | Accuracy and efficiency when locating ducts with OP (DGE vs. MAN) |
| 1ESP AND 1 EST (2 per group) |
|
| Chong BS et al. 2019 [76] | Use of DGE for guided endodontics |
| No data |
|
| Kostunov J et al. 2021 [27] | Success rate and tissue removal required for CA (SGE vs. MAN in teeth with OP) |
| 1 ESP for both groups |
|
| Jain SD et al. 2020 [34] | Minimally invasive AC and channel localisation with simulated OP (in DGE) |
| 1 ESP |
|
| Connert T et al. 2019 [28] |
|
| 1 ESP 1 DG 1 recent graduate | SGE entails:
|
| Zubizarreta Macho A et al. 2020 [20] | Accuracy of SGE and DGE for AC (SGE vs. DGE vs. MAN) |
| 1 same operator for both | SGE and DGE enable more accurate CAs than conventional techniques. |
| Fan Y et al. 2019 [15] | Compare accuracy of OT and AP (with SGE using a grid as a guide vs. MAN) |
| 1 ESP | The use of prefabricated grids in guided endodontic surgery proved to be more accurate than using no guide at all. |
| Smith BG et al. 2021 [77] | Implications of the location of the greater palatine artery in relation to the molars for the performance of OT and AP. Feasibility of a flapless palatal access technique (with SGE) |
| 2 ESP |
|
| Galino Buniag A et al. 2021 [78] | OT and PA results after 1 year (with SGE) |
| 2 ESP |
|
| Aldahmash SA et al. 2022 [29] |
|
| 1 ESP (with microscope for MAN) Yes |
|
| Dianat O et al. 2021 [16] | Accuracy and efficiency of DGE for OT and AP (DGE vs. MAN) |
| 1 ESP (with microscope for MAN) |
|
| Gaffuri S et al. 2021 [79] | Accuracy of minimally invasive guides for OT and AP (with SGE) |
| 1 ESP 1 EST |
|
| Ackerman S et al. 2019 [14] | Guide accuracy in OT and AP (with SGE vs. MAN) |
| No data |
|
| Leontiev W et al. 2021 [80] | Suitability of IMR instead of CBCT for CA (with SGE) |
| 1 operator with 2 years of professional experience |
|
| Janabi A et al. 2021 [30] | Accuracy and efficiency for PR towards pre-treated teeth (with DGE vs. MAN) |
| 1ESP (with microscope for MAN) |
|
| Perez C et al. 2021 [81] | Reliability for RP when artefacts are present on CBCT(with SGE) |
| 2 operators |
|
| Author | Tooth | Diagnosis | Previous Treatment | Trauma | Problem | Type of EG | Results |
|---|---|---|---|---|---|---|---|
| Todd R et al. 2021 [60] | 2.1 | NP PAS | No | No | OP | SGE | Tooth without symptomatology after 24 h. |
| Buchgreitz J et al. 2019 [35] | 1.6 | PAS | Yes | No | OP | SGE | Tooth without symptomatology after 2 years. |
| Torres A et al. 2021 [36] | 1.4 | NP PAS | No | No | OP | SGE | Bone regeneration at one year |
| Lara Mendes STO et al. 2018 [37] | 2.7, 2.8 | PAS | No | No | OP | SGE | No symptoms and bone regeneration after one year |
| Fonseca Tavares WL et al. 2018 [3] | (a) 1.1 (b) 1.1 | (a) NP PAS (b) PAS | (a) No (b) Yes | Yes | OP | SGE | (a) At 15 days, there was no symptomatology. (b) Tooth asymptomatic at 30 days. |
| Lara Mendes STO et al. 2018 [38] | 2.1 | PAS | No | Yes | OP | SGE | Tooth without symptomatology after 1 year. |
| Maia LM et al. 2019 [39] | (a) 2.6 (b) 2.5 (c) 1.5 | (a) PAS (b) NP Bruxismo (c) PAS | (a) No (b) Yes (c) Yes | No | OP | SGE | Complete healing after 1 year |
| Fonseca Tavares WL et al. 2020 [40] | 2.3 | PAS | No | No | OP, complex root anatomy | SGE and photo-dynamic dynamics | Asymptomatic tooth at 12 months. |
| Fernandes Goncalves W. 2021 [41] | (a) 2.3 (b) 4.6 | PAS | (a) No (b) Yes | No | OP RP | SGE | (a) At one year, the size of the apical lesion was reduced and there was no symptomatology. (b) No signs or symptoms at one-year review. |
| Fonseca Tavares WL et al. 2020 [42] | (a) 4.7 (b) 4.6 (c) 1.6 | PAS | (a) Yes (b) Yes (c) Yes | No | OP | SGE | (a) Tooth asymptomatic at 12 months. (b) No data. (c) No symptoms at 12 months. |
| Maia LM, et al. 2020 [43] | 4.6 | NP PAS | Yes | No | OP | SGE | Complete healing after 24 months of revision. |
| Freire BB et al. 2021 [44] | 1.1 | NP PAS | No | Yes | OP | SGE | Complete healing and absence of symptomatology after 2 years. |
| Doranala S et al. 2020 [63] | 1.1 | NP PAS | No | Yes | OP | SGE | Signs of healing at 3 months and absence of symptomatology. |
| Casadei BDA et al. 2020 [45] | 1.5 | AAC | Yes | No | OP | SGE | Absence of symptomatology at one year together with a decrease in the size of the apical lesion. |
| Loureiro MAZ et al. 2021 [9] | 2.1 | PAA | Yes | Yes | OP | SGE | Satisfactory results at the 6-month checkup. |
| Villa Machado PA et al. 2022 [46] | 3.1 | NP PAS | No | Yes | OP | DGE | Asymptomatic at 12 months. |
| Connert T et al. 2018 [64] | 3.1, 4.1 | PAS | No | Yes | OP | SGE | There was no symptomatology at 2 weeks. |
| Torres A et al. 2019 [65] | 2.2 | PAS | No | No | OP | SGE | Apical lesion healing at 6 months. |
| Silva AS et al. 2020 [53] | 2.1 | NP | Yes | No | OP | SGE. | Successful results after 1 year. |
| Coelho Santiago M et al. 2022 [48] | 4.6 | NP | Yes | No | OP | SGE | Asymptomatic tooth at one year. |
| Krug R et al. 2020 [49] | 1.5, 1.2, 2.6, 3.6, 3.2, 3.1 and 4.6 | PAS Dysplasia dentinaria | Yes, en 3.6 | No. | OP | SGE | At one year, there was complete healing of 1.5, 2.6, 3.1, and 4.6, as well as reduction of apical lesion size by 3.6, 3.2, and 1.2. |
| Kaur G et al. 2021 [50] | 2.2 | PAS | No | Yes | OP | SGE | Tooth asymptomatic at 2 weeks. |
| Ali A et al. 2022 [51] | (a) 4.4 (b) 1.1, 1.2, 2.2. (c) 1.2, 2.1 | NP PAS | (a) No (b) No (c) No | (a) No (b) Yes (c) Yes | OP | SGE | At one year, there was absence of signs and symptoms in all cases. |
| Llaquet Pujol M et al. 2021 [52] | (a) 2.1 (b) 1.3 (c) 2.1 (d) 1.1 (e) 1.1 (f) 2.1 (g) 1.1 | (a) PAS (b) AAC (c) AAA (d) PAS (e) AAA (f) PAA (g) PAA | No | Yes | OP | SGE | No symptoms at one year. |
| Yan YQ et al. 2021 [54] | 2.7 | PAS | Yes | No | OP | SGE (mediate inlay unitario) | No symptoms at two years. |
| Mena Álvarez J et al. 2017 [55] | 2.1 | AAC | No | No | Dens evagina-tus | SGE | No symptoms at one year. |
| Moreira Maia L et al. 2020 [62] | 2.1 | PAS | Yes | Yes | RT RP | SGE | Injury healing at 18 months. |
| Perez C et al. 2020 [56] | 1.6 | PAS | Yes | No | RT RP | SGE | Healing of the periapical area at one year. |
| Strbac G et al. 2017 [57] | 1.5 y 1.6 | PAS | Yes | No | OT AP | SGE | Healing of the periapical area at one year. |
| Giacomino CM et al. 2018 [70] | (a) 1.7 (b) 2.6 (c) 3.5 | (a) AAC (b) PAA (c) PAS | (a) Yes (b) No (c) Yes | (a) No (b) Yes (c) No | OT AP | SGE | (a) No symptoms at 12 weeks. (b) Asymptomatic at one month. (c) Asymptomatic at one month. |
| Popowicz W et al. 2019 [69] | (a) 2.5 (b) 2.5 | a) PAS b) NP PAS | (a) Yes (b) Yes | (a) No (b) No | OT AP | SGE | (a) No symptoms at 7 months. (b) No symptoms at 8 months. |
| Benjamin G et al. 2021 [68] | (a) 2.6 (b) 3.6 (c) 2.6 | PAS | YES | No | OT AP | SGE | (a) No symptoms after 10 days. (b,c) No symptoms at 1 week. |
| Gómez Meda R et al. 2022 [58] | 2.3 | Impacted | No | No | OP AT AUT | SGE | Complete bone integration at 2 years. |
| Fu W et al. 2022 [67] | (a) 3.6 (b) 3.6 (c) 2.6 | (a) PAS (b) AAA (c) AAA | (a) Yes (b) Yes (c) Yes | No | OT, AP | DGE | (a) Asymptomatic at 9 months. (b) Cure at 6 months. (c) Asymptomatic at 3 months. |
| Fonseca Tavares WL et al. 2019 [66] | 2.5 | PAS | Yes | No | OT AP | SGE | Asymptomatic at 6 months. |
| Chaves GS et al. 2022 [59] | 3.6 | PAA RRE | Yes | No | OT AP | SGE | Asymptomatic at 1 year. |
| Gambarini G et al. 2019 [61] | 1.2 | PAS | Yes | No | OT AP | DGE | Successful healing after 1, 3, and 6 months of control. |
4. Discussion
5. Conclusions
- The advantages of SGE are as follows: it is independent of the operator’s experience, requires less treatment time for the patient, and is more accurate and safer than conventional endodontics.
- The disadvantages of SGE are as follows: more time is needed for the design and production of 3D guides, it involves linear access that only works for straight canals, and it is not very stable in the mouth in partially edentulous patients.
- The benefits of DGE are as follows: it is more ergonomic (in terms of having to look at the monitor during treatment), it allows for the real-time adjustment and repositioning of the working instruments, it is more accurate as it does not accumulate design errors, and it is useful in cases of multi-rooted teeth.
- The disadvantages of DGE are as follows: it is highly dependent on the operator’s experience and requires deeper learning for its mastery, and it requires simultaneous hand–eye coordination.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bastos, J.V.; Côrtes, M.I.S. Pulp canal obliteration after traumatic injuries in permanent teeth-scientific fact or fiction? Braz. Oral Res. 2018, 32, e75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spinas, E.; Deias, M.; Mameli, A.; Giannetti, L. Pulp canal obliteration after extrusive and lateral luxation in young permanent teeth: A scoping review. Eur. J. Paediatr. Dent. 2021, 22, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Fonseca Tavares, W.L.; Diniz Viana, A.C.; de Carvalho Machado, V.; Feitosa Henriques, L.C.; Ribeiro Sobrinho, A.P. Guided Endodontic Access of Calcified Anterior Teeth. J. Endod. 2018, 44, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Kristerson, L. Autotransplantation of human premolars. A clinical and radiographic study of 100 teeth. Int. J. Oral Surg. 1985, 14, 200–213. [Google Scholar] [CrossRef]
- Abd-Elmeguid, A.; ElSalhy, M.; Yu, D.C. Pulp canal obliteration after replantation of avulsed immature teeth: A systematic review. Dent. Traumatol. 2015, 31, 437–441. [Google Scholar] [CrossRef]
- Hecova, H.; Tzigkounakis, V.; Merglova, V.; Netolicky, J. A retrospective study of 889 injured permanent teeth. Dent. Traumatol. 2010, 26, 466–475. [Google Scholar] [CrossRef]
- Robertson, A.; Andreasen, F.M.; Bergenholtz, G.; Andreasen, J.O.; Norén, J.G. Incidence of pulp necrosis subsequent to pulp canal obliteration from trauma of permanent incisors. J. Endod. 1996, 22, 557–560. [Google Scholar] [CrossRef]
- Vinagre, A.; Castanheira, C.; Messias, A.; Palma, P.J.; Ramos, J.C. Management of Pulp Canal Obliteration-Systematic Review of Case Reports. Medicina 2021, 57, 1237. [Google Scholar] [CrossRef]
- Loureiro, M.A.Z.; Silva, J.A.; Chaves, G.S.; Capeletti, L.R.; Estrela, C.; Decurcio, D.A. Guided endodontics: The impact of new technologies on complex case solution. Aust. Endod. J. 2021, 47, 664–671. [Google Scholar] [CrossRef]
- McCabe, P.S.; Dummer, P.M. Pulp canal obliteration: An endodontic diagnosis and treatment challenge. Int. Endod. J. 2012, 45, 177–197. [Google Scholar] [CrossRef]
- Zehnder, M.S.; Connert, T.; Weiger, R.; Krastl, G.; Kühl, S. Guided endodontics: Accuracy of a novel method for guided access cavity preparation and root canal location. Int. Endod. J. 2016, 49, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Buchgreitz, J.; Buchgreitz, M.; Mortensen, D.; Bjørndal, L. Guided access cavity preparation using cone-beam computed tomography and optical surface scans—An ex vivo study. Int. Endod. J. 2016, 49, 790–795. [Google Scholar] [CrossRef]
- Krastl, G.; Zehnder, M.S.; Connert, T.; Weiger, R.; Kühl, S. Guided Endodontics: A novel treatment approach for teeth with pulp canal calcification and apical pathology. Dent. Traumatol. 2016, 32, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, S.; Aguilera, F.C.; Buie, J.M.; Glickman, G.N.; Umorin, M.; Wang, Q.; Jalali, P. Accuracy of 3-dimensional-printed Endodontic Surgical Guide: A Human Cadaver Study. J. Endod. 2019, 45, 615–618. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Glickman, G.N.; Umorin, M.; Nair, M.K.; Jalali, P. A Novel Prefabricated Grid for Guided Endodontic Microsurgery. J. Endod. 2019, 45, 606–610. [Google Scholar] [CrossRef]
- Dianat, O.; Nosrat, A.; Mostoufi, B.; Price, J.B.; Gupta, S.; Martinho, F.C. Accuracy and efficiency of guided root-end resection using a dynamic navigation system: A human cadaver study. Int. Endod. J. 2021, 54, 793–801. [Google Scholar] [CrossRef]
- van der Meer, W.J.; Vissink, A.; Ng, Y.L.; Gulabivala, K. 3D Computer aided treatment planning in endodontics. J. Dent. 2016, 45, 67–72. [Google Scholar] [CrossRef]
- Kim, B.N.; Son, S.A.; Park, J.K. Endodontic retreatment of a calcified anterior tooth using a 3D-printed endodontic guide. Int. J. Comput. Dent. 2021, 24, 419–427. [Google Scholar]
- Connert, T.; Weiger, R.; Krastl, G. Present status and future directions-Guided endodontics. Int. Endod. J. 2022, 10, 995–1002. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Muñoz, A.P.; Deglow, E.R.; Agustín-Panadero, R.; Álvarez, J.M. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Procedure for Endodontic Access Cavities: An in Vitro Study. J. Clin. Med. 2020, 9, 129. [Google Scholar] [CrossRef] [Green Version]
- Gambarini, G.; Galli, M.; Morese, A.; Stefanelli, L.V.; Abduljabbar, F.; Giovarruscio, M.; Di Nardo, D.; Seracchiani, M.; Testarelli, L. Precision of Dynamic Navigation to Perform Endodontic Ultraconservative Access Cavities: A Preliminary In Vitro Analysis. J. Endod. 2020, 46, 1286–1290. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.D.; Saunders, M.W.; Carrico, C.K.; Jadhav, A.; Deeb, J.G.; Myers, G.L. Dynamically Navigated versus Freehand Access Cavity Preparation: A Comparative Study on Substance Loss Using Simulated Calcified Canals. J. Endod. 2020, 46, 1745–1751. [Google Scholar] [CrossRef] [PubMed]
- Loureiro, M.A.Z.; Elias, M.R.A.; Capeletti, L.R.; Silva, J.A.; Siqueira, P.C.; Chaves, G.S.; Decurcio, D.A. Guided Endodontics: Volume of Dental Tissue Removed by Guided Access Cavity Preparation-An Ex Vivo Study. J. Endod. 2020, 46, 1907–1912. [Google Scholar] [CrossRef] [PubMed]
- Connert, T.; Leontiev, W.; Dagassan-Berndt, D.; Kühl, S.; ElAyouti, A.; Krug, R.; Krastl, G.; Weiger, R. Real-Time Guided Endodontics with a Miniaturized Dynamic Navigation System Versus Conventional Freehand Endodontic Access Cavity Preparation: Substance Loss and Procedure Time. J. Endod. 2021, 47, 1651–1656. [Google Scholar] [CrossRef]
- Ali, A.; Arslan, H. Effectiveness of the static-guided endodontic technique for accessing the root canal through MTA and its effect on fracture strength. Clin. Oral Investig. 2021, 25, 1989–1995. [Google Scholar] [CrossRef]
- Dianat, O.; Nosrat, A.; Tordik, P.A.; Aldahmash, S.A.; Romberg, E.; Price, J.B.; Mostoufi, B. Accuracy and Efficiency of a Dynamic Navigation System for Locating Calcified Canals. J. Endod. 2020, 46, 1719–1725. [Google Scholar] [CrossRef]
- Kostunov, J.; Rammelsberg, P.; Klotz, A.L.; Zenthöfer, A.; Schwindling, F.S. Minimization of Tooth Substance Removal in Normally Calcified Teeth Using Guided Endodontics: An In Vitro Pilot Study. J. Endod. 2021, 47, 286–290. [Google Scholar] [CrossRef]
- Connert, T.; Krug, R.; Eggmann, F.; Emsermann, I.; ElAyouti, A.; Weiger, R.; Kühl, S.; Krastl, G. Guided Endodontics versus Conventional Access Cavity Preparation: A Comparative Study on Substance Loss Using 3-dimensional-printed Teeth. J. Endod. 2019, 45, 327–331. [Google Scholar] [CrossRef]
- Aldahmash, S.A.; Price, J.B.; Mostoufi, B.; Griffin, I.L.; Dianat, O.; Tordik, P.A.; Martinho, F.C. Real-time 3-dimensional Dynamic Navigation System in Endodontic Microsurgery: A Cadaver Study. J. Endod. 2022, 48, 922–929. [Google Scholar] [CrossRef]
- Janabi, A.; Tordik, P.A.; Griffin, I.L.; Mostoufi, B.; Price, J.B.; Chand, P.; Martinho, F.C. Accuracy and Efficiency of 3-dimensional Dynamic Navigation System for Removal of Fiber Post from Root Canal-Treated Teeth. J. Endod. 2021, 47, 1453–1460. [Google Scholar] [CrossRef]
- Koch, G.K.; Gharib, H.; Liao, P.; Liu, H. Guided Access Cavity Preparation Using Cost-Effective 3D Printers. J. Endod. 2022, 48, 909–913. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Boelen, G.J.; Lambrechts, P.; Pedano, M.S.; Jacobs, R. Dynamic navigation: A laboratory study on the accuracy and potential use of guided root canal treatment. Int. Endod. J. 2021, 54, 1659–1667. [Google Scholar] [CrossRef] [PubMed]
- Krug, R.; Reich, S.; Connert, T.; Kess, S.; Soliman, S.; Reymus, M.; Krastl, G. Guided endodontics: A comparative in vitro study on the accuracy and effort of two different planning workflows. Int. J. Comput. Dent. 2020, 23, 119–128. [Google Scholar] [PubMed]
- Jain, S.D.; Carrico, C.K.; Bermanis, I. 3-Dimensional Accuracy of Dynamic Navigation Technology in Locating Calcified Canals. J. Endod. 2020, 46, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Buchgreitz, J.; Buchgreitz, M.; Bjørndal, L. Guided Endodontics Modified for Treating Molars by Using an Intracoronal Guide Technique. J. Endod. 2019, 45, 818–823. [Google Scholar] [CrossRef]
- Torres, A.; Lerut, K.; Lambrechts, P.; Jacobs, R. Guided Endodontics: Use of a Sleeveless Guide System on an Upper Premolar with Pulp Canal Obliteration and Apical Periodontitis. J. Endod. 2021, 47, 133–139. [Google Scholar] [CrossRef]
- Lara-Mendes, S.T.O.; Barbosa, C.F.M.; Santa-Rosa, C.C.; Machado, V.C. Guided Endodontic Access in Maxillary Molars Using Cone-beam Computed Tomography and Computer-aided Design/Computer-aided Manufacturing System: A Case Report. J. Endod. 2018, 44, 875–879. [Google Scholar] [CrossRef]
- Lara-Mendes, S.T.O.; Barbosa, C.F.M.; Machado, V.C.; Santa-Rosa, C.C. A New Approach for Minimally Invasive Access to Severely Calcified Anterior Teeth Using the Guided Endodontics Technique. J. Endod. 2018, 44, 1578–1582. [Google Scholar] [CrossRef]
- Maia, L.M.; de Carvalho Machado, V.; da Silva, N.; Brito Júnior, M.; da Silveira, R.R.; Moreira Júnior, G.; Ribeiro Sobrinho, A.P. Case Reports in Maxillary Posterior Teeth by Guided Endodontic Access. J. Endod. 2019, 45, 214–218. [Google Scholar] [CrossRef]
- Tavares, W.L.F.; Ferreira, M.V.L.; de Carvalho Machado, V.; Braga, T.; Amaral, R.R.; Cohen, S. Antimicrobial photodynamic therapy and guided endodontics: A case report. Photodiagn. Photodyn. Ther. 2020, 31, 101935. [Google Scholar] [CrossRef]
- Gonçalves, W.F.; Garcia, L.; Vieira-Schuldt, D.P.; Bortoluzzi, E.A.; Dias-Júnior, L.C.L.; Teixeira, C.D.S. Guided Endodontics in Root Canals with Complex Access: Two Case Reports. Braz. Dent. J. 2021, 32, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Tavares, W.L.F.; Machado, V.d.C.; Fonseca, F.O.; Vasconcellos, B.C.; Magalhães, L.C.; Viana, A.C.D.; Henriques, L.C.F. Guided Endodontics in Complex Scenarios of Calcified Molars. Iran. Endod. J. 2020, 15, 50–56. [Google Scholar] [CrossRef]
- Maia, L.M.; Toubes, K.M.; Moreira Júnior, G.; Tonelli, S.Q.; Machado, V.d.C.; Silveira, F.F.; Nunes, E. Guided Endodontics in Nonsurgical Retreatment of a Mandibular First Molar: A New Approach and Case Report. Iran. Endod. J. 2020, 15, 111–116. [Google Scholar] [CrossRef]
- Freire, B.B.; Vianna, S.; Nascimento, E.H.L.; Freire, M.; Chilvarquer, I. Guided Endodontic Access in a Calcified Central Incisor: A Conservative Alternative for Endodontic Therapy. Iran. Endod. J. 2021, 16, 56–59. [Google Scholar] [CrossRef]
- Casadei, B.A.; Lara-Mendes, S.T.O.; Barbosa, C.F.M.; Araújo, C.V.; de Freitas, C.A.; Machado, V.C.; Santa-Rosa, C.C. Access to original canal trajectory after deviation and perforation with guided endodontic assistance. Aus.t Endod. J. 2020, 46, 101–106. [Google Scholar] [CrossRef]
- Villa-Machado, P.A.; Restrepo-Restrepo, F.A.; Sousa-Dias, H.; Tobón-Arroyave, S.I. Application of computer-assisted dynamic navigation in complex root canal treatments: Report of two cases of calcified canals. Aust. Endod. J. 2022, 48, 187–196. [Google Scholar] [CrossRef]
- Silva, E.; Pinto, K.P.; Ferreira, C.M.; Belladonna, F.G.; De-Deus, G.; Dummer, P.M.H.; Versiani, M.A. Current status on minimal access cavity preparations: A critical analysis and a proposal for a universal nomenclature. Int. Endod. J. 2020, 53, 1618–1635. [Google Scholar] [CrossRef]
- Santiago, M.C.; Altoe, M.M.; de Azevedo Mohamed, C.P.; de Oliveira, L.A.; Salles, L.P. Guided endodontic treatment in a region of limited mouth opening: A case report of mandibular molar mesial root canals with dystrophic calcification. BMC Oral Health 2022, 22, 37. [Google Scholar] [CrossRef]
- Krug, R.; Volland, J.; Reich, S.; Soliman, S.; Connert, T.; Krastl, G. Guided endodontic treatment of multiple teeth with dentin dysplasia: A case report. Head Face Med. 2020, 16, 27. [Google Scholar] [CrossRef]
- Kaur, G.; Venkatesh, K.; Sihivahanan, D. Microguided endodontics: A case report of conservative approach for the management of calcified maxillary lateral incisors. Saudi Endod. J. 2021, 11, 266–270. [Google Scholar] [CrossRef]
- Ali, A.; Ishaq, A.; Jain, P.; Ali, S. Management of pulp canal obliteration using static-guided endodontic technique: Case series. Saudi Endod. J. 2022, 12, 120–128. [Google Scholar] [CrossRef]
- Llaquet Pujol, M.; Vidal, C.; Mercadé, M.; Muñoz, M.; Ortolani-Seltenerich, S. Guided Endodontics for Managing Severely Calcified Canals. J. Endod. 2021, 47, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.S.; Carvalho Santos, A.C.; de Sousa Caneschi, C.; Machado, V.C.; Moreira, A.N.; Dos Santos Alves Morgan, L.F.; Tavares, W.L.F. Adaptable fiberglass post after 3D guided endodontic treatment: Novel approaches in restorative dentistry. J. Esthet. Restor. Dent. 2020, 32, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.Q.; Wang, H.L.; Liu, Y.; Zheng, T.J.; Tang, Y.P.; Liu, R. Three-dimensional inlay-guided endodontics applied in variant root canals: A case report and review of literature. World J. Clin. Cases 2021, 9, 11425–11436. [Google Scholar] [CrossRef] [PubMed]
- Mena-Álvarez, J.; Rico-Romano, C.; Lobo-Galindo, A.B.; Zubizarreta-Macho, Á. Endodontic treatment of dens evaginatus by performing a splint guided access cavity. J. Esthet. Restor. Dent. 2017, 29, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Perez, C.; Finelle, G.; Couvrechel, C. Optimisation of a guided endodontics protocol for removal of fibre-reinforced posts. Aust. Endod. J. 2020, 46, 107–114. [Google Scholar] [CrossRef]
- Strbac, G.D.; Schnappauf, A.; Giannis, K.; Moritz, A.; Ulm, C. Guided Modern Endodontic Surgery: A Novel Approach for Guided Osteotomy and Root Resection. J. Endod. 2017, 43, 496–501. [Google Scholar] [CrossRef] [PubMed]
- Gómez Meda, R.; Abella Sans, F.; Esquivel, J.; Zufía, J. Impacted Maxillary Canine with Curved Apex: Three-Dimensional Guided Protocol for Autotransplantation. J. Endod. 2022, 48, 379–387. [Google Scholar] [CrossRef]
- Chaves, G.S.; Capeletti, L.R.; Miguel, J.G.; Loureiro, M.A.Z.; Silva, E.; Decurcio, D.A. A Novel Simplified Workflow for Guided Endodontic Surgery in Mandibular Molars With a Thick Buccal Bone Plate: A Case Report. J. Endod. 2022, 48, 930–935. [Google Scholar] [CrossRef]
- Todd, R.; Resnick, S.; Zicarelli, T.; Linenberg, C.; Donelson, J.; Boyd, C. Template-guided endodontic access. J. Am. Dent. Assoc. 2021, 152, 65–70. [Google Scholar] [CrossRef]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402.e1396. [Google Scholar] [CrossRef] [PubMed]
- Maia, L.M.; Bambirra Júnior, W.; Toubes, K.M.; Moreira Júnior, G.; de Carvalho Machado, V.; Parpinelli, B.C.; Ribeiro Sobrinho, A.P. Endodontic guide for the conservative removal of a fiber-reinforced composite resin post. J. Prosthet. Dent. 2022, 128, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Doranala, S.; Vemisetty, H.; Punna, R.; Alwala, A.M. Endodontic Management of Canal Calcification in Maxillary Central Incisor Using 3D Prototyping Technique: A Case Report. J. Adv. Oral Res. 2020, 11, 93–96. [Google Scholar] [CrossRef]
- Connert, T.; Zehnder, M.S.; Amato, M.; Weiger, R.; Kühl, S.; Krastl, G. Microguided Endodontics: A method to achieve minimally invasive access cavity preparation and root canal location in mandibular incisors using a novel computer-guided technique. Int. Endod. J. 2018, 51, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Shaheen, E.; Lambrechts, P.; Politis, C.; Jacobs, R. Microguided Endodontics: A case report of a maxillary lateral incisor with pulp canal obliteration and apical periodontitis. Int. Endod. J. 2019, 52, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Tavares, W.L.F.; Fonseca, F.O.; Maia, L.M.; de Carvalho Machado, V.; França Alves Silva, N.R.; Junior, G.M.; Ribeiro Sobrinho, A.P. 3D Apicoectomy Guidance: Optimizing Access for Apicoectomies. J. Oral Maxillofac. Surg. 2020, 78, 357.e351–357.e358. [Google Scholar] [CrossRef]
- Fu, W.; Chen, C.; Bian, Z.; Meng, L. Endodontic Microsurgery of Posterior Teeth with the Assistance of Dynamic Navigation Technology: A Report of Three Cases. J. Endod. 2022, 48, 943–950. [Google Scholar] [CrossRef]
- Benjamin, G.; Ather, A.; Bueno, M.R.; Estrela, C.; Diogenes, A. Preserving the Neurovascular Bundle in Targeted Endodontic Microsurgery: A Case Series. J. Endod. 2021, 47, 509–519. [Google Scholar] [CrossRef]
- Popowicz, W.; Palatyńska-Ulatowska, A.; Kohli, M.R. Targeted Endodontic Microsurgery: Computed Tomography-based Guided Stent Approach with Platelet-rich Fibrin Graft: A Report of 2 Cases. J. Endod. 2019, 45, 1535–1542. [Google Scholar] [CrossRef]
- Giacomino, C.M.; Ray, J.J.; Wealleans, J.A. Targeted Endodontic Microsurgery: A Novel Approach to Anatomically Challenging Scenarios Using 3-dimensional-printed Guides and Trephine Burs-A Report of 3 Cases. J. Endod. 2018, 44, 671–677. [Google Scholar] [CrossRef] [Green Version]
- Connert, T.; Zehnder, M.S.; Weiger, R.; Kühl, S.; Krastl, G. Microguided Endodontics: Accuracy of a Miniaturized Technique for Apically Extended Access Cavity Preparation in Anterior Teeth. J. Endod. 2017, 43, 787–790. [Google Scholar] [CrossRef] [PubMed]
- Buchgreitz, J.; Buchgreitz, M.; Bjørndal, L. Guided root canal preparation using cone beam computed tomography and optical surface scans—An observational study of pulp space obliteration and drill path depth in 50 patients. Int. Endod. J. 2019, 52, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.C.; Kwok, J.W.; Vinculado, F.; Fried, D. Computer-Controlled CO(2) Laser Ablation System for Cone-beam Computed Tomography and Digital Image Guided Endodontic Access: A Pilot Study. J. Endod. 2021, 47, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Chen, C.; Lin, C.; Lee, H.; Chen, K.; Lin, Y.; Chuang, F. Guided endodontics: Accuracy of access cavity preparation and discrimination of angular and linear deviation on canal accessing ability-an ex vivo study. BMC Oral Health 2021, 21, 606. [Google Scholar] [CrossRef]
- Choi, Y.; Jeon, W.S.; Cho, J.M.; Jeong, H.G.; Shin, Y.; Park, W. Access opening guide produced using a 3D printer (AOG-3DP) as an effective tool in difficult cases for dental students. J. Dent. Educ. 2021, 85, 1640–1645. [Google Scholar] [CrossRef]
- Chong, B.S.; Dhesi, M.; Makdissi, J. Computer-aided dynamic navigation: A novel method for guided endodontics. Quintessence Int. 2019, 50, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.G.; Pratt, A.M.; Anderson, J.A.; Ray, J.J. Targeted Endodontic Microsurgery: Implications of the Greater Palatine Artery. J. Endod. 2021, 47, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Buniag, A.G.; Pratt, A.M.; Ray, J.J. Targeted Endodontic Microsurgery: A Retrospective Outcomes Assessment of 24 Cases. J. Endod. 2021, 47, 762–769. [Google Scholar] [CrossRef]
- Gaffuri, S.; Audino, E.; Salvadori, M.; Garo, M.L.; Salgarello, S. Accuracy of a minimally invasive surgical guide in microsurgical endodontics: A human cadaver study. G. Ital. Endod. 2021, 35, 30–36. [Google Scholar] [CrossRef]
- Leontiev, W.; Bieri, O.; Madörin, P.; Dagassan-Berndt, D.; Kühl, S.; Krastl, G.; Krug, R.; Weiger, R.; Connert, T. Suitability of Magnetic Resonance Imaging for Guided Endodontics: Proof of Principle. J. Endod. 2021, 47, 954–960. [Google Scholar] [CrossRef]
- Perez, C.; Sayeh, A.; Etienne, O.; Gros, C.I.; Mark, A.; Couvrechel, C.; Meyer, F. Microguided endodontics: Accuracy evaluation for access through intraroot fibre-post. Aust. Endod. J. 2021, 47, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Ballester, B.; Giraud, T.; Ahmed, H.M.A.; Nabhan, M.S.; Bukiet, F.; Guivarc’h, M. Current strategies for conservative endodontic access cavity preparation techniques-systematic review, meta-analysis, and decision-making protocol. Clin. Oral Investig. 2021, 25, 6027–6044. [Google Scholar] [CrossRef] [PubMed]
- Shabbir, J.; Zehra, T.; Najmi, N.; Hasan, A.; Naz, M.; Piasecki, L.; Azim, A.A. Access Cavity Preparations: Classification and Literature Review of Traditional and Minimally Invasive Endodontic Access Cavity Designs. J. Endod. 2021, 47, 1229–1244. [Google Scholar] [CrossRef]
- Reeh, E.S.; Messer, H.H.; Douglas, W.H. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J. Endod. 1989, 15, 512–516. [Google Scholar] [CrossRef]
- Nematollahi, H.; Sarraf Shirazi, A.; Mehrabkhani, M.; Sabbagh, S. Clinical and radiographic outcomes of laser pulpotomy in vital primary teeth: A systematic review and meta-analysis. Eur. Arch. Paediatr. Dent. 2018, 19, 205–220. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Arslan, H.; Jethani, B. Conservative management of Type II dens invaginatus with guided endodontic approach: A case series. J. Conserv. Dent. 2019, 22, 503–508. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Ferreiroa, A.; Agustín-Panadero, R.; Rico-Romano, C.; Lobo-Galindo, A.B.; Mena-Álvarez, J. Endodontic re-treatment and restorative treatment of a dens invaginatus type II through new technologies. J. Clin. Exp. Dent. 2019, 11, e570–e576. [Google Scholar] [CrossRef] [PubMed]
- Schmid, C.; Lotz, M.; Pieralli, S.; Valdec, S. Guided flapless apicoectomy of the palatal root of a maxillary molar: A case presentation. Quintessence Int. 2022, 53, 608–614. [Google Scholar] [CrossRef]
- Capriotti, L.; Greco, K.; Paolone, G.; Sberna, M.T.; Cantatore, G. Removal of fiber posts during endodontic retreatments using ultrasonic tips: A comparison between two different endodontic fiber posts. G. Ital. Endod. 2018, 32, 47–50. [Google Scholar] [CrossRef]
- Jawed, A.; Alghmlas, A.S.; Khurshid, Z. 15-Fiber post: Physics, chemistry, adhesive properties, and its implications on root canal retreatment. In Biomaterials in Endodontics; Khurshid, Z., Zafar, M.S., Najeeb, S., Eds.; Woodhead Publishing: Thorston, UK, 2022; pp. 357–378. [Google Scholar]
- Scotti, N.; Bergantin, E.; Alovisi, M.; Pasqualini, D.; Berutti, E. Evaluation of a simplified fiber post removal system. J. Endod. 2013, 39, 1431–1434. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kulinkovych-Levchuk, K.; Pecci-Lloret, M.P.; Castelo-Baz, P.; Pecci-Lloret, M.R.; Oñate-Sánchez, R.E. Guided Endodontics: A Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 13900. https://doi.org/10.3390/ijerph192113900
Kulinkovych-Levchuk K, Pecci-Lloret MP, Castelo-Baz P, Pecci-Lloret MR, Oñate-Sánchez RE. Guided Endodontics: A Literature Review. International Journal of Environmental Research and Public Health. 2022; 19(21):13900. https://doi.org/10.3390/ijerph192113900
Chicago/Turabian StyleKulinkovych-Levchuk, Kateryna, María Pilar Pecci-Lloret, Pablo Castelo-Baz, Miguel Ramón Pecci-Lloret, and Ricardo E. Oñate-Sánchez. 2022. "Guided Endodontics: A Literature Review" International Journal of Environmental Research and Public Health 19, no. 21: 13900. https://doi.org/10.3390/ijerph192113900






