Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Selection of Subjects
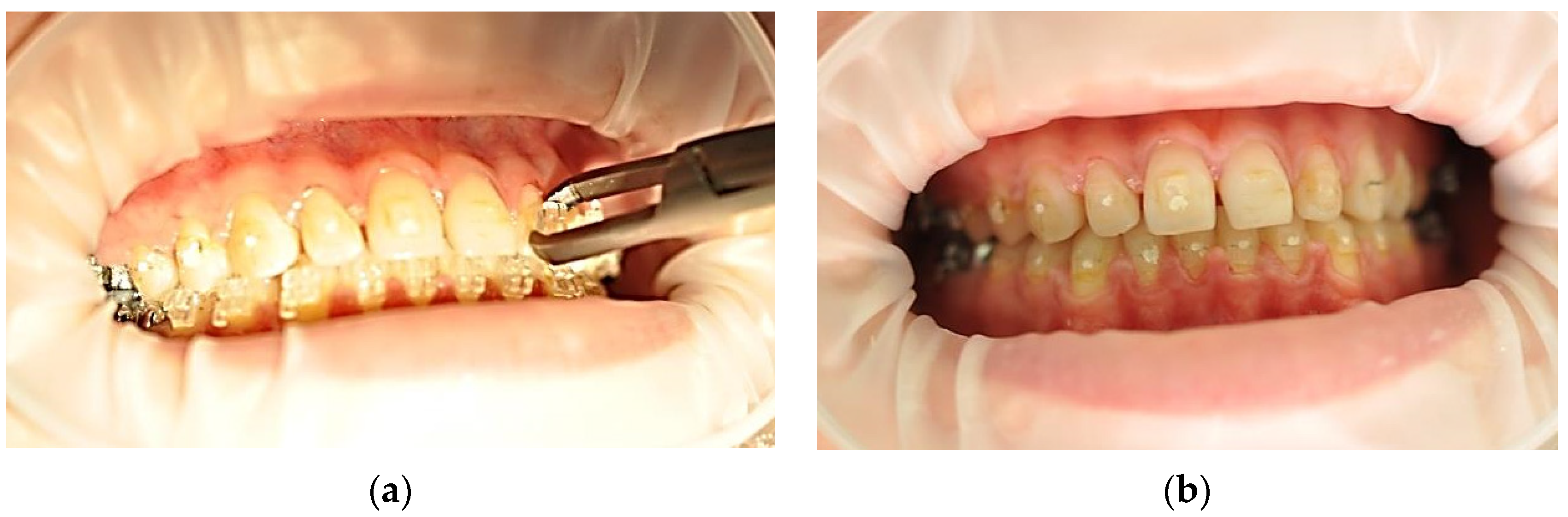
2.3. Debonding Systems
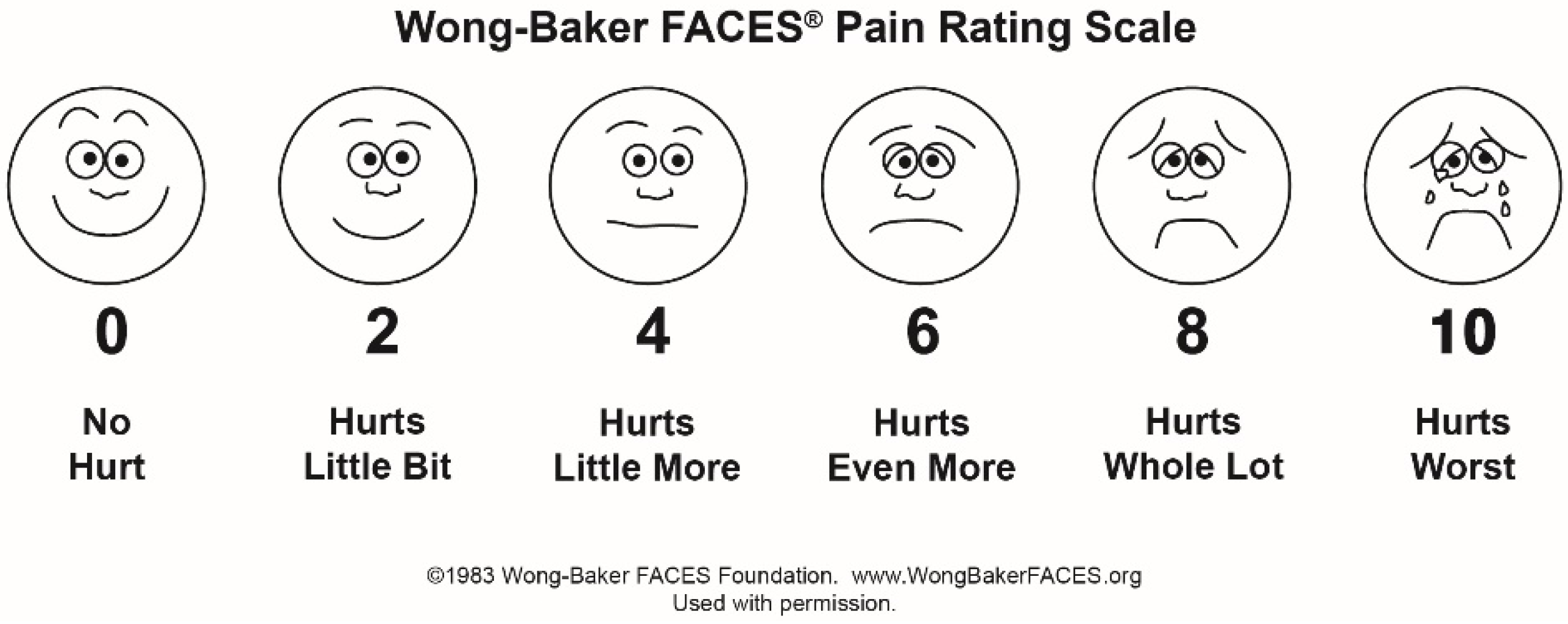
2.4. Evaluating the Therapeutic Response
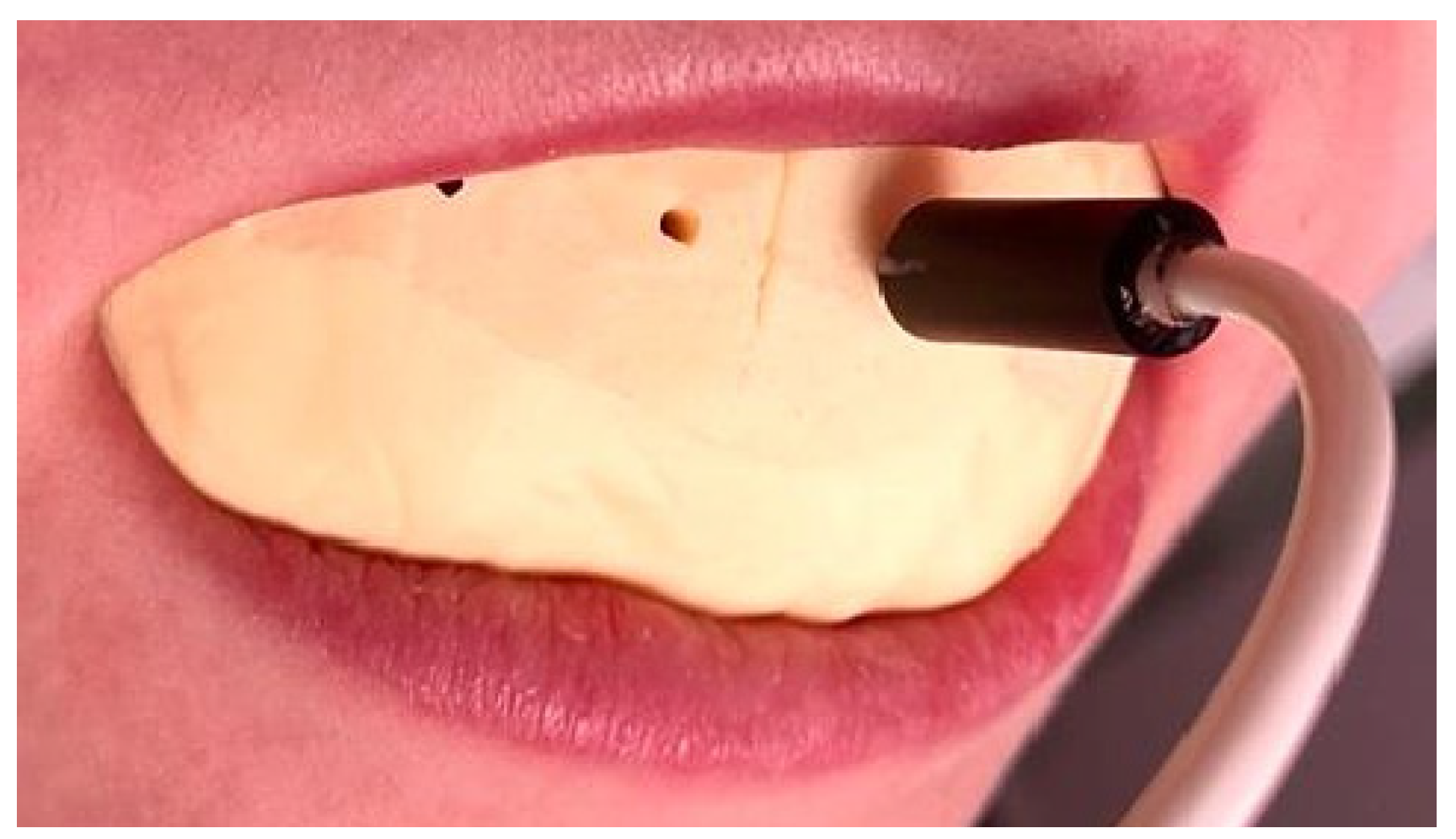
2.5. The Working Technique
2.6. Data Analysis
2.6.1. Analysis of the Wong–Baker Pain Rating Scale Pain Scores
2.6.2. Analysis of the Working Time
2.6.3. Analysis of the Laser Doppler Flowmetry Measurements
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of variance |
| ICC | Intra-class correlation coefficient |
| LDF | laser Doppler flowmetry |
| M | mean |
| MDC | mean detectable change |
| Er:YAG | erbium-doped yttrium aluminum garnet; Er: Y3Al5O12 |
| PI | pain intensity |
| PU | perfusion units |
| SD | standard deviation |
| VSP | Very short pulse |
References
- Maiman, T.H. Stimulated Optical Radiation in Ruby. Nature 1960, 187, 493–494. [Google Scholar] [CrossRef]
- Fornaini, C.; Fekrazad, R.; Rocca, J.P.; Zhang, S.; Merigo, E. Use of Blue and Blue-Violet Lasers in Dentistry: A Narrative Review. J. Lasers Med. Sci. 2021, 12, e31. [Google Scholar] [CrossRef]
- Serban, C.; Lungeanu, D.; Bota, S.D.; Cotca, C.C.; Negrutiu, M.L.; Duma, V.F.; Sinescu, C.; Craciunescu, E.L. Emerging Technologies for Dentin Caries Detection—A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 674. [Google Scholar] [CrossRef] [PubMed]
- Pagano, S.; Lombardo, G.; Orso, M.; Abraha, I.; Capobianco, B.; Cianetti, S. Lasers to prevent dental caries: A systematic review. BMJ Open 2020, 10, e038638. [Google Scholar] [CrossRef] [PubMed]
- Cronshaw, M.; Parker, S.; Anagnostaki, E.; Mylona, V.; Lynch, E.; Grootveld, M. Photobiomodulation Dose Parameters in Dentistry: A Systematic Review and Meta-Analysis. Dent. J. 2020, 8, 114. [Google Scholar] [CrossRef] [PubMed]
- Tzanakakis, E.C.; Skoulas, E.; Pepelassi, E.; Koidis, P.; Tzoutzas, I.G. The Use of Lasers in Dental Materials: A Review. Materials 2021, 14, 3370. [Google Scholar] [CrossRef]
- Yavagal, C.M.; Matondkar, S.P.; Yavagal, P.C. Efficacy of Laser Photobiomodulation in Accelerating Orthodontic Tooth Movement in Children: A Systematic Review with Meta-analysis. Int. J. Clin. Pediatr. Dent. 2021, 14, S94–S100. [Google Scholar] [CrossRef]
- Sobouti, F.; Aryana, M.; Dadgar, S.; Alizadeh Navaei, R.; Rakhshan, V. Effects of Novel versus Conventional Porcelain Surface Treatments on Shear Bond Strength of Orthodontic Brackets: A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2022, 2022, 8246980. [Google Scholar] [CrossRef]
- Mesaroș, A.; Mesaroș, M.; Buduru, S. Orthodontic Bracket Removal Using LASER-Technology—A Short Systematic Literature Review of the Past 30 Years. Materials 2022, 15, 548. [Google Scholar] [CrossRef]
- Cochrane, N.J.; Lo, T.W.G.; Adams, G.G.; Schneider, P.M. Quantitative analysis of enamel on debonded orthodontic brackets. Am. J. Orthod. Dentofacial. Orthop. 2017, 152, 312–319. [Google Scholar] [CrossRef]
- Hoteit, M.; Nammour, S.; Zeinoun, T. Evaluation of Enamel Topography after Debonding Orthodontic Ceramic Brackets by Different Er,Cr:YSGG and Er:YAG Lasers Settings. Dent. J. 2020, 8, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalil, A.S.; Tamish, N.M.; Elkalza, A.R. Assessment of chemical, ultrasonic, diode laser and Er:YAG laser application on debonding of ceramic brackets. BMC Oral Health 2022, 22, 79. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.; Rahman, N.A.; Alam, M.K. Comparison of Orthodontic Bracket Debonding Force and Bracket Failure Pattern on Different Teeth In Vivo by a Prototype Debonding Device. Biomed. Res. Int. 2021, 2021, 6663683. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Matys, J.; Żmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Brugnera Junior, A.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Nalbantgil, D.; Tozlu, M.; Oztoprak, M.O. Comparison of Different Energy Levels of Er:YAG Laser Regarding Intrapulpal Temperature Change during Safe Ceramic Bracket Removal. Photomed. Laser Surg. 2018, 36, 209–213. [Google Scholar] [CrossRef]
- Reza, F.; Kalhori, A.M.; Farzaneh, A.; Katayoun, K.A.M.; Nikoo, T. Laser in Orthodontics; IntechOpen: London, UK, 2011. [Google Scholar] [CrossRef] [Green Version]
- Lam, R.; Goonewardene, M.S.; Naoum, S. Pulp blood flow and sensibility in patients with a history of dental trauma undergoing maxillary expansion. Angle Orthod. 2020, 90, 695–701. [Google Scholar] [CrossRef]
- Miron, M.; Lungeanu, D.; Ciora, E.; Ogodescu, E.; Todea, C. Using Laser-Doppler Flowmetry to Evaluate the Therapeutic Response in Dentin Hypersensitivity. Int. J. Environ. Res. Public Health 2020, 17, 8787. [Google Scholar] [CrossRef]
- Lesaffre, E.; Philstrom, B.; Needleman, I.; Worthington, H. The design and analysis of split-mouth studies: What statisticians and clinicians should know. Stat. Med. 2009, 28, 3470–3482. [Google Scholar] [CrossRef]
- Karcioglu, O.; Topacoglu, H.; Dikme, O.; Dikme, O. A systematic review of the pain scales in adults: Which to use? Am. J. Emerg. Med. 2018, 36, 707–714. [Google Scholar] [CrossRef]
- Rocha, M.O.C.; Cruz, A.A.C.F.; Santos, D.O.; Douglas-De-Oliveira, D.W.; Flecha, O.D.; Gonçalves, P.F. Sensitivity and specificity of assessment scales of dentin hypersensitivity—An accuracy study. Braz. Oral Res. 2020, 34, e043. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Anwer, S.; Iqbal, A.; Iqbal, Z.A. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating and verbal rating scales for measurement of osteoarthritic knee pain. J. Pain Res. 2018, 11, 851–856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marilyn, J.H.; David, W. (Eds.) Pain Assessment and Management. In Wong’s Nursing Care of Infants and Children, 10th ed.; Mosby: Maryland Heights, MO, USA, 2015; Chapter 5; ISBN 9780323222419. [Google Scholar]
- Adeboye, A.; Hart, R.; Senapathi, S.H.; Ali, N.; Holman, L.; Thomas, H.W. Assessment of Functional Pain Score by Comparing to Traditional Pain Scores. Cureus 2021, 13, e16847. [Google Scholar] [CrossRef] [PubMed]
- Ghouth, N.; Duggal, M.S.; BaniHani, A.; Nazzal, H. The diagnostic accuracy of laser Doppler flowmetry in assessing pulp blood flow in permanent teeth: A systematic review. Dent. Traumatol. 2018, 34, 311–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lima, T.F.R.; Dos Santos, S.L.; da Silva Fidalgo, T.K.; Silva, E.J.N.L. Vitality Tests for Pulp Diagnosis of Traumatized Teeth: A Systematic Review. J. Endod. 2019, 45, 490–499. [Google Scholar] [CrossRef] [PubMed]
- Todea, C.; Cânjau, S.; Miron, M.; Vitez, B.; Noditi, G. Laser Doppler flowmetry evaluation of the microcirculation in dentistry. In Microcirculation Revisited—From Molecules to Clinical Practice; Lenasi, H., Ed.; InTech: London, UK, 2016; pp. 203–230. ISBN 9789535127314. [Google Scholar]
- Miron, M.I.; Dodenciu, D.; Sârbescu, P.F.; Filip, L.; Balabuc, C.A.; Hanigovski, E.; Todea, C. Optimization of the laser Doppler signal acquisition technique in pulp vitality tests. Arch. Balk. Med. Union 2011, 46, 280–284. [Google Scholar]
- Salles, A.W.; Salles, A.M.; Nogueira, G.E. Laser Doppler Blood-Flow Signals from Human Teeth during an Alignment and Leveling Movement Using a Superelastic Archwire. ISRN Dent. 2013, 2013, 102816. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Nanda, R.S.; Kawata, T. Effect of orthodontic forces on blood flow in human gingiva. Angle Orthod. 1991, 61, 193–203. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Nanda, R.S. Blood flow changes in gingival tissues due to the displacement of teeth. Angle Orthod. 1992, 62, 257–264. [Google Scholar] [CrossRef]
- Hossaini, S.; Bahador, A. Application of the high intensity laser therapies on ceramic brakets debonding: A literature review. Ann. Dent. Spec. 2018, 1, 363–366. [Google Scholar]
- Tozlu, M.; Oztoprak, M.O.; Arun, T. Comparison of shear bond strengths of ceramic brackets after different time lags between lasing and debonding. Lasers Med. Sci. 2012, 27, 1151–1155. [Google Scholar] [CrossRef]
- Kim, W.T.; Bayome, M.; Park, J.B.; Park, J.H.; Baek, S.H.; Kook, Y.A. Effect of frequent laser irradiation on orthodontic pain. Angle Orthod. 2013, 83, 611–616. [Google Scholar] [CrossRef]
- Hoteit, M.; Nammour, S.; Zeinoun, T. Assessment of microcracks and shear bond strength after debonding orthodontic ceramic brackets on enamel priorly etched by different Er,Cr:YSGG and Er:YAG laser settings without acid application: An in vitro study. Int. Orthod. 2019, 17, 744–757. [Google Scholar] [CrossRef] [PubMed]
- Ghouth, N.; Duggal, M.S.; Kang, J.; Nazzal, H. A Diagnostic Accuracy Study of Laser Doppler Flowmetry for the Assessment of Pulpal Status in Children’s Permanent Incisor Teeth. J. Endod. 2019, 45, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Miron, M.I.; Dodenciu, D.; Sarbescu, P.; Canjau, S.; Ardelean, L.; Rusu, L.C.; Todea, C. Condensation silicones and light-curing resin used within a laser Doppler pulp vitality testing method. Mater. Plast. 2012, 49, 171–175. [Google Scholar]
- Todea, C.; Canjau, S.; Dodenciu, D.; Miron, M.I.; Tudor, A.; Bălăbuc, C. Laser Doppler flowmetry evaluation of gingival recovery response after laser treatment Head and Neck Optical diagnostics. In SPIE Proceedings; Optica Publishing Group: Washington, DC, USA, 2013; p. 880508. [Google Scholar] [CrossRef]
- Canjau, S.; Miron, M.I.; Todea, C.D. Laser Doppler flowmetry evaluation of gingival microcirculation recovery in gingivitis. Arch. Balk. Med. Union 2015, 50, 354–359. [Google Scholar]
- Noditi, G.; Todea, C. Laser Doppler imaging—As a non-invasive method for assesing regional microcirculation when using plastic materials for guided healing. Mater. Plast. 2013, 1, 40–43. [Google Scholar]
- Sant’Anna, E.F.; Araújo, M.T.S.; Nojima, L.I.; Cunha, A.C.D.; Silveira, B.L.D.; Marquezan, M. High- intensity laser application in Orthodontics. Dent. Press J. Orthod. 2017, 22, 99–109. [Google Scholar] [CrossRef] [Green Version]
- Dumbryte, I.; Jonavicius, T.; Linkeviciene, L.; Linkevicius, T.; Peciuliene, V.; Malinauskas, M. The prognostic value of visually assessing enamel microcracks: Do debonding and adhesive removal contribute to their increase? Angle Orthod. 2016, 86, 437–447. [Google Scholar] [CrossRef]
- Heidari, S.; Torkan, S. Laser applications in orthodontics. J. Lasers Med. Sci. 2013, 4, 151–158. [Google Scholar]




| Laser Er:YAG-Assisted a | Conventional a | p-Value a | |
|---|---|---|---|
| M ± SD | 0.47 ± 0.86 | 3.07 ± 1.46 | <0.001 ** |
| Laser Er:YAG-Assisted a | Conventional a | p-Value a | |
|---|---|---|---|
| M ± SD | 0.94 ± 0.25 | 1.64 ± 0.57 | <0.001 ** |
| Difference between paired teeth: −0.697 ± 0.703; 95% CI (−0.959; −0.434) | |||
| Time of Measurements | Laser Er:YAG-Assisted a | Conventional a | Two-Way ANOVA |
|---|---|---|---|
| Before debonding | 11.49 ± 2.66 | 12.26 ± 2.76 | Model: p < 0.160 |
| PatientID: p < 0.024 * | |||
| Treatment: p = 0.243 | |||
| After debonding | 12.56 ± 3.94 | 12.10 ± 3.90 | Model: p < 0.224 |
| PatientID: p < 0.289 | |||
| Treatment: p = 0.628 | |||
| 7 days after debonding | 16.27 ± 5.56 | 14.89 ± 4.39 | Model: p < 0.044 * |
| PatientID: p < 0.017 * | |||
| Treatment: p = 0.233 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mocuta, D.-E.; Miron, M.I.; Lungeanu, D.; Mateas, M.; Ogodescu, E.; Todea, C.D. Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets. Int. J. Environ. Res. Public Health 2022, 19, 14564. https://doi.org/10.3390/ijerph192114564
Mocuta D-E, Miron MI, Lungeanu D, Mateas M, Ogodescu E, Todea CD. Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets. International Journal of Environmental Research and Public Health. 2022; 19(21):14564. https://doi.org/10.3390/ijerph192114564
Chicago/Turabian StyleMocuta, Daliana-Emanuela, Mariana I. Miron, Diana Lungeanu, Marius Mateas, Emilia Ogodescu, and Carmen D. Todea. 2022. "Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets" International Journal of Environmental Research and Public Health 19, no. 21: 14564. https://doi.org/10.3390/ijerph192114564
APA StyleMocuta, D.-E., Miron, M. I., Lungeanu, D., Mateas, M., Ogodescu, E., & Todea, C. D. (2022). Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets. International Journal of Environmental Research and Public Health, 19(21), 14564. https://doi.org/10.3390/ijerph192114564









