Operational and Financial Impacts of Digital Health Technology: A Study on Canadian Healthcare System during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Source Data
- Canadian Institute for Health Information
- Financial Accountability Office of Ontario
- Government of Alberta
- Government of British Columbia
- Government of Canada
- Government of Manitoba
- Government of New Brunswick
- Government of Nova Scotia
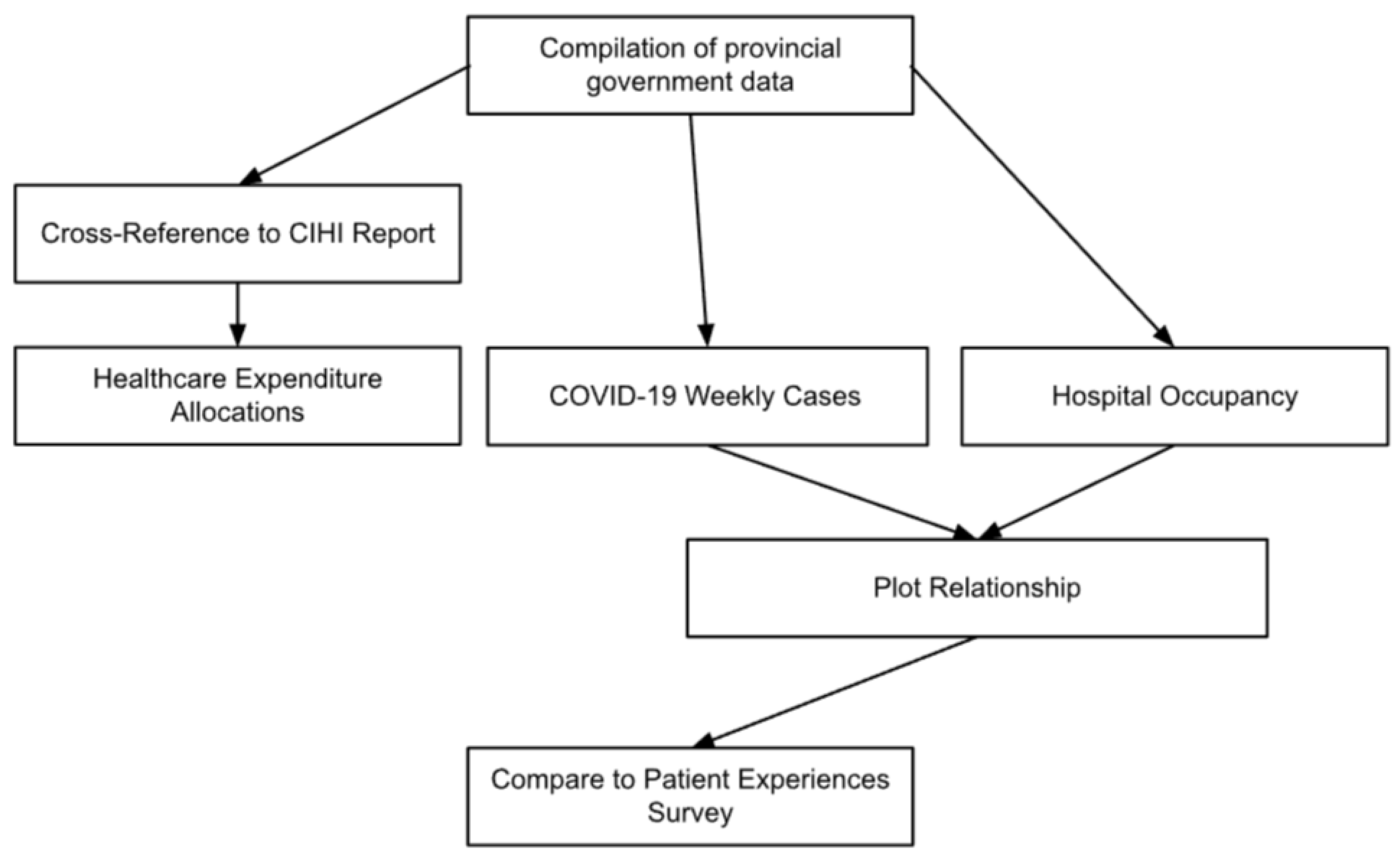
2.2. Workflow
2.3. Software
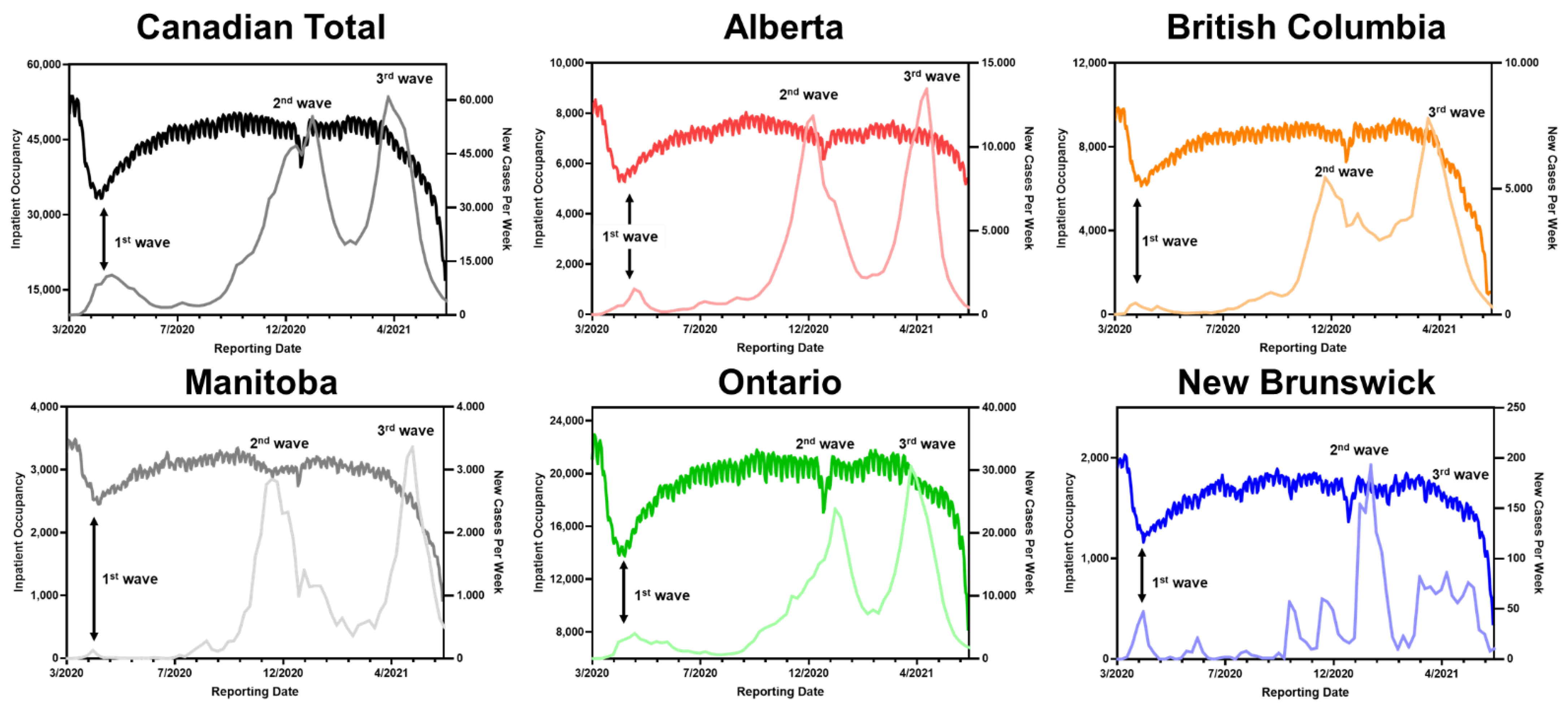
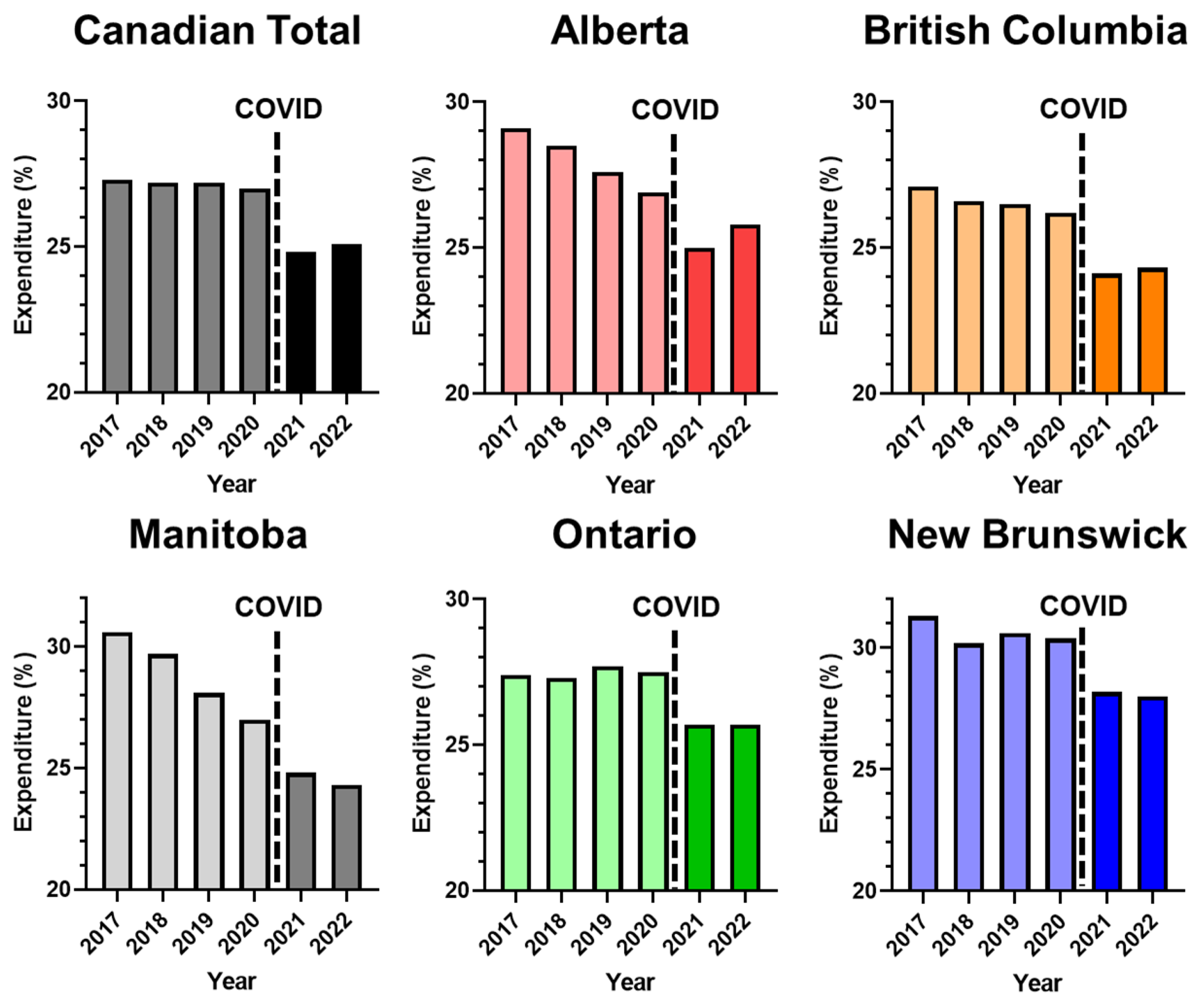
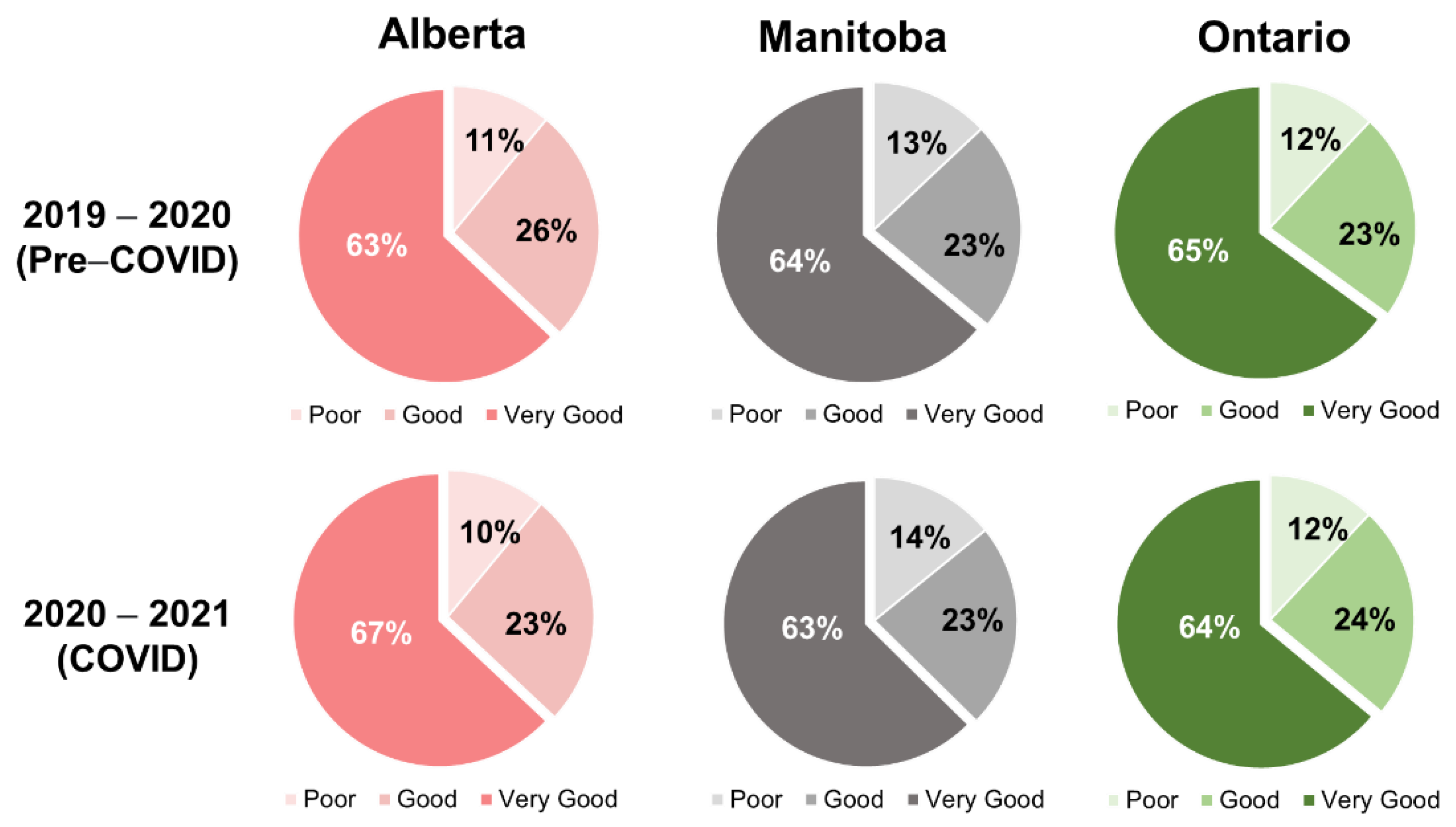
3. Results
Hospital Service and Patient Experience under COVID-19
4. Discussion
Digital Health Implementation in Canadian Hospitals
5. Recommendation
5.1. Information Management System
5.2. Accessibility of Service
5.3. Quality of Service
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus pandemic (COVID-19). Our World Data 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 7 September 2022).
- Overview: COVID-19’s Impact on Health Care Systems. Available online: https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/the-big-picture (accessed on 7 September 2022).
- A Coordinated Global Research Roadmap. Available online: https://www.who.int/publications/m/item/a-coordinated-global-research-roadmap (accessed on 7 September 2022).
- Budd, J.; Miller, B.S.; Manning, E.M.; Lampos, V.; Zhuang, M.; Edelstein, M.; Rees, G.; Emery, V.C.; Stevens, M.M.; Keegan, N.; et al. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020, 26, 1183–1192. [Google Scholar] [CrossRef]
- NHS Funding Data Analysis. The British Medical Association Is the Trade Union and Professional Body for Doctors in the UK. Available online: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/funding/nhs-funding-data-analysis (accessed on 7 September 2022).
- Hanson, K.; Brikci, N.; Erlangga, D.; Alebachew, A.; Allegri, M.D.; Balabanova, D.; Blecher, M.; Cashin, C.; Esperato, A.; Hipgrave, D.; et al. The Lancet Global Health Commission on financing primary health care: Putting people at the centre. Lancet Glob. Health 2022, 10, e715–e772. [Google Scholar] [CrossRef]
- Coronavirus Disease 2019 (COVID-19): Information for NIH Applicants and Recipients of NIH Funding. Available online: https://grants.nih.gov/policy/natural-disasters/corona-virus.htm (accessed on 7 September 2022).
- Patil, U.; Kostareva, U.; Hadley, M.; Manganello, J.A.; Okan, O.; Dadaczynski, K.; Massey, P.M.; Agner, J.; Sentell, T. Health literacy, digital health literacy, and COVID-19 pandemic attitudes and behaviors in U.S. college students: Implications for interventions. Int. J. Environ. Res. Public. Health 2021, 18, 3301. [Google Scholar] [CrossRef] [PubMed]
- Scott, B.K.; Miller, G.T.; Fonda, S.J.; Yeaw, R.E.; Gaudaen, J.C.; Pavliscsak, H.H.; Quinn, M.T.; Pamplin, J.C. Advanced digital health technologies for COVID-19 and future emergencies. Telemed. E-Health 2020, 26, 1226–1233. [Google Scholar] [CrossRef]
- Kadakia, K.; Patel, B.; Shah, A. Advancing digital health: FDA innovation during COVID-19. Npj Digit. Med. 2020, 3, 161. [Google Scholar] [CrossRef] [PubMed]
- McMahon, M.; Nadigel, J.; Thompson, E.; Glazier, R.H. Informing Canada’s health system response to COVID-19: Priorities for health services and policy research. Healthc. Policy 2020, 16, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [PubMed]
- National Health Expenditure Trends. Available online: https://www.cihi.ca/en/national-health-expenditure-trends (accessed on 7 September 2022).
- Financial Accountability Office of Ontario. Available online: https://www.fao-on.org/en/Blog/Publications/health-2020 (accessed on 7 September 2022).
- Weissman, G.E.; Crane-Droesch, A.; Chivers, C.; Luong, T.; Hanish, A.; Levy, M.Z.; Lubken, J.; Becker, M.; Draugelis, M.E.; Anesi, G.L.; et al. Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann. Intern. Med. 2020, 173, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, J.J.; Donoho, D.A.; Forman, H.P. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic—Planning for the nth patient. JAMA Health Forum 2020, 1, e200345. [Google Scholar] [CrossRef] [PubMed]
- Reporting Patient Experience Data. Available online: https://www.cihi.ca/en/patient-experience/reporting-patient-experience-data (accessed on 7 September 2022).
- Wachler, A. The High Cost of Long Wait Times. Available online: https://www.phreesia.com/2020/03/05/infographic-the-high-cost-of-long-wait-times/ (accessed on 7 September 2022).
- Bleustein, C.; Rothschild, D.B.; Valen, A.; Valatis, E.; Schweitzer, L.; Jones, R. Wait times, patient satisfaction scores, and the perception of care. Am. J. Manag. Care 2014, 20, 393–400. [Google Scholar] [PubMed]
- Chu, H.; Westbrook, R.A.; Njue-Marendes, S.; Giordano, T.P.; Dang, B.N. The psychology of the wait time experience–what clinics can do to manage the waiting experience for patients: A longitudinal, qualitative study. BMC Health Serv. Res. 2019, 19, 459. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.M. The ontario telemedicine network: A case report. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2013, 19, 373–376. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Su, M.; Zhang, M.; Li, R. Integrating digital technologies and public health to fight COVID-19 pandemic: Key technologies, applications, challenges and outlook of digital healthcare. Int. J. Environ. Res. Public. Health 2021, 18, 6053. [Google Scholar] [CrossRef] [PubMed]
- Hardcastle, L.; Ogbogu, U. Virtual care: Enhancing access or harming care? Healthc. Manag. Forum 2020, 33, 288–292. [Google Scholar] [CrossRef] [PubMed]
- VIRTUAL CARE IN CANADA: Discussion Paper. Canadian Medical Association. 2020, pp. 6–7. Available online: https://www.cma.ca/sites/default/files/pdf/News/Virtual_Care_discussionpaper_v2EN.pdf (accessed on 7 September 2022).
- Virtual Care|Canada Health Infoway. Available online: https://www.infoway-inforoute.ca/en/digital-health-initiatives/virtual-care (accessed on 7 September 2022).
- Canadians’ Health Care Experiences during COVID-19|Canada Health Infoway. Available online: https://www.infoway-inforoute.ca/en/component/edocman/3828-canadians-health-care-experiences-during-covid-19/ (accessed on 7 September 2022).
- Rose, S.; Hurwitz, H.M.; Mercer, M.B.; Hizlan, S.; Gali, K.; Yu, P.-C.; Franke, C.; Martinez, K.; Stanton, M.; Faiman, M.; et al. Patient experience in virtual visits hinges on technology and the patient-clinician relationship: A large survey study with open-ended questions. J. Med. Internet Res. 2021, 23, e18488. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.cma.ca/sites/default/files/pdf/virtual-care/cma-virtual-care-public-poll-june-2020-e.pdf (accessed on 7 September 2022).
- Patients Love Telehealth—Physicians Are Not So Sure. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/patients-love-telehealth-physicians-are-not-so-sure (accessed on 7 September 2022).
- Hardy, K.; Anistratov, A.; He, W.; Daeninck, F.; Gu, J.; Vergis, A. Bariatric patient experience with virtual care during the COVID-19 pandemic. Obes. Surg. 2022, 32, 940–943. [Google Scholar] [CrossRef] [PubMed]
- Uscher-Pines, L.; Thompson, J.; Taylor, P.; Dean, K.; Yuan, T.; Tong, I.; Mehrotra, A. Where virtual care was already a reality: Experiences of a nationwide telehealth service provider during the COVID-19 pandemic. J. Med. Internet Res. 2020, 22, e22727. [Google Scholar] [CrossRef] [PubMed]
- Journal of Medical Internet Research-Patient Care during the COVID-19 Pandemic: Use of Virtual Care. Available online: https://www.jmir.org/2021/1/e20621/ (accessed on 7 September 2022).
- McMaughan, D.J.; Oloruntoba, O.; Smith, M.L. Socioeconomic status and access to healthcare: Interrelated drivers for healthy aging. Front. Public Health 2020, 8, 231. [Google Scholar] [CrossRef] [PubMed]
- Digital Health: An Opportunity to Advance Health Equity. Available online: https://www.mckinsey.com/industries/life-sciences/our-insights/digital-health-an-opportunity-to-advance-health-equity (accessed on 7 September 2022).
- Schilling, L.; Uhlig, H. Some Simple Bitcoin Economics. J. Monet. Econ. 2019, 106, 16–26. [Google Scholar] [CrossRef]
- PricewaterhouseCoopers Time for Trust: How Blockchain Will Transform Business and the Economy. Available online: https://www.pwc.com/gx/en/industries/technology/publications/blockchain-report-transform-business-economy.html (accessed on 7 September 2022).
- GP at Hand: Patients Are Less Sick Than Others but Use Services More, Evaluation Finds. Available online: https://www.bmj.com/content/365/bmj.l2333 (accessed on 7 September 2022).
- Digital Technologies for Health Financing: What Are the Benefits and Risks for UHC? Available online: https://www.who.int/publications/i/item/9789240031005 (accessed on 7 September 2022).
- Srinivasan, M.; Phadke, A.J.; Zulman, D.; Israni, S.T.; Madill, E.S.; Savage, T.R.; Downing, N.L.; Nelligan, I.; Artandi, M.; Sharp, C. Enhancing patient engagement during virtual care: A conceptual model and rapid implementation at an academic medical center. NEJM Catal. Innov. Care Deliv. 2020, 2–5. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0262 (accessed on 7 September 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, Z.; Wang, Z. Operational and Financial Impacts of Digital Health Technology: A Study on Canadian Healthcare System during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 15025. https://doi.org/10.3390/ijerph192215025
Jin Z, Wang Z. Operational and Financial Impacts of Digital Health Technology: A Study on Canadian Healthcare System during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(22):15025. https://doi.org/10.3390/ijerph192215025
Chicago/Turabian StyleJin, Zixin (Jessie), and Zongjie Wang. 2022. "Operational and Financial Impacts of Digital Health Technology: A Study on Canadian Healthcare System during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 22: 15025. https://doi.org/10.3390/ijerph192215025
APA StyleJin, Z., & Wang, Z. (2022). Operational and Financial Impacts of Digital Health Technology: A Study on Canadian Healthcare System during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(22), 15025. https://doi.org/10.3390/ijerph192215025






