Abstract
This study attempted to explore the barriers to physical activity of older patients with Hypertension. It aimed to provide robust evidence produced through their eyes. First, through the data analysis of the accelerometer and the decision of the research team, 10 out of the 30 applicants were invited to participate in a photovoice study. Photovoice is one example of participatory action research. Photovoice participants can communicate their unique experiences through photographs, providing a highly realistic and authentic perspective that is not possible to be understood with traditional qualitative research. This study inductively identified four main themes; health illiteracy, distortion of health information, fear of physical activity, and rejection of any life changes. Based on a specific understanding of the population’s perception of physical activity, this study attempted to provide evidence of why many elderly Korean patients with Hypertension stay inactive.
1. Introduction
In Korea, the prevalence of hypertension among older adults aged 70 years and older is overwhelming. Among people over the age of 70 years, 59.5% of men and 72.4% of women have Hypertension [1,2]. Hypertension is twice as high as the prevalence of diabetes, which is the second most common chronic disease among the elderly population in Korea. In 2022, a new guideline for assessing high blood pressure was changed to 130/80 mmHg. People with blood pressure at this standard are now categorized as a high-risk group. Korea ranks first in the world in increasing the number of hypertension patients based on the traditional standard of 140/90 mmHg [3]. With the new guidelines of 2021, the number of people with hypertension in Korea has exceeded 12 million [4].
Hypertension is one of the major risk factors associated with death [5]. Hypertension is a causal factor that can affect various functional disorders in the heart, brain, kidneys, eyes, etc., and can eventually lead to diseases such as stroke, chronic kidney disease, myocardial infarction, dementia, necrosis, hypertensive retinopathy, as well as sudden death [6,7]. Moreover, hypertension is known as a silent killer because it is difficult to recognize at an early stage.
There are several treatment modalities for hypertension that have been studied to assess their effectiveness. These include diet/nutritional counseling, smoking cessation programs, stress management [8], and the use of medication [9]. When hypertension is diagnosed, medication is prescribed [4].
One of the characteristics of older adults with hypertension is that they have high systolic blood pressure. As the age increases, the systolic blood pressure gradually increases, and after a certain age, the diastolic blood pressure tends to decrease. This is because the elasticity of blood vessels is weakened and stiffened with aging. However, older adults with hypertension can obtain sufficient benefits from regular physical activity, which reduces social costs.
Several previous studies have shown that physical activity has a positive effect on hypertension [10,11]. Current research also shows that the amount of physical activity has a positive effect on people diagnosed with hypertension, in addition to the use of medication. In other words, physical activity is one of the most effective interventions for patients with hypertension [1,12]. Other studies have shown that physical activity can reduce or eliminate the use of medication by controlling blood pressure levels as the cardiovascular system improves [13,14,15].
The American College of Sports Medicine (ACSM), World Health Organization, and National Institutes of Health provide physical activity guidelines for people with hypertension. Specifically, ACSM recommendations include that elderly patients with hypertension engage in aerobic exercise daily for at least 30–60 min at a moderate intensity level and resistance training/exercises 2–3 times a week. However, some studies have shown that low-intensity physical activity may also have a positive effect on hypertension [16,17]. Research studies from Korea have similarly reported that regular physical activity reduced the total cost of hypertension treatment by 30% [18]. Participation in physical activity can have a positive effect in terms of personal and social costs. Physical activity should be an essential treatment intervention for the older population with hypertension [18,19].
In Korea, several problems have been identified as impediments towards physical activity as an alternative or complementary treatment for hypertension. One of the first problems is the lack of consistent guidelines for physical activity among Koreans diagnosed with hypertension. Many countries have published physical activity guidelines for people with hypertension. However, it is difficult to find these guidelines in Korea and there are differences between these guidelines. The absence of specific and consistent guidelines for healthcare providers and the absence of healthcare providers who recommend them are negative factors for physical activity in older adults with hypertension [20]. Treatment of the elderly Korean population with hypertension should involve an interdisciplinary, collaborative approach that includes patients, healthcare providers, and exercise professionals. This interdisciplinary treatment approach can significantly improve the lifestyle and pharmaceutical adherence of this population, as well as improve overall health and reduce social costs [13].
The second problem identified is the lack of physical activity or exercise among the older population in Korea, especially those diagnosed with hypertension. In Korea, the older population is generally physically inactive. It is reported that about 77% of older adults do not participate in regular physical activity at least once a week [21]. The Korea Disease Control and Prevention Agency (KDCPA) reported that the walking practice rate for hypertensive patients in Korea over the age of 30 was about 38%, and similar figures were also observed in the area our research team studied. It can be reasonably estimated that the walking practice rate of hypertensive patients aged 70–75 years, the subject of this study, is much lower. Moreover, this fact is the main basis for inferring that the proportion of hypertensive patients aged 70–75 who are practicing a moderate-intensity level of physical activity suggested by ACSM is very low [2]. Physical activity is one of the most cost-effective interventions for older adults with hypertension, but when considering the physical activity level of the general older population, it can be reasonably inferred that older adults with hypertension may not actively participate in physical activity.
The third problem in Korean society can be the increase in the burden on the National Health Insurance Service (NHIS). In the case of Korea, where the NHIS has developed, the NHIS covers most of the cost of primary medication treatment for hypertension, which dominates the prevalence rate. The payment of such medical insurance is currently a huge burden on society [16]. Similarly, in North America, hypertension is the most costly of all cardiovascular diseases, with an estimated direct cost of $69.9 billion in 2010. In addition, in 2015, the indirect cost of hypertension was $27.2 billion, accounting for 23% of the total cost, and the direct cost was $91.4 billion [17].
Previous studies on the treatment and management of older hypertensive patients’ physical activity include intervention or experimental studies. Several studies looked at the utilization of various physical activities to reduce hypertension [20,21], financial costs [22,23], pharmacological and non-pharmacological treatment strategies as well as changes in dietary or nutritional intake [24,25], and various medical treatments including nutrition intake [26,27,28,29,30,31,32,33,34,35,36]. The problems of the existing studies so far are as follows: (1) There has been very little research examining objective data on the amount of physical activity in the “daily life” of older adults with hypertension, (2) Currently, there are participatory action research that analyzes the meaning or obstructive factors of physical activity from the perspective of the patient, rather than the researcher. Participatory action research utilizing photovoice has a relatively high possibility to reveal causes of the elderly population’s physical inactivity compared to traditional research methods [37]. In other words, previous research has failed to prove the delicate causes of low levels of physical activity in older adults with hypertension.
This study will utilize community participatory research with photovoice to investigate why Korean older adults with hypertension are not likely to participate in physical activity. This study will focus on understanding the emotional and other barriers to engaging in daily physical activity to reduce hypertension.
2. Method
2.1. Study Design
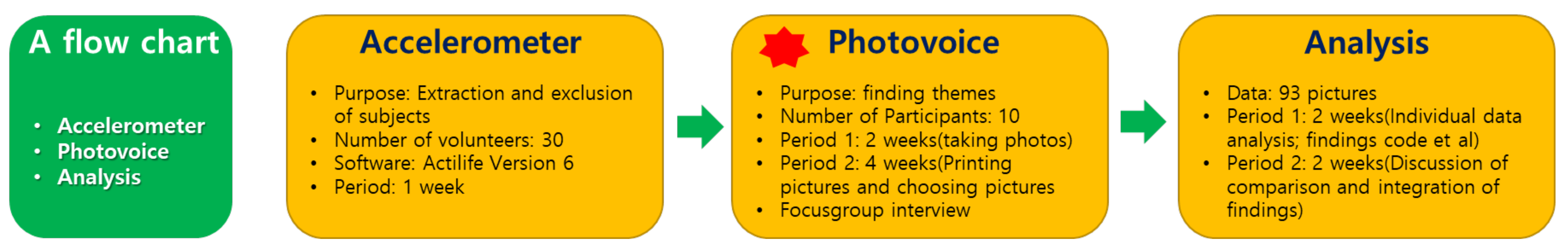
Figure 1 below briefly shows the flow of this study. This qualitative study can be seen as a participatory study in the sense that participants are directly involved in the research process through photovoice techniques. This study also corresponds to a case study in the philosophical aspect of qualitative research [38] because it explored older hypertensive patients’ physical inactivity [39,40]. This study was prepared based on the Consolidated criteria for reporting qualitative research (COREQ), a guideline for qualitative research. Unlike the previous study [21], where we relied on the study subjects’ statements (i.e., patients with panic disorder), we added the use of the accelerometer to assess physical activity instead of relying on the study subjects’ assessment of their physical activity levels (Table 1).
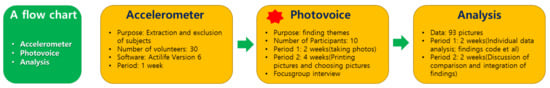
Figure 1.
A study Flow Chart.

Table 1.
The philosophical background of this study.
Therefore, in this study, ten subjects with low physical activity were selected based on objective decisions through the accelerometer. To this end, 30 older adults with hypertension first participated in the accelerometer measurement process. Afterward, to objectively check the amount of physical activity and to exclude the possibility of lowering physical activity due to another chronic disease, the co-researchers who are doctors, exercise physiologists, and aging research experts, held a meeting to select the final ten. Since the purpose of this process was to screen candidates to select ten suitable people to perform photovoice, it can be said that the work was conducted to improve the completeness of the photovoice research (Figure 1).
2.2. Keep as Participant Selection
We recruited 47 potential research participants through purposeful sampling from November 2021 to March 2022. All research volunteers filled out the questionnaires regarding demographic data, and the ACSM 2020 PAR-Q+ questionnaire was modified by Dr. Kim to check for chronic diseases. Among the 47 volunteers, 17 patients who had physical activity restrictions due to chronic diseases other than hypertension (e.g., depression) were excluded from participating in the accelerometer study process. Thirty participants were invited to the accelerometer process. For inclusion in the study, the co-researchers reviewed the 30 participants’ accelerometer data to objectively assess the amount of physical activity, or lack thereof. Exclusion criteria included lower physical activity due to other chronic diseases. Ten people who met the criteria were invited to participate in the photovoice research. Their general characteristics are shown in Table 2 below.

Table 2.
General Characteristics of Participant.
After that, ten people were invited to the photovoice research through a meeting of experts. All participants in this study were patients with hypertension living in Daegu, one of the largest cities in Korea. Participants in this study met the following criteria: (a) patient with hypertension, (b) older adult aged 70 to 75 years of Korean nationality, (c) a person with no problems with communication, (d) a person who does not meet the ACSM hypertension patient physical activity standard and (e) a person with no restrictions in physical activity due to other clinical diseases or musculoskeletal dysfunction (d was determined by M.D. Ryu). For reference, the reason why the participants of this study were operationally limited to those aged 70 to 75 was to minimize errors in the loss of physical activity due to natural aging (Extensive studies of patients aged 75 years and older are likely to cause large errors in quantitative values and subjective perceptions of physical activity). In addition, the number of participants considered suitable for the photovoice study is known to be between 7 and 15 individuals [37].
2.3. Research Team and Reflexivity
The research team consisted of two qualitative research experts (1 male and 1 female), one exercise physiologist (1 male), a psychological counselor (1 male), a social welfare field specialist (1 female), and a medical doctor (1 male) who want to understand the various problems experienced by research participants. Based on their own specialized experiences, the research team has rich knowledge and understanding of data collection and analysis for patients with hypertension. To avoid their specializations from becoming a bias during the study, the researchers conducted discussions and interactions in various ways during the research period. Specifically, Dr. Kim conceptualized and organized this study, Dr. Lee (male), a professional counselor, conducted three focus group interviews, and MD. Ryu (male), a medical doctor, accompanied all interviews to minimize the risk posed by interviewing patients. Dr. Kim and Dr. Butler analyzed all the qualitative data. Dr. Chung operated accelerometer data and supervised all the processes between Kinesiologist and the other specialist. Dr. Kim received various training related to qualitative research at the University of Illinois. In particular, Dr. Kim completed his education on the diversity of qualitative research through Dr. Denzin’s class as well as Dr. Greene’s class.
2.4. Measurement
In this study, an accelerometer was used to select photovoice participants based on objective evidence of the participant’s physical activity. An accelerometer typically uses a week’s worth of data. It objectifies physical activity at all times, including the study participant’s sedentary time. In addition, it is very accurate compared to the questionnaire technique, which reflects individual subjectivity in objectively understanding the amount of physical activity [41,42]. By using the present photovoice, participants can share their unique experiences through photographs, providing the study with a very realistic and authentic perspective that cannot be understood with traditional qualitative research [40]. In this study, the accelerometer is meaningful in accurately recruiting the research participants targeted by photovoice. Therefore, other indicators (ex. Steps, Bout, PA pattern et. al) produced by the accelerometer were not used in this study.
The photovoice study, which is the core of this study, was conducted with the final ten people selected through accelerometer data and expert meetings. In North America, photovoice research has recently expanded to the field of Kinesiology [37]. The present study is based on a protocol developed by Baker and Wang and modified by Kim, which is divided into three main stages: orientation, photovoice implementation, and focus group interview [43].
During the orientation, Dr. Kim, Dr. Lee, and M.D. Ryu attempted to create rapport with the participants and introduced them to all researchers and their achievements. In particular, Ryu, a medical doctor, was asked about their symptoms and medications. Finally, these interactions allowed the researchers and participants to become more trustworthy.
In the photovoice implementation session, participants were trained on the use of disposable cameras, the decision of what photographs to take, and ethical issues related to taking photographs. Every participant received disposable cameras, with an approximate capacity of 27 photographs. The disposable camera was for taking photographs related to perceived problems or barriers to physical activity. After the orientation, participants resumed their daily routines for approximately two weeks and took photographs [21]. In addition, gifts such as terabands and grip balls were given to the older adults who participated even in one research process.
2.5. Data Analysis
The accelerometer data was analyzed through Actilife software, and only physical activity data among various indexes were used for the study.
The photovoice data extracted by the objective amount of physical activity were analyzed with the photovoice analysis and content analysis [21]. Specifically, both researchers and participants in the study have worked on finding some initial codes, themes, theme reviews, entitling their photographs, etc. Researchers have conducted content analysis to discover and classify the statements and themes of interview data produced through focus groups as well as all the research participants’ reviews.
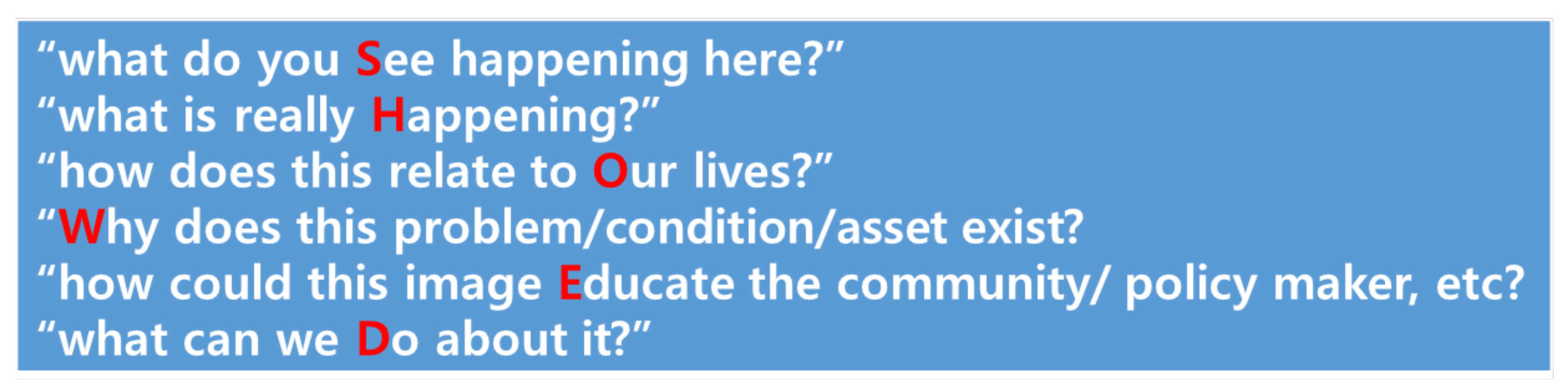
As a result of this process, 93 photos were acquired in total. At the discretion of the researcher, reduplicated photos, and not appropriate printed photos were excluded or important photos were added. The ten participants in this research also got involved in this classification work through pilot interviews and telephone conversations and selected up to four photos they thought were important. In the end, a total of 17 photos were selected that both research participants and researchers agreed were the most meaningful. A focus group interview of these selected photos was conducted with field memos. The SHOWeD technique was employed [37] to lead the focus group interview. The SHOWeD technique is described in Figure 2.
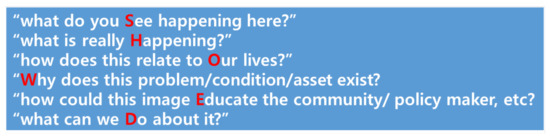
Figure 2.
Detail of the SHOWeD Technique.
Data collection for focus group interviews was conducted until saturation. In addition, all recordings of the interview were transcribed. After the research was completed, all data on photographs and interviews were discarded. All focus group interviews consisted of two sessions with four participants, one researcher, and one doctor. Each interview lasted between an hour and an hour and a half, with additional interviews being conducted for saturation.
All participants’ statements were recorded and transcribed. The recordings will be destroyed for research ethics after the study is finally published. The interview data were translated from Korean to English with the help of professional translation services. The problematic linguistic expressions based on cultural differences were carefully revised with the expert’s advice. Then, the entire manuscript, as well as the interview data, was modified with the help of editing services. Through these processes, the interviews were translated into English language.
Researchers interpreted the data from focus group interviews and significant statements. The principal researcher arranged the statements with photographs. Then, the research team had several rounds of discussion to derive and refine the statements and themes with photographs [21]. The flow of data analysis is shown in Table 3 below.

Table 3.
Data analysis process.
2.6. Authenticity and Trustworthiness
The present study attempted to increase authenticity and trustworthiness via triangulation, peer debriefing, an independent review panel, thick description, and an audit trail. For triangulation, data such as photographs, statements, and field memos were integrated. There have been several discussion processes to categorize themes for peer debriefings [44]. Further, two independent reviewers will screen the titles of our manuscript and then review the full texts. All researchers attempted to give a rich description, and external experts in the field of qualitative study were asked to audit the process and results of the study, and no particular problems were found. Finally, this study continuously applied the principle of reflexivity to minimize our influence on the participatory study [21,44,45].
3. Results
3.1. Accelerometer
“The ACSM recommends that individuals with hypertension engage in moderate- intensity (3.2–4.7 MET), aerobic exercise 5–7 d/wk” [16]
Of the 30 study participants who wore the accelerometer, only 25 succeeded in wearing the accelerometer continuously for a week. The remaining 5 participants were unable to wear the accelerometer continuously for a week, and the data generated from them were excluded from the analysis.
Although there are some studies that very low or low levels of physical activity are effective for hypertension [17], the ACSM guidelines, produced by experts and accumulated evidence, recommend moderate-intensity physical activity for older adults with hypertension. This is to give sufficient advantages to hypertensive patients through physical activities [16]. 7 out of 25 participants practiced moderate-intensity physical activity recommended. This result shows a similar tendency to the walking practice rate of 38.5% of hypertensive patients over the age of 30 in Korea. It was also found that the amount of physical activity naturally decreased with age. The results of this study also showed that less than a third of the older adults participated in moderate-intensity physical activity. The result may indicate that older adults with hypertension do not actively participate in physical activity.
The physical activity data of 25 participants are shown in the table above. Most of the research participants had a high proportion of sedentary life during the past week. Seven of the accelerometer process participants engaged in moderate-intensity physical activity for an average of 30 min or longer, which is the standard of physical activity for hypertensive patients. The rest of the participants did not meet the guidelines of ACSM. None of the applicants exceeded the ACSM’s light activity standard of an average of 1.6 MET per week. All of the light activity shown in Table 4 corresponds to very light activity based on ACSM guidelines for older hypertension patients. Most of the research participants showed the minimum degree of movement to lead a life and generally participated in a moderate-intensity activity at a low rate. Out of a total of 25 participants, 7 participants who exceeded the ACSM’s moderation activity criterion were first excluded from the study. Next, M.D. Ryu and the research team excluded four participants with chronic diseases that could interfere with physical activity in addition to hypertension. Finally, ten photovoice research participants were selected through a meeting of the research team (criterion and purposive sampling). As such, accelerometer data were importantly used to extract older adult hypertensive patients with objectively low physical activity (Table 4).

Table 4.
Physical Activity Data for a week measured by an accelerometer.
3.2. Photovoice
The photovoice research was analyzed based on the data produced from the research participants’ perspectives. Through the entire focus group interview process, it was found that the Korean elderly were more familiar with the word “exercise” than with the word “physical activity”, so the research team used the word “exercise” to interact with the participants. During the photovoice process, the research team found out that most of the participants, who had stated that they had no chronic diseases other than hypertension, also had other chronic diseases such as low back pain, mild arthritis, and chronic headaches. However, it was also recognized that this did not significantly affect the physical activity of older adults with hypertension. The crucial factors affecting the physical activity of older adults are summarized in the table below. And in this process, microscopic factors that interfere with the physical activity of elderly hypertensive patients were found. In this study, 17 photographs, 9 sub-themes, and 4 main themes emerged (Table 5).

Table 5.
Presentation of the obtained findings.
3.2.1. Health Illiteracy
Many studies have reported that physical activity is important for the prevention of hypertension and its complications. However, there was a big difference between the opinion of the academic world and the perception of patients. The older adults who participated in this study were generally unaware of the positive effects of physical activity on hypertension. They had no idea when, how much, or what kind of physical activity was effective. In addition, they were completely unaware of the existence of physical activity guidelines for hypertension.
Medication Dependency
Medication is the most common way to treat hypertension. Although other alternative methods have a positive effect on lowering blood pressure such as lifestyle, nutrition, and physical activity. However, some older participants in this study showed blind faith in using medication. The participant below directly shows the belief about medication through the picture of the blood pressure gauge.
The following research participant also made a similar statement with Figure 3.

Figure 3.
Blood pressure gauge.
Hypertension is nothing compared to other diseases…We only need to take one pill a day. Take your medicine and check your blood pressure! My blood pressure is completely normal. What are you worried about? Worrying too much is a worse habit… (I)
The following research participant also made a similar statement with Figure 4.

Figure 4.
Medication.
I take my medicine well…I also drank the onion juice (healthy food) that my children gave to me… No problem. I take medicine and my blood pressure is under control… Except for high blood pressure, I am healthy. I am not ill with a fatal disease. Don’t worry. (J)
Hypertension is a very dangerous factor that can damage the blood vessels of the brain, heart, and kidneys, and it can cause various complications such as stroke, myocardial infarction, heart failure, renal failure, arteriosclerosis, and certain cancers [45,46,47,48]. However, most of the older adults who participated in this study were not aware of this.
A Negative Reference Group
The older adults who participated in this photovoice study were negatively affected in physical activity due to a negative reference group (physically inactive older adults around them). According to M.S. Park, who works at a senior welfare center, there are a lot of older people over the age of 75 here, and most of them have hypertension. These older adults become a physically inactive reference group. In addition, it was observed that most of the older adults in the center preferred programs related to recreational activity over physical activity. In other words, it is natural for the study participants to see that people around them have hypertension but only take medicine and do their preferred activities without any intervention or care. In the center, individuals who manage hypertension with special care are rare, which can also be a negative cause of participation in physical activity (Figure 5).

Figure 5.
Space in the social welfare center.
Take a look here and there Does anyone exercise? Hypertension is not even a disease anymore. You only need to take one pill … No one works out. No one is exercising. If I exercise alone here, other people will look at me strangely. (B)
The following study participant showing Figure 4 was willing to participate in physical activity but did not because of peer pressure at the welfare center (Figure 6).
Figure 6.
Korean chess.
I know that exercise is good for everything, not just for hypertension. I also want to do it sometimes. But everybody plays like that (Figure 6), so I hang out too. Is it fun to exercise alone? (C)
Misperception of Appropriate Physical Activity
Some older adults who participated in this study thought that they were physically active. This indicates the difference between subjectivity and objectivity for physical activity. If this study did not employ the use of the accelerometer, it is assumed that this difference would have been overlooked. (Figure 7).
Figure 7.
Pedometer.
I don’t exercise like this. Is this machine (accelerometer) broken? I’ve also tried a pedometer, but it is not accurate. I cannot believe this (result)…I cannot understand. (A)
The above study participant had a strong belief in his subjective cognition that he could not even trust the accuracy of the accelerometer. The following study participant also talked similarly about his exercise participation with Figure 8.
Figure 8.
Table tennis court.
I also play table tennis and walk… I exercise a lot, but the machine is weird. Is this machine accurate? No matter how I think about it, it’s weird… (D)
M.S. Park, who is well acquainted with this study participant, explains that the participant usually does exercise for a while and then quits because it is hard. This participant also plays table tennis, but after a while, he usually sits and rests. It is noteworthy that the amount of physical activity most objectively measured with an accelerometer does not match the amount of physical activity subjectively perceived by hypertensive patients.
3.2.2. Distortion of Health Information
Unlike Health Literacy, the older adults who participated in this study reinterpreted unspecific information on their own or received distorted information from those around them. Therefore, there were cases in which they could not do physical activity even if they were willing to do or it were unable to perform the physical activity due to incorrect information.
Inappropriate Health Information from M.D.
The participant in the study below did not understand the words “moderate exercise” often referred to by doctors when they prescribe medication. This is not a problem for the study participant. It may be possible that Korean physicians may not be aware that patients do not understand what is meant by moderate physical activity. Therefore, they may assume that patients know what moderate physical activity entails and do not seek patient’s understanding (Figure 9).

Figure 9.
Hospital.
Every time I go to the hospital, the doctor says, ‘Take your medicine and exercise moderately’, but I don’t know what he means by moderate exercise. So I just walk around town from time to time on my terms. The doctor told me to exercise moderately, and after I was diagnosed with hypertension, I stopped going to my favorite gate ball. When I hit the ball, I have to use my strength… I wonder if I’m walking too much while playing gateball… (B)
The study participant below believed that he had the will to do the physical activity but believed the wrong information that people with hypertension could not do it because their blood pressure would rise if they did the physical activity (Figure 10).

Figure 10.
Playground.
Figure 10 shows the playground…I know that exercise is good…But I have hypertension… When hypertensive patients exercise… It is said that exercise makes blood pressure increase and it’s dangerous.… But what kind of exercise can I do? I also want to do my favorite exercise and go to the sauna if I don’t have hypertension. (F)
Regular physical activity by itself lowers blood pressure [49]. Although physical activity has a positive effect on blood pressure, regardless of medication, the older adults in this study did not participate in physical activity due to the acquisition of insufficient and distorted information. Some of this misinformation may be due to physicians not providing accurate information regarding physical activity and its effects on reducing blood pressure.
Lack of Expertise in the Organization
This study population of older adults attended a senior welfare center. There is no obligation for nurses or doctors to provide services at senior welfare centers in Korea. It is also not obligatory to hire a professional who can guide physical activity. Therefore, most of the systems in the center are operated by social workers. In this regard, it is politically favorable for the senior welfare center not to engage in excessive physical activity. In addition, it is not easy to obtain related information. This has an important influence on the wrong choice of physical activity among older adults.
The following study participant made the statement with Figure 11.

Figure 11.
The back of a social worker.
Is there anyone here who is not sick at the welfare center? Each one hurts. But who teaches us what to do?… There is an exercise program. But how do I know if it’s right for me or not? I’m not an expert… Then I just sit down, watch TV, talk, and play with people. (C)
As a result of analyzing the physical activity programs of several senior welfare centers, the research team found that most of them required the lowest level of physical movement. For example, the most provided exercise was the one for flexibility and balance. A more serious problem is that the proportion of physical activity programs in the total programs provided by senior welfare centers is very low. This may be due to the current physical activity programs that are organized with a focus on preventing accidents or injuries that may occur during physical activity, rather than focusing on individualized physical activity programs.
One participant showed Figure 12 and stated as follows:
Figure 12.
Friends.
There are so many people here, so we have to choose the program by ourselves. I have hypertension, but who makes a program for hypertensive patients? No… Still, my friends know that I have hypertension, so they tell me not to take some programs (physical activity)… (G)
This participant was accepting the reality of insufficient and distorted information from neighbors or friends quite naturally. A problem with the institution affects the older adults individually.
3.2.3. Fear of Physical Activity
Trauma or the Fear Experienced
Some of the research participants had negative feelings about physical activity. This is not limited to hypertensive patients, but it is common in older adults. Whether it happened to them or others, some things can be traumatic for older adults.
The following study participant talks about her trauma through Figure 13.

Figure 13.
Emergency.
My son also had hypertension. He often exercise, saying that he could get better when he exercised. But one day, he suddenly collapsed, and from then on, he was hospitalized…After all, I am older than him, what kind of exercise can I do? My son is like that now after he exercised… I cannot. (I)
The study participant below shares a similar experience.
My sister had hypertension, and she collapsed from walking too much… So I (with hypertension) also took a computed tomography… From then on, I try not to do anything too hard. (H)
It is not possible to find out exactly why the son with hypertension suffers from sequelae because we could not get a detailed explanation. We also did not get any details of why the study participant collapsed from walking. However, these incidents were extremely rare cases. As a result, this study participant had trauma from physical activity and for this reason, she refused to engage in physical activity
In the following case, the study participant stopped doing physical activity after experiencing a negative experience. This can be seen as a kind of traumatic reaction (Figure 14).

Figure 14.
Korean 911(119).
I like mountains, so I have been climbing for a long time … I went climbing while taking hypertension medication. But it was a cold day, maybe… I was going up the mountain regardless of the weather. Suddenly I felt dizzy and my legs were losing strength… Other hikers called 911 (See Figure 14). It must have been about two years ago. Since then, I haven’t exercised at all. (E)
The study participant below also made very similar statements.
I used to walk often because I heard that exercise was good for hypertension… In the evening… But one day, while walking, my hands started to swell. I was startled, so I quit exercising right away, went home, and took a rest. I haven’t exercised at all since then. I can just take the medicine… For what benefit did I do it… (J)
Numbness, pain, discomfort, and muscle aches are the side effects that hypertensive patients can have after participating in physical activity [49], and various side effects can appear when exercising at an appropriate level or higher. However, physical changes caused by physical activity can be a great fear for older adults when they do not know these facts.
Anticipatory Anxiety
The following study participant was unable to participate in physical activity due to anticipatory anxiety (Figure 15).
Figure 15.
Friends.
It would be fine if I exercised with my friends (See Figure 15) at my age… <omitted>… If I fall while exercising alone, who can save me? I can’t help but die. Those who don’t have many friends like me are not good at doing things together. According to the news, an old man died while climbing the stairs and was found a few days later. I also have hypertension… I am scared. (H)
The following study participant also made similar statements with Figure 16.
Figure 16.
Pill case.
I went out to exercise because I heard that exercise is good for health… <omitted>… I remembered that I had not taken my pills for hypertension in the morning! All of a sudden I got scared… So I went straight home and took some medicine… I still carry my medicine with me all the time. After that, I cannot exercise… There are many times when I am confused as to whether I have taken the medicine or not… I often get confused as to whether I took the medicine or not…(E)
Due to extremely rare negative experiences or personal mechanisms to induce fear or anxiety, some older adults in this study were avoiding physical activity.
3.2.4. Rejection of Any Changes
The Importance of the Current Lifestyle
Finally, some study participants admitted that their current blood pressure was being maintained with medication and spoke as if they had no will to improve (Figure 17).

Figure 17.
Cigarette.
Do I have to exercise, watch my diet, and quit drinking and smoking to live longer at this age? I take medication for hypertension and my blood pressure is being treated well. So I do whatever I want to do. I eat my favorite food and enjoy drinking and smoking. (G)
As seen in Figure 17, the participant currently drinks and smokes. Drinking and smoking are the main factors that cause blood pressure increase, so hypertensive patients must avoid them. The participant knew this, but he was just satisfied with his current life. He was not aware of the reasons to improve his lifestyle. It can be thought that hypertension, which is called a silent killer, has different characteristics from diseases that alert patients because the symptoms of hypertension are not easily recognized, or there is no particular physical response to the process leading to complications.
Lack of Motivation to Improve Their Life
The following study participant showed an unwillingness to improve his lifestyle through Figure 18.

Figure 18.
Food.
I’m weak-willed, so no matter what I do, I can’t do it well until the end. Even if I go on a diet, I always fail. I tried to exercise too, but it doesn’t work for me. I just take medicine well… haha I just want to live well… I’ll die when I die… haha. (F)
One study participant made a similar statement with Figure 19.
Figure 19.
Television.
Exercise? How long to live.… I don’t want to get stressed and I want to do what I want to do… Who here doesn’t have hypertension? I want to live happily while I am alive. (I)
Although the statements of the two study participants appear similar, the details are slightly different. The first participant was satisfied with the present and had a strong attachment to the things she was doing, whereas the second participant had an easygoing personality and did not have great greed in all areas, including physical activity, due to his weak will.
Hypertension is very common, but it is also a very scary disease. However, the above research participants seemed to regard hypertension as having a cold. Both participants appeared so calm and carefree that the researcher was surprised that they were not worried about their hypertension.
4. Discussion
“Why more Korean older adults with hypertension are physically inactive?”
This study challenged to verify the microscopic cause of “Why do older adults with hypertension not participate in physical activity?” based on objective data from accelerometers that the majority of them do not engage in physical activity to improve hypertension. The final 10 participants who were physically inactive participated in the photovoice study. They repeatedly explored the unique interfering factors of their physical activity together with the research team until theoretical saturation was reached. As a result, this study discovered four decisive main themes: Health Illiteracy, Distortion of Health Information, Fear of Physical Activity, and Rejection of any changes.
4.1. Health Illiteracy
The first sub-theme related to this is “Medication Addition”. Although all study participants are taking medications for hypertension, hypertension is a terrifying chronic disease that requires overall well-controlled lifestyle habits [50]. However, some older adults in this study had a strong belief that medication would solve everything. Therefore, no reason to do physical activity daily. To them, hypertension was perceived as a mild chronic disease requiring only medication. This greatly increased the possibility of other health complications, as mentioned earlier [51]. Second, about “A negative reference group”, some older adults who participated in this study had negative influences from those around them. Due to their peers who also have hypertension and take medication to control it believed that they do not need to engage in physical activity, the study participants may be less likely to engage in physical activity as well. It is well known that peer pressure influences individual behaviors [52]. The study participants were not aware of the severity of having hypertension and did not have the opportunity to lower their dependence on medication, nor have support from their peers. Studies have shown that social support, lifestyle improvement, and physical activity decrease the dependence on the use of medication [53]. The third theme is “Misperception of appropriate physical activity” This was a very significant finding because this study objectively measured physical activity with an accelerometer. The difference between individual objectivity and subjectivity regarding physical activity was verified. Significantly, the meaning of “moderate physical activity” for older adults who are not experts in physical activity can vary greatly from person to person, while guidelines [54] published by most reliable institutions recommend moderate or higher physical activity to get benefits from physical activity. The lack of understanding of the level of physical activity is similarly reported in a Polish study [51].
4.2. Distortion of Health Information
The first sub-theme is “Inappropriate health information from M.D.” According to the statements of the study participants, doctors recommend “moderate exercise” while prescribing medication every month. However, it is more difficult for patients to estimate the appropriate physical activity for them, as they do not know how much moderate-intensity physical activity means because they are not a physical education expert. M.D.’s inadequate patient education has already been reported in research [55]. M.D.’s must provide older patients with hypertension with recommendations for cost-effective lifestyle interventions and individualized recommendations for physical activity as well as medication treatment. However, according to the statements of the study participants in this study, most doctors give counseling within 5 minutes, prescribe medication, and repeatedly talk about “appropriate physical activity and diet control”without providing specifics. Based on the statements, it can be inferred that there is little education on the treatment of hypertension, which calls for a change in patient counseling methods in the Korean medical community. In this regard, M.D. Ryu shared his opinion as follows.
What I’m talking about now is the opinions I’ve shared with some doctors around me, so it’s not a generalized answer. But I’m sharing a conversation with doctors around me about why they don’t prescribe exercise to older adults with hypertension. First of all, we rarely learn about specific exercise regimens. I recommend to patients to exercise while looking for medical guidelines or literature, but in reality, there are many difficulties… Because doctors are more interested in medication treatment, it is difficult to give exercise prescriptions. The second reason is that there is a lot of outpatient treatment, so there is less time to devote to each patient. So I have no choice but to spend my time on other more important issues (importance of taking medications, explaining test results, etc.) than exercise. Lastly, most hypertensive patients are mainly middle-aged or elderly. In fact, I know they usually don’t exercise even if I recommend exercising. So, rather, it seems to emphasize the importance of exercise relatively for young hypertensive patients.M.D. Ryu’s Statement
The second is the “Lack of expertise in the organization”. As mentioned above, senior welfare centers in Korea (most elderly care-related facilities) are not obligated to hire nurses, doctors, or physical activity specialists. Therefore, it is safe to say that most of the center programs are mainly operated by social workers. For social workers without specialized knowledge, it is practically reasonable to provide the lowest level of physical activity programs when older adults request physical activity programs. At these facilities, it may be more important to prevent injuries or accidents that may occur while older adults with various chronic diseases are physically active, than to improve their health. As a result of the observation of this research team, most of the physical activity programs at senior welfare centers were recreational programs, and many programs provided the lowest level of movement for groups rather than individuals. Accordingly, it is essential that Korean welfare centers need to be innovative, and request an appropriate budget allocation from the government to construct a professional human infrastructure, and secure the social responsibility of health care providers and others [56]. This will allow them to actively intervene in the health and wellness of the elderly.
As shown in the above two themes, it is socio-environmentally difficult for the elderly in Korea to obtain accurate information to protect their health.
4.3. Fear of Physical Activity
Through the themes mentioned before, it is possible to better understand why some older adults who participated in this study have a fear of physical activity. The first sub-theme that appeared in this theme is “Trauma or the fear experienced”. One of the participants gave up doing a physical activity because she was afraid of the situation in which her son, who also has hypertension, fell while exercising, and was afraid of the changes in the body that can normally occur during physical activity. In this case, a psychological treatment that can give a message that physical activity is safe may be necessary. Psychological treatment can improve the quality of life [57]. In the second sub-theme, study participants talk about fear of things that have not happened. This can be seen as a kind of “Anticipatory anxiety”. Through news and other indirect experiences, negative aspects of physical activity are recognized, which leads to avoidance of physical activity [57]. Furthermore, if the risk of accidents from physical activity due to other chronic diseases is significantly low, then older adults with hypertension should be encouraged to engage in physical activity by the current guidelines [49]. It has been noted that high-intensity physical activity has more disadvantages than significant advantages for older adults with hypertension, as compared to moderate-intensity physical activity [20]. To help reduce the fear and anxiety of exercising as mentioned by some of the study participants, it is recommended that participate in physical activity if they are accompanied by assistance from family members or close groups. Studies have shown that exercising with family, friends, or in a group can reduce such fears [58].
4.4. Rejection of Any Changes
Some of the study participants older adults who participated in this study believed that they were safe and only needed to take the required medication to control their HBP and did not need to do anything else to lower their hypertension with the current blood pressure index, which is controlled by medications, and did not show any other will to improve. This is a reflection of the first sub-theme, “the importance of the current lifestyle.” One study participant, who expressed his thoughts through a picture of a cigarette, stated that he was living his life doing whatever he wanted without worrying too much because his blood pressure was well controlled while he was taking medication. He stated that he did not control drinking alcohol or smoking at all. Furthermore, he stated that he was satisfied with his present life. He prioritized his present life over the future. This seems to be the case for one individual, but in general, the elderly tend to be “current oriented” [59]. This means that there is a stronger tendency to maintain the present way of life rather than considering the big gain in the foreseeable future. This patient seems to be pursuing the lifestyle he wants (alcohol, cigarettes, food, etc.) rather than worrying about the various complications that hypertension can cause. Other studies focusing on older adults have also reported this shown tendency [43]. To change this tendency among older adults, it is important to make them understand the relative advantage among the five most important factors to accept change, according to Rogers’ Diffusion of Innovation [59]. For example, the confidence and satisfaction that physical activity can lead to positive experiences among the older population with hypertension if they are repeatedly given encouragement. The second sub-theme is “Lack of motivation to improve their lives”. Regardless of whether the research participants are satisfied with their current life or not, their unwillingness of them to improve their overall health, as expressed through food, TV, and photographs, is common among older adults [60]. This lack of motivation to change their lifestyle to improve their overall health can also have psychological effects on their caregivers. Therefore, we propose to incorporate specific short-term goals that can motivate this older population with hypertension to engage in physical activity. Having short-term goals regarding physical activity can have a positive effect on their overall health by reducing their reliance on medication only for controlling hypertension. To promote physical activity among an older person with hypertension, this approach should include all those involved with their care, including the older person.
5. Limitations
The present study is subject to the following limitation. Although this study pursued more sophisticated sampling through the objective data of the amount of physical activity produced by the accelerometer, it did not examine any medical or physiological causal relationship using the accelerometer data. Moreover, resistant training or water activities are not analyzed by an accelerometer. That is, the data produced in this process cannot be given any meaning other than that it has been sampled. This point is related to the fact that only resistance training is not usually prescribed to hypertensive patients [61]. In addition, this study thoroughly follows the philosophy of qualitative research. Thus, the study conducted a photovoice with 10 research participants. This means that the findings of this study are not externally generalized. However, in a similar environment, this study can provide more precise information. Although photovoice, a method of participatory action research, was used as the research technique, this does not deviate from the framework of this study as a case study. Therefore, the findings of this study cannot be applied to all older adults with hypertension. That is, this study has an inherent limitation in that it cannot be externally generalized. However, it is significant in that the knowledge produced by this study can be applied more precisely to older adults in similar circumstances. This is expressed as an internal generalization by qualitative researchers [40]. Therefore, the accumulation of knowledge produced in this way is essential, which broadens the scope of research.
6. Conclusions
Many studies have investigated the benefits of physical activity in older adults with hypertension [8,9,10]. In addition, there have been some studies that directly analyzed the barriers to physical activity in older adults with hypertension [62]. However, most of the studies related to hypertension and physical activity in older adults have been conducted as experimental studies, questionnaire studies, and meta-analyses. There are no studies on how physical activity, which has a very positive effect on older adults with hypertension, is perceived from older adults’ perspective. This study attempted to find out why the majority of older adults with hypertension in Korea do not actively participate in physical activity by using participatory action research called photovoice. Participants in this study expressed their barriers to physical activity that were difficult to predict, difficult to understand from the outside, and invisible through photovoice. This study ultimately found barriers to participation in physical activity directly perceived by older adults with hypertension. If this kind of research continues and results are accumulated, the spectrum of intrinsic generalizations that can be applied in more diverse environments can be broadened. This research team expects that the quality of life of older adults with hypertension will be improved as the follow-up research continues so that they can enjoy a successful aging process. In addition, from a social and national perspective, we expect that the social costs consumed by pathological symptoms of older adults will be reduced through the continuous production of studies similar to this study.
Author Contributions
Conceptualization, K.-O.K. and J.-H.R.; methodology, K.-O.K.; formal analysis, K.-O.K., G.-Y.L., M.B. and J.-H.R.; investigation, G.-Y.L. and S.-H.P.; resources, G.-Y.L. and S.-H.P.; data curation, K.-O.K., G.-Y.L. and M.B.; writing—original draft preparation, K.-O.K. and M.B.; writing—review and editing; M.B.; writing—review and editing; visualization, H.-R.C.; supervision, J.-H.R. and H.-R.C.; project administration, K.-O.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study has been approved by the Kyungil University, Institutional Review Board (IRB) for the protection of human subjects (104459-202103-HR-002-01) and is additionally conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study after reading the research statement.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written and audio oral informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available to protect respondent privacy.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lee, H.-Y. New definition for hypertension. J. Korean Med. Assoc. 2018, 61, 485–492. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. Chronic Disease Health Statistics; Survey, C.H., Ed.; Korea Disease Control and Prevention Agency: Cheongju, Korea, 2022.
- Joo, K.M.; Hak, L.J.; Chul, H.S.; Ho, M.C.; Il, K.D. Comparative analysis of the prevalence of high blood pressure and diabetes according to the BMI of elderly women in Korea and the number of walking days for a week. J. Sport. Sci. 2021, 34, 55–62. [Google Scholar]
- Kim, H.C.; Cho, S.M.J.; Lee, H.; Lee, H.-H.; Baek, J.; Heo, J.E. Korea Hypertension Fact Sheet 2020: Analysis of Nationwide Population-Based Data. Clin. Hypertens. 2021, 27, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Arima, H.; Barzi, F.; Chalmers, J. Mortality patterns in hypertension. J. Hypertens. 2011, 29, S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Khosla, N.; Kalaitzidis, R.; Bakris, G.L. The kidney, hypertension, and remaining challenges. Med. Clin. N. Am. 2009, 93, 697–715. [Google Scholar] [CrossRef] [PubMed]
- Ponnuchamy, B.; Khalil, R.A. Cellular mediators of renal vascfular dysfunction in hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 296, R1001–R1018. [Google Scholar] [CrossRef]
- Rabi, D.M.; McBrien, K.A.; Sapir-Pichhadze, R.; Nakhla, M.; Ahmed, S.B.; Dumanski, S.M.; Butalia, S.; Leung, A.A.; Harris, K.C.; Cloutier, L.; et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can. J. Cardiol. 2020, 36, 596–624. [Google Scholar] [CrossRef]
- Flack, J.M.; Adekola, B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc. Med. 2020, 30, 160–164. [Google Scholar] [CrossRef]
- Bakker, E.A.; Sui, X.; Brellenthin, A.G.; Lee, D.-C. Physical activity and fitness for the prevention of hypertension. Curr. Opin. Cardiol. 2018, 33, 394–401. [Google Scholar] [CrossRef]
- Lin, Y.-Y.; Lee, S.-D. Cardiovascular benefits of exercise training in postmenopausal hypertension. Int. J. Mol. Sci. 2018, 19, 2523. [Google Scholar] [CrossRef]
- Pescatello, L.S.; Buchner, D.M.; Jakicic, J.M.; Powell, K.E.; Kraus, W.E.; Bloodgood, B.; Campbell, W.W.; Dietz, S.; Dipietro, L.; George, S.M.; et al. Physical activity to prevent and treat hypertension: A systematic review. Med. Sci. Sports Exerc. 2019, 51, 1314–1323. [Google Scholar] [CrossRef]
- Naci, H.; Salcher-Konrad, M.; Dias, S.; Blum, M.R.; Sahoo, S.A.; Nunan, D.; Ioannidis, J.P. How does exercise treatment compare with antihypertensive medications? A network meta-analysis of 391 randomised controlled trials assessing exercise and medication effects on systolic blood pressure. Br. J. Sport. Med. 2019, 53, 859–869. [Google Scholar] [CrossRef]
- Pescatello, L.S. Exercise measures up to medication as antihypertensive therapy: Its value has long been underestimated. Br. J. Sport. Med. 2019, 53, 849–852. [Google Scholar] [CrossRef]
- Dai, L.; Jiang, Y.; Wang, P.; Chen, K. Effects of Three Traditional Chinese Fitness Exercises Combined with Antihypertensive Drugs on Patients with Essential Hypertension: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Evid. Based Complement. Altern. Med. 2021, 2021, 2570472. [Google Scholar] [CrossRef]
- Riebe, D.; Ehrman, J.K.; Liguori, G.; Magal, M.; Medicine, A.C.o.S. ACSM’s Guidelines for Exercise Testing and Prescription; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2018. [Google Scholar]
- Pazmino, L.; Esparza, W.; Aladro-Gonzalvo, A.; León, E. Impact of Work and Recreational Physical Activity on Prediabetes Condition among US Adults: NHANES 2015–2016. Int. J. Environ. Res. Public Health 2021, 18, 1378. [Google Scholar] [CrossRef]
- Yoon, E.S.; Choo, J.; Kim, J.-Y.; Jae, S.Y. Effects of isometric handgrip exercise versus aerobic exercise on arterial stiffness and brachial artery flow-mediated dilation in older hypertensive patients. Korean J. Sport. Med. 2019, 37, 162–170. [Google Scholar] [CrossRef]
- O’Brien, M.W.; Johns, J.A.; Dorey, T.W.; Frayne, R.J.; Fowles, J.R.; Mekary, S.; Kimmerly, D.S. Meeting international aerobic physical activity guidelines is associated with enhanced cardiovagal baroreflex sensitivity in healthy older adults. Clin. Auton. Res. 2019, 30, 139–148. [Google Scholar] [CrossRef]
- Ahn, K.T.; Jin, S.-A.; Jeong, J.-O. Diagnosis and Treatment of Hypertension: Based on the Guidelines of the Korean Society of Hypertension. J. Korean Neurol. Assoc. 2019, 37, 123–134. [Google Scholar] [CrossRef]
- Kim, K.-O.; Ryu, J.-H.; Chung, H.-R.; Butler, M.; Gritzmacher, D. Understanding the Life, Pain, and Barriers to Physical Activity in Korean Patients with Panic Disorder: Photovoice Inquiry. Int. J. Environ. Res. Public Health 2021, 18, 8140. [Google Scholar] [CrossRef]
- Talamonti, D.; Vincent, T.; Fraser, S.; Nigam, A.; Lesage, F.; Bherer, L. The Benefits of Physical Activity in Individuals with Cardiovascular Risk Factors: A Longitudinal Investigation Using fNIRS and Dual-Task Walking. J. Clin. Med. 2021, 10, 579. [Google Scholar] [CrossRef]
- Arija, V.; Villalobos, F.; Pedret, R.; Vinuesa, A.; Jovani, D.; Pascual, G.; Basora, J. Physical activity, cardiovascular health, quality of life and blood pressure control in hypertensive subjects: Randomized clinical trial. Health Qual. Life Outcomes 2018, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Helgeson, S.A.; Menon, D.; Helmi, H.; Vadlamudi, C.; Moss, J.E.; Zeiger, T.K.; Burger, C.D. Psychosocial and financial burden of therapy in USA patients with pulmonary arterial hypertension. Diseases 2020, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhao, D.; Guo, J.; Lai, Y.; Chen, L.; Jin, S.; Huang, Y. Economic burden of depressive symptoms conditions among middle-aged and elderly people with hypertension in China. Int. J. Environ. Res. Public Health 2021, 18, 10009. [Google Scholar] [CrossRef]
- Cleven, L.; Krell-Roesch, J.; Nigg, C.R.; Woll, A. The association between physical activity with incident obesity, coronary heart disease, diabetes and hypertension in adults: A systematic review of longitudinal studies published after 2012. BMC Public Health 2020, 20, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Gambardella, J.; Morelli, M.B.; Wang, X.; Santulli, G. Pathophysiological mechanisms underlying the beneficial effects of physical activity in hypertension. J. Clin. Hypertens. 2020, 22, 291. [Google Scholar] [CrossRef] [PubMed]
- Rhee, E.-J.; Cho, J.-H.; Kwon, H.; Park, S.-E.; Jung, J.-H.; Han, K.-D.; Park, Y.-G.; Park, H.S.; Kim, Y.-H.; Yoo, S.-J.; et al. Association between abdominal obesity and increased risk for the development of hypertension regardless of physical activity: A nationwide population-based study. J. Clin. Hypertens. 2018, 20, 1417–1426. [Google Scholar] [CrossRef]
- Beyhaghi, H.; Viera, A.J. Comparative cost-effectiveness of clinic, home, or ambulatory blood pressure measurement for hypertension diagnosis in US adults: A modeling study. Hypertension 2019, 73, 121–131. [Google Scholar] [CrossRef]
- Burnier, M.; Polychronopoulou, E.; Wuerzner, G. Hypertension and drug adherence in the elderly. Front. Cardiovasc. Med. 2020, 7, 49. [Google Scholar] [CrossRef]
- Oliveros, E.; Patel, H.; Kyung, S.; Fugar, S.; Goldberg, A.; Madan, N.; Williams, K.A. Hypertension in older adults: Assessment, management, and challenges. Clin. Cardiol. 2020, 43, 99–107. [Google Scholar] [CrossRef]
- Herrod, P.J.; Doleman, B.; Blackwell, J.E.; O’Boyle, F.; Williams, J.P.; Lund, J.N.; Phillips, B.E. Exercise and other nonpharmacological strategies to reduce blood pressure in older adults: A systematic review and meta-analysis. J. Am. Soc. Hypertens. 2018, 12, 248–267. [Google Scholar] [CrossRef]
- De Lange-Jacobs, P.; Shaikh-Kader, A.; Thomas, B.; Nyakudya, T.T. An Overview of the Potential Use of Ethno-Medicinal Plants Targeting the Renin–Angiotensin System in the Treatment of Hypertension. Molecules 2020, 25, 2114. [Google Scholar] [CrossRef]
- Lan, N.S.H.; Massam, B.D.; Kulkarni, S.S.; Lang, C.C. Pulmonary arterial hypertension: Pathophysiology and treatment. Diseases 2018, 6, 38. [Google Scholar] [CrossRef]
- Greco, A.; Brugnera, A.; Adorni, R.; D’Addario, M.; Fattirolli, F.; Franzelli, C.; Giannattasio, C.; Maloberti, A.; Zanatta, F.; Steca, P. Protein intake and physical activity in newly diagnosed patients with acute coronary syndrome: A 5-year longitudinal study. Nutrients 2021, 13, 634. [Google Scholar] [CrossRef]
- Yu, H.-J.; Li, F.; Hu, Y.-F.; Li, C.-F.; Yuan, S.; Song, Y.; Zheng, M.; Gong, J.; He, Q.-Q. Improving the metabolic and mental health of children with obesity: A school-based nutrition education and physical activity intervention in Wuhan, China. Nutrients 2020, 12, 194. [Google Scholar] [CrossRef]
- Baker, T.A.; Wang, C.C. Photovoice: Use of a participatory action research method to explore the chronic pain experience in older adults. Qual. Health Res. 2006, 16, 1405–1413. [Google Scholar] [CrossRef]
- Onwuegbuzie, A.J.; Leech, N.L. A call for qualitative power analyses. Qual. Quant. 2007, 41, 105–121. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing among Five Approaches; Sage Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Berkemeyer, K.; Wijndaele, K.L.; White, T.O.H.; Cooper, A.J.M.; Luben, R.; Westgate, K.L.; Griffin, S.J.; Khaw, K.-T.; Wareham, N.J.; Brage, S. The descriptive epidemiology of accelerometer-measured physical activity in older adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 2. [Google Scholar] [CrossRef]
- Mañas, A.; del Pozo-Cruz, B.; Guadalupe-Grau, A.; Marín-Puyalto, J.; Alfaro-Acha, A.; Rodríguez-Mañas, L.; García-García, F.J.; Ara, I. Reallocating accelerometer-assessed sedentary time to light or moderate-to vigorous-intensity physical activity reduces frailty levels in older adults: An isotemporal substitution approach in the TSHA study. J. Am. Med. Dir. Assoc. 2018, 19, 185.e1–185.e6. [Google Scholar] [CrossRef]
- Kim, K. Socio-ecological Meaning, Concern, and Improvement Plan Associated with Physical Activity in Older Population in Rural Area: A Mixed Method Inquiry. Korean J. Phys. Educ. 2015, 54, 41–57. [Google Scholar]
- Maxwell, J.A. Qualitative Research Design: An Interactive Approach; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2005. [Google Scholar]
- Zaki, N.; Alashwal, H.; Ibrahim, S. Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with COVID-19 disease severity and fatality: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1133–1142. [Google Scholar] [CrossRef] [PubMed]
- Patel, Y.; Joseph, J. Sodium intake and heart failure. Int. J. Mol. Sci. 2020, 21, 9474. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Rebholz, C.M.; Wong, E.; Chen, Y.; Matsushita, K.; Coresh, J.; Grams, M.E. Association between hypertension and kidney function decline: The Atherosclerosis Risk in Communities (ARIC) study. Am. J. Kidney Dis. 2019, 74, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Seretis, A.; Cividini, S.; Markozannes, G.; Tseretopoulou, X.; Lopez, D.S.; Ntzani, E.E.; Tsilidis, K.K. Association between blood pressure and risk of cancer development: A systematic review and meta-analysis of observational studies. Sci. Rep. 2019, 9, 8565. [Google Scholar] [CrossRef] [PubMed]
- Brandner, C.R.; May, A.K.; Clarkson, M.J.; Warmington, S.A. Reported side-effects and safety considerations for the use of blood flow restriction during exercise in practice and research. Tech. Orthop. 2018, 33, 114–121. [Google Scholar] [CrossRef]
- Tam, H.L.; Wong, E.M.L.; Cheung, K. Effectiveness of Educational Interventions on Adherence to Lifestyle Modifications Among Hypertensive Patients: An Integrative Review. Int. J. Environ. Res. Public Health 2020, 17, 2513. [Google Scholar] [CrossRef]
- Paczkowska, A.; Hoffmann, K.; Kus, K.; Kopciuch, D.; Zaprutko, T.; Ratajczak, P.; Michalak, M.; Nowakowska, E.; Bryl, W. Impact of patient knowledge on hypertension treatment adherence and efficacy: A single-centre study in Poland. Int. J. Med. Sci. 2021, 18, 852. [Google Scholar] [CrossRef]
- Oshagan, H. Reference group influence on opinion expression. Int. J. Public Opin. Res. 1996, 8, 335–354. [Google Scholar] [CrossRef]
- Shahin, W.; Kennedy, G.A.; Stupans, I. The association between social support and medication adherence in patients with hypertension: A systematic review. Pharm. Pract. 2021, 19, 2300. [Google Scholar] [CrossRef]
- Lobelo, F.; Young, D.R.; Sallis, R.; Garber, M.D.; Billinger, S.A.; Duperly, J.; Hutber, A.; Pate, A.R.P.; Thomas, R.J.; Widlansky, M.E.; et al. Routine assessment and promotion of physical activity in healthcare settings: A scientific statement from the American Heart Association. Circulation 2018, 137, e495–e522. [Google Scholar] [CrossRef]
- Jung, M.-H.; Ihm, S.-H. Improving the quality of hypertension management: Multifaceted approach. Korean Circ. J. 2019, 49, 528–531. [Google Scholar] [CrossRef]
- Won, S.; Kim, H. Social participation, health-related behavior, and depression of older adults living alone in Korea. Asian Soc. Work. Policy Rev. 2020, 14, 61–71. [Google Scholar] [CrossRef]
- Tarantino, E.; Crescenzo, P.; Campobasso, M.; D’alessandro, F.; Argiento, P.; Romeo, E.; Ghio, S.; Vitulo, P.; Parisi, F.; Mulè, M.; et al. Psychological counselling interventions to improve perceived quality of life and counter anxiety and depression in pulmonary-arterial-hypertension patients: A clinical trial. J. Health Soc. Sci. 2020, 5, 533–542. [Google Scholar]
- Xiao, M.; Zhang, F.; Xiao, N.; Bu, X.; Tang, X.; Long, Q. Health-related quality of life of hypertension patients: A population-based cross-sectional study in Chongqing, China. Int. J. Environ. Res. Public Health 2019, 16, 2348. [Google Scholar] [CrossRef]
- Rogers, E.M. Elements of diffusion. Diffus. Innov. 2003, 5, 1–38. [Google Scholar]
- Kim, K.-O. Exploring Pain, Life, and Meaning of Physical Activity Among Dementia Caregivers: A Photovoice Study. Korean J. Phys. Educ. 2017, 56, 11–30. [Google Scholar] [CrossRef]
- Ramirez-Jimenez, M.; Morales-Palomo, F.; Ortega, J.; Mora-Rodriguez, R. Effects of intense aerobic exercise and/or antihypertensive medication in individuals with metabolic syndrome. Scand. J. Med. Sci. Sport. 2018, 28, 2042–2051. [Google Scholar] [CrossRef]
- Cascino, T.M.; Cascino, T.M.; McLaughlin, V.V.; Richardson, C.R.; Behbahani-Nejad, N.; Moles, V.M.; Visovatti, S.H.; Jackson, E.A. Barriers to physical activity in patients with pulmonary hypertension. Pulm. Circ. 2019, 9, 2045894019847895. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).