Social Frailty and Meaningful Activities among Community-Dwelling Older Adults with Heart Disease
Abstract
1. Introduction
2. Materials and Methods
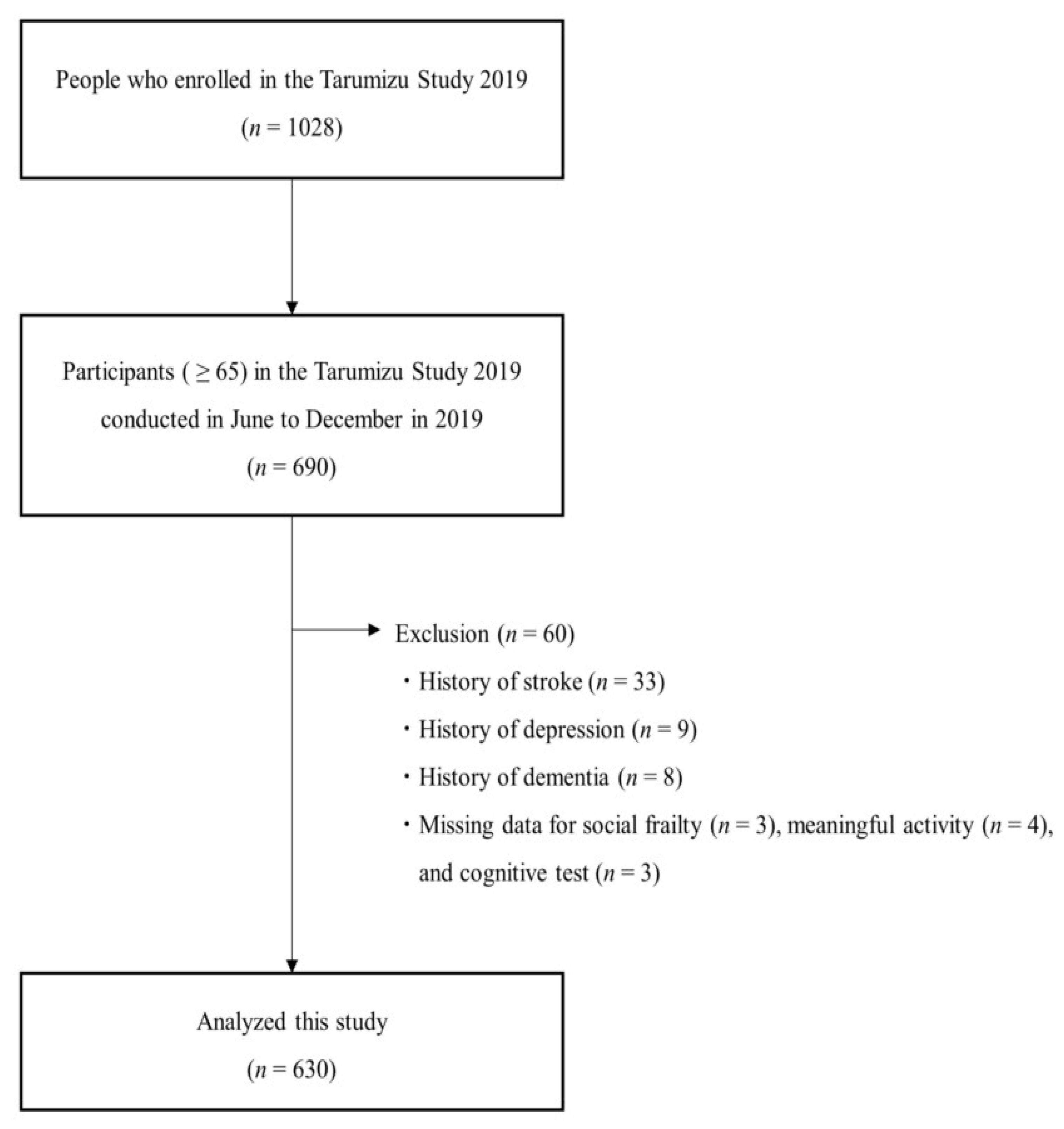
2.1. Participants
2.2. Measures
2.2.1. Determination of Heart Disease
2.2.2. Assessment of Social Frailty
2.2.3. Assessment of Meaningful Activities
2.2.4. Other Variables
2.3. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Association between Heart Disease and Social Frailty
3.3. Association between Heart Disease and the Five Elements of Social Frailty
3.4. Characteristics of Meaningful Activities in Those with and without Heart Disease
4. Discussion
4.1. Heart Disease and Social Frailty in Community-Dwelling Older Adults
4.2. Characteristics of Meaningful Activities of Community-Dwelling Older Adults with Heart Disease
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labor and Welfare. Patient Survey. 2017. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/kanja/17/index.html (accessed on 20 December 2021).
- Hata, J.; Ninomiya, T.; Hirakawa, Y.; Nagata, M.; Mukai, N.; Gotoh, S.; Fukuhara, M.; Ikeda, F.; Shikata, K.; Yoshida, D.; et al. Secular trends in cardiovascular disease and its risk factors in Japanese: Half-Century data from the Hisayama Study (1961–2009). Circulation 2013, 128, 1198–1205. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Vaes, B.; Depoortere, D.; Van Pottelbergh, G.; Matheï, C.; Neto, J.; Degryse, J. Association between traditional cardiovascular risk factors and mortality in the oldest old: Untangling the role of frailty. BMC Geriatr. 2017, 17, 234. [Google Scholar] [CrossRef] [PubMed]
- Gobbens, R.J.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M. Toward a conceptual definition of frail community dwelling older people. Nurs. Outlook 2010, 58, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Shimada, H.; Lee, S.; Doi, T.; Bae, S.; Tsutsumimoto, K.; Arai, H. Prevalence of Psychological Frailty in Japan: NCGG-SGS as a Japanese National Cohort Study. J. Clin. Med. 2019, 8, 1554. [Google Scholar] [CrossRef] [PubMed]
- Shimada, H.; Makizako, H.; Lee, S.; Doi, T.; Tsutsumimoto, K.; Harada, K.; Hotta, R.; Bae, S.; Nakakubo, S.; Suzuki, T. Impact of Cognitive Frailty on Daily Activities in Older Persons. J. Nutr. Health Aging 2016, 20, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Shimada, H.; Tsutsumimoto, K.; Lee, S.; Doi, T.; Nakakubo, S.; Hotta, R.; Suzuki, T. Social Frailty in Community-Dwelling Older Adults as a Risk Factor for Disability. J. Am. Med. Dir. Assoc. 2015, 16, 1003.e7–1003.e11. [Google Scholar] [CrossRef]
- Kleipool, E.E.; Hoogendijk, E.O.; Trappenburg, M.C.; Handoko, M.L.; Huisman, M.; Peters, M.J.; Muller, M. Frailty in Older Adults with Cardiovascular Disease: Cause, Effect or Both? Aging Dis. 2018, 9, 489–497. [Google Scholar] [CrossRef]
- Jujo, K.; Kagiyama, N.; Saito, K.; Kamiya, K.; Saito, H.; Ogasahara, Y.; Maekawa, E.; Konishi, M.; Kitai, T.; Iwata, K.; et al. Impact of Social Frailty in Hospitalized Elderly Patients With Heart Failure: A FRAGILE-HF Registry Subanalysis. J. Am. Heart Assoc. 2021, 10, e019954. [Google Scholar] [CrossRef]
- Shoemaker, M.J.; Mattern, M.; Scholten, H.; Zeitler, J.; Gore, S. Subjective Daily Physical Activity Measures in Heart Disease: A Systematic Review. J. Phys. Act. Health 2021, 18, 450–460. [Google Scholar] [CrossRef]
- Norberg, E.B.; Boman, K.; Löfgren, B.; Brännström, M. Occupational performance and strategies for managing daily life among the elderly with heart failure. Scand J. Occup. Ther. 2014, 21, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Miyata, H.; Maruta, M.; Makizako, H.; Han, G.; Ikeda, Y.; Nakamura, A.; Tokuda, K.; Shimokihara, S.; Akaida, S.; Hidaka, Y.; et al. Association between satisfaction with meaningful activities and social frailty in community-dwelling Japanese older adults. Arch. Gerontol. Geriatr. 2022, 100, 104665. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, M.; Kamiya, K.; Hamazaki, N.; Nozaki, K.; Saito, H.; Saito, K.; Ogasahara, Y.; Maekawa, E.; Konishi, M.; Kitai, T.; et al. Work status before admission relates to prognosis in older patients with heart failure partly through social frailty. J. Cardiol. 2022, 79, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Klinpudtan, N.; Kabayama, M.; Godai, K.; Gondo, Y.; Masui, Y.; Akagi, Y.; Srithumsuk, W.; Kiyoshige, E.; Sugimoto, K.; Akasaka, H.; et al. Association between physical function and onset of coronary heart disease in a cohort of community-dwelling older populations: The SONIC study. Arch. Gerontol. Geriatr. 2021, 95, 104386. [Google Scholar] [CrossRef]
- Benhar, H.; Idri, A.; Fernández-Alemán, J.L. Data preprocessing for heart disease classification: A systematic literature review. Comput. Methods Programs Biomed. 2020, 195, 105635. [Google Scholar] [CrossRef]
- Japan Socio-Gerontological Society. Available online: http://184.73.219.23/rounenshakai/other/frail.htm (accessed on 5 November 2022).
- Matsue, Y.; Kamiya, K.; Saito, H.; Saito, K.; Ogasahara, Y.; Maekawa, E.; Konishi, M.; Kitai, T.; Iwata, K.; Jujo, K.; et al. Prevalence and prognostic impact of the coexistence of multiple frailty domains in elderly patients with heart failure: The FRAGILE-HF cohort study. Eur. J. Heart Fail. 2020, 22, 2112–2119. [Google Scholar] [CrossRef]
- Maruta, M.; Makizako, H.; Ikeda, Y.; Miyata, H.; Nakamura, A.; Han, G.; Shimokihara, S.; Tokuda, K.; Kubozono, T.; Ohishi, M.; et al. Associations between Depressive Symptoms and Satisfaction with Meaningful Activities in Community-Dwelling Japanese Older Adults. J. Clin. Med. 2020, 9, 795. [Google Scholar] [CrossRef]
- Tomori, K.; Uezu, S.; Kinjo, S.; Ogahara, K.; Nagatani, R.; Higashi, T. Utilization of the iPad application: Aid for Decision-making in Occupation Choice. Occup Ther. Int. 2012, 19, 88–97. [Google Scholar] [CrossRef]
- Tomori, K.; Saito, Y.; Nagayama, H.; Seshita, Y.; Ogahara, K.; Nagatani, R.; Higashi, T. Reliability and validity of individualized satisfaction score in aid for decision-making in occupation choice. Disabil. Rehabil. 2013, 35, 113–117. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Park, H.; Doi, T.; Yoshida, D.; Uemura, K.; Tsutsumimoto, K.; Suzuki, T. Evaluation of multidimensional neurocognitive function using a tablet personal computer: Test-retest reliability and validity in community-dwelling older adults. Geriatr. Gerontol. Int. 2013, 13, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Shimada, H.; Doi, T.; Tsutsumimoto, K.; Hotta, R.; Nakakubo, S.; Makino, K.; Suzuki, T. Comorbid Mild Cognitive Impairment and Depressive Symptoms Predict Future Dementia in Community Older Adults: A 24-Month Follow-Up Longitudinal Study. J. Alzheimers. Dis. 2016, 54, 1473–1482. [Google Scholar] [CrossRef] [PubMed]
- Kume, Y.; Takahashi, T.; Itakura, Y.; Lee, S.; Makizako, H.; Ono, T.; Shimada, H.; Ota, H. Polypharmacy and Lack of Joy Are Related to Physical Frailty among Northern Japanese Community-Dwellers from the ORANGE Cohort Study. Gerontology 2021, 67, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Kume, Y.; Kodama, A. Association between on-road driving performance test and usual walking speed or sustainable attention in the elderly; Preliminary survey. Traffic Inj. Prev. 2022, 23, 57–60. [Google Scholar] [CrossRef]
- Kondo, R.; Miyano, I.; Lee, S.; Shimada, H.; Kitaoka, H. Association between self-reported night sleep duration and cognitive function among older adults with intact global cognition. Int. J. Geriatr. Psychiatry 2021, 36, 766–774. [Google Scholar] [CrossRef]
- Iwasa, H.; Masui, Y.; Inagaki, H.; Yoshida, Y.; Shimada, H.; Otsuka, R.; Kikuchi, K.; Nonaka, K.; Yoshida, H.; Suzuki, T. Assessing competence at a higher level among older adults: Development of the Japan Science and Technology Agency Index of Competence (JST-IC). Aging Clin. Exp. Res. 2018, 30, 383–393. [Google Scholar] [CrossRef]
- Almeida, O.P.; Almeida, S.A. Short versions of the geriatric depression scale: A study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int. J. Geriatr. Psychiatry 1999, 14, 858–865. [Google Scholar] [CrossRef]
- de Craen, A.J.; Heeren, T.J.; Gussekloo, J. Accuracy of the 15-item geriatric depression scale (GDS-15) in a community sample of the oldest old. Int. J. Geriatr. Psychiatry 2003, 18, 63–66. [Google Scholar] [CrossRef]
- Yesavage, J.A. Geriatric Depression Scale. Psychopharmacol. Bull 1988, 24, 709–711. [Google Scholar]
- Park, H.; Jang, I.Y.; Lee, H.Y.; Jung, H.W.; Lee, E.; Kim, D.H. Screening Value of Social Frailty and Its Association with Physical Frailty and Disability in Community-Dwelling Older Koreans: Aging Study of PyeongChang Rural Area. Int. J. Environ. Res. Public Health 2019, 16, 2809. [Google Scholar] [CrossRef]
- Tsutsumimoto, K.; Doi, T.; Makizako, H.; Hotta, R.; Nakakubo, S.; Makino, K.; Suzuki, T.; Shimada, H. Association of Social Frailty With Both Cognitive and Physical Deficits Among Older People. J. Am. Med. Dir. Assoc. 2017, 18, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Barth, J.; Schneider, S.; von Känel, R. Lack of social support in the etiology and the prognosis of coronary heart disease: A systematic review and meta-analysis. Psychosom. Med. 2010, 72, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Lorente, L.; Tordera, N.; Peiró, J.M. How Work Characteristics Are Related to European Workers’ Psychological Well-Being. A Comparison of Two Age Groups. Int. J. Environ. Res. Public Health 2018, 15, 127. [Google Scholar] [CrossRef] [PubMed]
- Hirase, T.; Makizako, H.; Okubo, Y.; Lord, S.R.; Inokuchi, S.; Okita, M. Chronic pain is independently associated with social frailty in community-dwelling older adults. Geriatr. Gerontol. Int. 2019, 19, 1153–1156. [Google Scholar] [CrossRef]
- Fujiwara, Y.; Shinkai, S.; Kumagai, S.; Amano, H.; Yoshida, Y.; Yoshida, H.; Kim, H.; Suzuki, T.; Ishizaki, T.; Haga, H.; et al. Longitudinal changes in higher-level functional capacity of an older population living in a Japanese urban community. Arch. Gerontol. Geriatr. 2003, 36, 141–153. [Google Scholar] [CrossRef]
- Kodama, A.; Kume, Y.; Lee, S.; Makizako, H.; Shimada, H.; Takahashi, T.; Ono, T.; Ota, H. Impact of COVID-19 Pandemic Exacerbation of Depressive Symptoms for Social Frailty from the ORANGE Registry. Int. J. Environ. Res. Public Health 2022, 19, 986. [Google Scholar] [CrossRef]
- Aung, M.N.; Moolphate, S.; Aung, T.N.; Katonyoo, C.; Khamchai, S.; Wannakrairot, P. The social network index and its relation to later-life depression among the elderly aged ≥80 years in Northern Thailand. Clin. Interv. Aging 2016, 11, 1067–1074. [Google Scholar] [CrossRef]
- Uchmanowicz, I.; Wleklik, M.; Gobbens, R.J. Frailty syndrome and self-care ability in elderly patients with heart failure. Clin. Interv. Aging 2015, 10, 871–877. [Google Scholar] [CrossRef]
- Reed, K.L.; Sanderson, S.N. Concepts of Occupational Therapy; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1999. [Google Scholar]
- Xie, B.; Ma, C. Effect of social participation on the development of physical frailty: Do type, frequency and diversity matter? Maturitas 2021, 151, 48–54. [Google Scholar] [CrossRef]
- Katsi, V.; Georgiopoulos, G.; Mitropoulou, P.; Kontoangelos, K.; Kollia, Z.; Tzavara, C.; Soulis, D.; Toutouzas, K.; Oikonomou, D.; Aimo, A.; et al. Exercise tolerance and quality of life in patients with known or suspected coronary artery disease. Qual. Life Res. 2021, 30, 2541–2550. [Google Scholar] [CrossRef]
- Toback, M.; Clark, N. Strategies to improve self-management in heart failure patients. Contemp. Nurse 2017, 53, 105–120. [Google Scholar] [CrossRef] [PubMed]
| With Heart Disease (n = 79) | Without Heart Disease (n = 551) | p-Value | |
|---|---|---|---|
| Age, mean ± SD (years) | 76.3 ± 6.4 | 73.9 ± 6.3 | <0.001 a |
| Female, n (%) | 38 (48.1%) | 358 (65.0%) | 0.004 b |
| Medications, mean ± SD (numbers) | 6.5 ± 3.7 | 2.9 ± 2.8 | <0.001 b |
| Married, n (%) | 74 (93.7%) | 530 (96.2%) | 0.293 a |
| Educational history, mean ± SD (years) | 11.1 ± 2.1 | 11.5 ± 2.2 | 0.238 a |
| History of hypertension, n (%) | 37 (46.8%) | 269 (48.8%) | 0.810 a |
| Poor cognitive status, n (%) | 25 (31.6%) | 110 (20.0%) | 0.018 b |
| Physical frailty, n (%) | 11 (13.9%) | 37 (6.7%) | 0.011 b |
| slowness, n (%) | 12 (15.2%) | 48 (8.7%) | 0.067 b |
| weakness, n (%) | 21 (26.6%) | 70 (12.7%) | <0.001 b |
| exhaustion, n (%) | 17 (21.5%) | 99 (18.0%) | 0.446 b |
| low physical activity, n (%) | 15 (19.0%) | 88 (16.0%) | 0.498 b |
| weight loss, n (%) | 17 (21.5%) | 99 (18.0%) | 0.446 b |
| Higher-level competence, mean ± SD (points) | 10.6 ± 3.2 | 12.0 ± 3.0 | <0.001 a |
| Social frailty, n (%) | 26 (32.9%) | 91 (16.5%) | 0.002 b |
| Crude Model | Adjusted Model 1 | Adjusted Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p- Value | OR | 95% CI | p- Value | OR | 95% CI | p- Value | |
| Heart disease | 2.48 | 1.47–4.17 | 0.001 | 2.20 | 1.28–3.74 | 0.004 | 2.21 | 1.01–4.83 | 0.047 |
| With Heart Disease (n = 79) | Without Heart Disease (n = 551) | ES | p-Value a | |
|---|---|---|---|---|
| going out less frequently compared with last year (yes), n (%) | 18 (22.8%) | 82 (14.9%) | 0.07 | 0.072 |
| not visiting friends sometimes (yes), n (%) | 20 (25.3%) | 102 (18.5%) | 0.06 | 0.152 |
| not feeling helpful to friends or family (yes), n (%) | 11 (13.9%) | 33 (6.0%) | 0.10 | 0.010 |
| living alone (yes), n (%) | 26 (32.9%) | 152 (27.6%) | 0.04 | 0.326 |
| not talking with someone every day (yes), n (%) | 13 (16.5%) | 50 (9.1%) | 0.08 | 0.041 |
| With Heart Disease (n = 79) | Without Heart Disease (n = 551) | ES | p-Value | |
|---|---|---|---|---|
| Category of meaningful activities, n (%) | 0.09 | 0.549 b | ||
| self-care | 6 (7.6%) | 70 (12.7%) | ||
| mobility | 0 (0%) | 6 (1.1%) | ||
| domestic life | 12 (15.2%) | 85 (15.4%) | ||
| work/education | 6 (7.6%) | 31 (5.6%) | ||
| interpersonal interaction | 14 (17.7%) | 93 (16.9%) | ||
| social life | 4 (5.1%) | 54 (9.8%) | ||
| sport | 10 (12.7%) | 64 (11.6%) | ||
| leisure | 27 (34.2%) | 148 (26.9%) | ||
| Satisfaction of meaningful activities, Median (IQR) | 5 (4–5) | 5 (4–5) | 0.01 | 0.847 c |
| Performance of meaningful activities, Median (IQR) | 9 (7–10) | 9 (7–10) | 0.03 | 0.452 c |
| Frequency of meaningful activities, mean ± SD (days) | 212.2 ± 147.3 | 247.7 ± 143.9 | 0.25 | 0.041 a |
| With Heart Disease (n = 79) | Without Heart Disease (n = 551) | ES | p-Value | |
|---|---|---|---|---|
| self-care, mean ± SD (days) | 260.5 ± 143.8 (n = 6) | 343.4 ± 75.6 (n = 70) | 0.91 | 0.020 a |
| mobility, mean ± SD (days) | (n = 0) | 330.0 ± 54.2 (n = 6) | ||
| domestic life, mean ± SD (days) | 318.2 ± 113.6 (n = 12) | 325.2 ± 101.7 (n = 85) | 0.07 | 0.826 a |
| work/education, mean ± SD (days) | 234.3 ± 130.4 (n = 6) | 260.6 ± 115.8 (n = 31) | 0.22 | 0.621 a |
| interpersonal interaction, mean ± SD (days) | 112.8 ± 111.7 (n = 14) | 214.5 ± 153.7 (n = 93) | 0.68 | 0.019 a |
| social life, mean ± SD (days) | 129.3 ± 161.6 (n = 4) | 138.3 ± 144.1 (n = 54) | 0.06 | 0.905 a |
| sport, mean ± SD (days) | 170.8 ± 121.5 (n = 10) | 192.2 ± 136.6 (n = 64) | 0.16 | 0.642 a |
| leisure, mean ± SD (days) | 228.6 ± 157.9 (n = 27) | 236.6 ± 145.2 (n = 148) | 0.05 | 0.796 a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akasaki, Y.; Tabira, T.; Maruta, M.; Makizako, H.; Miyata, M.; Han, G.; Ikeda, Y.; Nakamura, A.; Shimokihara, S.; Hidaka, Y.; et al. Social Frailty and Meaningful Activities among Community-Dwelling Older Adults with Heart Disease. Int. J. Environ. Res. Public Health 2022, 19, 15167. https://doi.org/10.3390/ijerph192215167
Akasaki Y, Tabira T, Maruta M, Makizako H, Miyata M, Han G, Ikeda Y, Nakamura A, Shimokihara S, Hidaka Y, et al. Social Frailty and Meaningful Activities among Community-Dwelling Older Adults with Heart Disease. International Journal of Environmental Research and Public Health. 2022; 19(22):15167. https://doi.org/10.3390/ijerph192215167
Chicago/Turabian StyleAkasaki, Yoshihiko, Takayuki Tabira, Michio Maruta, Hyuma Makizako, Masaaki Miyata, Gwanghee Han, Yuriko Ikeda, Atsushi Nakamura, Suguru Shimokihara, Yuma Hidaka, and et al. 2022. "Social Frailty and Meaningful Activities among Community-Dwelling Older Adults with Heart Disease" International Journal of Environmental Research and Public Health 19, no. 22: 15167. https://doi.org/10.3390/ijerph192215167
APA StyleAkasaki, Y., Tabira, T., Maruta, M., Makizako, H., Miyata, M., Han, G., Ikeda, Y., Nakamura, A., Shimokihara, S., Hidaka, Y., Kamasaki, T., Kubozono, T., & Ohishi, M. (2022). Social Frailty and Meaningful Activities among Community-Dwelling Older Adults with Heart Disease. International Journal of Environmental Research and Public Health, 19(22), 15167. https://doi.org/10.3390/ijerph192215167








