Telemedicine Interventions as an Attempt to Improve the Mental Health of Populations during the COVID-19 Pandemic—A Narrative Review
Abstract
:1. Introduction
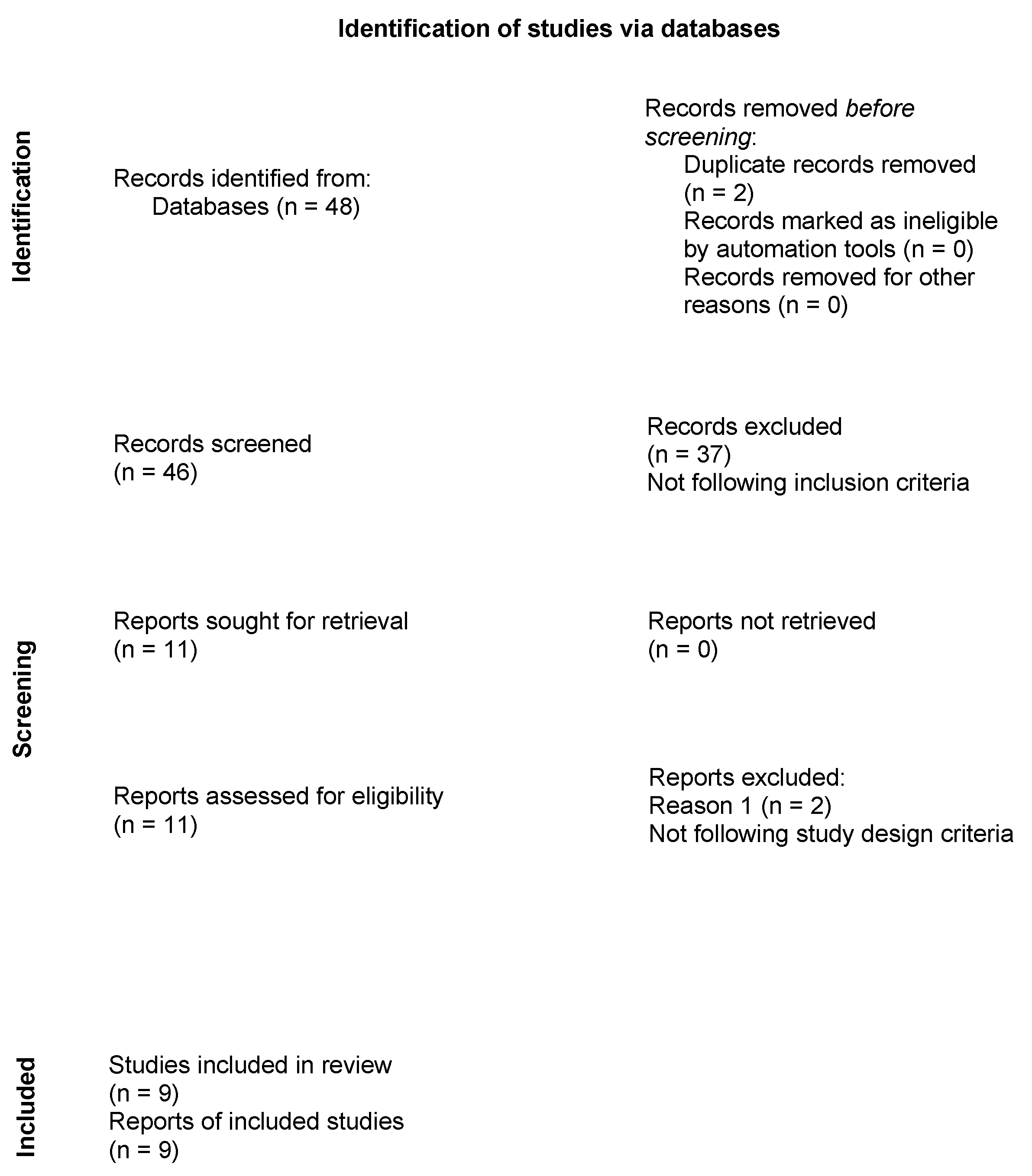
2. Materials and Methods
2.1. Electronic Searches
2.2. Assessment of Methodological Quality
3. Results
3.1. Characteristics of Included Studies
3.1.1. Internet-Based Intervention
3.1.2. Mobile-Based Intervention
3.1.3. Real-Time Video or Phone Call
3.2. Assessment of Methodological Quality
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alshaeri, H.K.; Natto, Z.S. A contemporary look at COVID-19 medications: Available and potentially effective drugs. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9188–9195. [Google Scholar] [CrossRef] [PubMed]
- Rutkowska, A.; Kacperak, K.; Rutkowski, S.; Cacciante, L.; Kiper, P.; Szczegielniak, J. The Impact of Isolation Due to COVID-19 on Physical Activity Levels in Adult Students. Sustainability 2021, 13, 446. [Google Scholar] [CrossRef]
- Wilke, J.; Mohr, L.; Tenforde, A.S.; Edouard, P.; Fossati, C.; Gonzalez-Gross, M.; Sanchez Ramirez, C.; Laino, F.; Tan, B.; Pillay, J.D.; et al. A Pandemic within the Pandemic? Physical Activity Levels Substantially Decreased in Countries Affected by COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2235. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Despres, J.P. Physical Activity, Sedentary Behaviours, and Cardiovascular Health: When Will Cardiorespiratory Fitness Become a Vital Sign? Can. J. Cardiol. 2016, 32, 505–513. [Google Scholar] [CrossRef]
- Jingjie, W.; Yang, L.; Jing, Y.; Ran, L.; Yiqing, X.; Zhou, N. Sedentary time and its association with risk of cardiovascular diseases in adults: An updated systematic review and meta-analysis of observational studies. BMC Public Health 2022, 22, 286. [Google Scholar] [CrossRef]
- Compernolle, S.; DeSmet, A.; Poppe, L.; Crombez, G.; De Bourdeaudhuij, I.; Cardon, G.; van der Ploeg, H.P.; Van Dyck, D. Effectiveness of interventions using self-monitoring to reduce sedentary behavior in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 63. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. S3), 1–72. [Google Scholar] [CrossRef] [Green Version]
- Martin, A.; Fitzsimons, C.; Jepson, R.; Saunders, D.H.; van der Ploeg, H.P.; Teixeira, P.J.; Gray, C.M.; Mutrie, N.; Euro, F.I.T.c. Interventions with potential to reduce sedentary time in adults: Systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1056–1063. [Google Scholar] [CrossRef] [Green Version]
- Gardner, B.; Smith, L.; Lorencatto, F.; Hamer, M.; Biddle, S.J. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol. Rev. 2016, 10, 89–112. [Google Scholar] [CrossRef]
- Galper, D.I.; Trivedi, M.H.; Barlow, C.E.; Dunn, A.L.; Kampert, J.B. Inverse association between physical inactivity and mental health in men and women. Med. Sci. Sports Exerc. 2006, 38, 173–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denche-Zamorano, A.; Franco-Garcia, J.M.; Carlos-Vivas, J.; Mendoza-Munoz, M.; Pereira-Payo, D.; Pastor-Cisneros, R.; Merellano-Navarro, E.; Adsuar, J.C. Increased Risks of Mental Disorders: Youth with Inactive Physical Activity. Healthcare 2022, 10, 237. [Google Scholar] [CrossRef]
- Falck, R.S.; Davis, J.C.; Liu-Ambrose, T. What is the association between sedentary behaviour and cognitive function? A systematic review. Br. J. Sports Med. 2017, 51, 800–811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saunders, T.J.; McIsaac, T.; Douillette, K.; Gaulton, N.; Hunter, S.; Rhodes, R.E.; Prince, S.A.; Carson, V.; Chaput, J.-P.; Chastin, S.; et al. Sedentary behaviour and health in adults: An overview of systematic reviews. Appl. Physiol. Nutr. Metab. 2020, 45, S197–S217. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.J.; Alrawili, A.S.; Alkhawaja, F.Z. The Anxiety and Stress of the Public during the Spread of Novel Coronavirus (COVID-19). J. Pharm. Res. Int. 2020, 32, 54–59. [Google Scholar] [CrossRef]
- Baliyan, S.; Cimadevilla, J.M.; de Vidania, S.; Pulopulos, M.M.; Sandi, C.; Venero, C. Differential susceptibility to the impact of the COVID-19 pandemic on working memory, empathy, and perceived stress: The role of cortisol and resilience. Brain Sci. 2021, 11, 348. [Google Scholar] [CrossRef]
- Elhusseiny, K.M.; Abd-Elhay, F.A.E.; Kamel, M.G. Possible therapeutic agents for COVID-19: A comprehensive review. Expert Rev. Anti-Infect. Ther. 2020, 18, 1005–1020. [Google Scholar] [CrossRef]
- Đogaš, Z.; Kalcina, L.L.; Dodig, I.P.; Demirović, S.; Madirazza, K.; Valić, M.; Pecotić, R. The effect of COVID-19 lockdown on lifestyle and mood in Croatian general population: A cross-sectional study. Croat. Med. J. 2020, 61, 309–318. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Rutkowska, A.; Liska, D.; Cieslik, B.; Wrzeciono, A.; Brodani, J.; Barcalova, M.; Gurin, D.; Rutkowski, S. Stress Levels and Mental Well-Being among Slovak Students during e-Learning in the COVID-19 Pandemic. Healthcare 2021, 9, 1356. [Google Scholar] [CrossRef]
- Paczkowska, A.; Nowakowska, E.; Michalska, J.; Ficner, H.; Tyrchniewicz, J.; Szymański, A.; Wańkowicz, K.; Namyślak, K.; Gala, A.; Sulimiera Michalak, S.; et al. Impact of the COVID-19 pandemic and lockdown on mental health among the general population in Poland and on the availability of psychological support. Psychol. Health Med. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rutkowska, A.; Cieślik, B.; Tomaszczyk, A.; Szczepańska-Gieracha, J. Mental Health Conditions among E-Learning Students during the COVID-19 Pandemic. Front. Public Health 2022, 10, 871934. [Google Scholar] [CrossRef] [PubMed]
- Thakur, V.; Jain, A. COVID 2019-suicides: A global psychological pandemic. Brain Behav. Immun. 2020, 88, 952–953. [Google Scholar] [CrossRef] [PubMed]
- Shirotsuki, K.; Sugaya, N.; Nakao, M. Descriptive review of internet-based cognitive behavior therapy on anxiety-related problems in children under the circumstances of COVID-19. Biopsychosoc. Med. 2022, 16, 3. [Google Scholar] [CrossRef]
- Holst, A.; Nejati, S.; Bjorkelund, C.; Eriksson, M.C.; Hange, D.; Kivi, M.; Wikberg, C.; Petersson, E.L. Patients’ experiences of a computerised self-help program for treating depression—A qualitative study of Internet mediated cognitive behavioural therapy in primary care. Scand. J. Prim. Health Care 2017, 35, 46–53. [Google Scholar] [CrossRef] [Green Version]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [Green Version]
- Foley, N.C.; Teasell, R.W.; Bhogal, S.K.; Speechley, M.R. Stroke rehabilitation evidence-based review: Methodology. Top. Stroke Rehabil. 2003, 10, 1–7. [Google Scholar] [CrossRef]
- Comer, J.S.; Furr, J.M.; Del Busto, C.; Silva, K.; Hong, N.; Poznanski, B.; Sanchez, A.; Cornacchio, D.; Herrera, A.; Coxe, S.; et al. Therapist-Led, Internet-Delivered Treatment for Early Child Social Anxiety: A Waitlist-Controlled Evaluation of the iCALM Telehealth Program. Behav. Ther. 2021, 52, 1171–1187. [Google Scholar] [CrossRef]
- Rachamim, L.; Zimmerman-Brenner, S.; Rachamim, O.; Mualem, H.; Zingboim, N.; Rotstein, M. Internet-based guided self-help comprehensive behavioral intervention for tics (ICBIT) for youth with tic disorders: A feasibility and effectiveness study with 6 month-follow-up. Eur. Child Adolesc. Psychiatry 2022, 31, 275–287. [Google Scholar] [CrossRef]
- Wagner, L.I.; Tooze, J.A.; Hall, D.L.; Levine, B.J.; Beaumont, J.; Duffecy, J.; Victorson, D.; Gradishar, W.; Leach, J.; Saphner, T.; et al. Targeted eHealth Intervention to Reduce Breast Cancer Survivors’ Fear of Recurrence: Results From the FoRtitude Randomized Trial. J. Natl. Cancer Inst. 2021, 113, 1495–1505. [Google Scholar] [CrossRef]
- Anthony, C.A.; Rojas, E.; Glass, N.; Keffala, V.; Noiseux, N.; Elkins, J.; Brown, T.S.; Bedard, N.A. A Psycholgical Intervention Delivered by Automated Mobile Phone Messaging Stabilized Hip and Knee Function During the COVID-19 Pandemic: A Randomized Controlled Trial. J. Arthroplast. 2022, 37, 431–437.e433. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Lin, D.; Goldberg, S.; Shen, Z.; Chen, P.; Qiao, S.; Brewer, J.; Loucks, E.; Operario, D. A mindfulness-based mobile health (mHealth) intervention among psychologically distressed university students in quarantine during the COVID-19 pandemic: A randomized controlled trial. J. Couns. Psychol. 2022, 69, 157–171. [Google Scholar] [CrossRef] [PubMed]
- Al-Alawi, M.; McCall, R.K.; Sultan, A.; Al Balushi, N.; Al-Mahrouqi, T.; Al Ghailani, A.; Al Sabti, H.; Al-Maniri, A.; Panchatcharam, S.M.; Al Sinawi, H. Efficacy of a Six-Week-Long Therapist-Guided Online Therapy Versus Self-help Internet-Based Therapy for COVID-19-Induced Anxiety and Depression: Open-label, Pragmatic, Randomized Controlled Trial. JMIR Ment. Health 2021, 8, e26683. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, A.L.; Simpson, K.M.; Salisbury, M.R.; Bobula, J.; Penner-Goeke, L.; Berard, L.; Rioux, C.; Giesbrecht, G.F.; Giuliano, R.; Lebel, C.; et al. Building Emotional Awareness and Mental Health (BEAM): A Pilot Randomized Controlled Trial of an App-Based Program for Mothers of Toddlers. Front. Psychiatry 2022, 13, 880972. [Google Scholar] [CrossRef] [PubMed]
- Policarpo, S.; Machado, M.V.; Cortez-Pinto, H. Telemedicine as a tool for dietary intervention in NAFLD-HIV patients during the COVID-19 lockdown: A randomized controlled trial. Clin. Nutr. ESPEN 2021, 43, 329–334. [Google Scholar] [CrossRef]
- Prato, A.; Maugeri, N.; Chiarotti, F.; Morcaldi, L.; Vicario, C.M.; Barone, R.; Rizzo, R. A Randomized Controlled Trial Comparing Videoconference vs. Face-to-Face Delivery of Behavior Therapy for Youths with Tourette Syndrome in the Time of COVID-19. Front. Psychiatry 2022, 13, 862422. [Google Scholar] [CrossRef]
- Saunders, E.C.; Moore, S.K.; Gardner, T.; Farkas, S.; Marsch, L.A.; McLeman, B.; Meier, A.; Nesin, N.; Rotrosen, J.; Walsh, O.; et al. Screening for Substance Use in Rural Primary Care: A Qualitative Study of Providers and Patients. J. Gen. Intern. Med. 2019, 34, 2824–2832. [Google Scholar] [CrossRef]
- Bashshur, R.L.; Shannon, G.W.; Bashshur, N.; Yellowlees, P.M. The Empirical Evidence for Telemedicine Interventions in Mental Disorders. Telemed. J. E-Health 2016, 22, 87–113. [Google Scholar] [CrossRef] [Green Version]
- Rutkowski, S. Management Challenges in Chronic Obstructive Pulmonary Disease in the COVID-19 Pandemic: Telehealth and Virtual Reality. J. Clin. Med. 2021, 10, 1261. [Google Scholar] [CrossRef]
- Komariah, M.; Amirah, S.; Faisal, E.G.; Prayogo, S.A.; Maulana, S.; Platini, H.; Suryani, S.; Yosep, I.; Arifin, H. Efficacy of Internet-Based Cognitive Behavioral Therapy for Depression and Anxiety among Global Population during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis of a Randomized Controlled Trial Study. Healthcare 2022, 10, 1224. [Google Scholar] [CrossRef]
- Olthuis, J.V.; Watt, M.C.; Bailey, K.; Hayden, J.A.; Stewart, S.H. Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst. Rev. 2016, 3, CD011565. [Google Scholar] [CrossRef] [PubMed]
- Berryhill, M.B.; Halli-Tierney, A.; Culmer, N.; Williams, N.; Betancourt, A.; King, M.; Ruggles, H. Videoconferencing psychological therapy and anxiety: A systematic review. Fam. Pract. 2018, 36, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Videoconferencing Psychotherapy and Depression: A Systematic Review. Telemed. E-Health 2019, 25, 435–446. [CrossRef] [PubMed]
- Currie, C.L.; Larouche, R.; Voss, M.L.; Trottier, M.; Spiwak, R.; Higa, E.; Scott, D.R.; Tallow, T. Effectiveness of Live Health Professional-Led Group eHealth Interventions for Adult Mental Health: Systematic Review of Randomized Controlled Trials. J. Med. Internet Res. 2022, 24, e27939. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Hamatani, S.; Shimizu, E. Effectiveness of Videoconference-Delivered Cognitive Behavioral Therapy for Adults With Psychiatric Disorders: Systematic and Meta-Analytic Review. J. Med. Internet Res. 2021, 23, e31293. [Google Scholar] [CrossRef] [PubMed]
- Evans, K.; Rennick-Egglestone, S.; Cox, S.; Kuipers, Y.; Spiby, H. Remotely Delivered Interventions to Support Women With Symptoms of Anxiety in Pregnancy: Mixed Methods Systematic Review and Meta-analysis. J. Med. Internet Res. 2022, 24, e28093. [Google Scholar] [CrossRef]
- Singleton, A.C.; Raeside, R.; Hyun, K.K.; Partridge, S.R.; Di Tanna, G.L.; Hafiz, N.; Tu, Q.; Tat-Ko, J.; Sum, S.C.M.; Sherman, K.A.; et al. Electronic Health Interventions for Patients With Breast Cancer: Systematic Review and Meta-Analyses. J. Clin. Oncol. 2022, 40, 2257–2270. [Google Scholar] [CrossRef]
- Drissi, N.; Ouhbi, S.; Marques, G.; de la Torre Díez, I.; Ghogho, M.; Janati Idrissi, M.A. A Systematic Literature Review on e-Mental Health Solutions to Assist Health Care Workers during COVID-19. Telemed. J. E-Health 2021, 27, 594–602. [Google Scholar] [CrossRef]
| Authors, Year, Study Design | Study Location | Recruitment | Sample Size | Mean Age | Participants Characteristics | Intervention | Frequency | Assessment | Effects |
|---|---|---|---|---|---|---|---|---|---|
| Al-Alawi (2021) et al. RCT | Oman | Recruitment was based on an online survey. The research team contacted eligible participants by email | 46 Adults: 36 Female, 10 Male | 28.5 | Individuals with depression and anxiety. Participants were mostly singles and completed education up to the college level. The majority were self-quarantining. | iCBT | 6 sessions | PHQ-9, GAD-7 | Online therapist-guided therapy led to a significant reduction in psychological distress. Both GAD-7 and PHG-9 scores in the intervention group were more reduced than in the control group |
| Anthony (2022) et al. RCT | United States | Recruitment was based on a phone call among patients on the waiting list for surgery | 90 Adults: 35.5% Female, 64.5% Male | 64 | Patients scheduled for ATH or TKA who experienced a surgical delay due to the COVID-19 pandemic. Participants presented minimal to severe levels of anxiety regarding becoming infected with COVID-19 | ACT | Twice a day text messages communicating an ACT-based intervention for 14 days | PROM MH, PROM PH, HOOS JR, KOOS JR | An automated mobile phone ACT’S messages can prevent clinically significant decline, and improve physical function and joint-specific PROMs in patients who experience a surgical delay |
| Comer (2021) et al. RCT | United States | Recruitment was based on a phone call, REDCap survey, and/or videoconferencing among caregivers of children registering for university-affiliated child mental health centre | 40 Children: 72.5% Female 27.5% Male | 6.2 | Children with social anxiety disorder. The majority was a racial minority. Over half of the caregivers were born outside of the United States. | iCALM Telehealth Program | 16-weeks remotely delivered treatment | CBCL, CBQ, CAIS, DASS | iCALM led to significantly greater reductions than waitlist in child anxiety symptoms, fear, discomfort, and anxiety-related social impairment, and greater improvements in child soothability. |
| MacKinnon (2022) et al. RCT | Canada | Recruitment was based on an online advertisement on social media, likewise postings by community partner agencies via electronic mailing lists or public announcements. | 65 Adults: 100% Female | 33.8 | Mothers of toddlers with moderate-to-severe depression | BEAM | 10-week app-based digital intervention | PHQ-9, PSI-SF, GAD-7, PROMIS | The BEAM group revealed greater reductions in overall mental health problems, specifically anxiety and sleep symptoms, compared to control group. |
| Policarpo (2021) et al. RCT | Portugal | Recruitment was conducted among patients from an outpatient clinic | 55 Adults: 15 Females 40 Males | 54.2 | Patients diagnosed with NAFLD-HIV, receiving dietary recommendations or for structured dietary intervention | Video and/or telephone interview | 3-months follow-up | Body composition, dietary and lifestyle behaviours | The application of remote maintenance of dietary intervention can mitigate the change in eating habits and physical activity pattern, preventing significant weight gain. |
| Prato (2022) et al. RCT | Italy | Recruitment was conducted among patients from an outpatient clinic | 40 Youths: 4 Females 36 Males | 13.5 | Youth patients with Tourette Syndrome | Videoconferencing behaviour therapy | 8 weekly sessions | YGTSS, PUTS, WISC-IV, YGTSS, CY-BOCS, MASC, PUTS, CDI, CPRS | Online remote and face-to-face behaviour therapy are equally effective in the treatment of severity of tics, obsessive-compulsive symptoms, and anxiety symptoms. Yet remote therapy was more effective for reducing depressive symptoms |
| Rachamim (2022) et al. cross-over study | Israel | Recruitment was based on a phone call with child’s parent, among proteges of children’s hospital, medical centre and local association | 41 Youths: 12 Females 29 Males | 11.2 | Children and adolescents with tic disorders | iCBIT | 9-week program | YGTSS, CGI-I, CGAS | Adolescents using iCBIT experienced improvements in self-esteem and comorbidities. A high retention rate (92%) was noted. |
| Sun (2022) et al. RCT | China | Recruitment was based on online WeChat-based flyers and websites targeting college students | 114 Students: 73% Female 27% Male | 22.2 | University students with depression and anxiety symptoms. The majority were undergraduate females. | Mindfulness-based mHealth | 4-week program | PHQ-9, GAD-7 | Mindfulness mHealth intervention had a superior effect on anxiety compared to social support mHealth, while both conditions had a similar effect on improved depression. |
| Wagner (2021) et al. RCT | United States | Recruitment was conducted among patients from a cancer centre and three cancer institutes | 196 Adults | 54.7 | Breast cancer survivors. Most were non-hispanic whites, employed ≥32 h/wk, with various histories of oncology treatment. | iCBT | 4-week program | FoR, CARS | The results indicate that CBT and HMC made similar contributions to reducing FCRI scores, and Telecoaching programme was associated with lower absenteeism and higher website use. |
| Article | Eligibility Criteria | Random Allocation | Concealed Allocation | Baseline Comparability | Blind Subjects | Blind Therapist | Blind Assessors | Adequate Follow-Up | Intention-to-Treat Analysis | Between-Group Comparison | Point Estimate and Variability | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Al-Alawi et al. | Y | Y | U | Y | N | N | Y | Y | N | Y | Y | 7 |
| Anthony et al. | U | Y | U | Y | N | U | U | Y | N | Y | Y | 5 |
| Comer et al. | Y | Y | U | Y | N | U | U | Y | Y | Y | Y | 7 |
| MacKinnon et al. | Y | Y | Y | Y | N | U | Y | Y | Y | Y | Y | 9 |
| Policarpo et al. | Y | Y | U | Y | N | N | U | U | N | Y | Y | 5 |
| Prato et al. | Y | Y | U | Y | N | N | Y | Y | N | Y | Y | 7 |
| Rachamim et al. | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 9 |
| Sun et al. | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 10 |
| Wagner et al. | Y | Y | U | Y | Y | Y | U | Y | Y | Y | N | 8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rutkowska, A. Telemedicine Interventions as an Attempt to Improve the Mental Health of Populations during the COVID-19 Pandemic—A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 14945. https://doi.org/10.3390/ijerph192214945
Rutkowska A. Telemedicine Interventions as an Attempt to Improve the Mental Health of Populations during the COVID-19 Pandemic—A Narrative Review. International Journal of Environmental Research and Public Health. 2022; 19(22):14945. https://doi.org/10.3390/ijerph192214945
Chicago/Turabian StyleRutkowska, Anna. 2022. "Telemedicine Interventions as an Attempt to Improve the Mental Health of Populations during the COVID-19 Pandemic—A Narrative Review" International Journal of Environmental Research and Public Health 19, no. 22: 14945. https://doi.org/10.3390/ijerph192214945





