Proposed Safety Guidelines for Patient Assistants in an Open MRI Environment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Transmit RF Coil Modeling
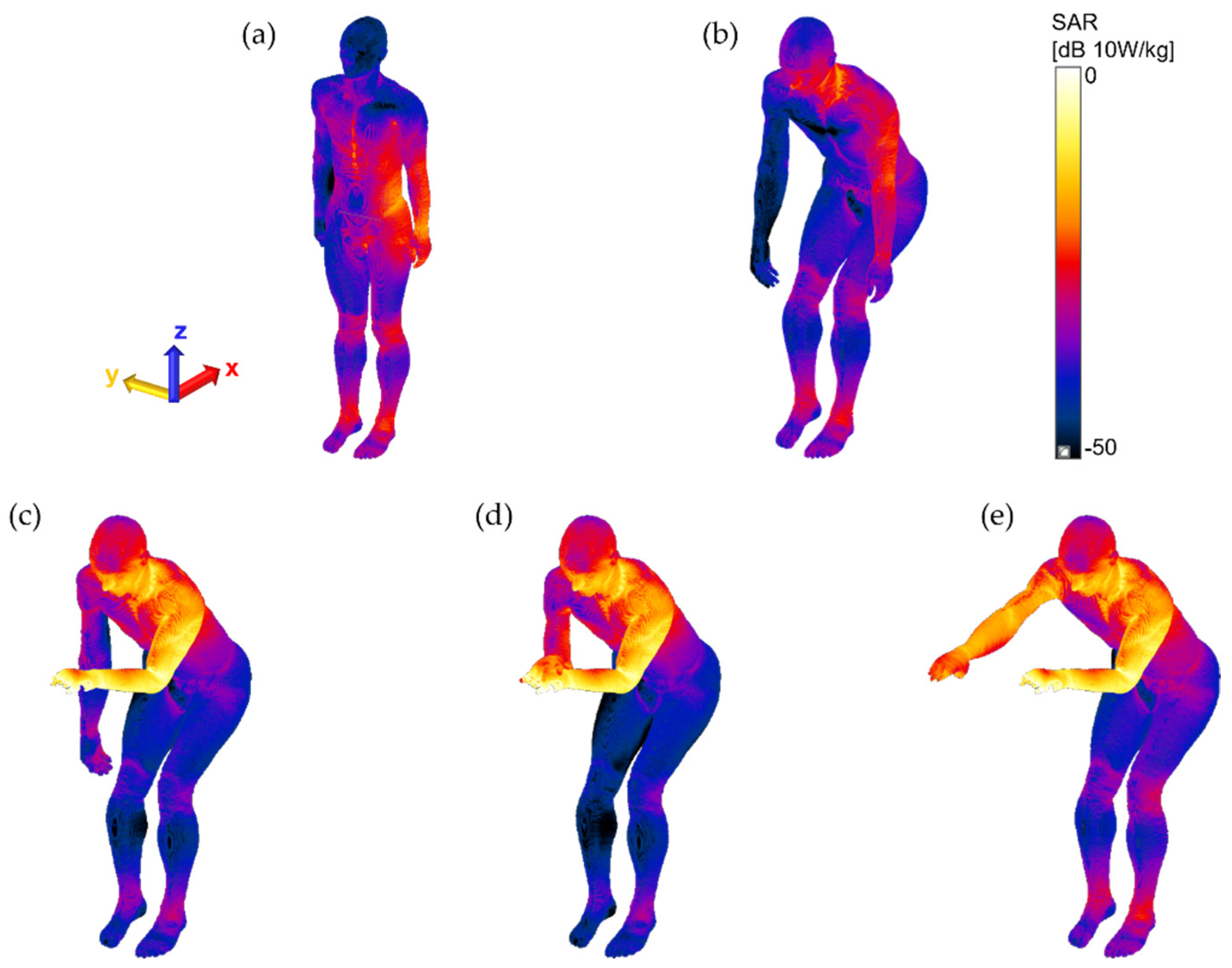
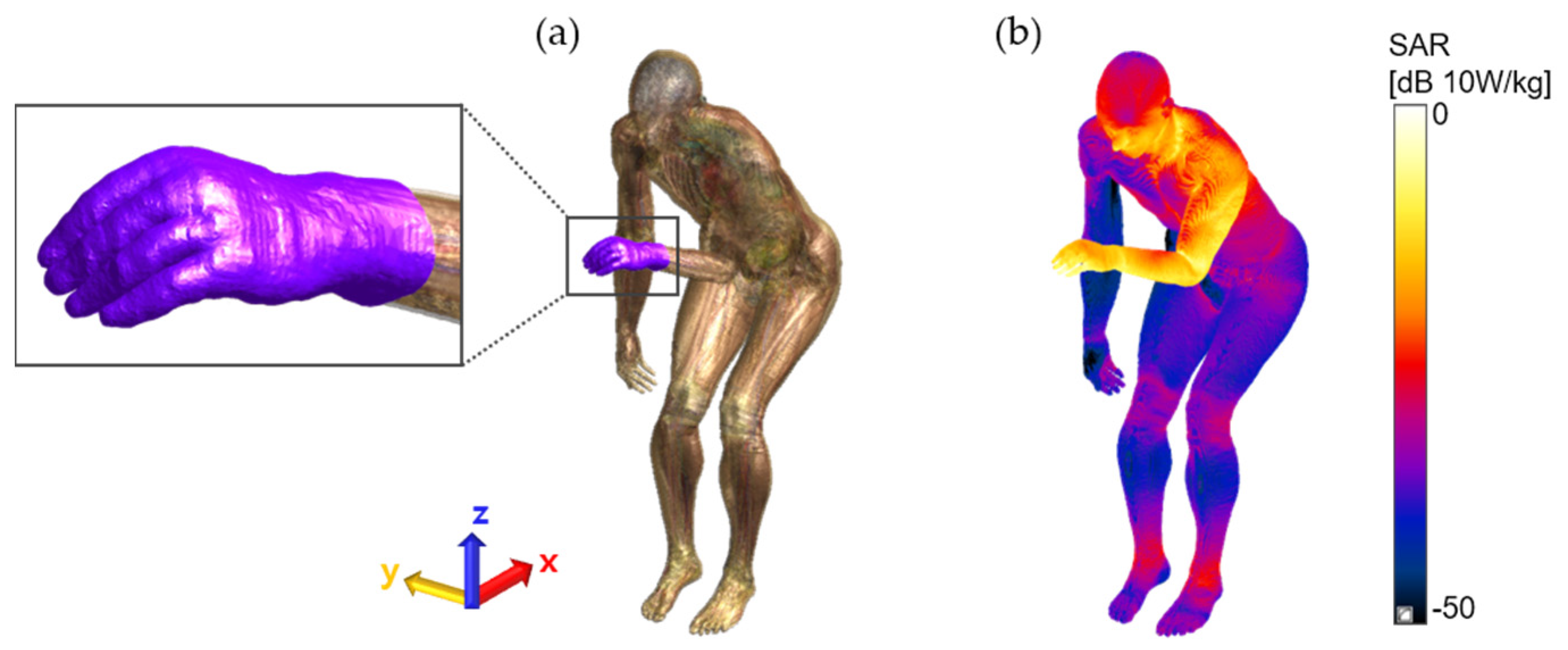
2.2. Numerical Human Body Models and RF Exposure Scenarios
3. Results and Discussion
4. Conclusions
- The patient assistants must not hold the patient’s body during the MRI scans unless otherwise instructed;
- If patient contact is required, the patient assistants must wear electrically insulated gloves whenever they are in the MRI scan room;
- The patient assistants must not touch any cables, equipment, or electronics of the MR scanner, even wearing insulating gloves.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Commission on Non-Ionizing Radiation Protection (ICNIRP). Guidelines for limiting exposure to time-varying electric, magnetic and electromagnetic fields (up to 300 GHz). Health Phys. 1998, 74, 494–522. [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP). Guidelines for limiting exposure to time-varying electric, magnetic and electromagnetic fields (1 Hz to 100 kHz). Health Phys. 2010, 99, 818–836. [Google Scholar] [CrossRef] [PubMed]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP). Guidelines for limiting exposure to time-varying electric, magnetic and electromagnetic fields (100 kHz to 300 GHz). Health Phys. 2020, 118, 483–524. [Google Scholar] [CrossRef]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP). Medical magnetic resonance (MR) procedures: Protection of patients. Health Phys. 2004, 87, 197–216. [Google Scholar] [CrossRef] [PubMed]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP). Statement amendment to the ICNIRP 2009 statement on medical magnetic resonance (MR) procedures: Protection of patients. Health Phys. 2009, 97, 259–261. [Google Scholar] [CrossRef] [PubMed]
- International Electrotechnical Commission (IEC). Chapter 201.12. IEC 60601-2-33: Medical Electrical Equipment-Part 2–33: Particular Requirements for the Basic Safety and Essential Performance of Magnetic Resonance Equipment for Medical Diagnosis. 2022. Available online: https://webstore.iec.ch/publication/67211 (accessed on 14 November 2022).
- Regulating Medicines and Medical Devices (MHRA). Safety Guidelines for Magnetic Resonance Imaging Equipment in Clinical Use; 2021. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/958486/MRI_guidance_2021-4-03c.pdf (accessed on 14 November 2022).
- International Society for Magnetic Resonance in Medicine (ISMRM). Best Practices for Safety Testing of Experimental RF Hardware. 2022. Available online: https://www.ismrm.org/safety/RF_Hardware_Safety_Testing_2022-03.pdf (accessed on 14 November 2022).
- Rianne, S.; Sachiko, Y.-S. Occupational exposure to electromagnetic fields from medical sources. Ind. Health 2018, 56, 96–105. [Google Scholar]
- Rathebe, R.; Weyers, C.; Raphela, F. A health and safety model for occupational exposure to radiofrequency fields and static magnetic fields from 1.5 and 3 T MRI scanners. Health Technol. 2019, 10, 39–50. [Google Scholar] [CrossRef]
- Huss, A.; Özdemir, E.; Schaap, K.; Kromhout, H. Occupational exposure to MRI-related magnetic stray fields and sleep quality among MRI-Technicians—A cross-sectional study in the Netherlands. Int. J. Hyg. Environ. Health. 2021, 231, 113636. [Google Scholar] [CrossRef]
- Hartwig, V.; Virgili, G.; Mattei, F.; Biagini, C.; Romeo, S.; Zeni, O.; Scarfi, M.R.; Massa, R.; Campanella, F.; Landini, L.; et al. Occupational exposure to electromagnetic fields in magnetic resonance environment: An update on regulation, exposure assessment techniques, health risk evaluation, and surveillance. Med. Biol. Eng. Comput. 2022, 60, 297–320. [Google Scholar] [CrossRef]
- Cho, Y.; Yoo, H. RF heating of implants in MRI: Electromagnetic analysis and solutions. Investig. Magn. Reson. Imaging 2020, 24, 67–75. [Google Scholar] [CrossRef]
- Fujimot, K.; Angelone, L.M.; Lucano, E.; Rajan, S.S.; Lacono, M.I. Radio-frequency safety assessment of stents in blood vessels during magnetic resonance imaging. Front. Physiol. 2018, 9, 1439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Golestanirad, L.; Rahsepar, A.A.; Kirsch, J.E.; Suwa, K.; Collins, J.C.; Angelone, L.M.; Keil, B.; Passman, R.S.; Bonmassar, G.; Serano, P.; et al. Changes in the specific absorption rate (SAR) of radiofrequency energy in patients with retained cardiac leads during MRI at 1.5 T and 3 T. Magn. Reson. Med. 2019, 81, 653–669. [Google Scholar] [CrossRef] [PubMed]
- Rahsepar, A.A.; Zimmerman, S.L.; Hansford, R.; Guttman, M.A.; Castro, V.; McVeigh, D.; Kirsch, J.E.; Halperin, H.R.; Nazarian, S. The relationship between MRI radiofrequency energy and function of nonconditional implanted cardiac devices: A prospective evaluation. Radiology 2020, 295, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.; Wang, Z.J. Measurement and evaluation of specific absorption rate and temperature elevation caused by an artificial hip joint during MRI scanning. Sci. Rep. 2021, 11, 1134. [Google Scholar] [CrossRef] [PubMed]
- Rathebe, P.; Weyers, C.; Raphela, F. Exposure levels of radiofrequency magnetic fields and static magnetic fields in 1.5 and 3.0 T MRI units. SN Appl. Sci. 2021, 3, 157. [Google Scholar] [CrossRef]
- Murbach, M.; Neufeld, E.; Kainz, W.; Pruessmann, K.P.; Kuster, N. Whole-body and local RF absorption in human models as a function of anatomy and position within 1.5T body coil. Magn. Reson. Med. 2013, 71, 839–845. [Google Scholar] [CrossRef]
- Seo, J.H.; Noh, Y.; Kim, K.N.; Ryu, Y.C. Evaluation of the specific absorption rate for simultaneous multi frequency RF excitation in 7-T magnetic resonance imaging. J. Magn. 2017, 22, 637–641. [Google Scholar] [CrossRef]
- Liu, W.; Wang, H.; Zhang, P.; Li, C.; Sun, J.; Chen, Z.; Xing, S.; Liang, P.; Wu, T. Statistical evaluation of radiofrequency exposure during magnetic resonant imaging; application of whole-body individual human model and body motion in the coil. Int. J. Environ. Res. Public Health 2019, 16, 1069. [Google Scholar] [CrossRef] [Green Version]
- Hong, S.E.; Oh, S.; Choi, H.D. RF exposure assessment for various poses of patient assistant in open MRI environment. Appl. Sci. 2021, 11, 4947. [Google Scholar] [CrossRef]
- Collins, C.M.; Wang, Z. Calculation of radiofrequency electromagnetic fields and their effects in MRI of human subjects. Magn. Reson. Med. 2011, 65, 1470–1482. [Google Scholar] [CrossRef]
- Wei, S.; Yang, W.; Wang, H.; Chen, L. Analysis of a planar transmit coil used for vertical field MRI. In Proceedings of the 4th International Conference on Biomedical Engineering and Informatics, Shanghai, China, 15–17 October 2011; pp. 118–121. [Google Scholar]
- Boskamp, E.B. Flat RF body coil design for open MRI. In Proceedings of the 22nd Annual EMBS International Conference, Chicago, IL, USA, 23–28 July 2000; pp. 2387–2389. [Google Scholar]
- Collins, C.M.; Smith, M.B. Signal–to–noise ratio and absorbed power as functions of main magnetic field strength, and definition of “90°” RF pulse for the head in the birdcage coil. Magn. Reson. Med. 2001, 45, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Christ, A.; Kainz, W.; Hahn, E.G.; Honegger, K.; Zefferer, M.; Neufeld, E.; Rascher, W.; Janka, R.; Bautz, W.; Chen, J.; et al. The virtual family-development of surface-based anatomical models of two adults and two children for dosimetric simulations. Phys. Med. Biol. 2010, 55, N23–N38. [Google Scholar] [CrossRef] [PubMed]
- Gosselin, M.C.; Neufeld, E.; Moser, H.; Huber, E.; Farcito, S.; Gerber, L.; Jedensjö, M.; Hilber, I.; Di Gennaro, F.D.; Lloyd, B.; et al. Development of a new generation of high-resolution anatomical models for medical device evaluation: The virtual population 3.0. Phys. Med. Biol. 2014, 59, 5287–5303. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Role | Name (Gender) | Age | Height (cm)/Weight (kg) | # of Tissue |
|---|---|---|---|---|
| Patient assistant | Duke (male) | 34 | 173/70 | 77 |
| Patient | Billie (female) | 11 | 146/36 | 75 |
| Subject | Pose 1 | Max. 10 g SAR [W/kg] 2 | Location of Max. 10 g SAR 2 |
|---|---|---|---|
| Patient assistant | 1: standing | 0.1881 | left pelvis |
| 2: sitting | 0.1041 | left shoulder–neck | |
| 3: one hand placed | 5.2606 | left hand (at the edge of RF coil) | |
| 4: two hands stacked up | 4.7715 | left hand (at the edge of RF coil) | |
| 5: two hands on hand and thigh | 4.5892 | left hand (at the edge of RF coil) | |
| Patient | 1: standing | 18.0826 | left thumb–thigh (at the edge of RF coil) |
| 2: sitting | 18.2466 | left thumb–thigh (at the edge of RF coil) | |
| 3: one hand placed | 18.6861 | left thumb–thigh (at the edge of RF coil) | |
| 4: two hands stacked up | 18.6014 | left thumb–thigh (at the edge of RF coil) | |
| 5: two hands on hand and thigh | 17.3428 | left thumb–thigh (at the edge of RF coil) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, S.; Hong, S.-E.; Choi, H.-D. Proposed Safety Guidelines for Patient Assistants in an Open MRI Environment. Int. J. Environ. Res. Public Health 2022, 19, 15185. https://doi.org/10.3390/ijerph192215185
Oh S, Hong S-E, Choi H-D. Proposed Safety Guidelines for Patient Assistants in an Open MRI Environment. International Journal of Environmental Research and Public Health. 2022; 19(22):15185. https://doi.org/10.3390/ijerph192215185
Chicago/Turabian StyleOh, Sukhoon, Seon-Eui Hong, and Hyung-Do Choi. 2022. "Proposed Safety Guidelines for Patient Assistants in an Open MRI Environment" International Journal of Environmental Research and Public Health 19, no. 22: 15185. https://doi.org/10.3390/ijerph192215185






