Plantar Fasciitis in Soccer Players—A Systemic Review
Abstract
1. Introduction
1.1. Plantar Fascia and the Windlass Mechanism
1.2. Etiopathogenesis of Plantar Fasciitis
1.3. Plantar Fasciitis in Sport
2. Objectives
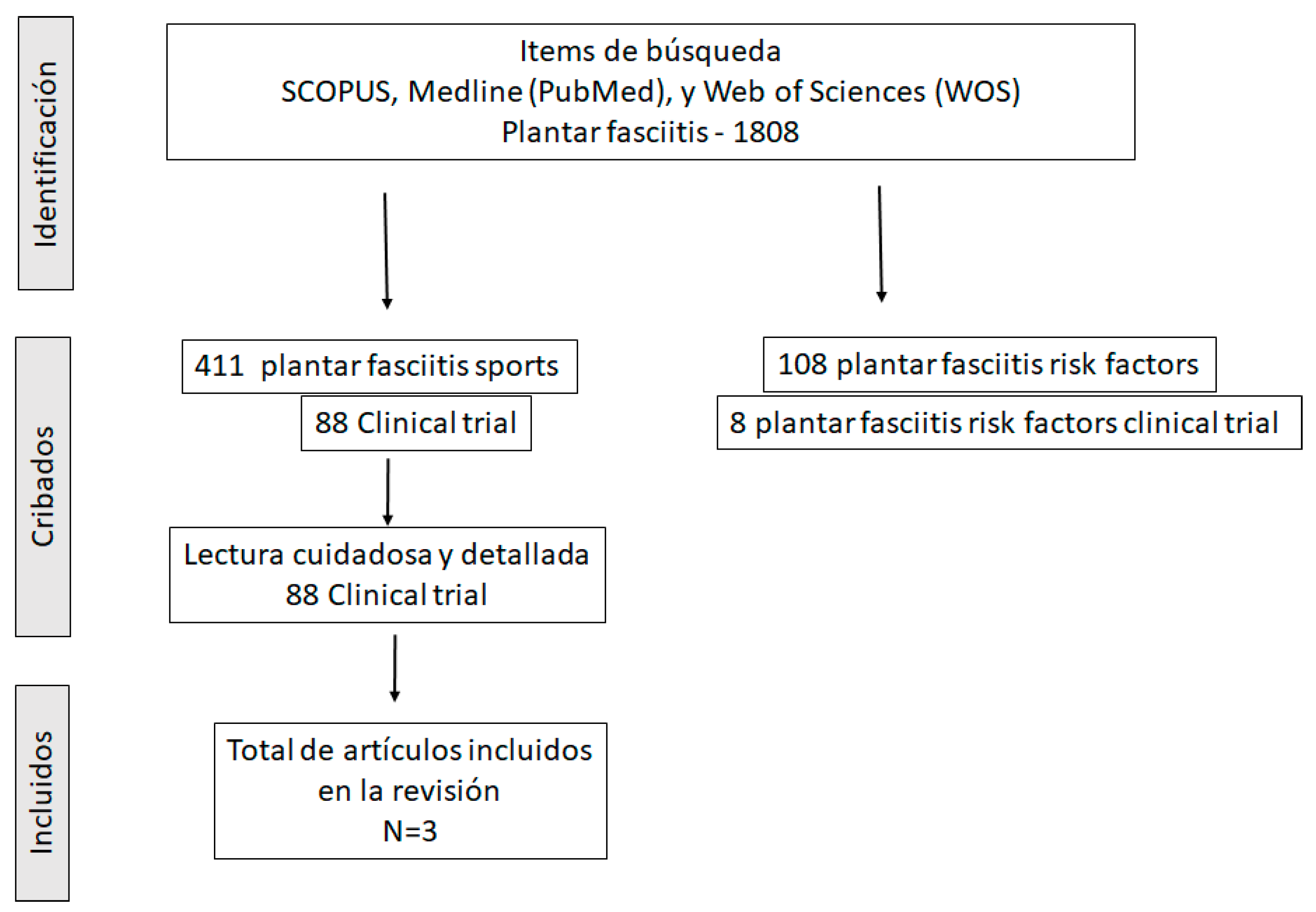
3. Methodology
3.1. Inclusion Criteria
3.2. Exclusion Criteria
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Petraglia, F.; Ramazzina, I.; Costantino, C. Plantar fasciitis in athletes: Diagnostic and treatment strategies. A systematic review. MLTJ 2017, 10, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Wearing, S.C.; Smeathers, J.E.; Urry, S.R.; Hennig, E.; Hills, A.P. The Pathomechanics of Plantar Fasciitis. Sport. Med. 2006, 36, 585–611. [Google Scholar] [CrossRef] [PubMed]
- Cornwall, M.W.; McPoil, T.G. Plantar fasciitis: Etiology and treatment. J. Orthop. Sports Phys. Ther. 1999, 29, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Trojian, T.; Tucker, A.K. Plantar Fasciitis. Am. Fam. Physician 2019, 99, 744–750. [Google Scholar] [PubMed]
- Córdova, A.; López, D.; Fernández-Lazaro, D.; Caballero, A. New vision of the treatment of plantar fasciitis in athletes. Usefulness of functional training through skiing. Investig. Clin. 2017, 58, 309–318. [Google Scholar]
- Riddle, D.L.; Pulisic, M.; Pidcoe, P.; Johnson, R.E. Risk factors for Plantar fasciitis: A matched case-control study. J. Bone Jt. Surg. Am. 2003, 85, 872–877. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.V.; Saini, S.S.; Reb, C.W.; Daniel, J.N. Diagnosis and Management of Plantar Fasciitis. J. Osteopat. Med. 2014, 114, 900–901. [Google Scholar] [CrossRef]
- Van Leeuwen, K.D.B.; Rogers, J.; Winzenberg, T.; Van Middelkoop, M. Higher body mass index is associated with plantar fasciopathy/‘plantar fasciitis’: Systematic review and meta-analysis of various clinical and imaging risk factors. Br. J. Sports Med. 2015, 50, 972–981. [Google Scholar] [CrossRef]
- Hamstra-Wright, K.L.; Bliven, K.C.H.; Bay, R.C.; Aydemir, B. Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis. Sport Health 2021, 13, 296–303. [Google Scholar] [CrossRef]
- Martinelli, N.; Bonifacini, C.; Romeo, G. Current therapeutic approaches for plantar fasciitis. Orthop. Res. Rev. 2014, 6, 33–40. [Google Scholar] [CrossRef][Green Version]
- Kirby, K. Biomechanics of the normal and abnormal foot. J. Am. Podiatr. Med. Assoc. 2000, 90, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Ker, R.F.; Bennett, M.B.; Bibby, S.R.; Kester, R.C.; Alexander, R.M. The spring in the arch of the human foot. Nature 1987, 325, 147–149. [Google Scholar] [CrossRef] [PubMed]
- A Bolgla, L.; Malone, T.R. Plantar fasciitis and the windlass mechanism: A biomechanical link to clinical practice. J. Athl. Train. 2004, 39, 77–82. [Google Scholar] [PubMed]
- Dananberg, H.J. Functional Hallux Limitus and its relationship to gait efficiency. JAPMA 1986, 76, 648–652. [Google Scholar]
- Padilla, V.; Orejana, Á.M.; Mendez, M.; Martínez-Santosa, A.; Moreno-Martína, F.J.; Sardón, S.; Tornero, M.C. Hallux limitus funcional y asociaciones clínicas. Rev. Esp. Podol. XXII 2011, 22, 190–194. [Google Scholar]
- Barry, M. Causation and risk factors of Plantar Fasciitis. ACC Res. 2016, 12, 1–37. [Google Scholar]
- García-Vidal, J.A.; Piñero, J.G.; Baño, A.; Sánchez-Martínez, M.P.; Medina-Mirapeix, F. Value of the Silfverskiöld test for the diagnosis of plantar. fasciitis. Rev. Int. Cienc. Podol. 2018, 13, 41–46. [Google Scholar]
- Sharkey, N.A.; Ferris, L.; Donahue, S.W. Biomechanical Consequences of Plantar Fascial Release or Rupture During Gait: Part I—Disruptions in Longitudinal Arch Conformation. Foot Ankle Int. 1998, 19, 812–820. [Google Scholar] [CrossRef]
- Erdemir, A.; Hamel, A.J.; Fauth, A.R.; Piazza, S.J.; Sharkey, N.A. Dynamic Loading of the Plantar Aponeurosis in Walking. J. Bone Jt. Surg. 2004, 86, 546–552. [Google Scholar] [CrossRef]
- Barry, L.D.; Barry, A.N.; Chen, Y. A retrospective study of standing gastrocnemius-soleus stretching versus night splinting in the treatment of plantar fasciitis. J. Foot Ankle Surg. 2002, 41, 221–227. [Google Scholar] [CrossRef]
- La Porta, G.A.; La Fata, P.C. Pathologic conditions of the plantar fascia. Clin. Podiatr. Med. Surg. 2005, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.M.; Cook, J.L.; Taunton, J.E.; Bonar, F. Overuse tendinosis, not tendinitis: A new paradigm for a difficult clinical problem (part 1). Phys. Sportsmed. 2000, 28, 38–48. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hicks, J.H. The mechanics of the foot. II. The plantar aponeurosis and the arch. J. Anat. 1954, 88, 25–30. [Google Scholar] [PubMed]
- Crosby, W.; Humble, R.N. Rehabilitation of plantar fasciitis. Clin. Pod. Med. Surg. 2001, 18, 225–231. [Google Scholar]
- Ben Kibler, W.; Goldberg, C.; Chandler, T.J. Functional biomechanical deficits in running athletes with plantar fasciitis. Am. J. Sport. Med. 1991, 19, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Lemont, H.; Ammirati, K.M.; Usen, N. Plantar fasciitis: A degenerative process (fasciosis) without inflammation. J. Am. Podiatr. Med. Assoc. 2003, 93, 234–237. [Google Scholar] [CrossRef]
- Buchbinder, R. Clinical practice. Plantar fasciitis. N. Engl. J. Med. 2004, 350, 2159–2166. [Google Scholar] [CrossRef]
- Torrijos, A.; Abián-Vicén, J.; Abián, P.; Abián, M. Plantar fasciitis treatment. J. Sport Health Res. 2009, 1, 123–131. [Google Scholar]
- Chang, R.; Rodrigues, P.A.; Van Emmerik, R.E.; Hamill, J. Multi-segment foot kinematics and ground reaction forces during gait of individuals with plantar fasciitis. J. Biomech. 2014, 47, 2571–2577. [Google Scholar] [CrossRef]
- Tenforde, A.S.; Yin, A.; Hunt, K.J. Foot and ankle injuries in runners. Phys. Med. Rehabil. Clin. N. Am. 2016, 27, 121–137. [Google Scholar] [CrossRef]
- Orchard, J. Plantar fasciitis. BMJ 2012, 345, e6603. [Google Scholar] [CrossRef] [PubMed]
- Sobhani, S.; Dekker, R.; Postema, K.; Dijkstra, P.U. Epidemiology of ankle and foot overuse injuries in sports: A systematic review. Scand. J. Med. Sci. Sport. 2012, 23, 669–686. [Google Scholar] [CrossRef] [PubMed]
- Elias, D.A.; Carne, A.; Bethapudi, S.; Engebretsen, L.; Budgett, R.; O’Connor, P. Imaging of plantar fascia and Achilles injuries undertaken at the London 2012 Olympics. Skelet. Radiol. 2013, 42, 1645–1655. [Google Scholar] [CrossRef]
- Saggini, R.; Migliorini, M.; Carmignano, S.M.; Ancona, E.; Russo, C.; Bellomo, R.G. Inferior heel pain in soccer players: A retrospective study with a proposal for guidelines of treatment. BMJ Open Sport Exerc. Med. 2018, 4, e000085. [Google Scholar] [CrossRef]
- Suzue, N.; Iwame, T.; Kato, K.; Takao, S.; Tateishi, T.; Takeda, Y.; Hamada, D.; Goto, T.; Takata, Y.; Matsuura, T.; et al. Plantar Fascia Rupture in a Professional Soccer Player. J. Med. Investig. 2014, 61, 413–416. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Costa, I.A.; Dyson, A. The integration of acetic acid iontophoresis, orthotic therapy and physical rehabilitation for chronic plantar fasciitis: A case study. J. Can. Chiropr. Assoc. 2007, 51, 166–174. [Google Scholar]
- Luffy, L.; Grosel, J.; Thomas, R.; So, E. Plantar fasciitis. J. Am. Acad. Physician Assist. 2018, 31, 20–24. [Google Scholar] [CrossRef]
- Wong, P. Soccer injury in the lower extremities. Br. J. Sports Med. 2005, 39, 473–482. [Google Scholar] [CrossRef]
- Schaff, P.; Hauser, W. Measuring pressure distribution on the human tibia in ski-boots. Sportverletz. Sportsc. 1987, 1, 118–129. [Google Scholar] [CrossRef]
- Cheung, J.T.-M.; Zhang, M.; An, K.-N. Effect of Achilles tendon loading on plantar fascia tension in the standing foot. Clin. Biomech. 2006, 21, 194–203. [Google Scholar] [CrossRef]
- Fu, F.H.; Stone, D.A. Sports Injuries: Mechanisms, Prevention, Treatment, 2nd ed.; Lippincott, Williams & Wilkins: Philadelphia, PA, USA, 1994. [Google Scholar]
- Brotzman, S.B.; Manske, R.C. Rehabilitación Ortopédica Clínica, 3rd ed.; Elsevier: Barcelona, Spain, 2012. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noriega, D.C.; Cristo, Á.; León, A.; García-Medrano, B.; Caballero-García, A.; Córdova-Martinez, A. Plantar Fasciitis in Soccer Players—A Systemic Review. Int. J. Environ. Res. Public Health 2022, 19, 14426. https://doi.org/10.3390/ijerph192114426
Noriega DC, Cristo Á, León A, García-Medrano B, Caballero-García A, Córdova-Martinez A. Plantar Fasciitis in Soccer Players—A Systemic Review. International Journal of Environmental Research and Public Health. 2022; 19(21):14426. https://doi.org/10.3390/ijerph192114426
Chicago/Turabian StyleNoriega, David C., Ángel Cristo, Alejandro León, Belén García-Medrano, Alberto Caballero-García, and Alfredo Córdova-Martinez. 2022. "Plantar Fasciitis in Soccer Players—A Systemic Review" International Journal of Environmental Research and Public Health 19, no. 21: 14426. https://doi.org/10.3390/ijerph192114426
APA StyleNoriega, D. C., Cristo, Á., León, A., García-Medrano, B., Caballero-García, A., & Córdova-Martinez, A. (2022). Plantar Fasciitis in Soccer Players—A Systemic Review. International Journal of Environmental Research and Public Health, 19(21), 14426. https://doi.org/10.3390/ijerph192114426







