Abstract
Regular follow-up attendance in primary care and routine blood glucose monitoring are essential in diabetes management, particularly for patients at higher cardiovascular (CV) risk. We sought to examine the regularity of follow-up attendance and blood glucose monitoring in a primary care sample of type 2 diabetic patients at moderate-to-high CV risk, and to explore factors associated with poor engagement. Cross-sectional data were collected from 2130 patients enrolled in a diabetic retinopathy screening programme in Guangdong province, China. Approximately one-third of patients (35.9%) attended clinical follow-up <4 times in the past year. Over half of patients (56.9%) failed to have blood glucose monitored at least once per month. Multivariable logistic regression analysis showed that rural residents (adjusted odds ratio [aOR] = 0.420, 95% confidence interval [CI] = 0.338–0.522, p < 0.001, for follow-up attendance; aOR = 0.580, 95%CI: 0.472–0.712, p < 0.001, for blood glucose monitoring) and subjects with poor awareness of adverse consequences of diabetes complications (aOR = 0.648, 95%CI = 0.527–0.796, p < 0.001, for follow-up attendance; aOR = 0.770, 95%CI = 0.633–0.937, p = 0.009, for blood glucose monitoring) were both less likely to achieve active engagement. Our results revealed an urban–rural divide in patients’ engagement in follow-up attendance and blood glucose monitoring, which suggested the need for different educational approaches tailored to the local context to enhance diabetes care.
1. Introduction
Prevention and control of diabetes and its complications represents a formidable public health challenge worldwide. Current estimates suggest that nearly 130 million people are living with diabetes in China, which accounts for 12.8% of the Chinese adult population [1]. As an independent risk factor for cardiovascular disease (CVD), type 2 diabetes mellitus (T2DM) often coexists with other CV risk factors, such as hypertension, obesity, and dyslipidaemia [2]. Diabetes not only harms patients’ physical well-being but also causes serious complications, which has imposed a considerable economic burden in China [3].
The pathogenesis and progressive nature of diabetes requires patients’ inputs to continuous care, regular monitoring of blood glucose, and adherence to tailored medications to control hyperglycaemia. It is therefore particularly important to ensure the routine delivery of effective and affordable healthcare services to diabetic patients. According to the Chinese national standards for delivering basic public service (third edition), people diagnosed with T2DM are provided with regular follow-up care and fasting plasma glucose monitoring on a free-of-charge basis at primary care facilities [4]. Patients are also encouraged to actively engage in diabetes education and annual check-ups.
Regular follow-up care and routine blood glucose monitoring are essential in diabetes management. The results of blood glucose monitoring are important information for physicians to provide appropriate treatment regimens with tailored lifestyle advice to achieve glycaemic control and prevent disease progression [5,6,7]. A large body of evidence has accumulated over the years documenting that regular follow-up care [8,9] and structured monitoring of blood glucose [10,11] could significantly prevent the deterioration in glycaemic status. However, previous investigations showed that more than two-fifth of patients with T2DM failed to achieve follow-up attendance at least once per quarter at community health centres [12], and that only less than one-fifth of T2DM patients were able to perform blood glucose monitoring on a regular basis [13].
Existing studies reported barriers to follow-up attendance at primary care facilities among Chinese T2DM patients. A cross-sectional study conducted in eastern China found that determinants of infrequent follow-up visits included lower household income, absence of health insurance, and lack of telephone communication and community outreach services [12]. A multi-site survey conducted earlier by our team demonstrated that higher education level of physicians, increased volume of daily patients seen, and no provision of home visits acted as risk factors for non-attainment of the target frequency of follow-up care for T2DM [14]. Patient-level factors associated with poor monitoring of blood glucose were also reported elsewhere [13,15,16].
However, there is limited evidence from studies conducted among T2DM patients at moderate to high CV risk, who account for a large proportion of diabetic patients seen in primary care practice and are more likely to experience major adverse outcomes. We therefore sought to examine the regularity of follow-up attendance and blood glucose monitoring in a primary care sample of T2DM patients at moderate to high CV risk, and to explore factors associated with patients’ poor engagement in routine diabetes care.
2. Materials and Methods
2.1. Study Design
This was a cross-sectional study conducted in an urban–rural fringe in Guangdong province, southern China. The study was part of a larger project on the screening for diabetic retinopathy (DR) in collaboration with the Zhongshan Ophthalmic Center, Sun Yat-Sen University. The screening cohort was originally designed to evaluate the prevalence, incidence, and progression rate of DR in T2DM patients. Diabetic patients enrolled in family doctor teams for routine diabetes management at local primary care facilities were invited for ophthalmoscopic exams. A semi-structured questionnaire was used to collect information on follow-up attendance and blood glucose monitoring among diabetic patients in the 2019 wave of DR screening.
2.2. Setting and Data Source
Data were collected at community and township health centres in the primary care settings. All subjects were interviewed face-to-face by trained clinical staff during on-site examination for DR screening. All completed questionnaires were scrutinised by a senior supervisor on a daily basis as a quality control measure. Information were gathered using a semi-structured questionnaire which included: (1) the patient’s basic information, including age, gender, place of residence, education level, marital status, and living relationships; (2) routine lifestyle behaviours, including smoking and drinking status; (2) disease-related information, including duration of diabetes, use of glucose-lowering medications, presence of comorbidity, as well as awareness of adverse consequences of diabetes complications; (4) health services utilisation, including follow-up attendance and blood glucose monitoring; and (5) the patient’s self-rated health scores.
2.3. Participants
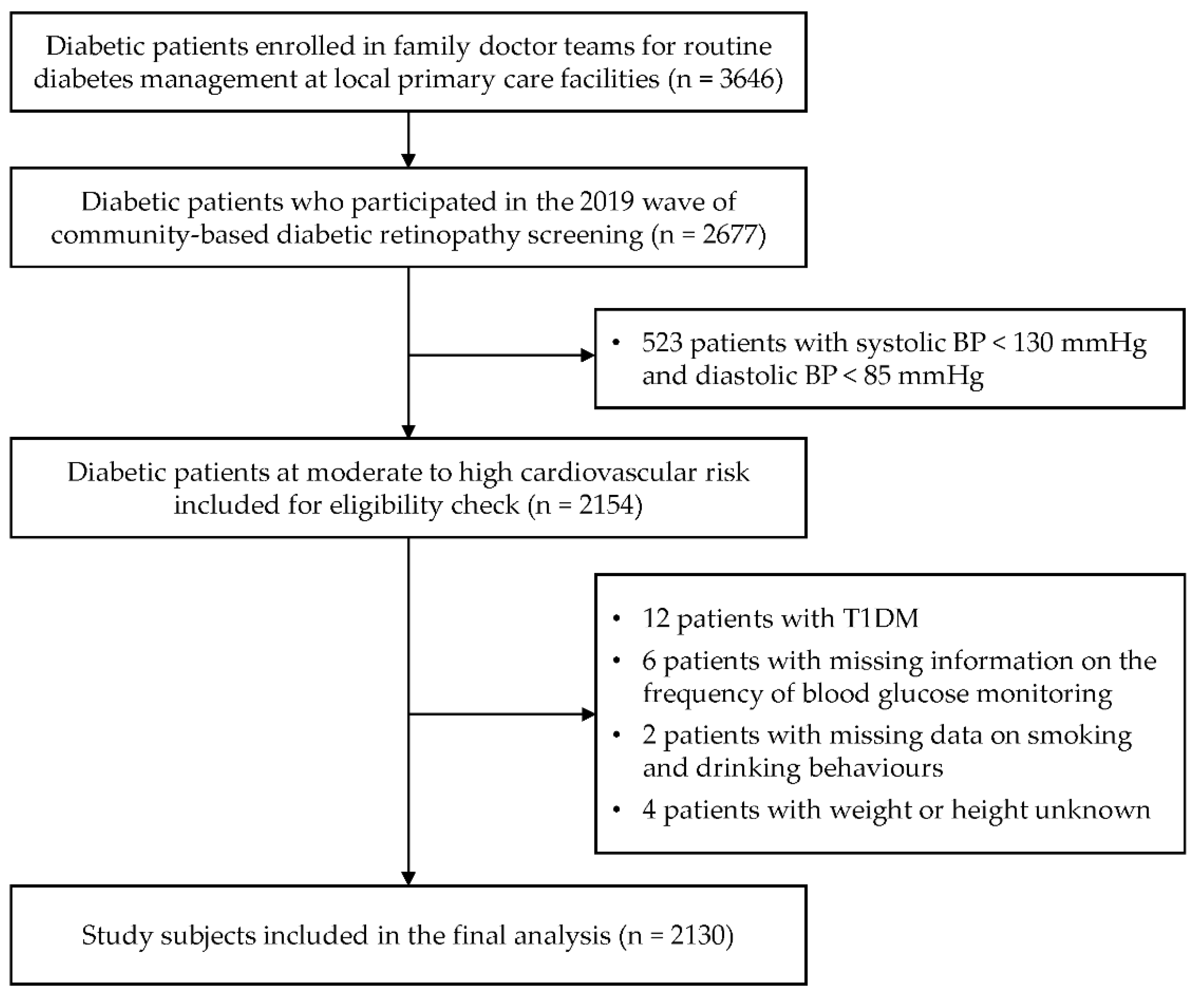
Study subjects were drawn from one community health centre and nine township health centres in an urban–rural fringe. Patients with T2DM at moderate to high (including very high) CV risk who participated in the 2019 wave of DR screening were included in the present study. Diabetes was diagnosed as having a fasting plasma glucose level ≥ 7.0 mmol/L or glycated haemoglobin (HbA1c) ≥ 6.5% [17]. The presence of diabetes was determined by the attending physician. The target subjects were T2DM patients who had systolic BP ≥ 130 mmHg or diastolic BP ≥ 85 mmHg in accordance with the clinical guideline [18]. The study flowchart was shown in Figure 1.
Figure 1.
Flow chart of the study. T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; BP, blood pressure.
2.4. Study Variables and Measurements
Weight and height were measured by trained medical staff according to a standardised protocol. Body weight was measured with light clothing. Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters (kg/m2). Blood pressure (BP) was measured in a seated position by routinely validated automatic sphygmomanometers. The arm with the higher BP values was obtained following the standard clinical operating procedure.
The dependent variables were the frequency of patients’ follow-up attendance at primary care facilities and blood glucose monitoring. Patients were asked “How many times did you visit the physician at the community or township health centre in 2018?” to collect information about follow-up attendance in the past year. The frequency of follow-up attendance was divided into <4 and ≥4 times per year, according to Chinese national standards (3rd edition) for delivering basic public health services [4]. Answers to the question “How often did you monitor your blood glucose?” were classified into five categories, i.e., never, only when not feeling well, 1–2 times a quarter, 1–2 times a month, and at least 1–2 times a week. We further divided the frequency into once or more per month vs. less than once per month [15], in the binary logistic regression analysis.
Independent variables included demographics, such as age (<65 or ≥65 years), gender (male or female), place of residence (urban or rural), marital status (married or others, with others including single, divorced, and widowed), living relationships (living alone or others), education level (no formal education or primary school and higher); routine lifestyle behaviours including smoking status (current smoking or others, with others including never smoking and past smoking) and regular drinking (regular drinking or others, with others including never drinking and past drinking); and disease-related variables including duration of diabetes (<10 or ≥10 years), use of glucose-lowing medications (yes or no), the presence of comorbidity (yes or no). Healthcare-related variables included venues for blood glucose testing (only at primary care facilities or others; primary care facilities referred to community health centres or township health centres, and other venues referred to home, pharmacy, village clinics, or secondary/tertiary-level hospitals), self-rated health scores (<3 or ≥3 in a range of 1 to 5 where higher scores representing better self-reported health status), overweight or obese (defined as BMI ≥ 24 kg/m2 [19]) and poor awareness of adverse consequences of diabetes complications (i.e., a negative answer to the question “do you know any of the adverse consequences of diabetes complications?”).
2.5. Statistical Analysis
Double-entry verification was performed in EpiData 3.1 (Odense, Denmark). Descriptive statistics were used to describe subject characteristics, frequency of follow-up attendance and the regularity of blood glucose monitoring. Independent t-tests or chi-square tests, where appropriate, were used to compare the characteristics of urban vs. rural patients. Univariate logistic regression analysis was performed to explore the relationship between each independent variable and frequency of follow-up attendance and blood glucose monitoring, respectively. Variables that were significant were further entered into the multivariable binary logistic regression model. Data analysis was conducted using IBM SPSS Statistics 26. A p-value less than 0.05 was considered statistically significant.
2.6. Ethics Consideration
All participants provided written informed consent. Data anonymisation was carried out by removing all patient identifiers from the dataset before data analysis. Ethics approval was granted by ethics committees at Zhongshan Ophthalmic Center, Sun Yat-Sen University (Ref: 2017KYPJ094) in accordance with the Declaration of Helsinki 2013.
3. Results
3.1. Characteristics of Study Participants
The study enrolled a total of 2130 eligible patients, of which, 885 were from urban areas and 1245 were from rural areas. Over half of patients were under 65 years of age (51.5%) and were female (55.6%). Less than one-fifth (16.2%) of participants had no formal education. The prevalence of active smoking (17.7%) and regular drinking (12.6%) was low. More than half of participants were overweight or obese. A substantial proportion of patients were diagnosed with diabetes within the past 10 years (78.7%), reported the presence of comorbidity (81.1%), and received glucose-lowering medications (82.3%). More than half (58.8%) of patients had poor awareness of adverse consequences of diabetes complications. We found that 37.9% of patients had their blood glucose tested only at primary care facilities. When compared to urban patients, rural subjects were younger, had less formal education with a higher prevalence of active smoking and regular drinking, had higher self-rated health scores, and had shorter duration of diagnosed disease with a poor awareness of adverse consequences of diabetes complications, but were as likely as urban patients to develop diabetes comorbidity (Table 1).

Table 1.
Characteristics of study participants.
3.2. Frequency of Follow-Up Attendance and Blood Glucose Monitoring
Of 2130 participants in total, 64.1% attended clinical follow-up at the community health centres or township health centres at least four times in the past year, while slightly more than one-third of patients did not achieve the target frequency of follow-up attendance for T2DM. With respect to the frequency of blood glucose monitoring, 13.6% of patients tested their blood glucose at least 1 to 2 times a week, and 51.3% of patients tested 1 to 2 times a quarter. We found a small proportion of patients who tested their blood glucose only when not feeling well and patients who did not have blood glucose tested in the past year. Overall, nearly half (43.1%) of patients were able to have their blood glucose tested once or more per month (Table 2).

Table 2.
Frequency of follow-up attendance and blood glucose monitoring among T2DM patients at moderate to high CV risk.
3.3. Factors Associated with the Frequency of Follow-Up Attendance
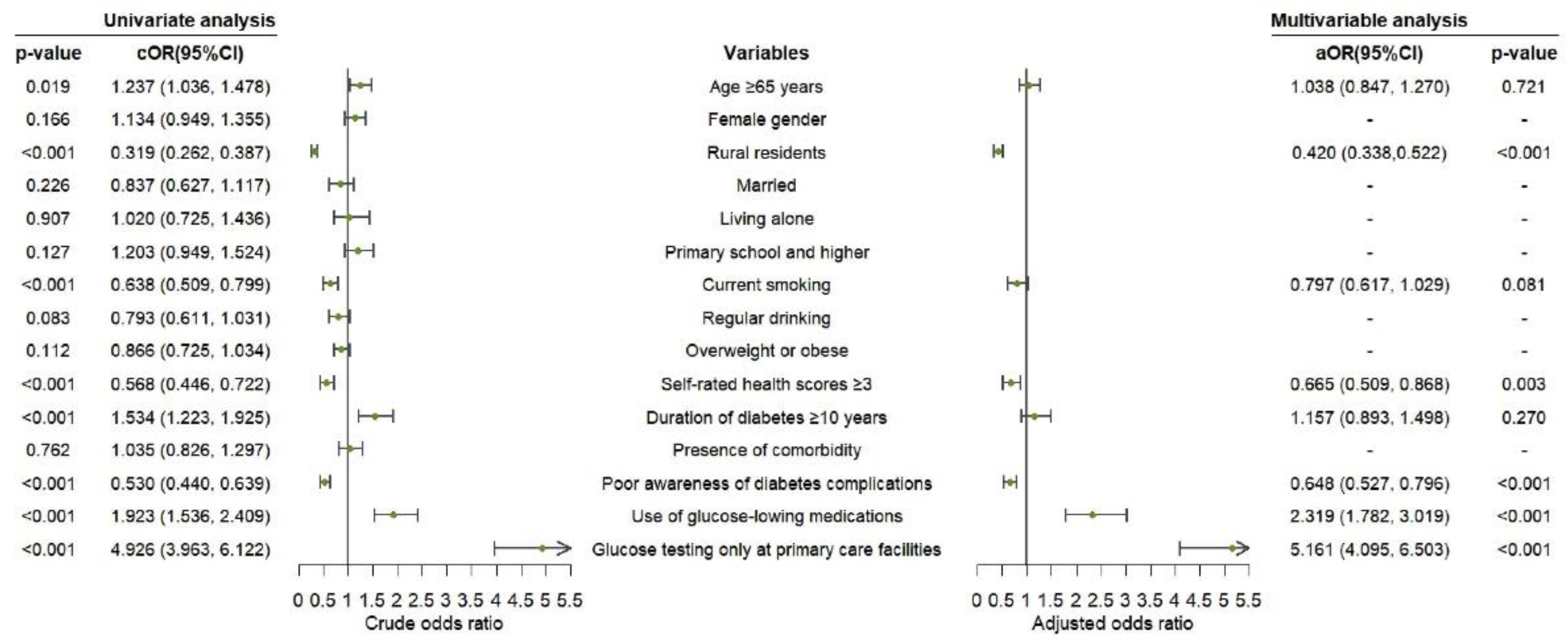
In the univariate analysis, age, place of residence, smoking status, self-rated health scores, duration of diabetes, awareness of adverse consequences of diabetes complications, use of glucose-lowering medications, and venues for testing blood glucose were associated with the frequency of follow-up attendance (p < 0.05), which were further entered in the multivariable analysis. In the further analysis, patients who received glucose-lowering medications (aOR = 2.319, 95%CI: 1.782–3.019; p < 0.001) or had blood glucose tested only at primary care facilities (aOR = 5.161, 95%CI: 4.095–6.503; p < 0.001) were more prone to have a higher regularity of follow-up attendance compared to their counterparts. However, patients who lived in rural areas (aOR = 0.420, 95%CI: 0.338–0.522; p < 0.001), had poor awareness of adverse consequences of diabetes complications (aOR = 0.648, 95%CI: 0.527–0.796; p < 0.001) with self-rated health scores ≥3 (aOR = 0.665, 95%CI: 0.509–0.868; p = 0.003) were less likely to attend clinical follow-up at least 4 times in the past year (Figure 2).
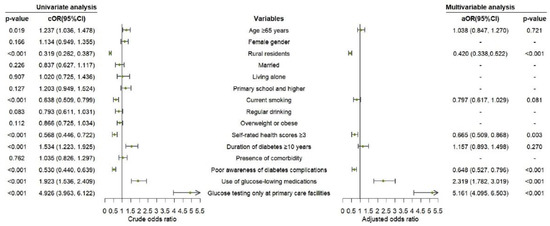
Figure 2.
Logistic regression analysis on factors associated with regular follow-up attendance among T2DM patients at moderate to high CV risk.
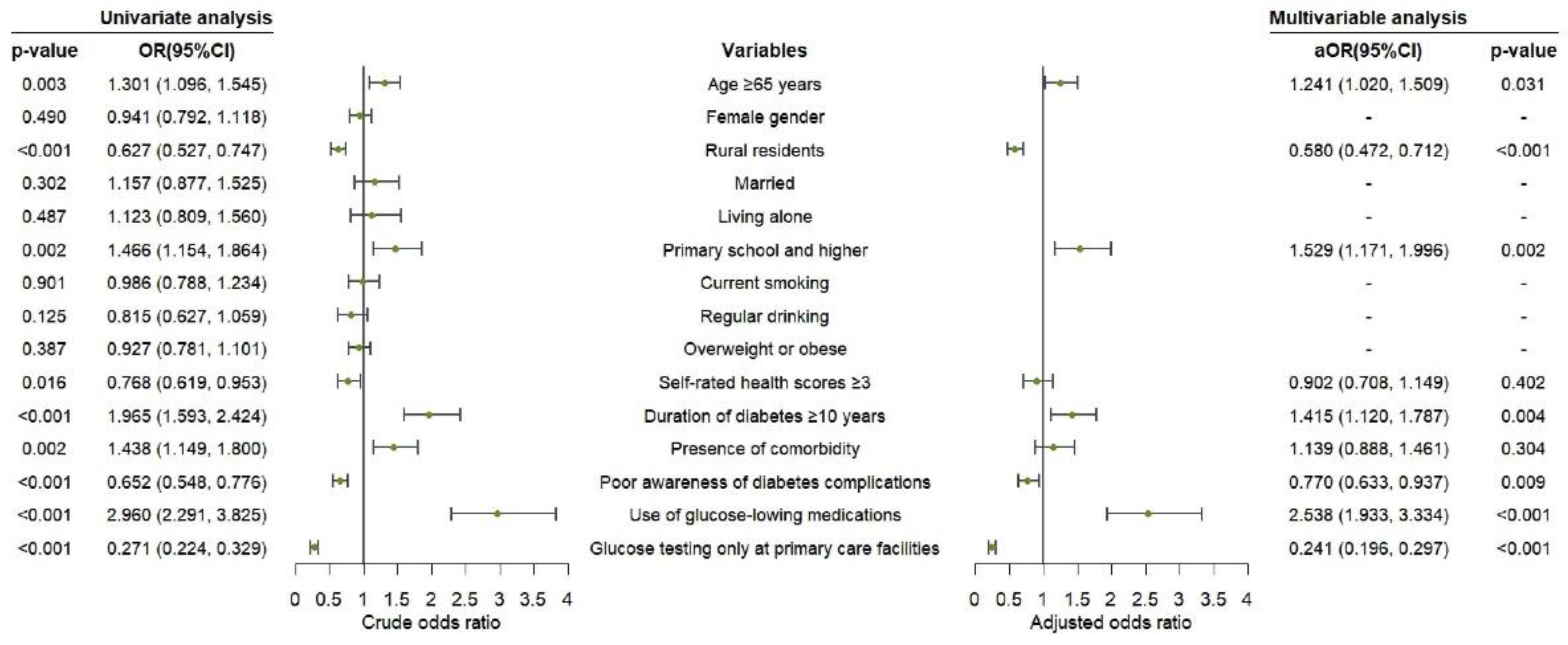
3.4. Factors Associated with the Frequency of Blood Glucose Monitoring
In the univariate analysis, age, place of residence, education level, self-rated health scores, duration of diabetes, presence of comorbidity, awareness of adverse consequences of diabetes complications, use of glucose-lowering medications, and venues for testing blood glucose were associated with the frequency of blood glucose monitoring (p <0.05), which were further entered in the multivariable analysis. In the further analysis, the following factors remained significantly associated with having blood glucose monitored once or more per month: age ≥ 65 years (aOR = 1.241, 95%CI: 1.020–1.509; p = 0.031), living in rural areas (aOR = 0.580, 95%CI: 0.472–0.712; p < 0.001), having formal education (aOR = 1.529, 95%CI: 1.171–1.996; p = 0.002), having a diagnosis of diabetes for over 10 years (aOR = 1.415, 95%CI: 1.120–1.787; p = 0.004), poor awareness of adverse consequences of diabetes complications (aOR = 0.770, 95%CI: 0.633–0.937; p = 0.009), use of glucose-lowering medications (aOR = 2.538, 95%CI: 1.933–3.334; p < 0.001), and having blood glucose tested only at primary care facilities (aOR = 0.241, 95%CI: 0.196–0.297; p < 0.001) (Figure 3).
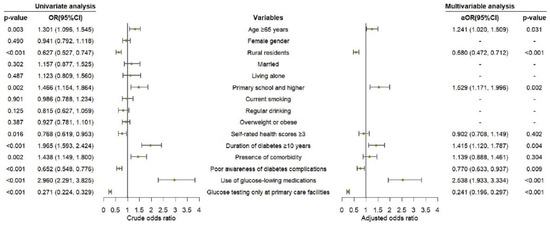
Figure 3.
Logistic regression analysis on factors associated with regular blood glucose monitoring among T2DM patients at moderate to high CV risk.
4. Discussion
4.1. Main Findings
We found that approximately one-third of patients (35.9%) attended clinical follow-up <4 times in the past year, and that slightly over half of patients (56.9%) failed to monitor their blood glucose at least once per month. Multivariable logistic regression analysis showed that place of residence, awareness of consequences of diabetes complications, use of glucose-lowering medications, and venue for testing blood glucose were factors associated with the regularity of both follow-up attendance and blood glucose monitoring. Moreover, current smoking and having better self-rated health status were negatively associated with the attainment of the recommended frequency target for follow-up visits at primary care facilities. Patients aged 65 years or older, having an education level of primary school and above, or having a diagnosed diabetes for over 10 years were more likely to have their blood glucose monitored once and above per month. Our results exhibited an urban–rural divide in patients’ engagement in follow-up attendance and blood glucose monitoring.
4.2. Relationship with Other Studies
In China, the management of T2DM has been integrated as part of the national basic public health service delivery [20]. Follow-up care is recommended to be provided to patients with T2DM on a quarterly basis according to the Chinese national standards (third edition) for delivering basic public health service [4]. In the present study, we found that up to two-thirds (64.1%) of T2DM patients at moderate to high CV risk attended clinical follow-up at least four times per year. The proportion was consistent with results from another cross-sectional survey conducted in western China [21], but was lower than that reported in a longitudinal study in Luxembourg, Belgium [22], where 90% of T2DM patients consulted physicians at least 4 times a year. Another cross-sectional study among the Norwegian population found that high adherence to recommended diabetes follow-up procedures in primary care was associated with better glycaemic control and lower estimated CV risk in diabetic patients [23].
Multivariable analysis revealed that rural residence, current smoking, higher self-rated health scores, lack of awareness of adverse consequences of diabetes complications, absence of drug use, and having mixed venues for blood glucose monitoring were factors associated with less regularity of follow-up attendance among study subjects. The results were consistent with our expectations and existing literature which shows that poor primary care gate-keeping is more common in deprived neighbourhoods [24]. A systematic review found that smoking and poor knowledge of diabetes complications were factors associated with follow-up non-attendance [25]. Our observation that patients who were not on glucose-lowering medications had fewer follow-up visits to primary care physicians was also similarly reported in other studies [22,26,27]. It is possible that patients who received antihyperglycaemic drugs were given greater attention through education programmes, personal instructions, and screening. Patients with a better self-rated health status were less likely to regularly attend clinical follow-up in the present study. Results from the Danish arm of the ADDITION-study did not report a significant association between self-rated health and attendance at clinical follow-up [28], but demonstrated that non-adherence to follow-up may occur if patients did not experience a need for extra care because of being relatively healthy. In the context of the Chinese basic public health service delivery, a free-of-charge blood glucose test on-site is available on a quarterly basis for T2DM patients attending primary care facilities [4]. In our study, it is not surprising to observe that patients who had their blood glucose tested only at primary care centres were more likely to achieve greater follow-up attendance.
Routine blood glucose monitoring helps provide timely information on blood glucose level of diabetic patients, in addition to diet, exercise, and medication adherence profiles, to inform evidence-based clinical decision-making. Fasting plasma glucose monitoring is recommended for patients with T2DM on a quarterly basis in primary care diabetes management [4]. In our study, 94.4% of patients with T2DM at moderate to high CVD risk monitored their blood glucose more than once per quarter, which was higher than that reported (88.4%) in another cross-sectional study conducted in Shandong, eastern China [16]. We found that most of patients utilised blood glucose testing services provided by primary care facilities. It is recommended that T2DM patients with lifestyle interventions or on oral hypoglycaemic drugs should have blood glucose monitoring at least twice a week on average [7]. However, the proportion of patients who had weekly blood glucose monitoring in the present study was much lower than that reported in western countries [29,30]. This implies a poor engagement in diabetes care among T2DM patients in China, particularly among those at moderate to high CV risk.
Earlier findings from a cross-sectional survey in eastern China suggested that diabetic patients who lived in urban areas, had a higher education level, had the presence of physician-diagnosed diabetes for over 10 years, and had insulin injection tended to achieve a higher frequency of blood glucose monitoring [15]. This was similarly observed in our study. We further found that a higher self-rated health status was associated with less frequent monitoring of blood glucose, although such association was attenuated after adjustment. It is possible that the motivation to perform blood glucose monitoring is largely influenced by the perceived concern on disease progression [31], and thus a poor self-rated health status was often associated with higher HbA1c levels [32,33]. Therefore, frequent monitoring of blood glucose among patients with poor self-rated health status may be explained by the fear of adverse consequences of diabetic hyperosmolar syndrome. Our results showed that poor awareness of consequences of diabetes complications was associated with less frequent monitoring of blood glucose. It was previously reported that a lower frequency of blood glucose monitoring profile was related to poor knowledge of blood glucose control [16]. It is reasonable to assume that patients who reported that they had their blood glucose tested only at primary care facilities may have no additional monitoring of blood glucose or blood pressure at home, which may contribute to the barriers to continuous treatment [34]. This may underscore a greater need for developing patients’ knowledge and skills required to control blood glucose among T2DM patients with risk factors identified in our study.
4.3. Implications for Research and Practice
The high rate of uncontrolled blood glucose reported in a large-scale survey in China [35] has posed a significant challenge for effective diabetes self-management and appropriate intervention with follow-up strategies, which are part of primary care for addressing multimorbidity [36,37]. Previous studies found that increased primary care visits and blood glucose monitoring could lead to improved glycaemic control and lower the risk of adverse CV outcomes [10,23,38]. Patients with T2DM at higher CV risk often need more intensive care, yet they were found to have poor engagement in follow-up attendance and blood glucose monitoring. In addition, inadequate awareness of adverse consequences of diabetes complications remained common, and was associated with a lower frequency of both follow-up attendance and blood glucose monitoring. Therefore, dedicated and continuous educational inputs from primary care practitioners [39], in combination with effective risk communications [40], are needed in daily clinical practice.
Continuous education on diabetes self-management to facilitate the knowledge and skills required for diabetes care can increase diabetes awareness and improve glycaemic control [41,42], and can exert positive effects on clinical visits and monitoring of blood glucose [43,44,45]. This may be particularly crucial for patients with less access to adequate, structured health education delivered by qualified professionals in primary care settings, compared to that in hospital-based specialist care settings [44]. Education of knowledge on diabetes and its complications should therefore be emphasised during clinical encounter in primary care, accompanied by standardised diabetes education and training programmes especially in rural areas where diabetic patients are less likely to be aware of diabetes complications. Furthermore, the urban–rural divide should be taken into account in diabetes education practice. Rural patients tend to be younger, have less formal education, smoke and drink more, and have shorter diagnosed disease duration, but are just as likely as urban patients to develop diabetes complications as shown in our study. Given the existing evidence on the association between socio-demographic factors and participation in diabetes education [46,47], various educational approaches tailored to the local socio-economic context will be essential to strengthen the capacity of diabetes care. Diabetes education with printed materials may help maximise the effective communication of health messages [48,49], which may be relevant to T2DM patients at higher CV risk who tend to have lower educational attainment in the urban–rural fringe.
4.4. Strengths and Weaknesses of the Study
The target subjects in this study consisted of T2DM patients at moderate to high CV risk, who are commonly encountered in daily primary care but are often struggling with barriers to engage in regular follow-up attendance and routine blood glucose monitoring. A semi-structured questionnaire was used to collect a broad range of information, including the patient’s demographics, routine lifestyle behaviours, disease-related information, healthcare utilisation, and self-reported health status through face-to-face interviews by trained medical practitioners. However, this study has some limitations that should be considered. First, we did not have an electronic health record system where data on follow-up attendance and blood glucose monitoring can be directly retrieved. Thus, recall bias may arise from self-reporting despite rigorous quality control. Secondly, the awareness of adverse consequences of diabetes complications was ascertained based on a single question. This may limit the extent to which our results are comparable with other studies due to inconsistent methodology. Third, subjects in this study were drawn from the register of diabetic management in primary care settings. Patients with T2DM who were not enrolled may not be captured in our study. Last but not least, we were not able to make inferences about causality or temporal ordering of events due to the cross-sectional nature of the study. Future research using data collected from computerised health records will help to provide longitudinal evidence for optimising diabetes care.
5. Conclusions
In the present study, our findings suggested that follow-up care delivered in primary care was not adequately utilised by Chinese patients with T2DM who were at moderate to high CV risk, and that patients’ engagement in blood glucose monitoring was suboptimal overall. Living in rural areas and having poor awareness of diabetes complications acted as significant barriers to both follow-up attendance and blood glucose monitoring. This would require dedicated and continuous educational inputs from primary care practitioners to increase awareness of adverse consequences of diabetes complications in daily clinical practice. Our results revealed a significant urban–rural divide in patients’ engagement in regular follow-up attendance and blood glucose monitoring, which suggested the need for different educational approaches tailored to the local socio-economic context to strengthen the capacity of diabetes care.
Author Contributions
Conceptualisation, Y.L. and Y.-T.L.; data curation, Y.-T.L. and W.H.; formal analysis, Y.L. and Q.Z.; validation, H.C.; methodology, Y.L.; project administration, Y.-T.L.; supervision, W.H. and H.H.X.W.; writing—original draft preparation, Y.L. and Y.-T.L.; writing—review and editing, S.Z. and H.H.X.W. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partly supported by the Open Research Funds of the State Key Laboratory of Ophthalmology [grant numbers 303060202400377 and 303060202400362]. The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Institutional Review Board Statement
Ethics approval was sought and granted by the Zhongshan Ophthalmic Center Medical Ethics Committee (Ref: 2017KYPJ094; approved on 25 October 2017) at Sun Yat-Sen University.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author.
Acknowledgments
We wish to thank our research collaborators and frontline staff who involved in survey design and data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Li, Y.; Teng, D.; Shi, X.; Qin, G.; Qin, Y.; Quan, H.; Shi, B.; Sun, H.; Ba, J.; Chen, B.; et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: National cross sectional study. BMJ 2020, 369, m997. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.; Hu, D.; Pan, C.; Weng, J.; Huo, Y.; Ma, C.; Mu, Y.; Hao, C.; Ji, Q.; Ran, X.; et al. Primacy of the 3B approach to control risk factors for cardiovascular disease in type 2 diabetes patients. Am. J. Med. 2013, 126, e11–e22. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Zhou, D.; Li, N.; Han, B. Predicting Diabetes and Estimating Its Economic Burden in China Using Autoregressive Integrated Moving Average Model. Int. J. Public Health 2022, 66, 1604449. [Google Scholar] [CrossRef] [PubMed]
- Department of Primary Health Care, National Health Commission, PRC. Standards for National Basic Public Health Services (3rd ed.). 2017. Available online: http://www.nhc.gov.cn/jws/s3578/201703/aefef3d0b2a14279b76ad57d7e7a2c4e.shtml (accessed on 30 October 2021).
- American Diabetes Association. Standards of Medical Care in Diabetes-2017 Abridged for Primary Care Providers. Clin. Diabetes 2017, 35, 5–26. [Google Scholar] [CrossRef]
- International Diabetes Federation Guideline Development Group. Global guideline for type 2 diabetes. Diabetes Res. Clin. Pract. 2014, 104, 1–52. [Google Scholar] [CrossRef]
- Jia, W.; Weng, J.; Zhu, D.; Ji, L.; Lu, J.; Zhou, Z.; Zou, D.; Guo, L.; Ji, Q.; Chen, L.; et al. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab. Res. Rev. 2019, 35, e3158. [Google Scholar] [CrossRef]
- Morrison, F.; Shubina, M.; Turchin, A. Encounter frequency and serum glucose level, blood pressure, and cholesterol level control in patients with diabetes mellitus. Arch Intern. Med. 2011, 171, 1542–1550. [Google Scholar] [CrossRef]
- Anjana, R.M.; Shanthirani, C.S.; Unnikrishnan, R.; Mugilan, P.; Amutha, A.; Nair, H.D.; Subhashini, S.; Venkatesan, U.; Ali, M.; Ranjani, H.; et al. Regularity of follow-up, glycemic burden, and risk of microvascular complications in patients with type 2 diabetes: A 9-year follow-up study. Acta Diabetol. 2015, 52, 601–609. [Google Scholar] [CrossRef]
- Ji, L.; Su, Q.; Feng, B.; Shan, Z.; Hu, R.; Xing, X.; Xue, Y.; Yang, T.; Hua, Y. Structured self-monitoring of blood glucose regimens improve glycemic control in poorly controlled Chinese patients on insulin therapy: Results from COMPASS. J. Diabetes 2017, 9, 495–501. [Google Scholar] [CrossRef]
- Chircop, J.; Sheffield, D.; Kotera, Y. Systematic Review of Self-Monitoring of Blood Glucose in Patients With Type 2 Diabetes. Nurs. Res. 2021, 70, 487–497. [Google Scholar] [CrossRef]
- Wang, J.; Zuo, H.; Chen, X.; Hou, L.; Ma, J. Analysis of factors influencing the frequency of primary care visits among diabetic patients in two provinces in China. BMC Public Health 2019, 19, 1267. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Guo, X.; Xiong, Z.; Lou, Q.; Shen, L.; Zhao, F.; Sun, Z.; Li, J. Self-monitoring of blood glucose in type 2 diabetic patients in China: Current status and influential factors. Chin. Med. J. (Engl.) 2014, 127, 201–207. [Google Scholar] [PubMed]
- Wang, Y.; Hu, X.-J.; Wang, H.H.X.; Duan, H.-Y.; Chen, Y.; Li, Y.-T.; Luo, Z.-L.; Li, X.; Wang, J.-J.; Mercer, S.W. Follow-up care delivery in community-based hypertension and type 2 diabetes management: A multi-centre, survey study among rural primary care physicians in China. BMC Fam. Pract. 2021, 22, 224. [Google Scholar] [CrossRef] [PubMed]
- Raoufi, A.M.; Tang, X.; Jing, Z.; Zhang, X.; Xu, Q.; Zhou, C. Blood Glucose Monitoring and Its Determinants in Diabetic Patients: A Cross-Sectional Study in Shandong, China. Diabetes Ther. 2018, 9, 2055–2066. [Google Scholar] [CrossRef]
- Yao, J.; Wang, H.; Yan, J.; Shao, D.; Sun, Q.; Yin, X. Understanding the Profiles of Blood Glucose Monitoring Among Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study in Shandong, China. Patient Prefer. Adherence 2021, 15, 399–409. [Google Scholar] [CrossRef]
- Weng, J.; Ji, L.; Jia, W.; Lu, J.; Zhou, Z.; Zou, D.; Zhu, D.; Chen, L.; Chen, L.; Guo, L.; et al. Standards of care for type 2 diabetes in China. Diabetes Metab. Res. Rev. 2016, 32, 442–458. [Google Scholar] [CrossRef]
- Liu, L.S.; Writing Group of 2018 Chinese Guidelines for the Management of Hypertension. Chinese Hypertension League and Chinese Society of Cardiology. 2018 Chinese guidelines for the management of hypertension. Chin. J. Cardiovasc. Med. 2019, 24, 1–46. [Google Scholar]
- Pan, X.-F.; Wang, L.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Tian, M.; Wang, H.; Tong, X.; Zhu, K.; Zhang, X.; Chen, X. Essential Public Health Services’ Accessibility and its Determinants among Adults with Chronic Diseases in China. PLoS ONE 2015, 10, e0125262. [Google Scholar] [CrossRef]
- He, M.; Gao, J.; Liu, W.; Tang, X.; Tang, S.; Long, Q. Case management of patients with Type 2 diabetes mellitus: A cross-sectional survey in Chongqing, China. BMC Health Serv. Res. 2017, 17, 129. [Google Scholar] [CrossRef]
- Renard, L.M.; Bocquet, V.; Vidal-Trecan, G.; Lair, M.-L.; Blum-Boisgard, C. Adherence to international follow-up guidelines in type 2 diabetes: A longitudinal cohort study in Luxembourg. PLoS ONE 2013, 8, e80162. [Google Scholar] [CrossRef] [PubMed]
- Nøkleby, K.; Berg, T.J.; Mdala, I.; Buhl, E.S.; Claudi, T.; Cooper, J.G.; Løvaas, K.F.; Sandberg, S.; Jenum, A.K. High adherence to recommended diabetes follow-up procedures by general practitioners is associated with lower estimated cardiovascular risk. Diabet. Med. 2021, 38, e14586. [Google Scholar] [CrossRef]
- Parker, M.M.; Moffet, H.H.; Schillinger, D.; Adler, N.; Fernandez, A.; Ciechanowski, P.; Karter, A.J. Ethnic differences in appointment-keeping and implications for the patient-centered medical home--findings from the Diabetes Study of Northern California (DISTANCE). Health Serv. Res. 2012, 47, 572–593. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Samsudin, M.; Thirumoorthy, T.; Low, L.; Kwan, Y. Factors affecting follow-up non-attendance in patients with Type 2 diabetes mellitus and hypertension: A systematic review. Singap. Med. J. 2019, 60, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Simmons, D.; Fleming, C. Prevalence and characteristics of diabetic patients with no ongoing care in South Auckland. Diabetes Care 2000, 23, 1791–1793. [Google Scholar] [CrossRef] [PubMed]
- Chew, B.-H.; Lee, P.-Y.; Shariff-Ghazali, S.; Cheong, A.-T.; Ismail, M.; Taher, S.-W. Predictive factors of follow-up non-attendance and mortality among adults with type 2 diabetes mellitus- an analysis of the Malaysian diabetes registry 2009. Curr. Diabetes Rev. 2015, 11, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Jensen, A.D.; Andersen, S.T.; Charles, M.; Bjerg, L.; Witte, D.R.; Gram, B.; Jørgensen, M.E.; Sandbæk, A.; Dalsgaard, E.-M. Factors associated with attendance at clinical follow-up of a cohort with screen-detected type 2 diabetes: ADDITION-Denmark. Prim. Care Diabetes. 2020, 14, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Skelly, A.H.; Arcury, T.A.; Snively, B.M.; Bell, R.A.; Smith, S.L.; Wetmore, L.K.; Quandt, S.A. Self-monitoring of blood glucose in a multiethnic population of rural older adults with diabetes. Diabetes Educ. 2005, 31, 84–90. [Google Scholar] [CrossRef]
- Barnard, K.D.; Young, A.J.; Waugh, N.R. Self-monitoring of blood glucose-a survey of diabetes UK members with type 2 diabetes who use SMBG. BMC Res. Notes 2010, 3, 318. [Google Scholar] [CrossRef]
- Al-Keilani, M.S.; Almomani, B.A.; Al-Sawalha, N.A.; Shhabat, B.A. Self-monitoring of blood glucose among patients with diabetes in Jordan: Perception, adherence, and influential factors. Diabetes Res. Clin. Pract. 2017, 126, 79–85. [Google Scholar] [CrossRef]
- Kane, N.S.; Hoogendoorn, C.J.; Commissariat, P.V.; Schulder, T.E.; Gonzalez, J.S. Glycemic control and self-rated health among ethnically diverse adolescents with type 1 diabetes. Pediatr. Diabetes 2020, 21, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Abualula, N.A.; Rodan, M.F.; Milligan, R.A.; Jacobsen, K.H. Self-rated health among American adolescents with type 1 diabetes in the T1D Exchange Clinic Registry. J. Diabetes Complicat. 2018, 32, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.H.X.; Mercer, S.W. Understanding Barriers to Adherence to Optimal Treatment of Elevated Blood Pressure and Hypertension-Insights From Primary Care. JAMA Netw. Open 2021, 4, e2138651. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.-N.; Lu, J.-M.; Guo, X.-H.; Yang, W.-Y.; Weng, J.-P.; Jia, W.-P.; Zou, D.-J.; Zhou, Z.-G.; Yu, D.-M.; Liu, J.; et al. Glycemic control among patients in China with type 2 diabetes mellitus receiving oral drugs or injectables. BMC Public Health 2013, 13, 602. [Google Scholar] [CrossRef] [PubMed]
- Loskutova, N.Y.; Tsai, A.G.; Callen, E.; Ajayi, K.; Carroll, J.K.; Harrington, M.; Turner, T.J.; Pace, W.D. Differences in perspectives regarding diabetes management between health care providers and patients. Transl. Behav. Med. 2018, 8, 328–340. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.-J.; Wang, H.H.X.; Li, Y.-T.; Wu, X.-Y.; Wang, Y.; Chen, J.-H.; Wang, J.-J.; Wong, S.Y.S.; Mercer, S.W. Healthcare needs, experiences and treatment burden in primary care patients with multimorbidity: An evaluation of process of care from patients’ perspectives. Health Expect. 2022, 25, 203–213. [Google Scholar] [CrossRef]
- Chudyk, A.; Shapiro, S.; Russell-Minda, E.; Petrella, R. Self-monitoring technologies for type 2 diabetes and the prevention of cardiovascular complications: Perspectives from end users. J. Diabetes Sci. Technol. 2011, 5, 394–401. [Google Scholar] [CrossRef]
- Wang, H.H.X.; Wang, J.J.; Zhou, Z.H.; Wang, X.W.; Xu, L. General practice education and training in southern China: Recent development and ongoing challenges under the health care reform. Malays. Fam. Physician 2013, 8, 2–10. [Google Scholar]
- Wang, H.H.X.; Li, Y.T.; Wong, M.C.S. Leveraging the power of health communication: Messaging matters not only in clinical practice but also in public health. Hong Kong Med. J. 2022, 28, 103–105. [Google Scholar] [CrossRef]
- Flores-Luevano, S.; Pacheco, M.; Shokar, G.S.; Dwivedi, A.K.; Shokar, N.K. Impact of a Culturally Tailored Diabetes Education and Empowerment Program in a Mexican American Population Along the US/Mexico Border: A Pragmatic Study. J. Clin. Med. Res. 2020, 12, 517–529. [Google Scholar] [CrossRef]
- Kim, G.H.; Park, Y.; Lim, H.-S. The Association between Diabetes Education and Glucose Control in Diabetic Patients: Using the 2008 and 2013 Korea National Health and Nutrition Examination Survey. Clin. Nutr. Res. 2020, 9, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Sukkarieh-Haraty, O.; Egede, L.E.; Khazen, G.; Abi Kharma, J.; Farran, N.; Bassil, M. Results from the first culturally tailored, multidisciplinary diabetes education in Lebanese adults with type 2 diabetes: Effects on self-care and metabolic outcomes. BMC Res. Notes 2022, 15, 39. [Google Scholar] [CrossRef] [PubMed]
- Lou, Q.; Wu, L.; Dai, X.; Cao, M.; Ruan, Y. Diabetes education in mainland China- a systematic review of the literature. Patient Educ. Couns. 2011, 85, 336–347. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.-J.; Wu, H.-F.; Li, Y.-T.; Wang, Y.; Cheng, H.; Wang, J.-J.; Mohammed, B.H.; Tan, I.; Wang, H.H.X. Influence of health education on clinical parameters in type 2 diabetic subjects with and without hypertension: A longitudinal, comparative analysis in routine primary care settings. Diabetes Res. Clin. Pract. 2020, 170, 108539. [Google Scholar] [CrossRef] [PubMed]
- Brown-Guion, S.Y.; Youngerman, S.M.; Hernandez-Tejada, M.A.; Dismuke, C.E.; Egede, L.E. Racial/ethnic, regional, and rural/urban differences in receipt of diabetes education. Diabetes Educ. 2013, 39, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H. Sociodemographic Factors Associated with Participation in Diabetes Education among Community-Dwelling Adults with Diabetes. Yonsei Med. J. 2020, 61, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Devchand, R.; Nicols, C.; Gallivan, J.M.; Tiktin, M.; Krause-Steinrauf, H.; Larkin, M.; Tuncer, D.M. The GRADE Research Group. Assessment of a National Diabetes Education Program diabetes management booklet: The GRADE experience. J. Am. Assoc. Nurse Pract. 2017, 29, 255–263. [Google Scholar] [CrossRef]
- Devchand, R.; Sheehan, P.; Gallivan, J.M.; Tuncer, D.M.; Nicols, C. D2d Research Group. Assessment of a National Diabetes Education Program diabetes prevention toolkit: The D2d experience. J. Am. Assoc. Nurse Pract. 2017, 29, 514–520. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).