Are Attitudes towards COVID-19 Pandemic Related to Subjective Physical and Mental Health?
Abstract
1. Introduction
1.1. Impact of the COVID-19 Pandemic on Human Health
1.2. Perception of the COVID-19 Pandemic by the Population
2. Materials and Methods
3. Results
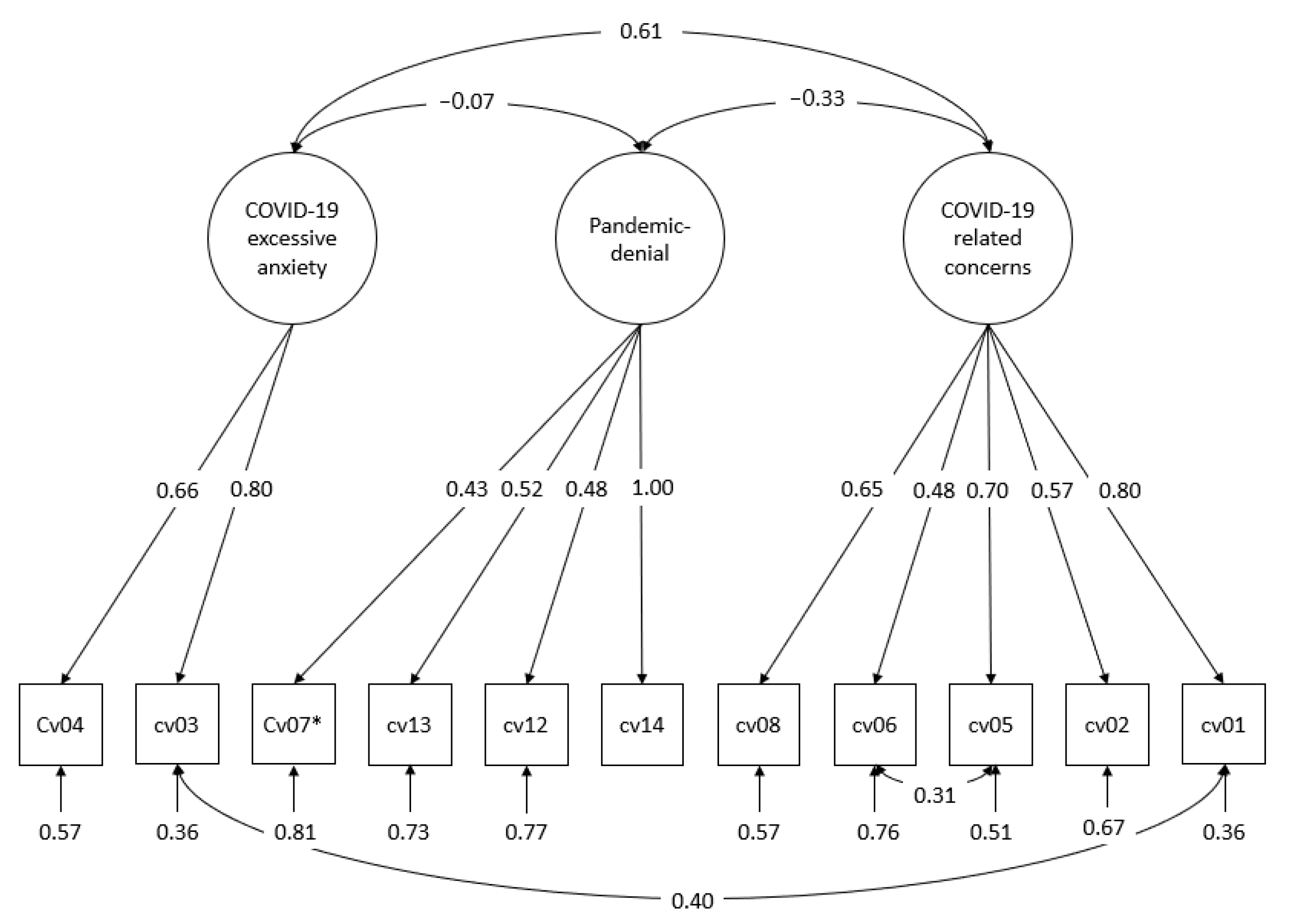
3.1. Dimensionality of COVID-19-Related Attitudes
3.2. Stability and Interaction between Psychological Distress and Subjective Physical Health over Time
3.3. Influence of D-Score and G-Score on COVID-19 Attitudes
3.4. Role of Socio-Demographic Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Gender (in %) | |
| Male | 46.4 |
| Female | 53.6 |
| Age (mean) | 48.4 |
| Children (in %) | 79.7 |
| Number of children (mean) | 1.79 |
| Family status (in %) | |
| Married living together | 55.0 |
| Married living separately | 3.4 |
| Single | 29.9 |
| Divorced | 10.0 |
| Widowed | 1.7 |
| Steady partner (in %) | 79.9 |
| Occupational status (in %) | |
| Worker | 19.7 |
| Employee | 60.3 |
| Self-employed | 6.9 |
| Housewife/househusband/parental leave | 1.0 |
| Civil servant | 6.9 |
| Unemployed | 2.4 |
| Other | 2.8 |
| Net household income in € (median) * | 3500 to 3999 |
| Migration background (in %) | |
| Immigrated to West Germany | 21.7 |
| Immigrated abroad | 2.7 |
| Lives in East Germany | 75.5 |
| Minimum “Disagree” | Maximum “Agree” | Mean | Standard Deviation | Skewness | Kurtosis | N | |
|---|---|---|---|---|---|---|---|
| I am afraid of becoming infected with COVID-19. | 1 | 5 | 2.87 | 1.263 | 0.034 | −1.236 | 291 |
| I feel like I have little control over whether or not I get infected with COVID-19. | 1 | 5 | 2.87 | 1.204 | 0.094 | −1.019 | 289 |
| I am afraid of infecting others with COVID-19. | 1 | 5 | 2.52 | 1.280 | 0.347 | −1.141 | 289 |
| My family and friends are afraid that they will get infected by me with COVID-19. | 1 | 5 | 2.09 | 1.063 | 0.709 | −−0.380 | 289 |
| COVID-19 worries me. | 1 | 5 | 3.38 | 1.203 | −0.572 | −0.686 | 290 |
| COVID-19 is not much worse than the annually recurring flu. | 1 | 5 | 2.54 | 1.318 | 0.470 | −0.941 | 290 |
| I feel like I have to give up because of COVID-19. | 1 | 5 | 1.46 | 0.835 | 1.920 | 3.244 | 291 |
| I feel like I would not survive a COVID-19 infection. | 1 | 5 | 1.87 | 0.939 | 1.025 | 0.682 | 291 |
| The German government has taken the right steps in dealing with COVID-19. | 1 | 5 | 2.51 | 1.212 | 0.238 | −1.218 | 290 |
| The COVID-19 crisis has been talked about in such a way that few can benefit from it. | 1 | 7 | 3.90 | 2.123 | −0.017 | 1.325 | 290 |
| The actual background of the coronavirus disease will never come to light. | 1 | 7 | 4.89 | 2.054 | −0.652 | −0.895 | 291 |
| 1 “No” | 2 “Yes, for a Few Months Now” | 3 “Yes, for Years” | Missing | |
|---|---|---|---|---|
| Measured in 2019 | ||||
| I often feel depressed and discouraged. | 77.0 | 11.0 | 11.7 | 0.3 |
| Sometimes I do not know what the meaning of my life is anymore. | 89.3 | 3.1 | 6.9 | 0.7 |
| I am often at a loss; I no longer understand the world. | 83.2 | 6.5 | 7.6 | 2.7 |
| Are you afraid of the future? | 74.9 | 13.7 | 10.7 | 0.7 |
| Measured in 2021 | ||||
| I often feel depressed and discouraged. | 75.3 | 14.1 | 10.3 | 0.3 |
| Sometimes I do not know what the meaning of my life is anymore. | 88.3 | 6.2 | 5.2 | 0.3 |
| I am often at a loss, I no longer understand the world. | 81.1 | 11.3 | 7.2 | 0.3 |
| Are you afraid of the future? | 72.2 | 19.6 | 7.6 | 0.7 |
| 1 “Never” | 2 “Seldom” | 3 “From Time to Time” | 4 “Frequently” | Missing | |
|---|---|---|---|---|---|
| Measured in 2019 | |||||
| Nervousness | 30.2 | 30.6 | 26.8 | 11.3 | 1.0 |
| Stomach trouble | 49.8 | 25.1 | 18.6 | 5.5 | 1.0 |
| Insomnia | 25.1 | 29.6 | 30.6 | 14.8 | 0.0 |
| Heart trouble | 68.4 | 15.8 | 11.3 | 2.4 | 2.1 |
| Measured in 2021 | |||||
| Nervousness | 35.4 | 27.8 | 26.5 | 8.9 | 1.4 |
| Stomach trouble | 54.6 | 20.3 | 17.5 | 7.2 | 0.3 |
| Insomnia | 31.6 | 25.4 | 27.5 | 14.4 | 1.0 |
| Heart trouble | 67.0 | 17.5 | 11.3 | 2.7 | 1.4 |
References
- Statista. Aktive Fälle, Geheilte Patienten und Todesfälle in Zusammenhang mit dem Coronavirus (COVID-19) Weltweit Seit Januar 2020. Available online: https://de.statista.com/statistik/daten/studie/1106392/umfrage/aktive-faelle-des-coronavirus-covid-19-weltweit/ (accessed on 17 September 2022).
- Sachverständigenausschuss. Evaluation der Rechtsgrundlagen und Maßnahmen der Pandemiepolitik: Bericht des Sachverständigenausschusses nach § 5 Abs. 9 IFSG; Bundesgesundheitsministerium: Berlin, Germany, 2022. [Google Scholar]
- Lazarus, R.S.; Cohen, J.B. Environmental stress. In Human Behavior and the Environment: Current Theory and Research; Altman, I., Wohlwill, J.F., Eds.; Plenum: New York, NY, USA, 1977; pp. 89–127. [Google Scholar]
- Lazarus, R.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Folkman, S.; Lazarus, R.S. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J. Personal. Soc. Psychol. 1985, 48, 150–170. [Google Scholar] [CrossRef]
- Petersen, E.L.; Goßling, A.; Adam, G.; Aepfelbacher, M.; Behrendt, C.-A.; Cavus, E.; Cheng, B.; Fischer, N.; Gallinat, J.; Kühn, S.; et al. Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme. Eur. Heart J. 2022, 43, 1124–1137. [Google Scholar] [CrossRef] [PubMed]
- Douaud, G.; Lee, S.; Alfaro-Almagro, F.; Arthofer, C.; Wang, C.; McCarthy, P.; Lange, F.; Andersson, J.L.R.; Griffanti, L.; Duff, E.; et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 2022, 604, 697–707. [Google Scholar] [CrossRef]
- Berth, H.; Brähler, E.; Zenger, M.; Stöbel-Richter, Y. Die sächsische Längsschnittstudie. Zahlen und Fakten. In 30 Jahre Ostdeutsche Transformation. Sozialwissenschaftliche Ergebnisse und Perspektiven der Sächsischen Längsschnittstudie; Berth, H., Brähler, E., Zenger, M., Stöbel-Richter, Y., Eds.; Psychosozial-Verlag: Gießen, Germany, 2020; pp. 21–31. [Google Scholar]
- Nehme, M.; Braillard, O.; Alcoba, G.; Aebischer Perone, S.; Courvoisier, D.; Chappuis, F.; Guessous, I. COVID-19 Symptoms: Longitudinal Evolution and Persistence in Outpatient Settings. Ann. Intern. Med. 2021, 174, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Del Rio, C.; Collins, L.F.; Malani, P. Long-term Health Consequences of COVID-19. JAMA 2020, 324, 1723–1724. [Google Scholar] [CrossRef] [PubMed]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Shakil, M.; Ashraf, F.; Muazzam, A.; Amjad, M.; Javed, S. Work status, death anxiety and psychological distress during COVID-19 pandemic: Implications of the terror management theory. Death Stud. 2022, 46, 1100–1105. [Google Scholar] [CrossRef]
- Ambelu, A.; Birhanu, Z.; Yitayih, Y.; Kebede, Y.; Mecha, M.; Abafita, J.; Belay, A.; Fufa, D. Psychological distress during the COVID-19 pandemic in Ethiopia: An online cross-sectional study to identify the need for equal attention of intervention. Ann. Gen. Psychiatry 2021, 20, 22. [Google Scholar] [CrossRef]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef]
- Sanchez-Gomez, M.; Giorgi, G.; Finstad, G.L.; Urbini, F.; Foti, G.; Mucci, N.; Zaffina, S.; León-Perez, J.M. COVID-19 Pandemic as a Traumatic Event and Its Associations with Fear and Mental Health: A Cognitive-Activation Approach. Int. J. Environ. Res. Public Health 2021, 18, 7422. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Kunzler, A.M.; Röthke, N.; Günthner, L.; Stoffers-Winterling, J.; Tüscher, O.; Coenen, M.; Rehfuess, E.; Schwarzer, G.; Binder, H.; Schmucker, C.; et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: Systematic review and meta-analyses. Glob. Health 2021, 17, 34. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Nie, P.; Qian, L. Do Quarantine Experiences and Attitudes Towards COVID-19 Affect the Distribution of Mental Health in China? A Quantile Regression Analysis. Appl. Res. Qual. Life 2021, 16, 1925–1942. [Google Scholar] [CrossRef] [PubMed]
- Entringer, T.M.; Kröger, H. Psychische Gesundheit im Zweiten COVID-19 Lockdown in Deutschland. SOEPpapers on Multidisciplinary Panel Data Research No. 1136. 2021. Available online: http://hdl.handle.net/10419/235757 (accessed on 11 June 2022).
- Hettich, N.; Entringer, T.M.; Kroeger, H.; Schmidt, P.; Tibubos, A.N.; Braehler, E.; Beutel, M.E. Impact of the COVID-19 pandemic on depression, anxiety, loneliness, and satisfaction in the German general population: A longitudinal analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2022. [Google Scholar] [CrossRef]
- Entringer, T.M.; Kröger, H.; Schupp, J.; Kühne, S.; Liebig, S.; Goebel, J.; Grabka, M.M.; Graeber, D.; Kroh, M.; Schröder, C.; et al. Psychische Krise Durch COVID-19? Sorgen Sinken, Einsamkeit Steigt, Lebenszufriedenheit Bleibt Stabil. SOEPpapers on Multidisciplinary Panel Data Research No. 1087. 2020. Available online: http://hdl.handle.net/10419/222647 (accessed on 11 June 2022).
- Veer, I.M.; Riepenhausen, A.; Zerban, M.; Wackerhagen, C.; Puhlmann, L.M.C.; Engen, H.; Köber, G.; Bögemann, S.A.; Weermeijer, J.; Uściłko, A.; et al. Psycho-social factors associated with mental resilience in the Corona lockdown. Transl. Psychiatry 2021, 11, 67. [Google Scholar] [CrossRef]
- Welzel, F.D.; Schladitz, K.; Förster, F.; Löbner, M.; Riedel-Heller, S.G. Gesundheitliche Folgen sozialer Isolation: Qualitative Studie zu psychosozialen Belastungen und Ressourcen älterer Menschen im Zusammenhang mit der COVID-19-Pandemie. Bundesgesundheitsblatt Gesundh. Gesundh. 2021, 64, 334–341. [Google Scholar] [CrossRef]
- Liebig, S.; Buchinger, L.; Entringer, T.; Kühne, S. Ost- und Westdeutschland in der Corona-Krise: Nachwendegeneration im Osten erweist sich als resilient. DIW Wochenber. 2020, 38, 721–729. [Google Scholar]
- Hoebel, J.; Haller, S.; Bartig, S.; Michalski, N.; Marquis, A.; Diercke, M.; Schmid-Küpke, N.; Wichmann, O.; Sarma, N.; Schaade, L.; et al. Soziale Ungleichheit und COVID-19 in Deutschland: Wo stehen wir in der vierten Pandemiewelle? Epidemiol. Bull. 2022, 5, 3–10. [Google Scholar]
- Richter, C.; Wächter, M.; Reinecke, J.; Salheiser, A.; Quent, M.; Wjst, M. Politische Raumkultur als Verstärker der Corona-Pandemie? Einflussfaktoren auf die regionale Inzidenzentwicklung in Deutschland in der ersten und zweiten Pandemiewelle 2020. ZRex–Z. Rechtsextremismusforschung 2021, 2, 191–211. [Google Scholar] [CrossRef]
- Spöri, T.; Eichhorn, J. Wer Glaubt an Corona-Verschwörungsmythen. Der Einfluss von Soziodemographie, Politischen Einstellungen und Werthaltungen in Deutschland. Available online: https://dpart.org/wp-content/uploads/2021/03/Corona-Verschw%C3%B6rungsmythen-und-Wertevorstellungen-in-Deutschland.pdf (accessed on 8 June 2022).
- Hettich, N.; Beutel, M.E.; Ernst, M.; Schliessler, C.; Kampling, H.; Kruse, J.; Braehler, E. Conspiracy endorsement and its associations with personality functioning, anxiety, loneliness, and sociodemographic characteristics during the COVID-19 pandemic in a representative sample of the German population. PLoS ONE 2022, 17, e0263301. [Google Scholar] [CrossRef]
- Schließler, C.; Hellweg, N.; Decker, O. Aberglaube, Esotereik und Verschwörungsmentalität in Zeiten der Pandemie. In Autoritäre Dynamiken: Alte Ressentiments-Neue Radikalität/Leipziger Autoritarismus Studie 2020; Decker, O., Brähler, E., Eds.; Psychosozial-Verlag: Gießen, Germany, 2020; pp. 283–308. [Google Scholar]
- Seddig, D.; Maskileyson, D.; Davidov, E.; Ajzen, I.; Schmidt, P. Correlates of COVID-19 vaccination intentions: Attitudes, institutional trust, fear, conspiracy beliefs, and vaccine skepticism. Soc. Sci. Med. 2022, 302, 114981. [Google Scholar] [CrossRef] [PubMed]
- Virchow, F.; Häusler, A. Pandemie-Leugnung und Extreme Rechte in Nordrhein-Westfalen. CoRE-NRW-Kurzgutachten No. 3, Bonn. 2020. Available online: https://www.bicc.de/uploads/tx_bicctools/CoRE_Kurzgutachten3_2020.pdf (accessed on 3 June 2022).
- Spitzer, M. Corona-Leugner und Impfgegner. Nervenheilkunde 2022, 41, 124–134. [Google Scholar] [CrossRef]
- Teufel, M.; Schweda, A.; Dörrie, N.; Musche, V.; Hetkamp, M.; Weismüller, B.; Lenzen, H.; Stettner, M.; Kohler, H.; Bäuerle, A.; et al. Not all world leaders use Twitter in response to the COVID-19 pandemic: Impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J. Public Health 2020, 42, 644–646. [Google Scholar] [CrossRef]
- Oti-Boadi, M.; Malm, E.; Dey, N.E.Y.; Oppong, S. Fear of COVID-19: Psychological distress and coping among university students in Ghana. Curr. Psychol. 2021, 41, 8260–8270. [Google Scholar] [CrossRef] [PubMed]
- Teufel, M.; Schweda, A.; Kohler, H.; Musche, V.; Fink, M.; Weismüller, B.; Moradian, S.; Skoda, E.-M.; Bäuerle, A. Corona doubt and scepticism: Repression and denial as psychological defence mechanisms to process distress? J. Public Health 2021, 43, e520–e522. [Google Scholar] [CrossRef]
- Berth, H.; Förster, P.; Stöbel-Richter, Y.; Balck, F.; Brähler, E. Arbeitslosigkeit und psychische Belastung. Ergebnisse einer Längsschnittstudie 1991 bis 2004. Z. Med. Psychol. 2006, 15, 111–116. [Google Scholar]
- Schneider, J.; Zenger, M.; Brähler, E.; Stöbel-Richter, Y.; Berth, H. Der G-Score–ein Screeninginstrument zur Erfassung der subjektiven körperlichen Gesundheit. Psychother. Psychosom. Med. Psychol. 2018, 68, 361–368. [Google Scholar] [CrossRef]
- Farugie, A.; Heller, A.; Beutel, M.; Tibubos, A.; Brähler, E. Psychische Belastungen in den alten und neuen Bundesländer 30 Jahre nach Mauerfall. Psychiatr. Prax. 2022, 49, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 1998–2017. [Google Scholar]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-offit measures. Methods Psychol. Res. Online 2003, 8, 23–74. [Google Scholar]
- West, S.G.; Taylor, A.B.; Wu, W. Model Fit and Model selection in Structural Equation Modeling. In Handbook of Structural Equation Modeling; Hoyle, R., Ed.; Guilford Press: New York, NY, USA, 2015; pp. 209–231. [Google Scholar]
- Chen, F.; Bollen, K.A.; Paxton, P.; Curran, P.J.; Kirby, J.B. Improper Solutions in Structural Equation Models: Causes, Consequences, and Strategies. Sociol. Methods Res. 2001, 29, 468–508. [Google Scholar] [CrossRef]
- Liu, Y.; Millsap, R.E.; West, S.G.; Tein, J.-Y.; Tanaka, R.; Grimm, K.J. Testing measurement invariance in longitudinal data with ordered-categorical measures. Psychol. Methods 2017, 22, 486–506. [Google Scholar] [CrossRef] [PubMed]
- Muthén, B.; Asparouhov, T. Latent Variable Analysis with Categorical Outcomes: Multiple-Group and Growth Modeling in Mplus. Available online: https://www.statmodel.com/download/webnotes/CatMGLong.pdf (accessed on 20 June 2022).
- Finney, S.J.; DiStefano, C. Non-normal and Categorical data in structural equation modeling. In Structural Equation Modeling: A Second Course; Hancock, G.R., Mueller, R.O., Eds.; Information Age Publishin: Greenwich, CT, USA, 2006; pp. 269–314. [Google Scholar]
- Cheung, G.W.; Rensvold, R.B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- Siflinger, B.; Paffenholz, M.; Seitz, S.; Mendel, M.; Gaudecker, H.M.v. The COVID-19 Pandemic and Mental Health: Disentangling Crucial Channels. ZEW Discussion Papers 21-044. 2021. Available online: https://madoc.bib.uni-mannheim.de/60165/ (accessed on 8 October 2022).
- Bakioğlu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and Positivity: Mediating Role of Intolerance of Uncertainty, Depression, Anxiety, and Stress. Int. J. Ment. Health Addict. 2021, 19, 2369–2382. [Google Scholar] [CrossRef]
- Agha, S. Mental well-being and association of the four factors coping structure model: A perspective of people living in lockdown during COVID-19. Ethics Med. Public Health 2021, 16, 100605. [Google Scholar] [CrossRef]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef]


| Modell | χ2 (df), p-Value | ∆χ2 (df), p-Value | CFI | TLI | RMSEA |
|---|---|---|---|---|---|
| Configural Invariance | 99.306 (90) p = 0.236 | 0.998 | 0.997 | 0.017 | |
| Loading Invariance | 102.508 (96) p = 0.304 | 1.636 (6) p = 0.950 | 0.999 | 0.998 | 0.014 |
| Threshold Invariance | 118.292 (106) p = 0.195 | 17.497 (10) p = 0.064 | 0.998 | 0.997 | 0.018 |
| Unique Factor Invariance | 136.804 (114) p = 0.072 | 16.725 (8) p = 0.033 | 0.995 | 0.995 | 0.024 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khachatryan, K.; Beutel, M.E.; Stöbel-Richter, Y.; Zenger, M.; Berth, H.; Brähler, E.; Schmidt, P. Are Attitudes towards COVID-19 Pandemic Related to Subjective Physical and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 14538. https://doi.org/10.3390/ijerph192114538
Khachatryan K, Beutel ME, Stöbel-Richter Y, Zenger M, Berth H, Brähler E, Schmidt P. Are Attitudes towards COVID-19 Pandemic Related to Subjective Physical and Mental Health? International Journal of Environmental Research and Public Health. 2022; 19(21):14538. https://doi.org/10.3390/ijerph192114538
Chicago/Turabian StyleKhachatryan, Kristine, Manfred E. Beutel, Yve Stöbel-Richter, Markus Zenger, Hendrik Berth, Elmar Brähler, and Peter Schmidt. 2022. "Are Attitudes towards COVID-19 Pandemic Related to Subjective Physical and Mental Health?" International Journal of Environmental Research and Public Health 19, no. 21: 14538. https://doi.org/10.3390/ijerph192114538
APA StyleKhachatryan, K., Beutel, M. E., Stöbel-Richter, Y., Zenger, M., Berth, H., Brähler, E., & Schmidt, P. (2022). Are Attitudes towards COVID-19 Pandemic Related to Subjective Physical and Mental Health? International Journal of Environmental Research and Public Health, 19(21), 14538. https://doi.org/10.3390/ijerph192114538






