Evaluation of Urinary Catheterization Competency and Self-Efficacy in Nursing Students Using the Flipped Classroom Approach
Abstract
:1. Introduction
2. Materials and Methods
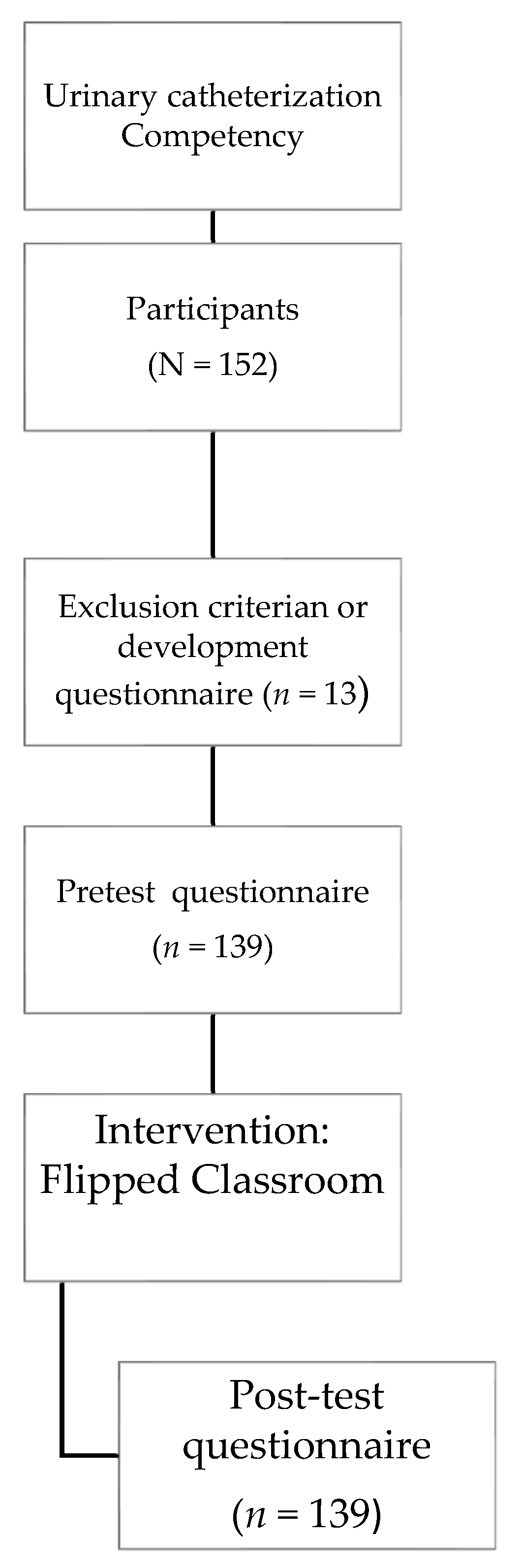
2.1. Design and Participant
2.2. Instruments
2.3. Data Collection
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. Socio-Demographic Characteristics of the Sample
3.2. Self-Efficacy Scale
3.3. Knowledge Questionnaire
3.4. Ability Scale
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van Horn, E.; Christman, J. Assessment of nursing student confidence using the clinical skills self-efficacy scale. Nurs. Educ. Perspect. 2017, 38, 344–346. [Google Scholar] [CrossRef] [PubMed]
- McNett, S. Teaching nursing psychomotor skills in a fundamentals laboratory: A literature review. Nurs. Educ. Perspect. 2012, 33, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Ewertsson, M.; Allvin, R.; Holmström, I.K.; Blomberg, K. Walking the bridge: Nursing students’ learning in clinical skill laboratories. Nurse Educ. Pract. 2015, 15, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Kol, E.; Ince, S.; Işik, R.D.; Ilaslan, E.; Mamakli, S. The effect of using standardized patients in the Simulated Hospital Environment on first-year nursing students psychomotor skills learning. Nurse Educ. Today 2021, 107, 105147. [Google Scholar] [CrossRef]
- Chuang, Y.H.; Lai, F.C.; Chang, C.C.; Wan, H.T. Effects of a skill demonstration video delivered by smartphone on facilitating nursing students’ skill competencies and self-confidence: A randomized controlled trial study. Nurse Educ. Today 2018, 66, 63–68. [Google Scholar] [CrossRef]
- Öztürk, D.; Dinç, L. Effect of web-based education on nursing students’ urinary catheterization knowledge and skills. Nurse Educ. Today 2014, 34, 802–808. [Google Scholar] [CrossRef]
- Beggs-Yeager, C.; Sharts-Hopko, N.; McDermott-Levy, R. The role of nurses in surveillance to enhance global health security: A delphi study. Nurs. Outlook 2021, 69, 1021–1029. [Google Scholar] [CrossRef]
- Kardong-Edgren, S.; Mulcock, P.M. Angoff method of setting cut scores for high-stakes testing: Foley catheter checkoff as an exemplar. Nurs. Educ. 2016, 41, 80–82. [Google Scholar] [CrossRef]
- Kardong-Edgren, S.; Breitkreuz, K.; Werb, M.; Foreman, S.; Ellertson, A. Evaluating the usability of a second-generation virtual reality game for refreshing sterile urinary catheterization skills. Nurs. Educ. 2019, 44, 137–141. [Google Scholar] [CrossRef]
- Stump, G.S.; Husman, J.; Brem, S.K. The nursing student self-efficacy scale: Development using item response theory. Nurs. Res. 2012, 61, 149–158. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control, 6th ed.; Freeman: New York, NY, USA, 1997. [Google Scholar]
- McMullan, M.; Jones, R.; Lea, S. Math anxiety, self-efficacy, and ability in British undergraduate nursing students. Res. Nurs. Health 2012, 35, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Robb, M. Self-efficacy with application to nursing education: A concept analysis. Nurs. Forum. 2012, 47, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Henderson, A.; Rowe, J.; Watson, K.; Hitchen-Holmes, D. Graduating nurses’ self-efficacy in palliative care practice: An exploratory study. Nurse Educ. Today 2016, 39, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Zengin, N.; Pınar, R.; Akinci, A.C.; Yildiz, H. Psychometric properties of the self-efficacy for clinical evaluation scale in Turkish nursing students. J. Clin. Nurs. 2014, 23, 976–984. [Google Scholar] [CrossRef]
- Henderson, A.; Harrison, P.; Rowe, J.; Edwards, S.; Barnes, M.; Henderson, S. Students take the lead for learning in practice: A process for building self-efficacy into undergraduate nursing education. Nurse Educ. Pract. 2018, 31, 14–19. [Google Scholar] [CrossRef] [Green Version]
- Oyelana, O.; Martin, D.; Scanlan, J.; Temple, B. Learner-centred teaching in a non-learner-centred world: An interpretive phenomenological study of the lived experience of clinical nursing faculty. Nurse Educ. Today 2018, 67, 118–123. [Google Scholar] [CrossRef]
- Mackintosh-Franklin, C. Pedagogical principles underpinning undergraduate nurse education in the UK: A review. Nurse Educ. Today 2016, 40, 118–122. [Google Scholar] [CrossRef]
- Betihavas, V.; Bridgman, H.; Kornhaber, R.; Cross, M. The evidence for ‘flipping out’: A systematic review of the flipped classroom in nursing education. Nurse Educ. Today 2016, 38, 15–21. [Google Scholar] [CrossRef]
- King, A.; Boysen-Osborn, M.; Cooney, R.; Mitzman, J.; Misra, A.; Williams, J.; Dulani, T.; Gottlieb, M. Curated collection for educators: Five key papers about the flipped classroom methodology. Cureus 2017, 9, e1801. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.K.; Chang, S.J.; Jang, S.J. Effects of the flipped classroom approach on the psychiatric nursing practicum course. J. Korean Acad. Psych. Ment. Health Nurs. 2017, 26, 196–203. [Google Scholar] [CrossRef]
- Green, R.D.; Schlairet, M.C. Moving toward heutagogical learning: Illuminating undergraduate nursing students’ experiences in a flipped classroom. Nurse Educ. Today 2017, 49, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Hew, K.F.; Lo, C.K. Flipped classroom improves student learning in health professions education: A meta-analysis. BMC Med. Educ. 2018, 18, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Jang, Y. Flipped learning with simulation in undergraduate nursing education. J. Nurs. Educ. 2017, 56, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Missildine, K.; Fountain, R.; Summers, L.; Gosselin, K. Flipping the classroom to improve student performance and satisfaction. J. Nurs. Educ. 2013, 52, 597–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ward, M.; Knowlton, M.C.; Laney, C.W. The flip side of traditional nursing education: A literature review. Nurse Educ. Pract. 2018, 29, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Abeysekera, L.; Dawson, P. Motivation and cognitive load in the flipped classroom: Definition, rationale and a call for research. High Educ. Res. Dev. 2015, 34, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Hu, R.; Gao, H.; Ye, Y.; Ni, Z.; Jiang, N.; Jiang, X. Effectiveness of flipped classrooms in Chinese baccalaureate nursing education: A meta-analysis of randomized controlled trials. Int. J. Nurs. Stud. 2018, 79, 94–103. [Google Scholar] [CrossRef]
- Xu, P.; Chen, Y.; Nie, W.; Wang, Y.; Song, T.; Li, H.; Li, J.; Yi, J.; Zhao, L. The effectiveness of a flipped classroom on the development of Chinese nursing students’ skill competence: A systematic review and meta-analysis. Nurse Educ. Today 2019, 80, 67–77. [Google Scholar] [CrossRef]
- Chu, T.L.; Wang, J.; Monrouxe, L.; Sung, Y.C.; Kuo, C.L.; Ho, L.H.; Lin, Y.E. The effects of the flipped classroom in teaching evidence based nursing: A quasi-experimental study. PLoS ONE 2019, 14, e0210606. [Google Scholar] [CrossRef]
- Zhu, L.; Lian, Z.; Engström, M. Use of a flipped classroom in ophthalmology courses for nursing, dental and medical students: A quasi-experimental study using a mixed-methods approach. Nurse Educ. Today 2020, 85, 104262. [Google Scholar] [CrossRef]
- Holland, A.; Smith, F.; McCrossan, G.; Adamson, E.; Watt, S.; Penny, K. Online video in clinical skills education of oral medication administration for undergraduate student nurses: A mixed methods, prospective cohort study. Nurse Educ. Today 2013, 33, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Salvendy, G. Development of a human information processing model for cognitive task analysis and design. Theor. Iss. Ergon. Sci. 2006, 7, 345–370. [Google Scholar] [CrossRef]
- Jokinen, P.; Mikkonen, I. Teachers’ experiences of teaching in a blended learning environment. Nurse Educ. Pract. 2013, 13, 524–528. [Google Scholar] [CrossRef]
- Simpson, V.; Richards, E. Flipping the classroom to teach population health: Increasing the relevance. Nurse Educ. Pract. 2015, 15, 162–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.C.Y. Using medical incidents to teach: Effects of vicarious experience on nursing students’ self-efficacy in performing urinary catheterization. J. Nurs. Educ. 2015, 54, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Critz, C.M.; Knight, D. Using the flipped classroom in graduate nursing education. Nurs. Educ. 2013, 38, 210–213. [Google Scholar] [CrossRef]
- Maxwell, K.L.; Wright, V.H. Evaluating the effectiveness of two teaching strategies to improve nursing students’ knowledge, skills, and attitudes about quality improvement and patient safety. Nurs. Educ. Perspect. 2016, 37, 291–292. [Google Scholar] [CrossRef]
- Peisachovich, E.H.; Murtha, S.; Phillips, A.; Messinger, G. Flipping the Classroom: A Pedagogical Approach to Applying Clinical Judgment by Engaging, Interacting, and Collaborating with Nursing Students. Learn. Teach. 2016, 5, 114–121. [Google Scholar] [CrossRef]
| Variable | Total (N = 139) | |
|---|---|---|
| n | % | |
| Sex | ||
| Male | 30 | 21.6 |
| Female | 109 | 78.4 |
| Age | 21.02 * | 6.11 ** |
| Previous studies | ||
| Completed high school | 114 | 82 |
| Professional training | 23 | 16.5 |
| University degree | 2 | 1.4 |
| Previous experience in hospitals or residences | ||
| Yes | 24 | 17.3 |
| No | 115 | 82.7 |
| Had seen a professional perform a urinary catheterization | ||
| Yes | 26 | 18.7 |
| No | 113 | 81.3 |
| Had previous opportunity to perform a urinary catheterization | ||
| Yes | 3 | 2.2 |
| No | 136 | 97.8 |
| Item | Pre-Test | Post-Test | ||
|---|---|---|---|---|
| M * | SD ** | M * | SD ** | |
| 32.55 | 27.42 | 71.37 | 25.25 |
| 95.32 | 10.85 | 97.19 | 8.68 |
| 76.22 | 27.032 | 84.82 | 23.23 |
| 63.35 | 32.10 | 87.59 | 15.97 |
| 90.04 | 15.61 | 96.26 | 8.62 |
| 62.52 | 33.03 | 95.40 | 10.91 |
| 96.12 | 9.59 | 97.77 | 6.37 |
| 90.50 | 13.63 | 95.14 | 10.37 |
| 57.27 | 31.24 | 90.43 | 14.63 |
| 88.49 | 19.14 | 94.32 | 12.22 |
| 79.10 | 21.06 | 92.37 | 12.75 |
| 49.86 | 33.62 | 90.18 | 13.49 |
| 31.58 | 28.137 | 70.04 | 21.89 |
| 57.84 | 33.63 | 93.71 | 11.48 |
| 46.96 | 33.19 | 92.66 | 14.06 |
| 38.20 | 31.30 | 96.65 | 87.40 |
| 44.96 | 33.73 | 90.51 | 14.78 |
| 51.83 | 32.39 | 88.85 | 16.15 |
| 62.48 | 30.29 | 94.24 | 9.47 |
| 30.22 | 28.70 | 78.88 | 17.96 |
| 30.72 | 29.33 | 82.30 | 17.70 |
| 36.33 | 32.55 | 86.19 | 17.042 |
| 30.65 | 27.77 | 84.75 | 18.74 |
| 68.92 | 27.54 | 95.68 | 78.97 |
| 49.35 | 34.99 | 85.32 | 19.31 |
| 77.34 | 28.14 | 93.45 | 13.11 |
| 43.81 | 33.60 | 87.23 | 17.27 |
| 57.19 | 36.09 | 92.45 | 12.73 |
| 86.04 | 19.95 | 94.39 | 10.84 |
| 81.94 | 22.83 | 93.45 | 10.54 |
| 86.04 | 21.08 | 93.81 | 14.07 |
| 95.11 | 10.17 | 95.40 | 13.20 |
| 88.67 | 80.37 | 89.28 | 17.51 |
| 39.78 | 31.74 | 80.58 | 19.62 |
| 42.29 | 23.57 | 75.04 | 14.39 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguilera-Manrique, G.; Gutiérrez-Puertas, L.; Gutiérrez-Puertas, V.; Ortiz-Rodríguez, B.; Márquez-Hernández, V.V. Evaluation of Urinary Catheterization Competency and Self-Efficacy in Nursing Students Using the Flipped Classroom Approach. Int. J. Environ. Res. Public Health 2022, 19, 15144. https://doi.org/10.3390/ijerph192215144
Aguilera-Manrique G, Gutiérrez-Puertas L, Gutiérrez-Puertas V, Ortiz-Rodríguez B, Márquez-Hernández VV. Evaluation of Urinary Catheterization Competency and Self-Efficacy in Nursing Students Using the Flipped Classroom Approach. International Journal of Environmental Research and Public Health. 2022; 19(22):15144. https://doi.org/10.3390/ijerph192215144
Chicago/Turabian StyleAguilera-Manrique, Gabriel, Lorena Gutiérrez-Puertas, Vanesa Gutiérrez-Puertas, Blanca Ortiz-Rodríguez, and Verónica V. Márquez-Hernández. 2022. "Evaluation of Urinary Catheterization Competency and Self-Efficacy in Nursing Students Using the Flipped Classroom Approach" International Journal of Environmental Research and Public Health 19, no. 22: 15144. https://doi.org/10.3390/ijerph192215144
APA StyleAguilera-Manrique, G., Gutiérrez-Puertas, L., Gutiérrez-Puertas, V., Ortiz-Rodríguez, B., & Márquez-Hernández, V. V. (2022). Evaluation of Urinary Catheterization Competency and Self-Efficacy in Nursing Students Using the Flipped Classroom Approach. International Journal of Environmental Research and Public Health, 19(22), 15144. https://doi.org/10.3390/ijerph192215144









