Unraveling the Role of Objective Food Environment in Chinese Elderly’s Diet-Related Diseases Epidemic: Considering Both Healthy Food Accessibility and Diversity
Abstract
:1. Introduction
2. Previous Literature
3. Data and Methods
3.1. Data
3.1.1. Diet-Related Health Outcomes
3.1.2. Food Environment Measures as Explanatory Variables
3.1.3. Individual Lifestyles as Moderator
3.2. Methods
3.2.1. Food Environment Measures
3.2.2. Empirical Strategy
4. Results
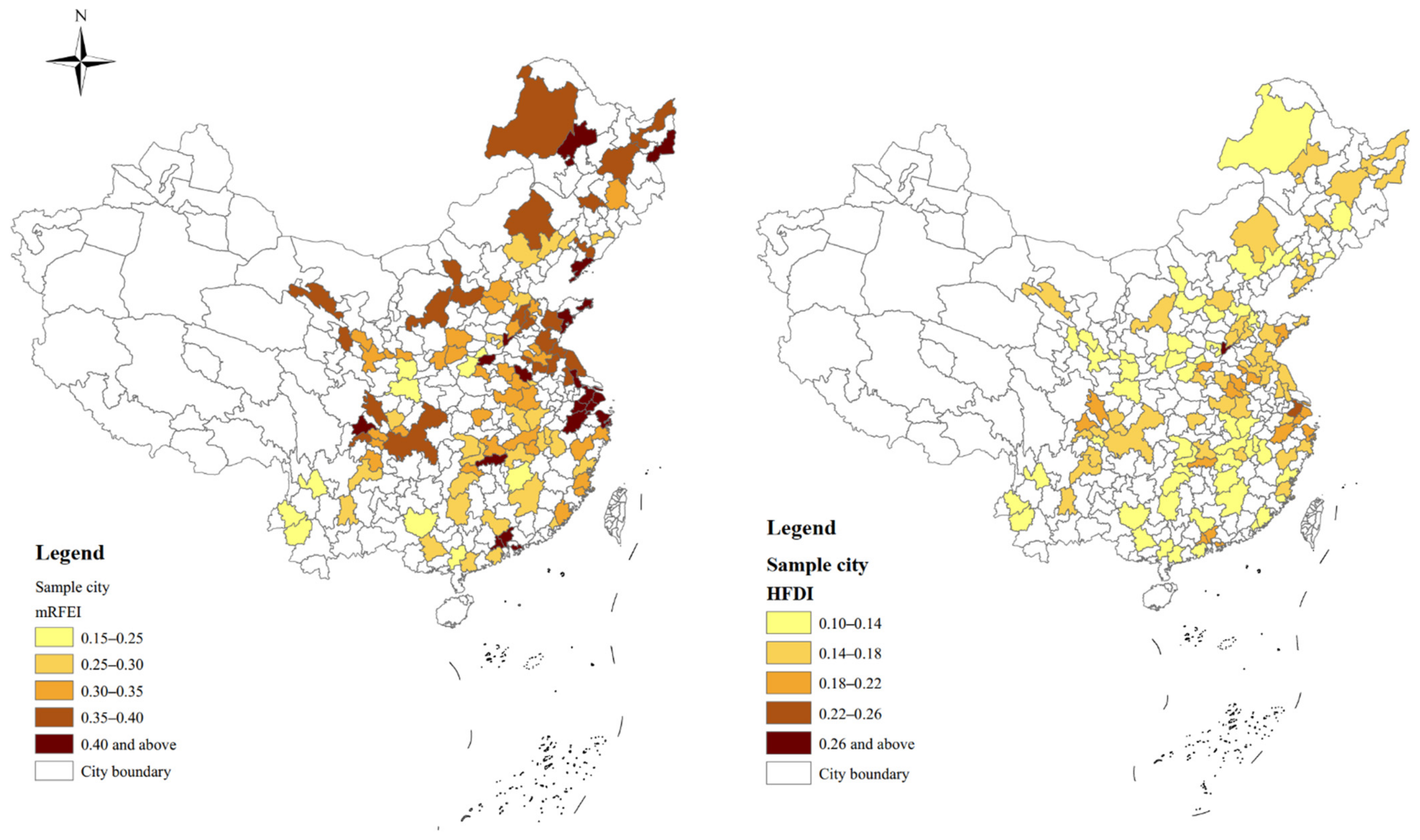
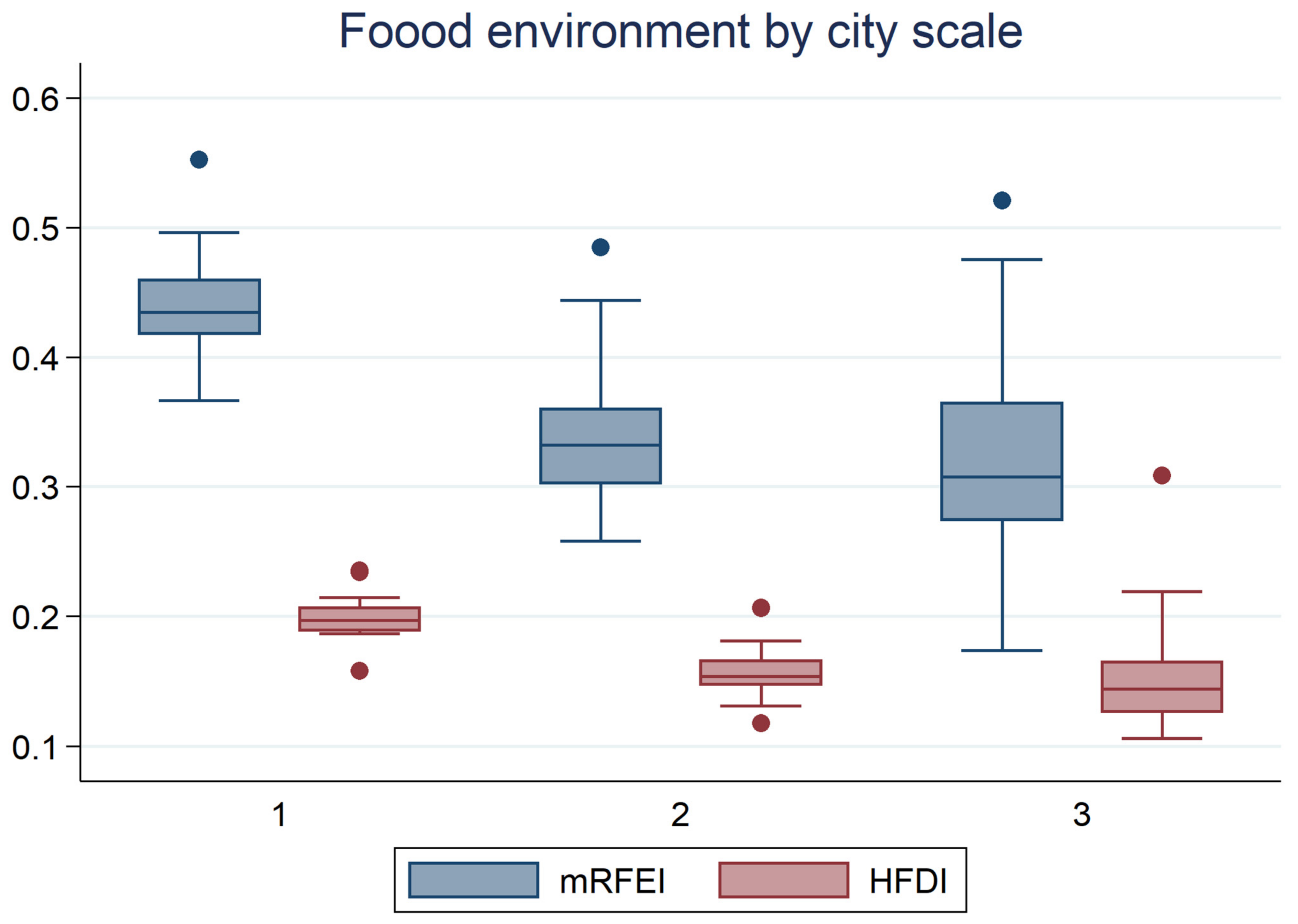
4.1. Descriptive Analysis
4.2. Empirical Results
4.2.1. Baseline Estimates
4.2.2. Moderating Role of Healthy Individual Lifestyles
4.2.3. Heterogeneity Effect of Food Environment by City Scale
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, Y. Annual Report on Elderly Health in China (2020–2021); The Social Sciences Academic Press: Beijing, China, 2021. [Google Scholar]
- Fitzpatrick, K.; Greenhalgh-Stanley, N.; Ver Ploeg, M. Food Deserts and Diet-Related Health Outcomes of the Elderly. Food Policy 2019, 87, 101747. [Google Scholar] [CrossRef]
- Gao, J.; Wang, L.; Liang, H.; He, Y.; Zhang, S.; Wang, Y.; Li, Z.; Ma, Y. The Association between a Combination of Healthy Lifestyles and the Risks of Hypertension and Dyslipidemia among Adults-Evidence from the Northeast of China. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; He, S.; Zhao, C.; Su, S.; Weng, M.; Li, G. Unraveling Urban Food Availability Dynamics and Associated Social Inequalities: Towards a Sustainable Food Environment in a Developing Context. Sustain. Cities Soc. 2022, 77, 103591. [Google Scholar] [CrossRef]
- Winson, A. Bringing Political Economy into the Debate on the Obesity Epidemic. Agric. Hum. Values 2004, 21, 299–312. [Google Scholar] [CrossRef]
- Clary, C.; Matthews, S.A.; Kestens, Y. Between Exposure, Access and Use: Reconsidering Foodscape Influences on Dietary Behaviours. Health Place 2017, 44, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Freire, T.; Rudkin, S. Healthy Food Diversity and Supermarket Interventions: Evidence from the Seacroft Intervention Study. Food Policy 2019, 83, 125–138. [Google Scholar] [CrossRef]
- Laar, A.; Barnes, A.; Aryeetey, R.; Tandoh, A.; Bash, K.; Mensah, K.; Zotor, F.; Vandevijvere, S.; Holdsworth, M. Implementation of Healthy Food Environment Policies to Prevent Nutrition-Related Non-Communicable Diseases in Ghana: National Experts’ Assessment of Government Action. Food Policy 2020, 93, 101907. [Google Scholar] [CrossRef]
- Minaker, L.M.; Raine, K.D.; Wild, T.C.; Nykiforuk, C.I.J.; Thompson, M.E.; Frank, L.D. Objective Food Environments and Health Outcomes. Am. J. Prev. Med. 2013, 45, 289–296. [Google Scholar] [CrossRef]
- Herforth, A.; Ahmed, S. The Food Environment, Its Effects on Dietary Consumption, and Potential for Measurement within Agriculture-Nutrition Interventions. Food Secur. 2015, 7, 505–520. [Google Scholar] [CrossRef] [Green Version]
- Bridle-Fitzpatrick, S. Food Deserts or Food Swamps?: A Mixed-Methods Study of Local Food Environments in a Mexican City. Soc. Sci. Med. 2015, 142, 202–213. [Google Scholar] [CrossRef]
- Hager, E.R.; Cockerham, A.; O’Reilly, N.; Harrington, D.; Harding, J.; Hurley, K.M.; Black, M.M. Food Swamps and Food Deserts in Baltimore City, MD, USA: Association with Dietary Behaviours among Urban Adolescent Girls. Public Health Nutr. 2016, 20, 2598–2670. [Google Scholar] [CrossRef] [Green Version]
- Amin, M.D.; Badruddoza, S.; McCluskey, J.J. Predicting Access to Healthful Food Retailers with Machine Learning. Food Policy 2021, 99, 101985. [Google Scholar] [CrossRef]
- Needham, C.; Strugnell, C.; Allender, S.; Orellana, L. Beyond Food Swamps and Food Deserts: Exploring Urban Australian Food Retail Environment Typologies. Public Health Nutr. 2022, 25, 1140–1152. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. Chinese Dietary Guidelines; People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- Caspi, C.E.; Sorensen, G.; Subramanian, S.V.; Kawachi, I. The Local Food Environment and Diet: A Systematic Review. Health Place 2012, 18, 1172–1187. [Google Scholar] [CrossRef] [Green Version]
- Lake, A.A. Neighbourhood Food Environments: Food Choice, Foodscapes and Planning for Health. Proc. Nutr. Soc. 2018, 77, 239–246. [Google Scholar] [CrossRef] [Green Version]
- Glanz, K.; Sallis, J.F.; Saelens, B.E.; Frank, L.D. Nutrition Environment Measures Survey in Stores (NEMS-S). Development and Evaluation. Am. J. Prev. Med. 2007, 32, 282–289. [Google Scholar] [CrossRef]
- Mahendra, A.; Polsky, J.Y.; Robitaille, É.; Lefebvre, M.; McBrien, T.; Minaker, L.M. Geographic Retail Food Environment Measures for Use in Public Health. Health Promot. Chronic Dis. Prev. Can. 2017, 37, 357–362. [Google Scholar] [CrossRef] [Green Version]
- Pradeilles, R.; Irache, A.; Wanjohi, M.N.; Holdsworth, M.; Laar, A.; Zotor, F.; Tandoh, A.; Klomegah, S.; Graham, F.; Muthuri, S.K.; et al. Urban Physical Food Environments Drive Dietary Behaviours in Ghana and Kenya: A Photovoice Study. Health Place 2021, 71, 102647. [Google Scholar] [CrossRef]
- Larson, N.I.; Story, M.T.; Nelson, M.C. Neighborhood Environments. Disparities in Access to Healthy Foods in the U.S. Am. J. Prev. Med. 2009, 36, 74–81. [Google Scholar] [CrossRef]
- Waters, C.N.; Zoellner, J.M.; Estabrooks, P.A.; Hill, J.L. Is the Availability of Healthy Foods Related to Fruit and Vegetable Consumption in a Rural, Health-Disparate Region? J. Hunger Environ. Nutr. 2018, 13, 289–303. [Google Scholar] [CrossRef]
- Granheim, S.I.; Løvhaug, A.L.; Terragni, L.; Torheim, L.E.; Thurston, M. Mapping the Digital Food Environment: A Systematic Scoping Review. Obes. Rev. 2022, 23, e13356. [Google Scholar] [CrossRef] [PubMed]
- Minaker, L.; Fisher, P.; Raine, K.; Frank, L. Measuring the Food Environment: From Theory to Planning Practice. J. Agric. Food Syst. Community Dev. 2011, 2, 65–82. [Google Scholar] [CrossRef]
- Dutko, P.; Ver Ploeg, M.; Farrigan, T. Characteristics and Influentialfactors of Food Deserts; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2013; pp. 1–40. [Google Scholar]
- Otterbach, S.; Oskorouchi, H.R.; Rogan, M.; Qaim, M. Using Google Data to Measure the Role of Big Food and Fast Food in South Africa’s Obesity Epidemic. World Dev. 2021, 140, 105368. [Google Scholar] [CrossRef]
- Mulrooney, T.; Foster, R.; Jha, M.; Beni, L.H.; Kurkalova, L.; Liang, C.L.; Miao, H.; Monty, G. Using Geospatial Networking Tools to Optimize Source Locations as Applied to the Study of Food Availability: A Study in Guilford County, North Carolina. Appl. Geogr. 2021, 128, 102415. [Google Scholar] [CrossRef]
- Gamba, R.J.; Schuchter, J.; Rutt, C.; Seto, E.Y.W. Measuring the Food Environment and Its Effects on Obesity in the United States: A Systematic Review of Methods and Results. J. Community Health 2015, 40, 464–475. [Google Scholar] [CrossRef]
- Stevenson, A.C.; Brazeau, A.S.; Dasgupta, K.; Ross, N.A. Neighbourhood Retail Food Outlet Access, Diet and Body Mass Index in Canada: A Systematic Review. Health Promot. Chronic Dis. Prev. Can. 2019, 39, 261–280. [Google Scholar] [CrossRef] [Green Version]
- Phillips, A.Z.; Rodriguez, H.P. U.S. County “Food Swamp” Severity and Hospitalization Rates among Adults with Diabetes: A Nonlinear Relationship. Soc. Sci. Med. 2020, 249, 112858. [Google Scholar] [CrossRef]
- Hawkes, C.; Ruel, M.T.; Salm, L.; Sinclair, B.; Branca, F. Double-Duty Actions: Seizing Programme and Policy Opportunities to Address Malnutrition in All Its Forms. Lancet 2020, 395, 142–155. [Google Scholar] [CrossRef]
- Zhao, Y.; Strauss, J.; Chen, X.; Wang, Y.; Gong, J.; Meng, Q.; Wang, G.; Wang, H. China Health and Retirement Longitudinal Study Wave 4 User’s Guide; National School of Development, Peking University: Beijing, China, 2020. [Google Scholar]
- Berry, C.H. Corporate Growth and Diversification. J. Law Econ. 1971, 14, 371–383. [Google Scholar] [CrossRef]
- Drescher, L.S.; Thiele, S.; Mensink, G.B.M. A New Index to Measure Healthy Food Diversity Better Reflects a Healthy Diet Than Traditional Measures. J. Nutr. 2007, 137, 647–651. [Google Scholar] [CrossRef]
- Belaïd, F.; Roubaud, D.; Galariotis, E. Features of Residential Energy Consumption: Evidence from France Using An Innovative Multilevel Modelling Approach. Energy Policy 2019, 125, 277–285. [Google Scholar] [CrossRef]
- Vadiveloo, M.K.; Sotos-Prieto, M.; Parker, H.W.; Yao, Q.; Thorndike, A.N. Contributions of Food Environments to Dietary Quality and Cardiovascular Disease Risk. Curr. Atheroscler. Rep. 2021, 23, 14. [Google Scholar] [CrossRef]
- Finlay, J.; Esposito, M.; Tang, S.; Gomez-Lopez, I.; Sylvers, D.; Judd, S.; Clarke, P. Fast-Food for Thought: Retail Food Environments as Resources for Cognitive Health and Wellbeing among Aging Americans? Health Place 2020, 64, 102379. [Google Scholar] [CrossRef]
- Naudin, S.; Solans Margalef, M.; Saberi Hosnijeh, F.; Nieters, A.; Kyrø, C.; Tjønneland, A.; Dahm, C.C.; Overvad, K.; Mahamat-Saleh, Y.; Besson, C.; et al. Healthy Lifestyle and the Risk of Lymphoma in the European Prospective Investigation into Cancer and Nutrition Study. Int. J. Cancer 2020, 147, 1649–1656. [Google Scholar] [CrossRef]
- Diaz, K.M.; Booth, J.N.I.; Calhoun, D.A.; Irvin, M.R.; Howard, G.; Safford, M.M.; Muntner, P.; Shimbo, D. Healthy Lifestyle Factors and Risk of Cardiovascular. Hypertension 2014, 64, 465–471. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Yin, C.; Shao, C. Heterogeneous Relationships between the Health-Related Lifestyle and Risk of Overweight and Obesity in Urbanizing China. J. Transp. Health 2021, 20, 101023. [Google Scholar] [CrossRef]
- Chu-Ko, F.; Chong, M.L.; Chung, C.J.; Chang, C.C.; Liu, H.Y.; Huang, L.C. Exploring the Factors Related to Adolescent Health Literacy, Health-Promoting Lifestyle Profile, and Health Status. BMC Public Health 2021, 21, 2196. [Google Scholar] [CrossRef]
- Liu, Q.; Huang, S.; Qu, X.; Yin, A. The Status of Health Promotion Lifestyle and Its Related Factors in Shandong Province, China. BMC Public Health 2021, 21, 1146. [Google Scholar] [CrossRef]
- Wang, R.; Feng, Z.; Liu, Y.; Qiu, Y. Is Lifestyle a Bridge between Urbanization and Overweight in China? Cities 2020, 99, 102616. [Google Scholar] [CrossRef]
| Food Group | Share of Food Subgroup % | Health Factors |
|---|---|---|
| Plant foods (69%) | 0.69× | |
| Vegetables/fruits/leaf salads/juices | 36 | 0.36 = 0.2484 |
| Wholemeal products/paddy | 28 | 0.28 = 0.1932 |
| Potatoes | 20 | 0.20 = 0.1380 |
| White-meal products/peeled rice | 12 | 0.12 = 0.0828 |
| Snacks and sweets | 4 | 0.04 = 0.0276 |
| Animal foods (29%) | 0.29× | |
| Fish/low-fat meat/low-fat meat products | 36 | 0.36 = 0.1044 |
| Low-fat milk/low-fat dairy products | 28 | 0.28 = 0.0812 |
| Milk/dairy products | 20 | 0.20 = 0.0580 |
| Meat products, sausages, eggs | 12 | 0.12 = 0.0348 |
| Bacon | 4 | 0.04 = 0.0116 |
| Fats and oil (2%) | 0.02× | |
| Oilseed rape/walnut oil | 36 | 0.36 = 0.0072 |
| Wheat germ oil/soybean oil | 28 | 0.28 = 0.0056 |
| Corn oil/sunflower oil | 20 | 0.20 = 0.0040 |
| Margarines/butter | 12 | 0.12 = 0.0024 |
| Lard/vegetable fat | 4 | 0.04 = 0.0008 |
| Variables | Description | Mean (Min, Max) |
|---|---|---|
| Outcome variables | ||
| Disease dummy | Yes = 1; No = 0 | 0.441 (0, 1) |
| Disease number | Count number of health-related diseases | 0.700 (0, 3) |
| Personal characteristics | ||
| Gender | Male = 1; Female = 0 | 0.511 (0, 1) |
| Age | Age in a single year | 64.27 (45, 118) |
| Marriage status | Legally married = 1; others = 0 | 0.835 (0, 1) |
| Education | High school and higher = 1; Other = 0 | 0.063 (0, 1) |
| Income | Annual income (¥10,000) | 1.629 (0, 60) |
| Physical activity | Doing physical activities more than 30 min every day = 1; otherwise = 0 | 0.535 (0, 1) |
| Drinking habit | Never drinking = 1; otherwise = 0 | 0.549 (0, 1) |
| Smoking habit | Never smoking = 1; otherwise = 0 | 0.639 (0, 1) |
| City-level Characteristics | ||
| mRFEI | Modified retail rood environment index (0–1) | 0.335 (0, 1) |
| HFDI | Healthy food diversity index (0–1) | 0.155 (0, 1) |
| Population density | Total number of population divided by city area (10,000 persons/km2) | 5.160 (0.097, 27.59) |
| GRP | Gross regional product (¥100,000,000) | 2.98 (0.016, 38.16) |
| Wage | Average wage of the city (¥10,000) | 8.266 (4.525, 17.32) |
| Buses | Total number of buses | 2512 (93, 38608) |
| Variable | Disease Dummy (Yes = 1; No = 0) | Disease Number | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Fixed parts | ||||
| Gender | −0.007 | −0.007 | −0.010 | −0.010 |
| Age | 0.004 *** | 0.004 *** | 0.007 *** | 0.008 *** |
| Marriage status | −0.008 * | −0.009 * | −0.020 * | −0.021 * |
| Education | −0.042 ** | −0.043 ** | −0.063 * | −0.064 * |
| Income | −0.040 * | −0.036 * | −0.007 * | −0.006 * |
| mRFEI | −0.255 ** | −0.427 ** | ||
| HFDI | −0.087 *** | −0.162 *** | ||
| Population density | −0.006 ** | −0.008 *** | −0.015 *** | −0.020 *** |
| GRP | −0.004 | −0.004 | −0.013 * | −0.014 ** |
| Wage | −0.010 * | −0.009 ** | −0.017 * | −0.020 * |
| Buses | 0.126 ** | 0.139 ** | 0.387 *** | 0.408 *** |
| City−tier | −0.023 ** | −0.022 ** | −0.048 * | −0.047 ** |
| Random parts | ||||
| 0.241 ** | 0.241 ** | 0.999 * | 0.999 * | |
| 0.048 * | 0.049 ** | 0.280 * | 0.280 ** | |
| Variable | Disease Dummy (Yes = 1; No = 0) | Disease Number | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Fixed parts | ||||
| Gender | 0.021 * | 0.021 * | 0.053 ** | 0.052 ** |
| Age | 0.004 *** | 0.004 *** | 0.007 *** | 0.007 *** |
| Marriage status | −0.009 | −0.010 | −0.022 | −0.022 |
| Education | 0.039 ** | 0.039 ** | 0.055 | 0.055 |
| Income | −0.004 * | −0.004 * | −0.008 * | −0.007 * |
| HLS | −0.033 * | −0.030 ** | −0.024 * | −0.034 ** |
| mRFEI | −0.243 ** | −0.333 ** | ||
| HFDI | −0.087 *** | −0.134 *** | ||
| mRFEI×HLS | −0.038 * | −0.048 ** | ||
| HFDI×HLS | −0.002 | −0.026 * | ||
| Population density | −0.005 ** | −0.008 *** | −0.015 *** | −0.020 *** |
| GRP | −0.004 | −0.004 | −0.013 * | −0.014 ** |
| Wage | −0.007 * | −0.009 * | −0.016 ** | −0.019 * |
| Buses | 0.128 *** | 0.142 *** | 0.390 *** | 0.413 *** |
| City-tier | −0.023 ** | −0.023 ** | −0.049 ** | −0.049 ** |
| Random parts | ||||
| 0.241 ** | 0.241 ** | 0.999 * | 0.998 * | |
| 0.049 * | 0.044 ** | 0.278 * | 0.258 ** | |
| Variable | Disease Dummy (Yes = 1; No = 0) | Disease Number | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Small cities | ||||
| HLS | −0.032 * | −0.031 * | −0.042 * | −0.041 * |
| mRFEI | −0.248 ** | −0.378 ** | ||
| HFDI | −0.108 ** | −0.213 ** | ||
| mRFEI×HLS | −0.066 * | −0.073 * | ||
| HFDI×HLS | −0.016 * | −0.018 * | ||
| Controls | Yes | |||
| Medium cities | ||||
| HLS | −0.023 * | −0.032 * | −0.025 * | −0.030 * |
| mRFEI | −0.167 * | −0.307 * | ||
| HFDI | −0.076 * | −0.117 ** | ||
| mRFEI×HLS | −0.029 * | −0.034 * | ||
| HFDI×HLS | −0.009 | 0.007 | ||
| Controls | Yes | |||
| Big cities | ||||
| HLS | −0.003 | −0.029 * | −0.018 * | −0.023 * |
| mRFEI | −0.080 * | −0.145 * | ||
| HFDI | −0.049 * | −0.043 * | ||
| mRFEI×HLS | −0.021 * | −0.027 * | ||
| HFDI×HLS | 0.010 | 0.003 | ||
| Controls | Yes | |||
| Variable | Disease Dummy (Yes = 1; No = 0) | Disease Number | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Low income | ||||
| HLS | −0.009 * | −0.023 ** | −0.014 * | −0.032 ** |
| mRFEI | −0.052 * | −0.129 * | ||
| HFDI | 0.083 | −0.061 | ||
| mRFEI×HLS | −0.032 * | −0.022 * | ||
| HFDI×HLS | −0.027 | −0.016 | ||
| Controls | Yes | |||
| Medium income | ||||
| HLS | −0.036 * | −0.020 ** | −0.034 * | −0.035 ** |
| mRFEI | −0.172 ** | −0.336 ** | ||
| HFDI | −0.039 * | −0.064 ** | ||
| mRFEI×HLS | −0.026 * | −0.045 * | ||
| HFDI×HLS | −0.049 | −0.017 * | ||
| Controls | Yes | |||
| High income | ||||
| HLS | −0.046 * | −0.068 ** | −0.061 * | −0.044 ** |
| mRFEI | −0.226 ** | −0.349 ** | ||
| HFDI | −0.188 ** | −0.248 *** | ||
| mRFEI×HLS | −0.032 * | −0.074 ** | ||
| HFDI×HLS | −0.013 | −0.036 * | ||
| Controls | Yes | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Z.; Luo, Y.; Zhang, Z.; Robinson, D.; Wang, X. Unraveling the Role of Objective Food Environment in Chinese Elderly’s Diet-Related Diseases Epidemic: Considering Both Healthy Food Accessibility and Diversity. Int. J. Environ. Res. Public Health 2022, 19, 13924. https://doi.org/10.3390/ijerph192113924
Zhang Z, Luo Y, Zhang Z, Robinson D, Wang X. Unraveling the Role of Objective Food Environment in Chinese Elderly’s Diet-Related Diseases Epidemic: Considering Both Healthy Food Accessibility and Diversity. International Journal of Environmental Research and Public Health. 2022; 19(21):13924. https://doi.org/10.3390/ijerph192113924
Chicago/Turabian StyleZhang, Zhaohua, Yuxi Luo, Zhao Zhang, Derrick Robinson, and Xin Wang. 2022. "Unraveling the Role of Objective Food Environment in Chinese Elderly’s Diet-Related Diseases Epidemic: Considering Both Healthy Food Accessibility and Diversity" International Journal of Environmental Research and Public Health 19, no. 21: 13924. https://doi.org/10.3390/ijerph192113924
APA StyleZhang, Z., Luo, Y., Zhang, Z., Robinson, D., & Wang, X. (2022). Unraveling the Role of Objective Food Environment in Chinese Elderly’s Diet-Related Diseases Epidemic: Considering Both Healthy Food Accessibility and Diversity. International Journal of Environmental Research and Public Health, 19(21), 13924. https://doi.org/10.3390/ijerph192113924





