E-Cigarette Vapour Increases ACE2 and TMPRSS2 Expression in a Flavour- and Nicotine-Dependent Manner
Abstract
1. Introduction
2. Materials and Methods
2.1. EVE and CSE Preparation
2.2. Preparation of Primary Bronchial Epithelial Cells
2.3. Monocyte-Derived Macrophages (MDM)
2.4. Sample Collection and cDNA Conversion
2.5. Taqman qPCR
2.6. Statistical Analysis
3. Results
3.1. MDM ACE2 and TMPRSS2 Expression
3.2. NHBE ACE2 and TMPRSS2 Expression
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus—Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Spuntarelli, V.; Luciani, M.; Bentivegna, E.; Marini, V.; Falangone, F.; Conforti, G.; Rachele, E.S.; Martelletti, P. COVID-19: Is it just a lung disease? A case-based review. SN Compr. Clin. Med. 2020, 2, 1401–1406. [Google Scholar] [CrossRef]
- Walls, A.C.; Park, Y.J.; Tortorici, M.A.; Wall, A.; McGuire, A.T.; Veesler, D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020, 181, 281–292.e6. [Google Scholar] [CrossRef]
- Patel, S.; Rauf, A.; Khan, H.; Abu-Izneid, T. Renin-angiotensin-aldosterone (RAAS): The ubiquitous system for homeostasis and pathologies. Biomed. Pharmacother. 2017, 94, 317–325. [Google Scholar] [CrossRef]
- Matsuyama, S.; Nagata, N.; Shirato, K.; Kawase, M.; Takeda, M.; Taguchi, F. Efficient Activation of the Severe Acute Respiratory Syndrome Coronavirus Spike Protein by the Transmembrane Protease TMPRSS2. J. Virol. 2010, 84, 12658–12664. [Google Scholar] [CrossRef]
- Lukassen, S.; Chua, R.L.; Trefzer, T.; Kahn, N.C.; Schneider, M.A.; Muley, T.; Winter, H.; Meister, M.; Veith, C.; Boots, A.W.; et al. SARS -CoV-2 receptor ACE 2 and TMPRSS 2 are primarily expressed in bronchial transient secretory cells. EMBO J. 2020, 39, e105114. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Wang, M.; Cao, R.; Zhang, L.; Yang, X.; Liu, J.; Xu, M.; Shi, Z.; Hu, Z.; Zhong, W.; Xiao, G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020, 30, 269–271. [Google Scholar] [CrossRef]
- Wrapp, D.; Wang, N.; Corbett, K.S.; Goldsmith, J.A.; Hsieh, C.-L.; Abiona, O.; Graham, B.S.; McLellan, J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 2020, 367, 1260–1263. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, M.; Ferguson, I.D.; Miao, W.; Khavari, P.A. SARS-CoV-2 B.1.1.7 and B.1.351 spike variants bind human ACE2 with increased affinity. Lancet Infect. Dis. 2021, 21, 1070. [Google Scholar] [CrossRef]
- Radzikowska, U.; Ding, M.; Tan, G.; Zhakparov, D.; Peng, Y.; Wawrzyniak, P.; Wang, M.; Li, S.; Morita, H.; Altunbulakli, C.; et al. Distribution of ACE2, CD147, CD26, and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors. Allergy 2020, 75, 2829–2845. [Google Scholar] [CrossRef]
- Qiao, Y.; Wang, X.M.; Mannan, R.; Pitchiaya, S.; Zhang, Y.; Wotring, J.W.; Xiao, L.; Robinson, D.R.; Wu, Y.M.; Tien, J.C.Y.; et al. Targeting transcriptional regulation of SARS-CoV-2 entry factors ACE2 and TMPRSS2. Proc. Natl. Acad. Sci. USA 2021, 118, e2021450118. [Google Scholar] [CrossRef] [PubMed]
- Muus, C.; Luecken, M.D.; Eraslan, G.; Sikkema, L.; Waghray, A.; Heimberg, G.; Kobayashi, Y.; Vaishnav, E.D.; Subramanian, A.; Smillie, C.; et al. Single-cell meta-analysis of SARS-CoV-2 entry genes across tissues and demographics. Nat. Med. 2021, 27, 546–559. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Chu, H.; Li, C.; Wong, B.H.-Y.; Cheng, Z.-S.; Poon, V.K.-M.; Sun, T.; Lau, C.C.-Y.; Wong, K.K.-Y.; Chan, J.Y.-W.; et al. Active Replication of Middle East Respiratory Syndrome Coronavirus and Aberrant Induction of Inflammatory Cytokines and Chemokines in Human Macrophages: Implications for Pathogenesis. J. Infect. Dis. 2014, 209, 1331–1342. [Google Scholar] [CrossRef]
- Desforges, M.; Miletti, T.C.; Gagnon, M.; Talbot, P.J. Activation of human monocytes after infection by human coronavirus 229E. Virus Res. 2007, 130, 228–240. [Google Scholar] [CrossRef]
- Okamura, A.; Rakugi, H.; Ohishi, M.; Yanagitani, Y.; Takiuchi, S.; Moriguchi, K.; Fennessy, P.A.; Higaki, J.; Ogihara, T. Upregulation of renin-angiotensin system during differentiation of monocytes to macrophages. J. Hypertens. 1999, 17, 537–545. [Google Scholar] [CrossRef]
- Song, X.; Hu, W.; Yu, H.; Zhao, L.; Zhao, Y.; Zhao, X.; Xue, H.; Zhao, Y. Little to no expression of angiotensin-converting enzyme-2 on most human peripheral blood immune cells but highly expressed on tissue macrophages. Cytom. Part A 2020. [Google Scholar] [CrossRef]
- Pence, B.D. Severe COVID-19 and aging: Are monocytes the key? Geroscience 2020, 42, 1051–1061. [Google Scholar] [CrossRef]
- Liao, M.; Liu, Y.; Yuan, J.; Wen, Y.; Xu, G.; Zhao, J.; Cheng, L.; Li, J.; Wang, X.; Wang, F.; et al. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat. Med. 2020, 26, 842–844. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Koh, J.Y.; Yi, K.; Kim, Y.I.; Park, S.J.; Kim, E.H.; Kim, S.-M.; Park, S.H.; Ju, Y.S.; Choi, Y.K.; et al. Single-cell transcriptome of bronchoalveolar lavage fluid reveals sequential change of macrophages during SARS-CoV-2 infection in ferrets. Nat. Commun. 2021, 12, 4567. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Wang, Z.; Qu, Y.; Zhu, H.; Zhu, Q.; Tong, W.; Bao, L.; Lv, Q.; Cong, J.; Li, D.; et al. Distinct uptake, amplification, and release of SARS-CoV-2 by M1 and M2 alveolar macrophages. Cell Discov. 2021, 7, 24. [Google Scholar] [CrossRef]
- Abassi, Z.; Knaney, Y.; Karram, T.; Heyman, S.N. The Lung Macrophage in SARS-CoV-2 Infection: A Friend or a Foe? Front. Immunol 2020, 11, 1312. [Google Scholar] [CrossRef] [PubMed]
- Meidaninikjeh, S.; Sabouni, N.; Marzouni, H.Z.; Bengar, S.; Khalili, A.; Jafari, R. Monocytes and macrophages in COVID-19: Friends and foes. Life Sci. 2021, 269, 119010. [Google Scholar] [CrossRef]
- Grant, R.A.; Morales-Nebreda, L.; Markov, N.S.; Swaminathan, S.; Querrey, M.; Guzman, E.R.; Abbott, D.A.; Donnelly, H.K.; Donayre, A.; Goldberg, I.A.; et al. Circuits between infected macrophages and T cells in SARS-CoV-2 pneumonia. Nature 2021, 590, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Patanavanich, R.; Glantz, S.A. Smoking Is Associated With COVID-19 Progression: A Meta-analysis. Nicotine Tob. Res. 2020, 22, 1653–1656. [Google Scholar] [CrossRef]
- Zhao, Q.; Meng, M.; Kumar, R.; Wu, Y.; Huang, J.; Lian, N.; Deng, Y.; Lin, S. The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J. Med. Virol. 2020, 92, 1915–1921. [Google Scholar] [CrossRef]
- Reddy, R.K.; Charles, W.N.; Sklavounos, A.; Dutt, A.; Seed, P.T.; Khajuria, A. The effect of smoking on COVID-19 severity: A systematic review and meta-analysis. J. Med Virol. 2021, 93, 1045–1056. [Google Scholar] [CrossRef]
- Patanavanich, R.; Glantz, S.A. Smoking is associated with worse outcomes of COVID-19 particularly among younger adults: A systematic review and meta-analysis. BMC Public Health 2021, 21, 1554. [Google Scholar] [CrossRef]
- Zhang, Q.; Yue, Y.; Tan, H.; Liu, Y.; Zeng, Y.; Xiao, L. Single Cell RNA-seq Data Analysis Reveals the Potential Risk of SARS-CoV-2 Infection Among Different Respiratory System Conditions. Front. Genet. 2020, 11, 942. [Google Scholar] [CrossRef]
- Yin, J.; Kasper, B.; Petersen, F.; Yu, X. Association of Cigarette Smoking, COPD, and Lung Cancer With Expression of SARS-CoV-2 Entry Genes in Human Airway Epithelial Cells. Front. Med. 2020, 7, 619453. [Google Scholar] [CrossRef] [PubMed]
- Leung, J.M.; Yang, C.X.; Tam, A.; Shaipanich, T.; Hackett, T.-L.; Singhera, G.K.; Dorscheid, D.R.; Sin, D.D. ACE-2 expression in the small airway epithelia of smokers and COPD patients: Implications for COVID-19. Eur. Respir. J. 2020, 55, 2000688. [Google Scholar] [CrossRef]
- Jose, T.; Croghan, I.T.; Hays, J.T.; Schroeder, D.R.; Warner, D.O. Electronic Cigarette Use Is Not Associated with COVID-19 Diagnosis. J. Prim. Care Community Health 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur. J. Intern. Med. 2020, 75, 107–108. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Rubio, J.; Navarro-López, C.; López-Nájera, E.; López-Nájera, A.; Jiménez-Díaz, L.; Navarro-López, J.D.; Nájera, A. A Systematic Review and Meta-Analysis of Hospitalised Current Smokers and COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 7394. [Google Scholar] [CrossRef]
- Russo, P.; Bonassi, S.; Giacconi, R.; Malavolta, M.; Tomino, C.; Maggi, F. COVID-19 and smoking: Is nicotine the hidden link? Eur. Respir. J. 2020, 55, 2001116. [Google Scholar] [CrossRef]
- Oakes, J.M.; Fuchs, R.M.; Gardner, J.D.; Lazartigues, E.; Yue, X. Nicotine and the renin-angiotensin system. Am. J. Physiol. Integr. Comp. Physiol. 2018, 315, R895–R906. [Google Scholar] [CrossRef]
- Bozier, J.; Chivers, E.K.; Chapman, D.G.; Larcombe, A.N.; Bastian, N.A.; Masso-Silva, J.A.; Byun, M.K.; McDonald, C.F.; Alexander, L.E.C.; Ween, M.P. The Evolving Landscape of Electronic Cigarettes: A Systematic Review of Recent Evidence. Chest 2020, 157, 1362–1390. [Google Scholar] [CrossRef]
- Ween, M.P.; Whittall, J.J.; Hamon, R.; Reynolds, P.N.; Hodge, S.J. Phagocytosis and Inflammation: Exploring the effects of the components of E-cigarette vapor on macrophages. Physiol. Rep. 2017, 5, e13370. [Google Scholar] [CrossRef]
- Ween, M.P.; Moshensky, A.; Thredgold, L.; Bastian, N.A.; Hamon, R.; Badiei, A.; Nguyen, P.T.; Herewane, K.; Jersmann, H.; Bojanowski, C.M.; et al. E-cigarettes and health risks: More to the flavour than just the name. Am. J. Physiol. Lung. Cell Mol. Physiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ween, M.P.; Hamon, R.; Macowan, M.; Thredgold, L.; Reynolds, P.N.; Hodge, S.J. Effects of E-cigarette E-liquid components on bronchial epithelial cells: Demonstration of dysfunctional efferocytosis. Respirology 2020, 25, 620–628. [Google Scholar] [CrossRef]
- Donnelly, L.E.; Tudhope, S.J.; Fenwick, P.S.; Barnes, P.J. Effects of formoterol and salmeterol on cytokine release from monocyte-derived macrophages. Eur. Respir. J. 2009, 36, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Ween, M.P.; White, J.B.; Tran, H.B.; Mukaro, V.; Jones, C.; Macowan, M.; Hodge, G.; Trim, P.J.; Snel, M.F.; Hodge, S.J. The role of oxidised self-lipids and alveolar macrophage CD1b expression in COPD. Sci. Rep. 2021, 11, 4106. [Google Scholar] [CrossRef]
- Ferrari, M.F.R.; Raizada, M.K.; Fior-Chadi, D.R. Differential Regulation of the Renin-Angiotensin System by Nicotine in WKY and SHR Glia. J. Mol. Neurosci. 2008, 35, 151–160. [Google Scholar] [CrossRef]
- Axelsson, G.T.; Eythorsson, E.S.; Hardardottir, H.; Gudmundsson, G.; Hansdottir, S. The impact of lung diseases, smoking and e-cigarette use on the severity of COVID-19 illness at diagnosis. Laeknabladid 2020, 106, 574–579. [Google Scholar]
- Rossato, M.; Russo, L.; Mazzocut, S.; Di Vincenzo, A.; Fioretto, P.; Vettor, R. Current smoking is not associated with COVID-19. Eur. Respir. J. 2020, 55, 2001290. [Google Scholar] [CrossRef] [PubMed]
- Tsigaris, P.; Silva, J.A.T.D. Smoking Prevalence and COVID-19 in Europe. Nicotine Tob. Res. 2020, 22, 1646–1649. [Google Scholar] [CrossRef]
- Simons, D.; Shahab, L.; Brown, J.; Perski, O. The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: A living rapid evidence review with Bayesian meta-analyses (version 7). Addiction 2021, 116, 1319–1368. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Alghamdi, S.M.; Almehmadi, M.; Alqahtani, A.S.; Quaderi, S.; Mandal, S.; Hurst, J.R. Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0233147. [Google Scholar] [CrossRef]
- Tattan-Birch, H.; Perski, O.; Jackson, S.; Shahab, L.; West, R.; Brown, J. COVID-19, smoking, vaping and quitting: A representative population survey in England. Addiction 2021, 116, 1186–1195. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Kyriakos, C. Cigarette and E-Cigarettes Dual Users, Exclusive Users and COVID-19: Findings from Four UK Birth Cohort Studies. Int. J. Environ. Res. Public Heal. 2021, 18, 3935. [Google Scholar] [CrossRef] [PubMed]
- Sharif-Askari, N.S.; Sharif-Askari, F.S.; Alabed, M.; Temsah, M.-H.; Al Heialy, S.; Hamid, Q.; Halwani, R. Airways Expression of SARS-CoV-2 Receptor, ACE2, and TMPRSS2 Is Lower in Children Than Adults and Increases with Smoking and COPD. Mol. Ther. - Methods Clin. Dev. 2020, 18, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Chakladar, J.; Li, W.; Chen, C.; Chang, E.; Wang-Rodriguez, J.; Ongkeko, W. Tobacco, but Not Nicotine and Flavor-Less Electronic Cigarettes, Induces ACE2 and Immune Dysregulation. Int. J. Mol. Sci. 2020, 21, 5513. [Google Scholar] [CrossRef]
- Matusiak, M.; Schurch, C.M. Expression of SARS-CoV-2 entry receptors in the respiratory tract of healthy individuals, smokers and asthmatics. Respir. Res. 2020, 21, 252. [Google Scholar] [CrossRef]
- Chakladar, J.; Shende, N.; Li, W.T.; Rajasekaran, M.; Chang, E.Y.; Ongkeko, W.M. Smoking-Mediated Upregulation of the Androgen Pathway Leads to Increased SARS-CoV-2 Susceptibility. Int. J. Mol. Sci. 2020, 21, 3627. [Google Scholar] [CrossRef]
- Kaur, G.; Yogeswaran, S.; Muthumalage, T.; Rahman, I. Persistently Increased Systemic ACE2 Activity Is Associated With an Increased Inflammatory Response in Smokers With COVID-19. Front. Physiol. 2021, 12, 653045. [Google Scholar] [CrossRef]
- Lobunets, K.A. Change in the hemodynamic indices of dogs after acute massive blood loss and the transfusion of modified globulin solutions. Fiziol. Zhurnal 1979, 25, 47–52. [Google Scholar]
- Dwyer, T.M. Cigarette Smoke-Induced Airway Inflammation as Sampled by the Expired Breath Condensate. Am. J. Med Sci. 2003, 326, 174–178. [Google Scholar] [CrossRef]
- Arcavi, L.; Benowitz, N.L. Cigarette Smoking and Infection. Arch. Intern. Med. 2004, 164, 2206–2216. [Google Scholar] [CrossRef]
- Gualano, R.C.; Hansen, M.J.; Vlahos, R.; E Jones, J.; A Park-Jones, R.; Deliyannis, G.; Turner, S.J.; A Duca, K.; Anderson, G.P. Cigarette smoke worsens lung inflammation and impairs resolution of influenza infection in mice. Respir. Res. 2008, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Ween, M.; Ahern, J.; Carroll, A.; Hodge, G.; Pizzutto, S.; Jersmann, H.; Reynolds, P.; Hodge, S. A small volume technique to examine and compare alveolar macrophage phagocytosis of apoptotic cells and non typeable Haemophilus influenzae (NTHi). J. Immunol. Methods 2016, 429, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; COPDMAP Consortium; Belchamber, K.B.R.; Fenwick, P.S.; Chana, K.; Donaldson, G.; Wedzicha, J.A.; Barnes, P.J.; Donnelly, L.E. Defective monocyte-derived macrophage phagocytosis is associated with exacerbation frequency in COPD. Respir. Res. 2021, 22, 113. [Google Scholar] [CrossRef] [PubMed]
- Sluimer, J.; Gasc, J.M.; Hamming, I.; van Goor, H.; Michaud, A.; Akker, L.H.V.D.; Jutten, B.; Cleutjens, J.; Bijnens, A.P.J.J.; Corvol, P.; et al. Angiotensin-converting enzyme 2 (ACE2) expression and activity in human carotid atherosclerotic lesions. J. Pathol. 2008, 215, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Keidar, S.; Strizevsky, A.; Raz, A.; Gamliel-Lazarovich, A. ACE2 activity is increased in monocyte-derived macrophages from prehypertensive subjects. Nephrol. Dial. Transplant. 2006, 22, 597–601. [Google Scholar] [CrossRef][Green Version]
- Sagawa, T.; Tsujikawa, T.; Honda, A.; Miyasaka, N.; Tanaka, M.; Kida, T.; Hasegawa, K.; Okuda, T.; Kawahito, Y.; Takano, H. Exposure to particulate matter upregulates ACE2 and TMPRSS2 expression in the murine lung. Environ. Res. 2021, 195, 110722. [Google Scholar] [CrossRef]
- Gnirss, K.; Kühl, A.; Karsten, C.; Glowacka, I.; Bertram, S.; Kaup, F.; Hofmann, H.; Pöhlmann, S. Cathepsins B and L activate Ebola but not Marburg virus glycoproteins for efficient entry into cell lines and macrophages independent of TMPRSS2 expression. Virology 2012, 424, 3–10. [Google Scholar] [CrossRef]
- Corriden, R.; Moshensky, A.; Bojanowski, C.M.; Meier, A.; Chien, J.; Nelson, R.K.; Alexander, L.E.C. E-cigarette use increases susceptibility to bacterial infection by impairment of human neutrophil chemotaxis, phagocytosis, and NET formation. Am. J. Physiol. Physiol. 2020, 318, C205–C214. [Google Scholar] [CrossRef]
- Gaiha, S.; Cheng, J.; Halpern-Felsher, B. Association Between Youth Smoking, Electronic Cigarette Use, and COVID-19. J. Adolesc. Heal. 2020, 67, 519–523. [Google Scholar] [CrossRef]
- Knoll, R.; Schultze, J.L.; Schulte-Schrepping, J. Monocytes and Macrophages in COVID-19. Front. Immunol. 2021, 12. [Google Scholar] [CrossRef]
- Kelesidis, T.; Zhang, Y.; Tran, E.; Sosa, G.; Middlekauff, H.R. Instigators of COVID-19 in Immune Cells Are Increased in Tobacco Cigarette Smokers and Electronic Cigarette Vapers Compared With Nonsmokers. Nicotine Tob. Res. 2022, 24, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Almeida-da-Silva, C.L.C.; Matshik Dakafay, H.; Liu, K.; Ojcius, D.M. Cigarette Smoke Stimulates SARS-CoV-2 Internalization by Activating AhR and Increasing ACE2 Expression in Human Gingival Epithelial Cells. Int. J. Mol. Sci. 2021, 22, 7669. [Google Scholar] [CrossRef]
- Uhal, B.D.; Li, X.; Piasecki, C.C.; Molina, M.M. Angiotensin signalling in pulmonary fibrosis. Int. J. Biochem. Cell Biol. 2012, 44, 465–468. [Google Scholar] [CrossRef]
- Gopallawa, I.; Uhal, B.D. Molecular and cellular mechanisms of the inhibitory effects of ACE-2/ANG1-7/Mas axis on lung injury. Curr. Top. Pharmacol. 2014, 18, 71–80. [Google Scholar] [PubMed]
- Wang, Y.; Pereira, E.F.R.; Maus, A.D.J.; Ostlie, N.S.; Navaneetham, D.; Lei, S.; Albuquerque, E.X.; Conti-Fine, B.M. Human Bronchial Epithelial and Endothelial Cells Express α7 Nicotinic Acetylcholine Receptors. Mol. Pharmacol. 2001, 60, 1201–1209. [Google Scholar] [CrossRef]
- Maus, A.D.J.; Pereira, E.F.R.; Karachunski, P.I.; Horton, R.M.; Navaneetham, D.; Macklin, K.; Cortes, W.S.; Albuquerque, E.X.; Conti-Fine, B.M. Human and Rodent Bronchial Epithelial Cells Express Functional Nicotinic Acetylcholine Receptors. Mol. Pharmacol. 1998, 54, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Sundar, I.K.; Li, D.; Lucas, J.H.; Muthumalage, T.; McDonough, S.R.; Rahman, I. E-cigarette-induced pulmonary inflammation and dysregulated repair are mediated by nAChR alpha7 receptor: Role of nAChR alpha7 in SARS-CoV-2 COVID-19 ACE2 receptor regulation. Respir. Res. 2020, 21, 154. [Google Scholar] [CrossRef]
- Lallai, V.; Manca, L.; Fowler, C.D. E-cigarette vape and lung ACE2 expression: Implications for coronavirus vulnerability. Environ. Toxicol. Pharmacol. 2021, 86, 103656. [Google Scholar] [CrossRef]
- Naidu, V.; Zeki, A.; Sharma, P. Sex differences in the induction of angiotensin converting enzyme 2 (ACE-2) in mouse lungs after e-cigarette vapor exposure and its relevance to COVID-19. J. Investig. Med. 2021, 69, 954–961. [Google Scholar] [CrossRef]
- Mihaltan, F.D.; Rajnoveanu, A.-G.; Rajnoveanu, R.-M. Impact of Smoking on Women During the Covid-19 Pandemic. Front. Med. 2021, 8, 584061. [Google Scholar] [CrossRef]
- Vahidy, F.S.; Pan, A.P.; Ahnstedt, H.; Munshi, Y.; Choi, H.A.; Tiruneh, Y.; Nasir, K.; Kash, B.A.; Andrieni, J.D.; McCullough, L.D. Sex differences in susceptibility, severity, and outcomes of coronavirus disease 2019: Cross-sectional analysis from a diverse US metropolitan area. PLoS ONE 2021, 16, e0245556. [Google Scholar] [CrossRef]
- Cai, H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir. Med. 2020, 8, e20. [Google Scholar] [CrossRef]
- Kale, D.; Herbec, A.; Perski, O.; Jackson, S.E.; Brown, J.; Shahab, L. Associations between vaping and COVID-19: Cross-sectional findings from the HEBECO study. Drug Alcohol Depend. 2021, 221, 108590. [Google Scholar] [CrossRef]
- McAlinden, K.D.; Lu, W.; Ferdowsi, P.V.; Myers, S.; Markos, J.; Larby, J.; Chia, C.; Weber, H.C.; Haug, G.; Eapen, M.S.; et al. Electronic Cigarette Aerosol Is Cytotoxic and Increases ACE2 Expression on Human Airway Epithelial Cells: Implications for SARS-CoV-2 (COVID-19). J. Clin. Med. 2021, 10, 1028. [Google Scholar] [CrossRef]
- Masso-Silva, J.A.; Moshensky, A.; Shin, J.; Olay, J.; Nilaad, S.; Advani, I.; Bojanowski, C.M.; Crotty, S.; Li, W.T.; Ongkeko, W.M.; et al. Chronic E-Cigarette Aerosol Inhalation Alters the Immune State of the Lungs and Increases ACE2 Expression, Raising Concern for Altered Response and Susceptibility to SARS-CoV-2. Front. Physiol. 2021, 12, 649604. [Google Scholar] [CrossRef]
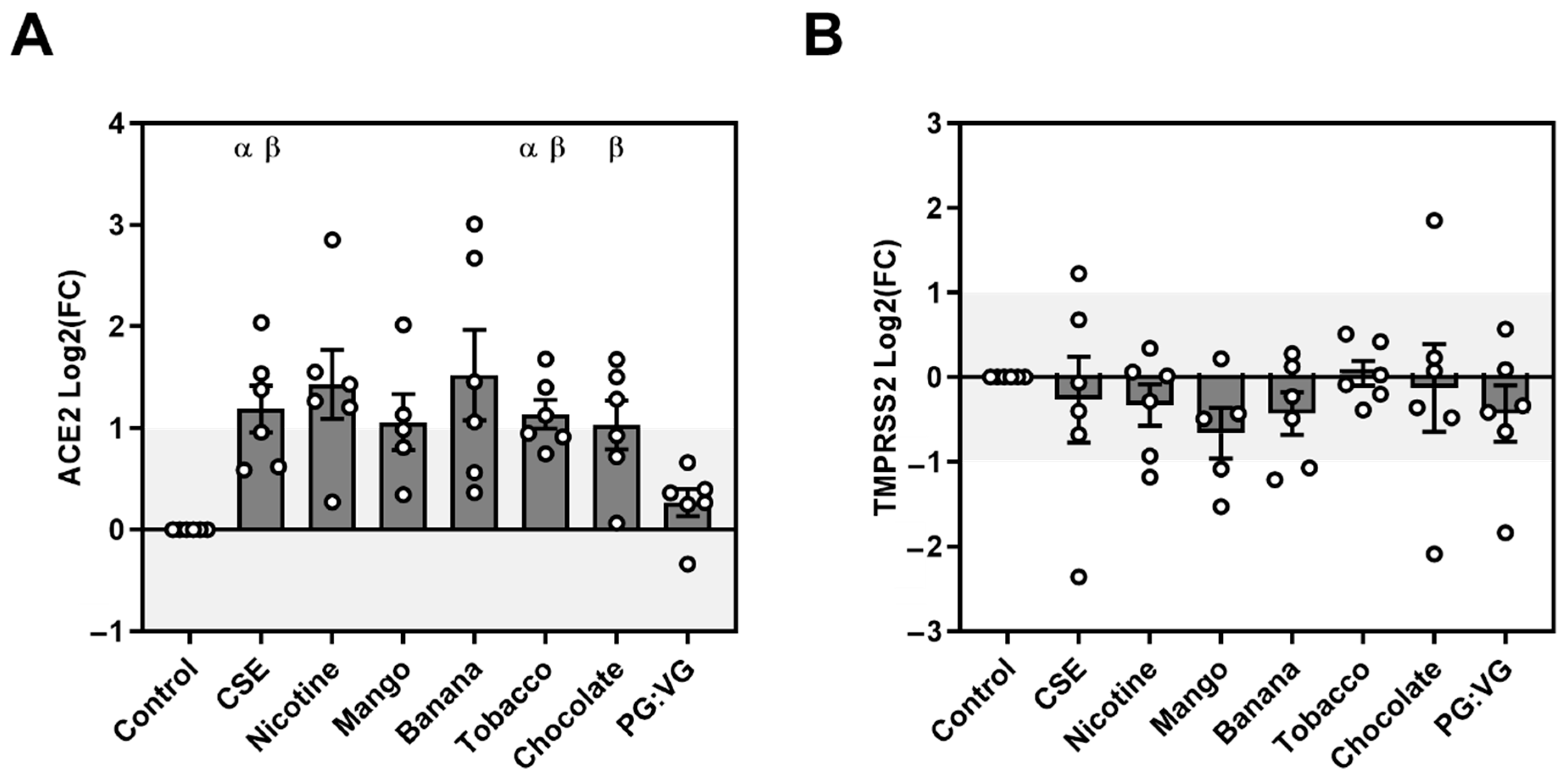

| MDM ACE2 mRNA Expression | MDM TMPRSS2 mRNA Expression | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tukey’s Multiple | Fold Change | Log2(FC) | Adjusted p Value | Fold Change | Log2(FC) | Adjusted p Value | |||
| Comparisons Test | Mean(SEM) | Mean(SEM) | Mean(SEM) | Mean(SEM) | |||||
| PG:VG vs. | Control | 1.23(0.10) | 0.26(1.06) | 0.570 | ns | 0.83(0.17) | −0.43(0.73) | 0.869 | ns |
| CSE vs. | Control | 2.43(0.41) | 1.18(1.09) | 0.035 | * | 1.08(0.31) | −0.27(1.06) | 0.999 | ns |
| PG:VG | 1.95(0.21) | 0.027 | * | 1.42(0.43) | 1.000 | ns | |||
| Nicotine EVE vs. | Control | 3.12(0.85) | 1.43(0.90) | 0.073 | ns | 0.93(0.11) | −0.33(1.02) | 0.850 | ns |
| PG:VG | 2.55(0.70) | 0.093 | ns | 1.23(0.22) | 0.999 | ns | |||
| Mango EVE vs | Control | 2.24(0.47) | 1.34(1.27) | 0.113 | ns | 0.69(0.14) | 0.08(0.63) | 0.439 | ns |
| PG:VG | 1.67(0.47) | 0.343 | ns | 1.05(0.17) | 0.986 | ns | |||
| Banana EVE vs. | Control | 3.66(1.16) | 1.52(0.89) | 0.154 | ns | 0.80(0.13) | −0.43(1.03) | 0.675 | ns |
| PG:VG | 3.42(1.27) | 0.431 | ns | 1.31(0.40) | 0.999 | ns | |||
| Tobacco EVE vs. | Control | 2.25(0.23) | 1.13(1.17) | 0.005 | ** | 1.06(0.11) | 0.05(0.81) | 0.999 | ns |
| PG:VG | 1.90(0.23) | 0.046 | * | 1.73(0.62) | 0.896 | ns | |||
| Chocolate EVE vs. | Control | 2.17(0.32) | 1.03(1.02) | 0.070 | ns | 1.26(0.49) | −0.13(1.21) | 0.999 | ns |
| PG:VG | 1.74(0.18) | 0.027 | * | 1.71(0.46) | 0.999 | ns | |||
| NHBE ACE2 mRNA Expression | NHBE TMPRSS2 mRNA Expression | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tukey’s Multiple | Fold Change | Log2 (FC) | Adjusted p Value | Fold Change | Log2 (FC) | Adjusted p Value | |||
| Comparisons Test | Mean(SEM) | Mean(SEM) | Mean(SEM) | Mean(SEM) | |||||
| PG:VG vs. | Control | 0.85(0.10) | −0.32(0.42) | 0.741 | Ns | 0.84(0.12) | −0.35(0.99) | 0.718 | ns |
| CSE vs. | Control | 2.11(0.28) | 0.99(0.34) | 0.018 | * | 3.77(0.71) | 1.76(0.85) | 0.003 | ** |
| PG:VG | 2.66(0.41) | 0.004 | ** | 5.78(1.93) | 0.016 | * | |||
| Nicotine EVE vs. | Control | 2.11(0.34) | 0.94(0.40) | 0.068 | Ns | 1.92(0.11) | 1.16(1.07) | 0.0002 | *** |
| PG:VG | 2.64(0.44) | 0.019 | * | 2.76(0.43) | 0.013 | * | |||
| Mango EVE vs. | Control | 1.57(0.25) | 0.52(0.35) | 0.484 | Ns | 1.19(0.16) | 0.17(1.00) | 0.969 | ns |
| PG:VG | 2.05(0.38) | 0.098 | Ns | 1.65(0.48) | 0.497 | ns | |||
| Banana EVE vs. | Control | 2.60(0.43) | 1.22(0.47) | 0.034 | * | 2.60(0.60) | 1.10(0.82) | 0.119 | ns |
| PG:VG | 3.23(0.50) | 0.011 | * | 3.51(1.10) | 0.073 | ns | |||
| Tobacco EVE vs. | Control | 1.38(0.24) | 0.30(0.50) | 0.918 | Ns | 1.22(0.23) | 0.11(0.98) | 1.000 | Ns |
| PG:VG | 1.62(0.19) | 0.100 | Ns | 1.4(0.08) | 0.034 | * | |||
| Chocolate EVE vs. | Control | 2.46(0.42) | 1.39(0.44) | 0.0009 | *** | 3.02(0.62) | 1.34(0.77) | 0.076 | Ns |
| PG:VG | 3.07(0.66) | 0.006 | ** | 4.07(0.93) | 0.035 | * | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamon, R.; Ween, M.P. E-Cigarette Vapour Increases ACE2 and TMPRSS2 Expression in a Flavour- and Nicotine-Dependent Manner. Int. J. Environ. Res. Public Health 2022, 19, 14955. https://doi.org/10.3390/ijerph192214955
Hamon R, Ween MP. E-Cigarette Vapour Increases ACE2 and TMPRSS2 Expression in a Flavour- and Nicotine-Dependent Manner. International Journal of Environmental Research and Public Health. 2022; 19(22):14955. https://doi.org/10.3390/ijerph192214955
Chicago/Turabian StyleHamon, Rhys, and Miranda P. Ween. 2022. "E-Cigarette Vapour Increases ACE2 and TMPRSS2 Expression in a Flavour- and Nicotine-Dependent Manner" International Journal of Environmental Research and Public Health 19, no. 22: 14955. https://doi.org/10.3390/ijerph192214955
APA StyleHamon, R., & Ween, M. P. (2022). E-Cigarette Vapour Increases ACE2 and TMPRSS2 Expression in a Flavour- and Nicotine-Dependent Manner. International Journal of Environmental Research and Public Health, 19(22), 14955. https://doi.org/10.3390/ijerph192214955





