Exploring the Black Box of an mHealth Intervention (LIFE4YOUth): A Qualitative Process and Outcome Evaluation of End-User Engagement
Abstract
:1. Introduction
2. Methods
2.1. Design
2.2. The LIFE4YOUth Intervention
2.3. Settings and Recruitment Process
2.4. Informants and Data Collection
2.5. Ethical Approval
2.6. Data Analysis
3. Results
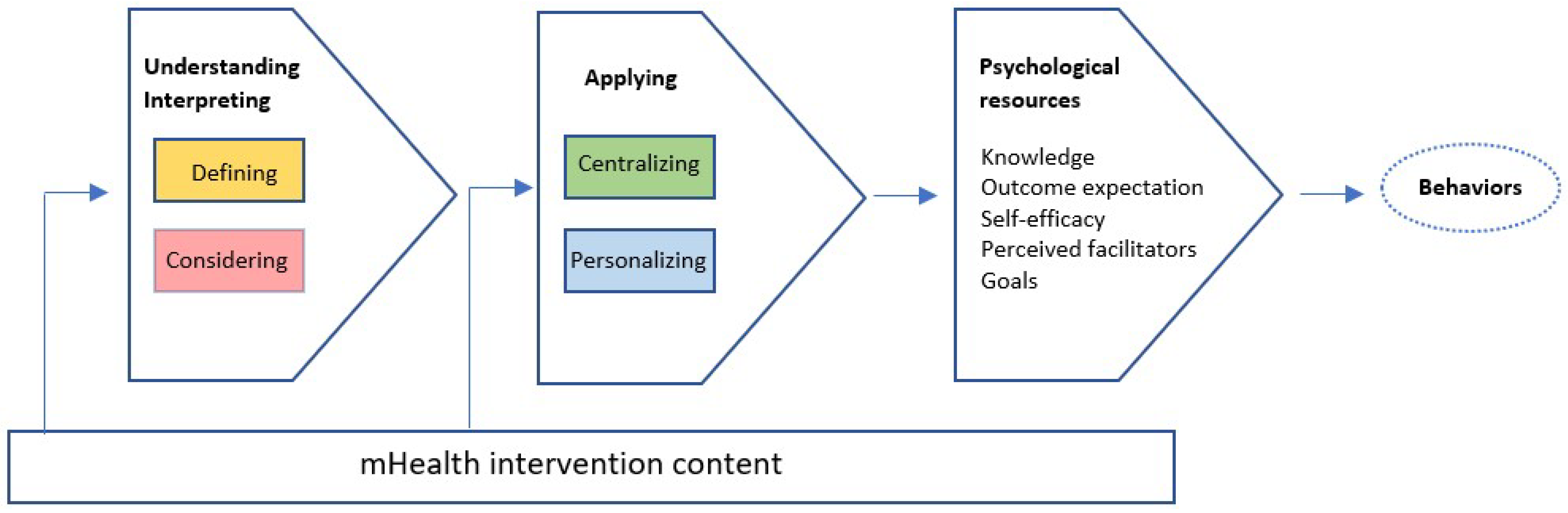
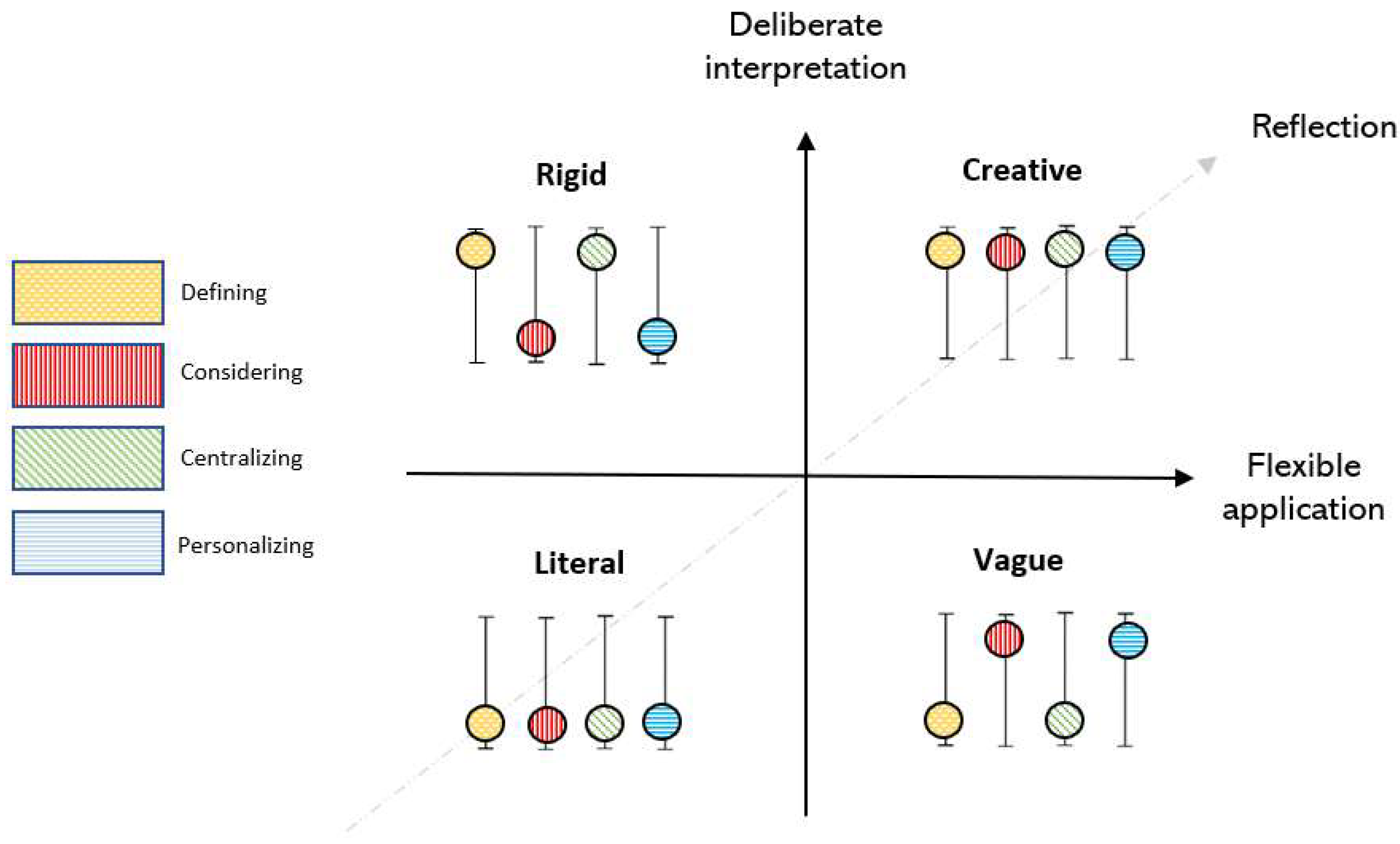
3.1. How the Intervention Was Understood, Interpreted, and Applied
3.1.1. Literal
3.1.2. Vague
3.1.3. Rigid
3.1.4. Creative
3.2. Interaction Outcomes Based on Social Cognitive Theory
3.2.1. Knowledge
3.2.2. Outcome Expectation
3.2.3. Self-Efficacy
3.2.4. Perceived Facilitators
3.2.5. Goals
4. Discussion
4.1. Result Discussion
4.1.1. Main Findings
4.1.2. Implications for Practice
4.1.3. Implications for Theory
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wiium, N.; Breivik, K.; Wold, B. Growth Trajectories of Health Behaviors from Adolescence through Young Adulthood. Int. J. Environ. Res. Public Health 2015, 12, 13711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lounassalo, I.; Hirvensalo, M.; Palomäki, S.; Salin, K.; Tolvanen, A.; Pahkala, K.; Rovio, S.; Fogelholm, M.; Yang, X.; Hutri-Kähönen, N.; et al. Life-course leisure-time physical activity trajectories in relation to health-related behaviors in adulthood: The Cardiovascular Risk in Young Finns study. BMC Public Health 2021, 21, 533. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frobel, W.; Grafe, N.; Meigen, C.; Vogel, M.; Hiemisch, A.; Kiess, W.; Poulain, T. Substance use in childhood and adolescence and its associations with quality of life and behavioral strengths and difficulties. BMC Public Health 2022, 22, 275. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Forouzanfar, M.H.; Daoud, F.; Mokdad, A.A.; El Bcheraoui, C.; Moradi-Lakeh, M.; Kyu, H.H.; Barber, R.M.; Wagner, J.; Cercy, K.; et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2016, 387, 2383–2401. [Google Scholar] [CrossRef]
- Catalano, R.F.; Fagan, A.A.; Gavin, L.E.; Greenberg, M.T.; Irwin, C.E.; Ross, D.A.; Shek, D. Worldwide application of prevention science in adolescent health. Lancet 2012, 379, 1653–1664. [Google Scholar] [CrossRef] [Green Version]
- Arigo, D.; Jake-Schoffman, D.E.; Wolin, K.; Beckjord, E.; Hekler, E.B.; Pagoto, S.L. The history and future of digital health in the field of behavioral medicine. J. Behav. Med. 2019, 42, 67–83. [Google Scholar] [CrossRef]
- Fiordelli, M.; Diviani, N.; Schulz, P.J. Mapping mHealth Research: A Decade of Evolution. J. Med. Internet Res. 2013, 15, e95. [Google Scholar] [CrossRef]
- Davis, T.L.; DiClemente, R.; Prietula, M. Taking mHealth Forward: Examining the Core Characteristics. JMIR mHealth uHealth 2016, 4, e97. [Google Scholar] [CrossRef]
- Gilbey, D.; Morgan, H.; Lin, A.; Perry, Y. Effectiveness, Acceptability, and Feasibility of Digital Health Interventions for LGBTIQ+ Young People: Systematic Review. J. Med. Internet Res. 2020, 22, e20158. [Google Scholar] [CrossRef]
- Lopez-Rodriguez, M.M.; Fernández-Millan, A.; Ruiz-Fernández, M.D.; Dobarrio-Sanz, I.; Fernández-Medina, I.M. New Technologies to Improve Pain, Anxiety and Depression in Children and Adolescents with Cancer: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 3563. [Google Scholar] [CrossRef] [PubMed]
- McMullan, M.; Millar, R.; Woodside, J.V. A systematic review to assess the effectiveness of technology-based interventions to address obesity in children. BMC Pediatr. 2020, 20, 242. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Wu, H.; Yu, F.; Fu, J.; Sun, S.; Huang, T.; Wang, R.; Chen, D.; Zhao, G.; Quan, M. Effects of Smartphone-Based Interventions on Physical Activity in Children and Adolescents: Systematic Review and Meta-analysis. JMIR mHealth uHealth 2021, 9, e22601. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, D.M.; Li, S.; Levine, M.J.; Auten, B.; Granson, M. Systematic Review of Smartphone Apps as a mHealth Intervention to Address Substance Abuse in Adolescents and Adults. J. Addict. Nurs. 2021, 32, 180–187. [Google Scholar] [CrossRef]
- Staiger, P.K.; O’Donnell, R.; Liknaitzky, P.; Bush, R.; Milward, J. Mobile Apps to Reduce Tobacco, Alcohol, and Illicit Drug Use: Systematic Review of the First Decade. J. Med. Internet Res. 2020, 22, e17156. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Kim, S.K.; Lee, M. Mobile phone interventions to improve adolescents’ physical health: A systematic review and meta-analysis. Public Health Nurs. 2019, 36, 787–799. [Google Scholar] [CrossRef]
- Ludwig, K.; Arthur, R.; Sculthorpe, N.; Fountain, H.; Buchan, D.S. Text Messaging Interventions for Improvement in Physical Activity and Sedentary Behavior in Youth: Systematic Review. JMIR mHealth uHealth 2018, 6, e10799. [Google Scholar] [CrossRef]
- Hagger, M.S.; Moyers, S.; McAnally, K.; McKinley, L.E. Known knowns and known unknowns on behavior change interventions and mechanisms of action. Health Psychol. Rev. 2020, 14, 199–212. [Google Scholar] [CrossRef] [Green Version]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef] [Green Version]
- Danaher, B.G.; Brendryen, H.; Seeley, J.R.; Tyler, M.S.; Woolley, T. From black box to toolbox: Outlining device functionality, engagement activities, and the pervasive information architecture of mHealth interventions. Internet Interv. 2015, 2, 91–101. [Google Scholar] [CrossRef]
- O’Brien, H.L.; Roll, I.; Kampen, A.; Davoudi, N. Rethinking (Dis)engagement in human-computer interaction. Comput. Hum. Behav. 2021, 128, 107109. [Google Scholar] [CrossRef]
- Rixon, L.; Baron, J.; McGale, N.; Lorencatto, F.; Francis, J.; Davies, A. Methods used to address fidelity of receipt in health intervention research: A citation analysis and systematic review. BMC Health Serv. Res. 2016, 16, 663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borrelli, B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J. Public Health Dent. 2011, 71, S52–S63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müssener, U. Digital encounters: Human interactions in mHealth behavior change interventions. Digit. Health 2021, 7, 20552076211029776. [Google Scholar] [CrossRef]
- Toomey, E.; Hardeman, W.; Hankonen, N.; Byrne, M.; McSharry, J.; Matvienko-Sikar, K.; Lorencatto, F. Focusing on fidelity: Narrative review and recommendations for improving intervention fidelity within trials of health behaviour change interventions. Health Psychol. Behav. Med. 2020, 8, 132–151. [Google Scholar] [CrossRef] [Green Version]
- Lewin, S.; Glenton, C.; Oxman, A.D. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: Methodological study. BMJ 2009, 339, b3496. [Google Scholar] [CrossRef] [Green Version]
- Bradway, M.; Leibowitz, K.; Garrison, K.A.; Howe, L.; Årsand, E. Qualitative Evaluations of mHealth Interventions: Current Gaps and Future Directions. Stud. Health Technol. Inform. 2020, 270, 1041–1045. [Google Scholar] [CrossRef]
- Cheng, K.K.F.; Metcalfe, A. Qualitative Methods and Process Evaluation in Clinical Trials Context. Int. J. Qual. Methods 2018, 17, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Begum, S.; Yada, A.; Lorencatto, F. How Has Intervention Fidelity Been Assessed in Smoking Cessation Interventions? A Systematic Review. J. Smok. Cessat. 2021, 2021, 6641208. [Google Scholar] [CrossRef]
- Bendtsen, M.; Seiterö, A.; Bendtsen, P.; Henriksson, H.; Henriksson, P.; Thomas, K.; Löf, M.; Müssener, U. mHealth intervention for multiple lifestyle behaviour change among high school students in Sweden (LIFE4YOUth): Protocol for a randomised controlled trial. BMC Public Health 2021, 21, 1406. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative Research and Evaluation Methods—Integrating Theory and Practice, 4th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- Müssener, U.; Löf, M.; Bendtsen, P.; Bendtsen, M. Using Mobile Devices to Deliver Lifestyle Interventions Targeting At-Risk High School Students: Protocol for a Participatory Design Study. JMIR Res. Protoc. 2020, 9, e14588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müssener, U.; Thomas, K.; Linderoth, C.; Löf, M.; Åsberg, K.; Henriksson, P.; Bendtsen, M. Development of an Intervention Targeting Multiple Health Behaviors Among High School Students: Participatory Design Study Using Heuristic Evaluation and Usability Testing. JMIR mHealth uHealth 2020, 8, e17999. [Google Scholar] [CrossRef] [PubMed]
- Seiterö, A.; Thomas, K.; Löf, M.; Müssener, U. Using Mobile Phones in Health Behaviour Change—An Exploration of Perceptions among Adolescents in Sweden. Int. J. Adolesc. Youth 2021, 26, 294–306. [Google Scholar] [CrossRef]
- Eccles, D.W.; Arsal, G. The think aloud method: What is it and how do I use it? Qual. Res. Sport Exerc. Health 2017, 9, 514–531. [Google Scholar] [CrossRef]
- Bandura, A. Health Promotion by Social Cognitive Means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Mazur, J.; Szkultecka-Dębek, M.; Dzielska, A.; Drozd, M.; Małkowska-Szkutnik, A. What does the Cantril Ladder measure in adolescence? Arch. Med. Sci. 2018, 1, 182–189. [Google Scholar] [CrossRef]
- Greenhalgh, T. How to Implement Evidence-Based Healthcare; Wiley Blackwell: Oxford, UK, 2018; pp. 35–36. [Google Scholar]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [Green Version]
- Perski, O.; Blandford, A.; West, R.; Michie, S. Conceptualising engagement with digital behaviour change interventions: A systematic review using principles from critical interpretive synthesis. Transl. Behav. Med. 2016, 7, 254–267. [Google Scholar] [CrossRef]
- Bell, L.; Garnett, C.; Qian, T.; Perski, O.; Williamson, E.; Potts, H.W. Engagement With a Behavior Change App for Alcohol Reduction: Data Visualization for Longitudinal Observational Study. J. Med. Internet Res. 2020, 22, e23369. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.; Díaz, Ó. Using Health Chatbots for Behavior Change: A Mapping Study. J. Med. Syst. 2019, 43, 135. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.P.; Lester, J.C. Artificial Intelligence for Personalized Preventive Adolescent Healthcare. J. Adolesc. Health 2020, 67, S52–S58. [Google Scholar] [CrossRef] [PubMed]
- Bellg, A.J.; Borrelli, B.; Resnick, B.; Hecht, J.; Minicucci, D.S.; Ory, M.G.; Ogedegbe, G.; Orwig, D.; Ernst, D.; Czajkowski, S. Enhancing Treatment Fidelity in Health Behavior Change Studies: Best Practices and Recommendations From the NIH Behavior Change Consortium. Health Psychol. 2004, 23, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Bruce, C.; Harrison, P.; Giammattei, C.; Desai, S.-N.; Sol, J.R.; Jones, S.; Schwartz, R. Evaluating Patient-Centered Mobile Health Technologies: Definitions, Methodologies, and Outcomes. JMIR mHealth uHealth 2020, 8, e17577. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and Promoting Effective Engagement With Digital Behavior Change Interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef] [Green Version]
- Short, C.E.; Desmet, A.; Woods, C.; Williams, S.L.; Maher, C.; Middelweerd, A.; Müller, A.M.; Wark, P.A.; Vandelanotte, C.; Poppe, L.; et al. Measuring Engagement in eHealth and mHealth Behavior Change Interventions: Viewpoint of Methodologies. J. Med. Internet Res. 2018, 20, e292. [Google Scholar] [CrossRef]
- Davis, S.R.; Peters, D.; Calvo, R.A.; Sawyer, S.M.; Foster, J.M.; Smith, L. “Kiss myAsthma”: Using a participatory design approach to develop a self-management app with young people with asthma. J. Asthma 2017, 55, 1018–1027. [Google Scholar] [CrossRef]
- Fleming, J.B.; Hill, Y.N.; Burns, M.N.; Lucassen, M.; Wahle, F.; Shepherd, M. Usability of a Culturally Informed mHealth Intervention for Symptoms of Anxiety and Depression: Feedback From Young Sexual Minority Men. JMIR Hum. Factors 2017, 4, e22. [Google Scholar] [CrossRef] [Green Version]
- Newton, A.; Bagnell, A.; Rosychuk, R.; Duguay, J.; Wozney, L.; Huguet, A.; Henderson, J.; Curran, J. A Mobile Phone-Based App for Use During Cognitive Behavioral Therapy for Adolescents With Anxiety (MindClimb): User-Centered Design and Usability Study. JMIR mHealth uHealth 2020, 8, e18439. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef] [PubMed]
| Intervention Components | Design Characteristics | BCT 1 | Physical Activity | Diet | Alcohol | Smoking |
|---|---|---|---|---|---|---|
| Weekly screening tool to prompt recording of health behaviors | Examples, predefined choices | Self-monitoring of behavior | x | x | x | x |
| Feedback on performance on behaviors | Colored feedback (green, yellow, red) | Feedback on behavior | x | x | x | x |
| Information to increase awareness of consequences of health behaviors | Text and pictures | Information about health consequences | x | x | x | x |
| Template to highlight consequences of behaviors | Predefined choices, examples, textual feedback | Information about social and environmental consequences | x | x | x | |
| Prompting and identifying motives for health behavior change | Predefined choices | Incompatible beliefs | x | x | x | x |
| Practical tips to increase confidence in behavior change | Text | Instruction on how to perform a behavior | x | x | x | x |
| Instructions to define goals | Checklist, examples, free text boxes | Goal setting (behavior) | x | x | ||
| Template to reflect on obstacles to behavior change | Examples, predefined choices, free text boxes | Problem solving Action planning | x | x | x | x |
| Variable | n (n = 16) |
|---|---|
| Sex | |
| Female | 9 |
| Male | 7 |
| Age, mean (range) | 17.5 (16–19) |
| Educational profile | |
| Theoretical | 12 |
| Vocational | 4 |
| Satisfaction with life 1 (0–10) | |
| 7–10 | 13 |
| 4–6 | 3 |
| 0–3 | 0 |
| Prior experiences of using mHealth | |
| None | 0 |
| Little | 14 |
| Considerable | 2 |
| Prior experiences of attempts to improve | |
| Physical activity | 13 |
| Food habits | 12 |
| Smoking cigarettes | 0 |
| Alcohol consumption | 1 |
| None | 1 |
| Health education in school | |
| Recently | 10 |
| Not recently | 6 |
| LIFE4YOUth health behavior module engagement | |
| Physical activity | 4 |
| Food habits | 9 |
| Alcohol consumption | 3 |
| Smoking cigarettes | 0 |
| Theme | Categories | Example of High and Low Degree |
|---|---|---|
| Deliberate | Defining | “Well, let’s see, last week…yeah, I don’t know, maybe… I mean, I guess that we talk about alcohol here, right? Not just water and things like that.” (illustrates reflection about core concepts (standard units)) “Then it was…When thinking about soda, it was four, otherwise I only drink water.” (responded to a question in the weekly screening without realizing that the question referred to alcohol) |
| Considering | “I usually don’t eat as much fruits as I did before, but I usually drink a lot of smoothies, though.” (How many 100 g portions (Equivalent to an average sized banana or one large apple) of fruit did you consume last week?) “I ate two bananas yesterday, so… I seldom eat apples.” | |
| Flexible | Centralizing | “… I’m not sure about what’s considered a [Swedish fika]. Well, I am thinking about sweet stuff. But I use to buy sandwiches and so on in the café because I usually work out and must energize myself.” “I’m choosing one because…well, one can per week, that sounds normal.” |
| Personalizing | “Yeah, which habit do I want to change? To sleep better, I mean, to get more sleep. It doesn’t have to be something related to exercise, right? It can be like sleep too?” “I…. right now, I’ve always eaten breakfast every day because I think it’s very important. […]. So, I maybe don’t have to put a goal on that, […] but maybe I should eat a bit more then, that could be a specific goal” (after reading about goal definition based on an example about having breakfast) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seiterö, A.; Thomas, K.; Löf, M.; Müssener, U. Exploring the Black Box of an mHealth Intervention (LIFE4YOUth): A Qualitative Process and Outcome Evaluation of End-User Engagement. Int. J. Environ. Res. Public Health 2022, 19, 14022. https://doi.org/10.3390/ijerph192114022
Seiterö A, Thomas K, Löf M, Müssener U. Exploring the Black Box of an mHealth Intervention (LIFE4YOUth): A Qualitative Process and Outcome Evaluation of End-User Engagement. International Journal of Environmental Research and Public Health. 2022; 19(21):14022. https://doi.org/10.3390/ijerph192114022
Chicago/Turabian StyleSeiterö, Anna, Kristin Thomas, Marie Löf, and Ulrika Müssener. 2022. "Exploring the Black Box of an mHealth Intervention (LIFE4YOUth): A Qualitative Process and Outcome Evaluation of End-User Engagement" International Journal of Environmental Research and Public Health 19, no. 21: 14022. https://doi.org/10.3390/ijerph192114022
APA StyleSeiterö, A., Thomas, K., Löf, M., & Müssener, U. (2022). Exploring the Black Box of an mHealth Intervention (LIFE4YOUth): A Qualitative Process and Outcome Evaluation of End-User Engagement. International Journal of Environmental Research and Public Health, 19(21), 14022. https://doi.org/10.3390/ijerph192114022






