Stability of Attention Performance of Adults with ADHD over Time: Evidence from Repeated Neuropsychological Assessments in One-Month Intervals
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
2.2.1. Self-Report Scales of ADHD Symptoms
2.2.2. Assessment of Selective Attention and Vigilance
Selective Attention
Vigilance
2.3. Procedure
2.4. Statistical Analysis
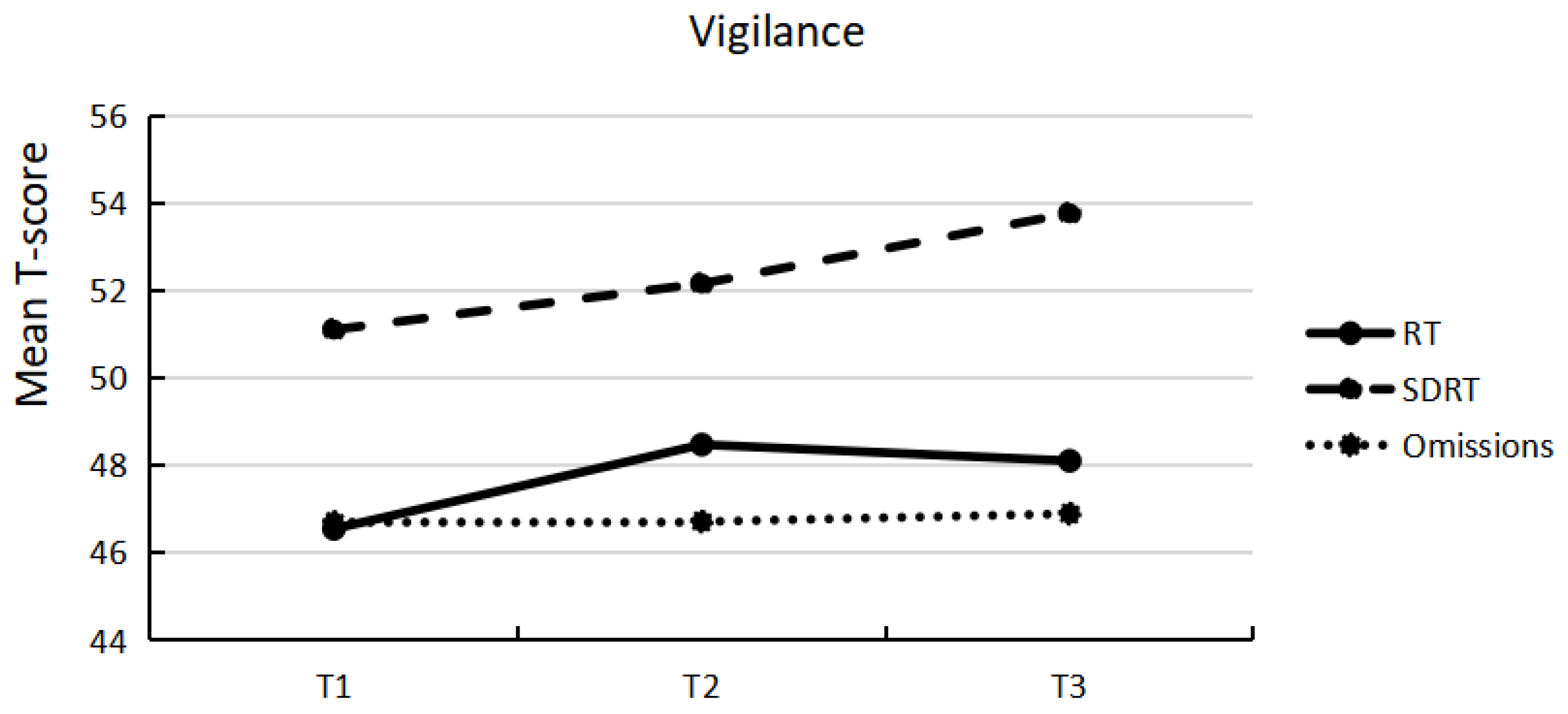
3. Results
4. Discussion
5. Limitations and Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing, Inc.: Washington, DC, USA, 2013. [Google Scholar]
- Song, P.; Zha, M.; Yang, Q.; Zhang, Y.; Li, X.; Rudan, I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. J. Glob. Health 2021, 11, 1965–1969. [Google Scholar] [CrossRef] [PubMed]
- Gmehlin, D.; Fuermaier, A.B.; Walther, S.; Tucha, L.; Koerts, J.; Lange, K.W.; Tucha, O.; Weisbrod, M.; Aschenbrenner, S. Attentional lapses of adults with attention deficit hyperactivity disorder in tasks of sustained attention. Arch. Clin. Neuropsychol. 2016, 31, 343–357. [Google Scholar] [CrossRef] [PubMed]
- Tucha, L.; Fuermaier, A.; Koerts, J.; Buggenthin, R.; Aschenbrenner, S.; Weisbrod, M.; Thome, J.; Lange, K.W.; Tucha, O. Sustained attention in adult ADHD: Time-on-task effects of various measures of attention. J. Neural Transm. 2017, 124, 39–53. [Google Scholar] [CrossRef] [PubMed]
- Onandia-Hinchado, I.; Pardo-Palenzuela, N.; Diaz-Orueta, U. Cognitive characterization of adult attention deficit hyperactivity disorder by domains: A systematic review. J. Neural Transm. 2021, 128, 893–937. [Google Scholar] [CrossRef] [PubMed]
- Schoechlin, C.; Engel, R.R. Neuropsychological performance in adult attention-deficit hyperactivity disorder: Meta-analysis of empirical data. Arch. Clin. Neuropsychol. 2005, 20, 727–744. [Google Scholar] [CrossRef]
- Fuermaier, A.; Tucha, L.; Koerts, J.; Aschenbrenner, S.; Kaunzinger, I.; Hauser, J.; Weisbrod, M.; Lange, K.W.; Tucha, O. Cognitive impairment in adult ADHD—Perspective matters! Neuropsychology 2015, 29, 45. [Google Scholar] [CrossRef] [PubMed]
- Tucha, O.; Mecklinger, L.; Laufkoetter, R.; Klein, H.; Walitza, S.; Lange, K.W. Methylphenidate-induced improvements of various measures of attention in adults with attention deficit hyperactivity disorder. J. Neural Transm. 2006, 113, 1575–1592. [Google Scholar] [CrossRef]
- Coghill, D.R.; Seth, S.; Matthews, K. A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in attention deficit hyperactivity disorder: Advancing beyond the three-pathway models. Psychol. Med. 2014, 44, 1989–2001. [Google Scholar] [CrossRef]
- Fabio, R.A.; Caprì, T. The executive functions in a sample of Italian adults with ADHD: Attention, response inhibition and planning/organization. Mediterr. J. Clin. Psychol. 2017, 5. [Google Scholar]
- Tucha, L.; Tucha, O.; Sontag, T.A.; Stasik, D.; Laufkötter, R.; Lange, K.W. Differential effects of methylphenidate on problem solving in adults with ADHD. J. Atten. Disord. 2011, 15, 161–173. [Google Scholar] [CrossRef]
- Alderson, R.M.; Kasper, L.J.; Hudec, K.L.; Patros, C.H. Attention-deficit/hyperactivity disorder (ADHD) and working memory in adults: A meta-analytic review. Neuropsychology 2013, 27, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Skodzik, T.; Holling, H.; Pedersen, A. Long-term memory performance in adult ADHD: A meta-analysis. J. Atten. Disord. 2017, 21, 267–283. [Google Scholar] [CrossRef] [PubMed]
- Fuermaier, A.B.; Tucha, L.; Koerts, J.; Aschenbrenner, S.; Westermann, C.; Weisbrod, M.; Lange, K.W.; Tucha, O. Complex prospective memory in adults with attention deficit hyperactivity disorder. PLoS ONE 2013, 8, e58338. [Google Scholar] [CrossRef] [PubMed]
- Mowinckel, A.M.; Pedersen, M.L.; Eilertsen, E.; Biele, G. A meta-analysis of decision-making and attention in adults with ADHD. J. Atten. Disord. 2015, 19, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Bangma, D.F.; Koerts, J.; Fuermaier, A.; Mette, C.; Zimmermann, M.; Toussaint, A.K.; Tucha, L.; Tucha, O. Financial decision-making in adults with ADHD. Neuropsychology 2019, 33, 1065–1077. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.E.; Hodgkins, P.; Kahle, J.; Madhoo, M.; Kewley, G. Long-term outcomes of ADHD: Academic achievement and performance. J. Atten. Disord. 2020, 24, 73–85. [Google Scholar] [CrossRef]
- Fuermaier, A.B.; Tucha, L.; Butzbach, M.; Weisbrod, M.; Aschenbrenner, S.; Tucha, O. ADHD at the workplace: ADHD symptoms, diagnostic status, and work-related functioning. J. Neural Transm. 2021, 128, 1021–1031. [Google Scholar] [CrossRef]
- Brunkhorst-Kanaan, N.; Libutzki, B.; Reif, A.; Larsson, H.; McNeill, R.V.; Kittel-Schneider, S. ADHD and accidents over the life span–A systematic review. Neurosci. Biobehav. Rev. 2021, 125, 582–591. [Google Scholar] [CrossRef]
- Beauchaine, T.P.; Ben-David, I.; Bos, M. ADHD, financial distress, and suicide in adulthood: A population study. Sci. Adv. 2020, 6, eaba1551. [Google Scholar] [CrossRef]
- Kalbag, A.S.; Levin, F.R.J.S.U. Misuse, Adult ADHD and substance abuse: Diagnostic and treatment issues. Subst. Use Misuse 2005, 40, 1955–1981. [Google Scholar] [CrossRef]
- Michielsen, M.; Comijs, H.C.; Aartsen, M.J.; Semeijn, E.J.; Beekman, A.T.; Deeg, D.J.; Kooij, J.S. The relationships between ADHD and social functioning and participation in older adults in a population-based study. J. Atten. Disord. 2015, 19, 368–379. [Google Scholar] [CrossRef] [PubMed]
- Mangels, J.A.; Craik, F.I.; Levine, B.; Schwartz, M.L.; Stuss, D.T. Effects of divided attention on episodic memory in chronic traumatic brain injury: A function of severity and strategy. Neuropsychologia 2002, 40, 2369–2385. [Google Scholar] [CrossRef]
- Barkley, R.A. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychol. Bull. 1997, 121, 65–94. [Google Scholar] [CrossRef] [PubMed]
- Spikman, J.M.; Zomeren, A.H.V.; Deelman, B.G. Deficits of attention after closed-head injury: Slowness only? J. Clin. Exp. Neuropsychol. 1996, 18, 755–767. [Google Scholar] [CrossRef] [PubMed]
- Butzbach, M.; Fuermaier, A.B.; Aschenbrenner, S.; Weisbrod, M.; Tucha, L.; Tucha, O. Basic processes as foundations of cognitive impairment in adult ADHD. J. Neural Transm. 2019, 126, 1347–1362. [Google Scholar] [CrossRef] [PubMed]
- Posner, M.; Rothbart, M. Attention, self–regulation and consciousness. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 1998, 353, 1915–1927. [Google Scholar]
- Posner, M.I.; Snyder, C.R.; Solso, R. Attention and cognitive control. In Cognitive Psychology: Key Readings; Balota, D., Marsh, E., Eds.; Psychology Press: London, UK, 2004; pp. 205–223. [Google Scholar]
- Kreitz, C.; Furley, P.; Memmert, D.; Simons, D.J. Working-memory performance is related to spatial breadth of attention. Psychol. Res. 2015, 79, 1034–1041. [Google Scholar] [CrossRef]
- Hüttermann, S.; Memmert, D.; Nerb, J. Individual differences in attentional capability are linked to creative decision making. J. Appl. Soc. Psychol. 2019, 49, 159–167. [Google Scholar] [CrossRef]
- Mohamed, S.M.; Butzbach, M.; Fuermaier, A.B.M.; Weisbrod, M.; Aschenbrenner, S.; Tucha, L.; Tucha, O. Basic and complex cognitive functions in Adult ADHD. PLoS ONE 2021, 16, e0256228. [Google Scholar] [CrossRef]
- Guo, N.; Fuermaier, A.; Koerts, J.; Mueller, B.W.; Diers, K.; Mroß, A.; Mette, C.; Tucha, L.; Tucha, O. Neuropsychological functioning of individuals at clinical evaluation of adult ADHD. J. Neural Transm. 2021, 128, 877–891. [Google Scholar] [CrossRef]
- Guo, N.; Fuermaier, A.; Koerts, J.; Tucha, O.; Scherbaum, N.; Müller, B.W. Networks of Neuropsychological Functions in the Clinical Evaluation of Adult ADHD. Assessment 2022. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.L.; Valentine, A.Z.; Groom, M.J.; Walker, G.M.; Sayal, K.; Daley, D.; Hollis, C. The clinical utility of the continuous performance test and objective measures of activity for diagnosing and monitoring ADHD in children: A systematic review. Eur. Child Adolesc. Psychiatry 2016, 25, 677–699. [Google Scholar] [CrossRef] [PubMed]
- Fuermaier, A.B.; Fricke, J.A.; de Vries, S.M.; Tucha, L.; Tucha, O. Neuropsychological assessment of adults with ADHD: A Delphi consensus study. Appl. Neuropsychol. Adult 2018, 26, 340–354. [Google Scholar] [CrossRef] [PubMed]
- Mapou, R.L. Counterpoint: Neuropsychological testing is not useful in the diagnosis of ADHD, but…. ADHD Rep. 2019, 27, 8–12. [Google Scholar] [CrossRef]
- Nikolas, M.A.; Marshall, P.; Hoelzle, J.B. The role of neurocognitive tests in the assessment of adult attention-deficit/hyperactivity disorder. Psychol. Assess. 2019, 31, 685–698. [Google Scholar] [CrossRef] [PubMed]
- Mostert, J.C.; Onnink, A.M.H.; Klein, M.; Dammers, J.; Harneit, A.; Schulten, T.; van Hulzen, K.J.; Kan, C.C.; Slaats-Willemse, D.; Buitelaar, J.K. Cognitive heterogeneity in adult attention deficit/hyperactivity disorder: A systematic analysis of neuropsychological measurements. Eur. Neuropsychopharmacol. 2015, 25, 2062–2074. [Google Scholar] [CrossRef]
- Manly, T.; Anderson, V.; Nimmo-Smith, I.; Turner, A.; Watson, P.; Robertson, I.H. The differential assessment of children’s attention: The Test of Everyday Attention for Children (TEA-Ch), normative sample and ADHD performance. J. Child Psychol. Psychiatry Allied Discip. 2001, 42, 1065–1081. [Google Scholar] [CrossRef]
- Salomone, S.; Fleming, G.R.; Bramham, J.; O’Connell, R.G.; Robertson, I.H. Neuropsychological deficits in adult ADHD: Evidence for differential attentional impairments, deficient executive functions, and high self-reported functional impairments. J. Atten. Disord. 2020, 24, 1413–1424. [Google Scholar] [CrossRef]
- Booth, J.R.; Burman, D.D.; Meyer, J.R.; Lei, Z.; Trommer, B.L.; Davenport, N.D.; Li, W.; Parrish, T.B.; Gitelman, D.R.; Marsel Mesulam, M.J.J.O.C.P. Psychiatry, Larger deficits in brain networks for response inhibition than for visual selective attention in attention deficit hyperactivity disorder (ADHD). J. Child Psychol. Psychiatry 2005, 46, 94–111. [Google Scholar] [CrossRef]
- Tucha, L.; Tucha, O.; Laufkötter, R.; Walitza, S.; Klein, H.; Lange, K. Neuropsychological assessment of attention in adults with different subtypes of attention-deficit/hyperactivity disorder. J. Neural Transm. 2008, 115, 269–278. [Google Scholar] [CrossRef]
- Marchetta, N.D.; Hurks, P.P.; De Sonneville, L.M.; Krabbendam, L.; Jolles, J. Sustained and focused attention deficits in adult ADHD. J. Atten. Disord. 2008, 11, 664–676. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.A.; Kelly, S.P.; Bellgrove, M.A.; Barry, E.; Cox, M.; Gill, M.; Robertson, I.H. Response variability in attention deficit hyperactivity disorder: Evidence for neuropsychological heterogeneity. Neuropsychologia 2007, 45, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Lundervold, A.J.; Adolfsdottir, S.; Halleland, H.; Halmøy, A.; Plessen, K.; Haavik, J. Attention Network Test in adults with ADHD-the impact of affective fluctuations. Behav. Brain Funct. 2011, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kofler, M.J.; Rapport, M.D.; Sarver, D.E.; Raiker, J.S.; Orban, S.A.; Friedman, L.M.; Kolomeyer, E.G. Reaction time variability in ADHD: A meta-analytic review of 319 studies. Clin. Psychol. Rev. 2013, 33, 795–811. [Google Scholar] [CrossRef]
- Buzy, W.M.; Medoff, D.R.; Schweitzer, J.B. Intra-individual variability among children with ADHD on a working memory task: An ex-Gaussian approach. Child Neuropsychol. 2009, 15, 441–459. [Google Scholar] [CrossRef]
- Friedman, L.M.; Rapport, M.D.; Fabrikant-Abzug, G. Consistently Inconsistent Working Memory Performance Among Children with ADHD: Evidence of Response Accuracy Variability (RAV). J. Psychopathol. Behav. Assess. 2022, 44, 787–799. [Google Scholar] [CrossRef]
- Klein, C.; Wendling, K.; Huettner, P.; Ruder, H.; Peper, M. Intra-subject variability in attention-deficit hyperactivity disorder. Biol. Psychiatry 2006, 60, 1088–1097. [Google Scholar] [CrossRef]
- Vaurio, R.G.; Simmonds, D.J.; Mostofsky, S.H. Increased intra-individual reaction time variability in attention-deficit/hyperactivity disorder across response inhibition tasks with different cognitive demands. Neuropsychologia 2009, 47, 2389–2396. [Google Scholar] [CrossRef]
- Gmehlin, D.; Fuermaier, A.B.; Walther, S.; Debelak, R.; Rentrop, M.; Westermann, C.; Sharma, A.; Tucha, L.; Koerts, J.; Tucha, O. Intraindividual variability in inhibitory function in adults with ADHD–an ex-Gaussian approach. PLoS ONE 2014, 9, e112298. [Google Scholar] [CrossRef]
- Tamm, L.; Narad, M.E.; Antonini, T.N.; O’Brien, K.M.; Hawk, L.W.; Epstein, J.N. Reaction time variability in ADHD: A review. Neurotherapeutics 2012, 9, 500–508. [Google Scholar] [CrossRef]
- Karalunas, S.L.; Geurts, H.M.; Konrad, K.; Bender, S.; Nigg, J.T. Annual research review: Reaction time variability in ADHD and autism spectrum disorders: Measurement and mechanisms of a proposed trans-diagnostic phenotype. J. Child Psychol. Psychiatry 2014, 55, 685–710. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.L.; Kennedy, T.M.; Joseph, H.M.; Riston, S.J.; Kipp, H.L.; Molina, B.S. Real-world changes in adolescents’ ADHD symptoms within the day and across school and non-school days. J. Abnorm. Child Psychol. 2020, 48, 1543–1553. [Google Scholar] [CrossRef] [PubMed]
- Schmid, J.; Stadler, G.; Dirk, J.; Fiege, C.; Gawrilow, C. ADHD symptoms in adolescents’ everyday Life: Fluctuations and symptom structure within and between individuals. J. Atten. Disord. 2020, 24, 1169–1180. [Google Scholar] [CrossRef] [PubMed]
- Guilmette, T.J.; Sweet, J.J.; Hebben, N.; Koltai, D.; Mahone, E.M.; Spiegler, B.J.; Stucky, K.; Westerveld, M.; Participants, C. American Academy of Clinical Neuropsychology consensus conference statement on uniform labeling of performance test scores. Clin. Neuropsychol. 2020, 34, 437–453. [Google Scholar] [CrossRef]
- Sibley, M.H. Empirically-informed guidelines for first-time adult ADHD diagnosis. J. Clin. Exp. Neuropsychol. 2021, 43, 340–351. [Google Scholar] [CrossRef]
- Retz-Junginger, P.; Retz, W.; Blocher, D.; Stieglitz, R.-D.; Georg, T.; Supprian, T.; Wender, P.; Rösler, M. Reliabilität und Validität der Wender-Utah-Rating-Scale-Kurzform: Retrospektive Erfassung von Symptomen aus dem Spektrum der Aufmerksamkeitsdefizit/Hyperaktivitätsstörung [Reliability and validity of the German short version of the Wender-Utah Rating Scale for the retrospective assessment of attention deficit/hyperactivity disorder]. Der Nervenarzt 2003, 74, 987–993. [Google Scholar]
- Christiansen, H.; Kis, B.; Hirsch, O.; Matthies, S.; Hebebrand, J.; Uekermann, J.; Abdel-Hamid, M.; Kraemer, M.; Wiltfang, J.; Graf, E. German validation of the Conners Adult ADHD Rating Scales (CAARS) II: Reliability, validity, diagnostic sensitivity and specificity. Eur. Psychiatry 2012, 27, 321–328. [Google Scholar] [CrossRef]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 1994; p. xxvii, 886. [Google Scholar]
- Schuhfried Vienna Test System (VTS) 8, version 8.2.00; [Computer Software]; SCHUHFRIED: Mödling, Austria, 2013.
- Fuermaier, A.B.; Tucha, L.; Guo, N.; Mette, C.; Müller, B.W.; Scherbaum, N.; Tucha, O. It Takes Time: Vigilance and Sustained Attention Assessment in Adults with ADHD. Int. J. Environ. Res. Public Health 2022, 19, 5216. [Google Scholar] [CrossRef]
- Ramm, M.; Jafarpour, A.; Boentert, M.; Lojewsky, N.; Young, P.; Heidbreder, A.J.J.O.S.R. The perception and attention functions test battery as a measure of neurocognitive impairment in patients with suspected central disorders of hypersomnolence. J. Sleep Res. 2018, 27, 275–282. [Google Scholar] [CrossRef]
- Ramm, M.; Boentert, M.; Lojewsky, N.; Jafarpour, A.; Young, P.; Heidbreder, A. Disease-specific attention impairment in disorders of chronic excessive daytime sleepiness. Sleep Med. 2019, 53, 133–140. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Huang-Pollock, C.L.; Karalunas, S.L.; Tam, H.; Moore, A.N. Evaluating vigilance deficits in ADHD: A meta-analysis of CPT performance. J. Abnorm. Psychol. 2012, 121, 360. [Google Scholar] [CrossRef] [PubMed]
- Tucha, L.; Tucha, O.; Walitza, S.; Sontag, T.A.; Laufkötter, R.; Linder, M.; Lange, K.W. Vigilance and sustained attention in children and adults with ADHD. J. Atten. Disord. 2009, 12, 410–421. [Google Scholar] [CrossRef] [PubMed]
- Konrad, K.; Neufang, S.; Hanisch, C.; Fink, G.R.; Herpertz-Dahlmann, B. Dysfunctional attentional networks in children with attention deficit/hyperactivity disorder: Evidence from an event-related functional magnetic resonance imaging study. Biol. Psychiatry 2006, 59, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Cao, Q.; Zang, Y.; Zhu, C.; Cao, X.; Sun, L.; Zhou, X.; Wang, Y. Alerting deficits in children with attention deficit/hyperactivity disorder: Event-related fMRI evidence. Brain Res. 2008, 1219, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Rubia, K.; Smith, A.B.; Brammer, M.J.; Taylor, E. Temporal lobe dysfunction in medication-naive boys with attention-deficit/hyperactivity disorder during attention allocation and its relation to response variability. Biol. Psychiatry 2007, 62, 999–1006. [Google Scholar] [CrossRef]
- Marshall, P.; Hoelzle, J.; Nikolas, M. Diagnosing Attention-Deficit/Hyperactivity Disorder (ADHD) in young adults: A qualitative review of the utility of assessment measures and recommendations for improving the diagnostic process. Clin. Neuropsychol. 2021, 35, 165–198. [Google Scholar] [CrossRef]
- Pettersson, R.; Söderström, S.; Nilsson, K.W. Diagnosing ADHD in adults: An examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments. J. Atten. Disord. 2018, 22, 1019–1031. [Google Scholar] [CrossRef]
- Kooij, J.; Bijlenga, D.; Salerno, L.; Jaeschke, R.; Bitter, I.; Balazs, J.; Thome, J.; Dom, G.; Kasper, S.; Filipe, C.N. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur. Psychiatry 2019, 56, 14–34. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Some examples of regression towards the mean. BMJ Br. Med. J. 1994, 309, 780. [Google Scholar] [CrossRef]

| Adults with ADHD (n = 21) | |||||
|---|---|---|---|---|---|
| Sex (Male/Female) | 8/13 | ||||
| Education (1/2/3/4/5/6) a | 0/1/8/6/5/1 | ||||
| Min | Max | Median | Mean | SD | |
| Age (in years) b | 20 | 65 | 47.5 | 46.1 | 11.6 |
| Childhood ADHD symptoms c | 11 | 57 | 41 | 39.3 | 13.1 |
| Current ADHD symptoms d | |||||
| Inattention | 1 | 22 | 13 | 13.2 | 6.2 |
| Hyperactivity/Impulsivity | 3 | 24 | 13 | 12.2 | 6.0 |
| Total symptoms | 6 | 46 | 25 | 25.5 | 10.7 |
| Attention Performance Test Scores | T1 | T2 | T3 | Friedman Test | Pairwise Comparisons a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 vs. T2 | T1 vs. T3 | T2 vs. T3 | ||||||||||||
| Median | IQR | % Below Average b | Median | IQR | % Below Average b | Median | IQR | % Below Average b | X2 | p | Cohen’s rc | Cohen’s rc | Cohen’s rc | |
| Selective attention d—RT | 394.00 | 158.00 | 23.8 | 354.00 | 136.00 | 14.29 | 339.00 | 166.50 | 21.05 | 0.12 | 0.94 | 0.15 | 0.02 | 0.12 |
| Selective attention d—SDRT | 1.24 | 0.12 | 19.05 | 1.20 | 0.07 | 10.53 | 1.25 | 0.10 | 17.65 | 0.92 | 0.63 | 0.09 | 0.09 | 0.25 |
| Selective attention d—Omissions | 0 | 1.00 | 19.05 | 0 | 0.75 | 15.00 | 0 | 0.25 | 16.67 | 0.26 | 0.88 | 0.08 | 0.09 | 0.11 |
| Selective attention e | 33.33 | 19.04 | 36.84 | |||||||||||
| Vigilance f—RT | 440.00 | 109.50 | 15.00 | 421.00 | 150.00 | 23.81 | 434.00 | 163.00 | 21.05 | 3.35 | 0.19 | 0.13 | 0.09 | 0.05 |
| Vigilance f—SDRT | 1.24 | 0.08 | 5.26 | 1.24 | 0.09 | 5.26 | 1.21 | 0.06 | 0 | 0.52 | 0.77 | 0.13 | 0.25 | 0.08 |
| Vigilance f—Omissions | 0 | 1.00 | 15.00 | 1.00 | 1.00 | 9.52 | 1.00 | 1.00 | 0 | 0.35 | 0.84 | 0.09 | 0.06 | 0.05 |
| Vigilance e | 20.00 | 38.10 | 21.05 | |||||||||||
| Attention Performance Test Scores | T1–T2 a | T1–T3 a | T2–T3 a | % Consistent Test Score Interpretations across the Three Assessments | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range | M | % Consistent Test Score Interpretations b | rc | Range | M | % Consistent Test Score Interpretations b | rc | Range | M | % Consistent Test Score Interpretations b | rc | ||
| Selective attention d—RT | 2–17 | 5.86 | 81 | 0.828 * | 0–19 | 4.95 | 79 | 0.833 * | 0–9 | 4.58 | 95 | 0.927 * | 79 |
| Selective attention d—SDRT | 1–23 | 8.79 | 89 | 0.369 | 1–22 | 7.82 | 76 | 0.556 | 0–21 | 8.00 | 88 | 0.265 | 75 |
| Selective attention d—Omissions | 0–23 | 4.10 | 80 | 0.569 * | 0–23 | 4.78 | 83 | 0.489 | 0–14 | 3.24 | 100 | 0.592 * | 82 |
| Vigilance e—RT | 0–17 | 4.35 | 80 | 0.779 * | 0–29 | 6.05 | 84 | 0.591 * | 0–13 | 5.53 | 84 | 0.784 * | 74 |
| Vigilance e—SDRT | 1–24 | 8.59 | 88 | 0.379 | 2–19 | 6.65 | 95 | 0.441 | 1–33 | 8.88 | 94 | 0.238 | 88 |
| Vigilance e—Omissions | 0–23 | 5.85 | 75 | 0.465 | 0–23 | 5.95 | 85 | 0.221 | 0–23 | 5.05 | 89 | 0.290 | 74 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, N.; Koerts, J.; Tucha, L.; Fetter, I.; Biela, C.; König, M.; Bossert, M.; Diener, C.; Aschenbrenner, S.; Weisbrod, M.; et al. Stability of Attention Performance of Adults with ADHD over Time: Evidence from Repeated Neuropsychological Assessments in One-Month Intervals. Int. J. Environ. Res. Public Health 2022, 19, 15234. https://doi.org/10.3390/ijerph192215234
Guo N, Koerts J, Tucha L, Fetter I, Biela C, König M, Bossert M, Diener C, Aschenbrenner S, Weisbrod M, et al. Stability of Attention Performance of Adults with ADHD over Time: Evidence from Repeated Neuropsychological Assessments in One-Month Intervals. International Journal of Environmental Research and Public Health. 2022; 19(22):15234. https://doi.org/10.3390/ijerph192215234
Chicago/Turabian StyleGuo, Nana, Janneke Koerts, Lara Tucha, Isabel Fetter, Christina Biela, Miriam König, Magdalena Bossert, Carsten Diener, Steffen Aschenbrenner, Matthias Weisbrod, and et al. 2022. "Stability of Attention Performance of Adults with ADHD over Time: Evidence from Repeated Neuropsychological Assessments in One-Month Intervals" International Journal of Environmental Research and Public Health 19, no. 22: 15234. https://doi.org/10.3390/ijerph192215234
APA StyleGuo, N., Koerts, J., Tucha, L., Fetter, I., Biela, C., König, M., Bossert, M., Diener, C., Aschenbrenner, S., Weisbrod, M., Tucha, O., & Fuermaier, A. B. M. (2022). Stability of Attention Performance of Adults with ADHD over Time: Evidence from Repeated Neuropsychological Assessments in One-Month Intervals. International Journal of Environmental Research and Public Health, 19(22), 15234. https://doi.org/10.3390/ijerph192215234







