A Systematic Review on Modeling Methods and Influential Factors for Mapping Dengue-Related Risk in Urban Settings
Abstract
1. Introduction
- (1)
- Reviewing available modeling tools for generating predictive maps of dengue-related risk since 2014;
- (2)
- Investigating determinants in urban settings used for spatial and spatio-temporal modeling;
- (3)
- Discussing the limitations and advantages of different methods for developing dengue-related risk;
- (4)
- Proposing improvements for future works.
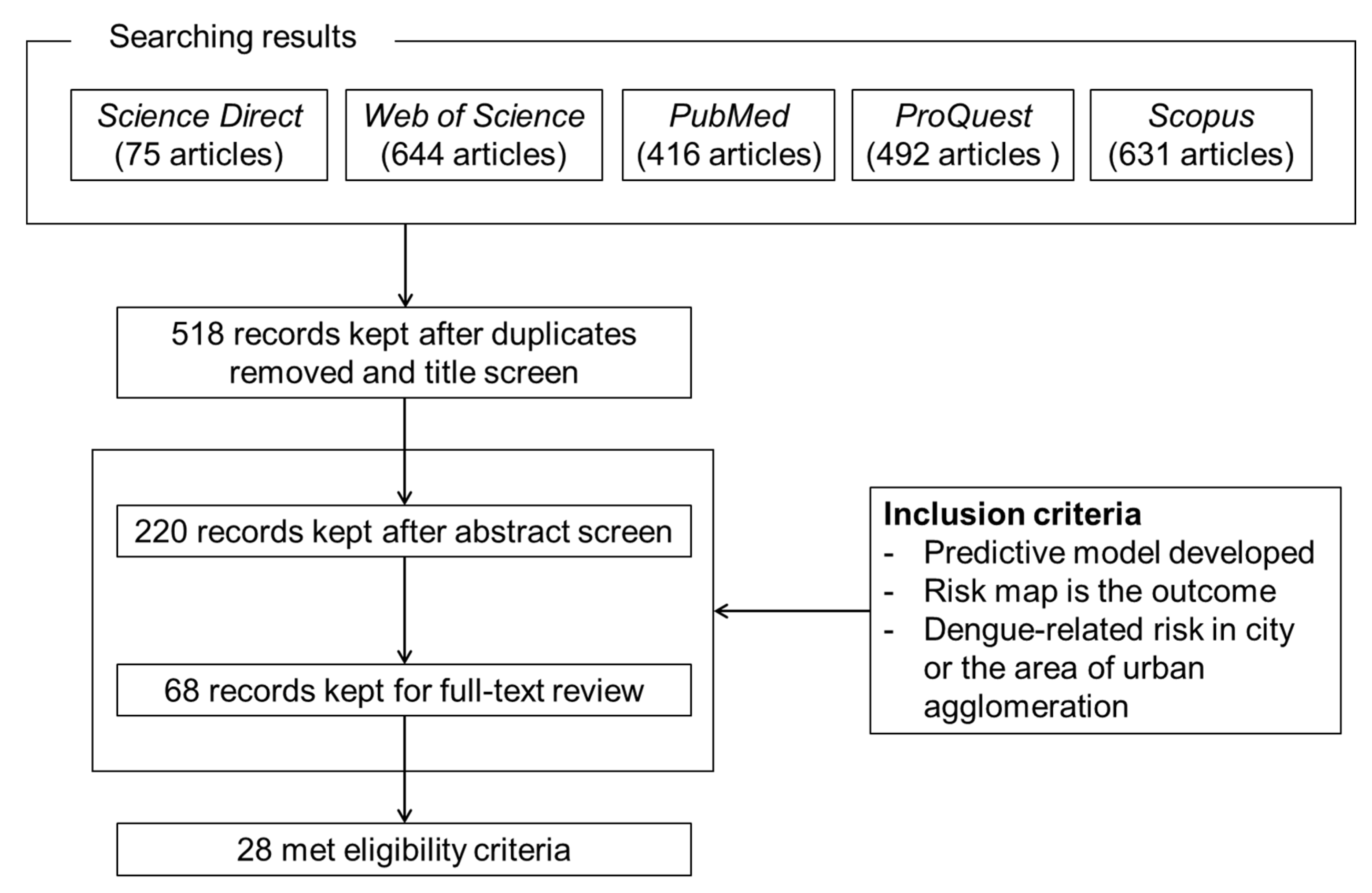
2. Methods
2.1. Search Terms and Selection Criteria
- Articles published from January 2014 to May 2022;
- In an English peer-reviewed paper or non-conference proceedings;
- A spatial or spatio-temporal modeling tool employed to predict the potential dengue risk distribution;
- A predictive risk map or early warning system about dengue-related burden in a city or area of urban agglomeration as the outcome;
- Includes an investigation of the impacts of environmental and socio-economic determinants for modeling.
2.2. Data Extraction
3. Results
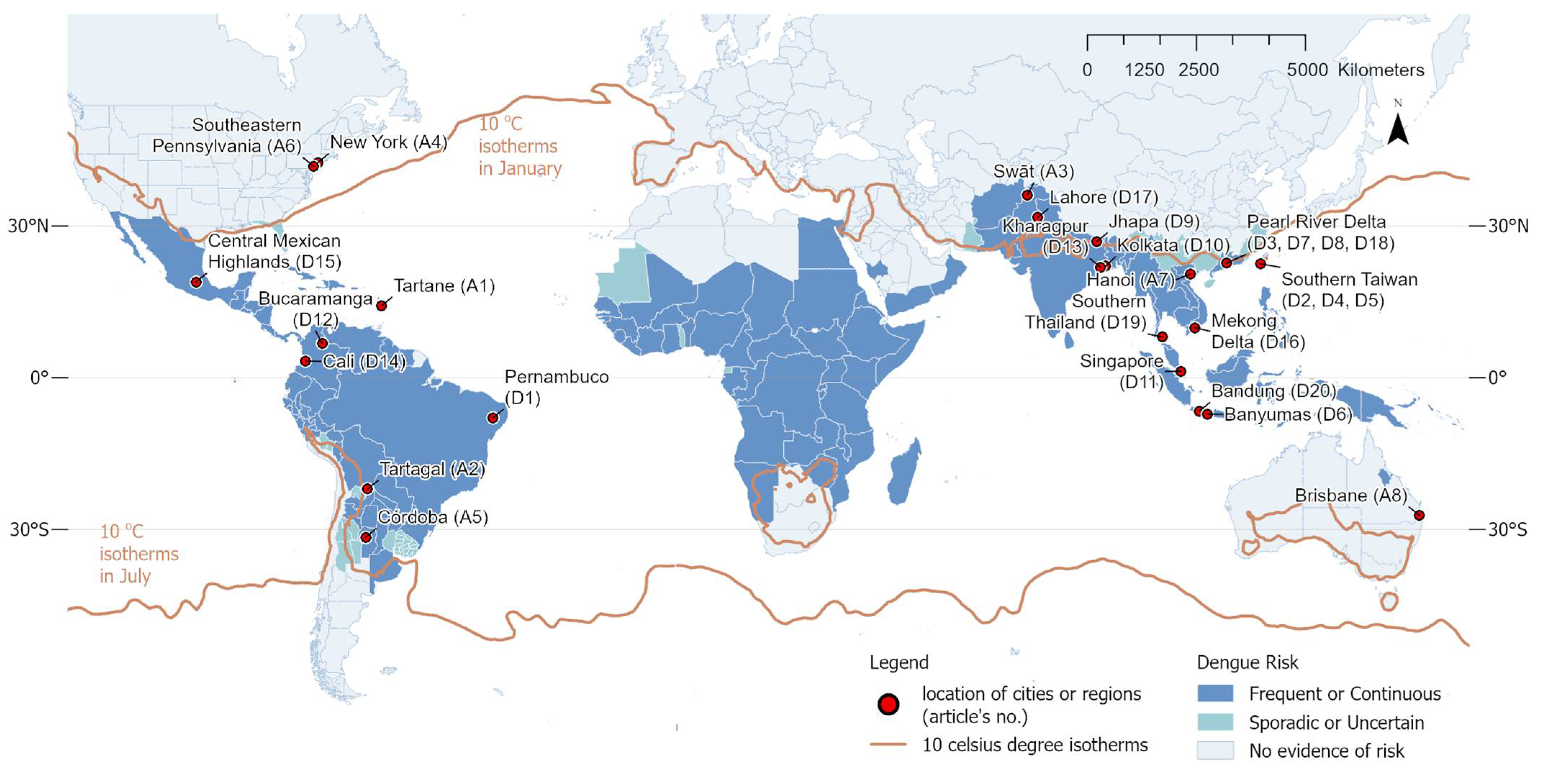
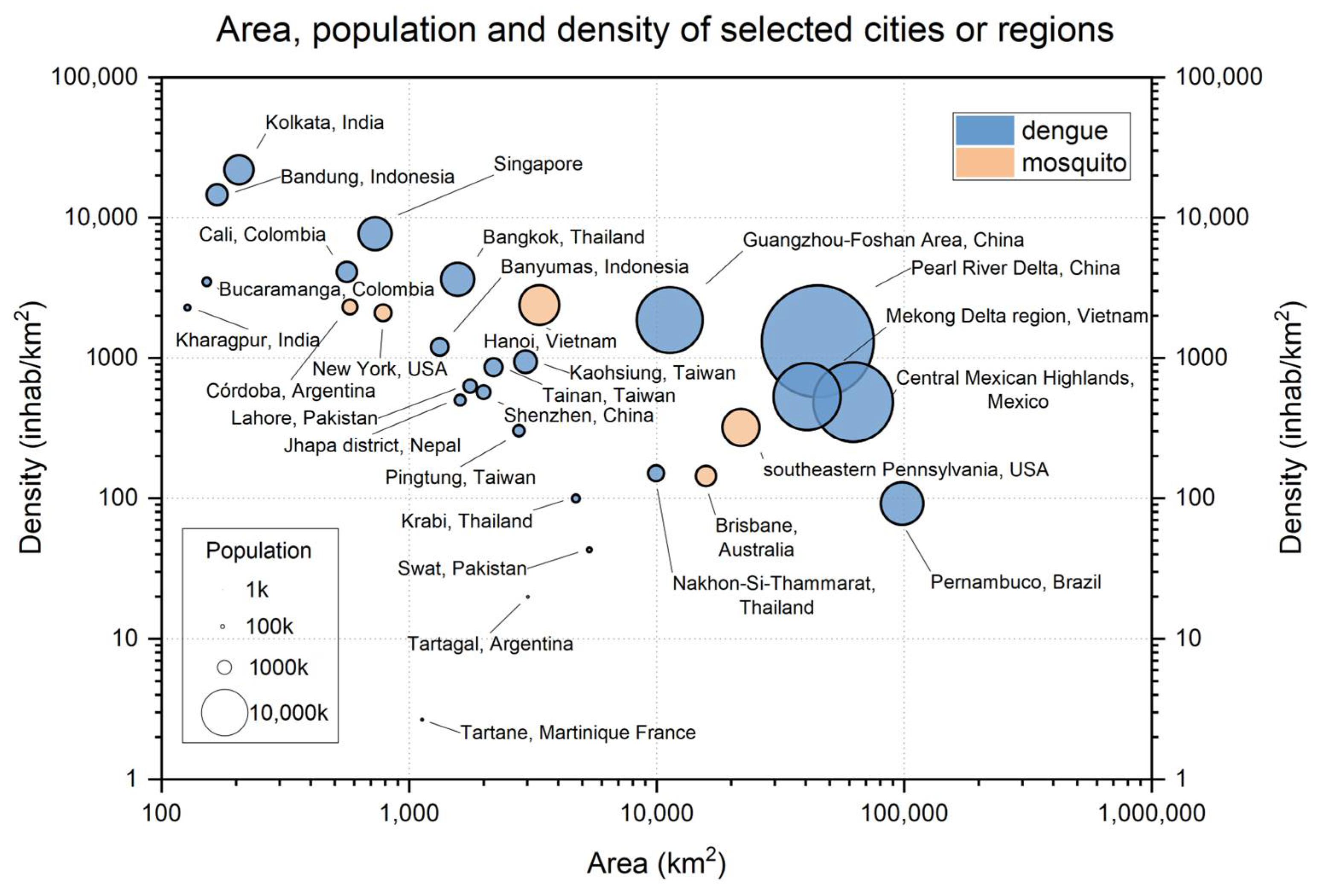
3.1. General Observation
3.2. Data Characters
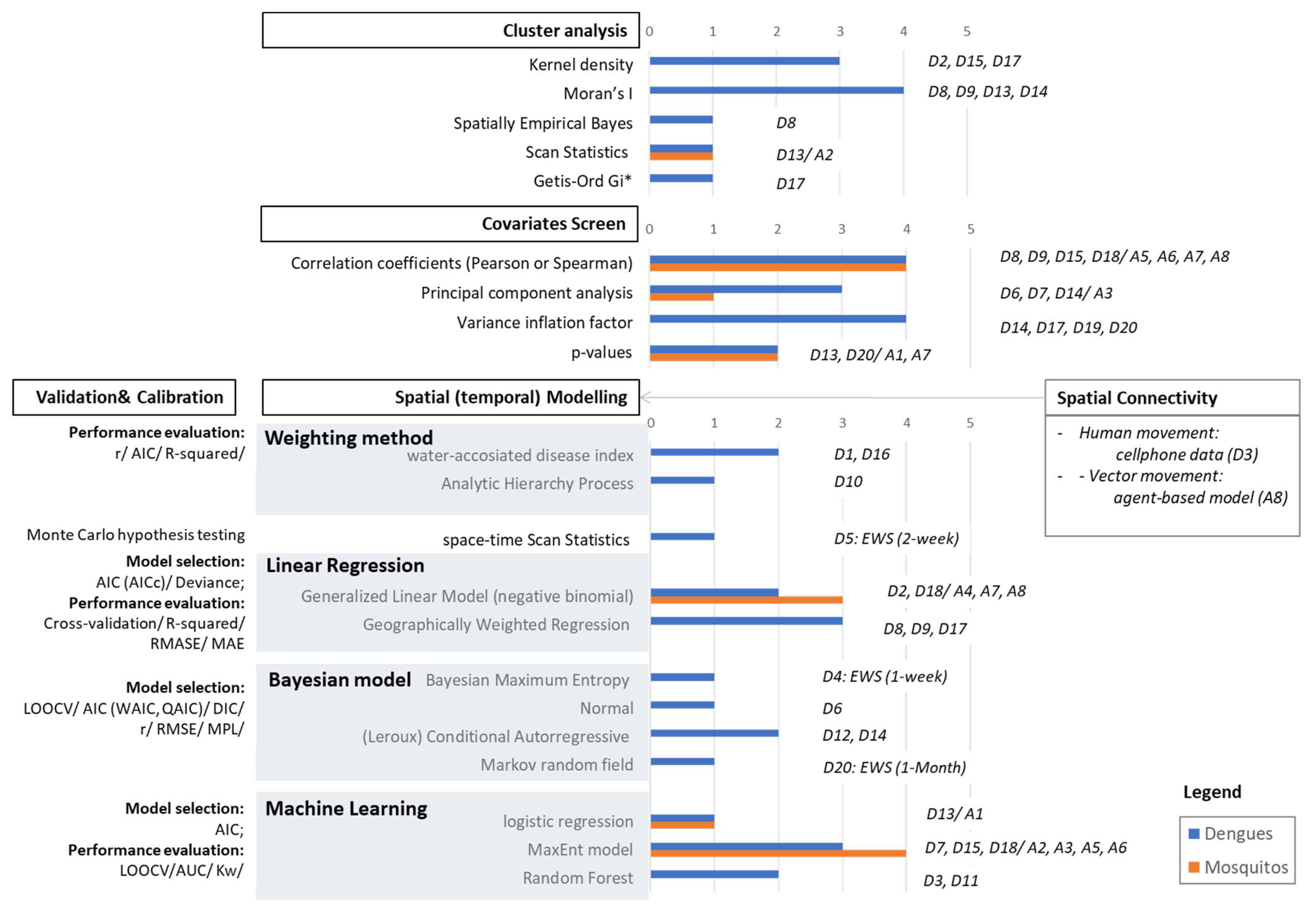
3.3. Modeling Approaches
3.3.1. Cluster Analysis
3.3.2. Covariates Screen
3.3.3. Spatial Modelling
3.3.4. Calibration and Validations
3.4. Influential Factors
3.4.1. Climatic Variables
3.4.2. Built Environmental Variables
3.4.3. Socio-Economic Variables
4. Discussion
4.1. Study Areas
4.2. Effective Predictors
4.2.1. Entomological Data
4.2.2. Climatic Data
4.2.3. Built Environmental Data
4.2.4. Socio-Economic Data
4.3. Modeling Techniques
4.3.1. Predictive Models
4.3.2. Calibration and Validation
4.4. Mapping Methodology Design
4.5. Improvement Suggestions
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| No. | Mapping Spatial Unit * | Surveillance | Species ** | Buffer (m) | Predictors *** | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Epidemic | Entomologic | Climatic (Time) | Built Environmental Variables | Socio-Economic Variables | Other Variables | |||||||||||||
| LULC | MOR | LS | ROAD | EST | INFRA | TOPO | POP | DEV | DEMO | CONDI | ||||||||
| D1 | 250 m |  | Aeg and Alb |  (month) (month) |  |  |  |  |  | |||||||||
| D2 | 300 m |  |  | Aeg and Alb |  | |||||||||||||
| D3 | 100 m |  | Alb |  (month) (month) |  |  |  |  |  | Cellphone data | ||||||||
| D4 | District |  | Aeg |  (day) (day) | ||||||||||||||
| D5 | District |  |  |  | ||||||||||||||
| D6 | District |  | Aeg |  (month) (month)  |  |  |  |  | ||||||||||
| D7 | 1 km |  |  (season) (season) |  |  |  |  |  | ||||||||||
| D8 | 2 km |  | Alb |  (year) (year)  |  |  |  |  |  | |||||||||
| D9 | District |  | Aeg |  (year) (year)  |  |  |  |  | ||||||||||
| D10 | 30 m | Aeg | 200 |  (year) (year) |  |  |  |  | ||||||||||
| D11 | 1 km |  |  | Aeg and Alb | 150 |  |  |  |  |  | ||||||||
| D12 | District |  |  (day) (day)  |  | ||||||||||||||
| D13 | 30 m |  | Aeg |  (month) (month) |  |  |  |  |  | |||||||||
| D14 | Neighborhood |  | Aeg and Alb |  (week) (week) |  |  |  |  |  |  | ||||||||
| D15 | 200 m |  |  | Aeg |  (month) (month) |  |  | |||||||||||
| D16 | Township |  |  (month) (month)  |  |  |  | ||||||||||||
| D17 | 250 m |  | Aeg |  (year) (year)  |  |  | ||||||||||||
| D18 | 1 km |  | Alb |  (month) (month) |  |  |  |  |  | Future scenario | ||||||||
| D19 | District |  | Aeg and Alb |  (season) (season) |  |  | Artificial containers | |||||||||||
| D20 | District |  | Aeg and Alb |  (month) (month) | ||||||||||||||
| A1 | Building |  | Aeg | 50 |  (day) (day) |  |  | |||||||||||
| A2 | 10 m |  | Aeg | 150 |  |  |  |  | ||||||||||
| A3 | 30 m |  | Aeg |  (season) (season) |  |  |  |  | ||||||||||
| A4 | District |  | Alb | 200 |  (month) (month) |  | ||||||||||||
| A5 | Neighborhood |  | Aeg | 500 |  |  |  |  |  | |||||||||
| A6 | 232 m |  | Alb | 250 |  (month) (month) |  |  |  |  | |||||||||
| A7 | 30 m |  | Culex | 250 |  (month) (month)  |  |  |  | ||||||||||
| A8 | District | Aeg | 75 |  |  |  | Rainwater tank | |||||||||||
 represents the data applied for modeling.
represents the data applied for modeling.  represents applied remote sensing data for climatic variables, including land surface temperature in daytime and nighttime.
represents applied remote sensing data for climatic variables, including land surface temperature in daytime and nighttime.References
- Gubler, D.J. Dengue, Urbanization and Globalization: The Unholy Trinity of the 21(st) Century. Trop. Med. Health 2011, 39 (Suppl. S4), 3–11. [Google Scholar] [CrossRef] [PubMed]
- Lambrechts, L.; Paaijmans, K.P.; Fansiri, T.; Carrington, L.B.; Kramer, L.D.; Thomas, M.B.; Scott, T.W. Impact of daily temperature fluctuations on dengue virus transmission by Aedes aegypti. Proc. Natl. Acad. Sci. USA 2011, 108, 7460–7465. [Google Scholar] [CrossRef] [PubMed]
- WHO. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Araujo, R.V.; Albertini, M.R.; Costa-da-Silva, A.L.; Suesdek, L.; Franceschi, N.C.; Bastos, N.M.; Katz, G.; Cardoso, V.A.; Castro, B.C.; Capurro, M.L.; et al. Sao Paulo urban heat islands have a higher incidence of dengue than other urban areas. Braz. J. Infect. Dis. 2015, 19, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Messina, J.P.; Brady, O.J.; Golding, N.; Kraemer, M.U.G.; Wint, G.R.W.; Ray, S.E.; Pigott, D.M.; Shearer, F.M.; Johnson, K.; Earl, L.; et al. The current and future global distribution and population at risk of dengue. Nat. Microbiol. 2019, 4, 1508–1515. [Google Scholar] [CrossRef]
- Johnson, D. Cartographies of Disease: Maps, Mapping, and Medicine; Taylor & Francis: Abingdon, UK, 2007. [Google Scholar]
- Whiteman, A.; Loaiza, J.R.; Yee, D.A.; Poh, K.C.; Watkins, A.S.; Lucas, K.J.; Rapp, T.J.; Kline, L.; Ahmed, A.; Chen, S.; et al. Do socioeconomic factors drive Aedes mosquito vectors and their arboviral diseases? A systematic review of dengue, chikungunya, yellow fever, and Zika Virus. One Health 2020, 11, 100188. [Google Scholar] [CrossRef]
- Marti, R.; Li, Z.; Catry, T.; Roux, E.; Mangeas, M.; Handschumacher, P.; Gaudart, J.; Tran, A.; Demagistri, L.; Faure, J.-F.; et al. A Mapping Review on Urban Landscape Factors of Dengue Retrieved from Earth Observation Data, GIS Techniques, and Survey Questionnaires. Remote Sens. 2020, 12, 932. [Google Scholar] [CrossRef]
- Li, Y.; Dou, Q.; Lu, Y.; Xiang, H.; Yu, X.; Liu, S. Effects of ambient temperature and precipitation on the risk of dengue fever: A systematic review and updated meta-analysis. Environ. Res. 2020, 191, 110043. [Google Scholar] [CrossRef]
- Naish, S.; Dale, P.; Mackenzie, J.S.; McBride, J.; Mengersen, K.; Tong, S. Climate change and dengue: A critical and systematic review of quantitative modelling approaches. BMC Infect. Dis. 2014, 14, 167. [Google Scholar] [CrossRef]
- Aswi, A.; Cramb, S.M.; Moraga, P.; Mengersen, K. Bayesian spatial and spatio-temporal approaches to modelling dengue fever: A systematic review. Epidemiol. Infect. 2018, 147, e33. [Google Scholar] [CrossRef]
- Louis, V.R.; Phalkey, R.; Horstick, O.; Ratanawong, P.; Wilder-Smith, A.; Tozan, Y.; Dambach, P. Modeling tools for dengue risk mapping—A systematic review. Int. J. Health Geogr. 2014, 13, 50. [Google Scholar] [CrossRef]
- Rogers, D.J.; Suk, J.E.; Semenza, J.C. Using global maps to predict the risk of dengue in Europe. Acta Trop. 2014, 129, 1–14. [Google Scholar] [CrossRef]
- Tsheten, T.; Clements, A.C.A.; Gray, D.J.; Wangdi, K. Dengue risk assessment using multicriteria decision analysis: A case study of Bhutan. PLoS Negl. Trop. Dis. 2021, 15, 17. [Google Scholar] [CrossRef]
- Guzzetta, G.; Montarsi, F.; Baldacchino, F.A.; Metz, M.; Capelli, G.; Rizzoli, A.; Pugliese, A.; Rosa, R.; Poletti, P.; Merler, S. Potential Risk of Dengue and Chikungunya Outbreaks in Northern Italy Based on a Population Model of Aedes albopictus (Diptera: Culicidae). PLoS Negl. Trop. Dis. 2016, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Bailey, T.C.; Stephenson, D.B.; Graham, R.J.; Coelho, C.A.S.; Carvalho, M.S.; Barcellos, C. Spatio-temporal modelling of climate-sensitive disease risk: Towards an early warning system for dengue in Brazil. Comput. Geosci. 2011, 37, 371–381. [Google Scholar] [CrossRef]
- Ortiz, P.L.; Rivero, A.; Linares, Y.; Perez, A.; Vazquez, J.R. Spatial Models for Prediction and Early Warning of Aedes aegypti Proliferation from Data on Climate Change and Variability in Cuba. MEDICC Rev. 2015, 17, 20–28. [Google Scholar] [PubMed]
- Perkins, T.A.; Reiner, R.C.; Rodriguez-Barraquer, I.; Smith, D.L.; Scott, T.W.; Cummings, D.A. A review of transmission models of dengue: A quantitative and qualitative analysis of model features. In Dengue and Dengue Hemorrhagic Fever, 2nd ed.; Gubler, D.J., Ooi, E.E., Vasudevan, S., Farrar, J., Eds.; CABI: Wallingford, UK, 2014; pp. 99–114. [Google Scholar]
- Brady, O.J.; Gething, P.W.; Bhatt, S.; Messina, J.P.; Brownstein, J.S.; Hoen, A.G.; Moyes, C.L.; Farlow, A.W.; Scott, T.W.; Hay, S.I. Refining the global spatial limits of dengue virus transmission by evidence-based consensus. PLoS Negl. Trop. Dis. 2012, 6, e1760. [Google Scholar] [CrossRef]
- Attaway, D.F.; Jacobsen, K.H.; Falconer, A.; Manca, G.; Waters, N.M. Assessing the methods needed for improved dengue mapping: A SWOT analysis. Pan. Afr. Med. J. 2014, 17, 289. [Google Scholar] [CrossRef]
- Rogers, D.; Wilson, A.; Hay, S.; Graham, A. The global distribution of yellow fever and dengue. Adv. Parasitol. 2006, 62, 181–220. [Google Scholar]
- Sallam, M.F.; Fizer, C.; Pilant, A.N.; Whung, P.Y. Systematic Review: Land Cover, Meteorological, and Socioeconomic Determinants of Aedes Mosquito Habitat for Risk Mapping. Int. J. Environ. Res. Public Health 2017, 14, 1230. [Google Scholar] [CrossRef]
- Lee, S.A.; Jarvis, C.I.; Edmunds, W.J.; Economou, T.; Lowe, R. Spatial connectivity in mosquito-borne disease models: A systematic review of methods and assumptions. J. R. Soc. Interface 2021, 18, 20210096. [Google Scholar] [CrossRef]
- Dickin, S.K.; Schuster-Wallace, C.J. Assessing changing vulnerability to dengue in northeastern Brazil using a water-associated disease index approach. Glob. Environ. Change 2014, 29, 155–164. [Google Scholar] [CrossRef]
- Machault, V.; Yebakima, A.; Etienne, M.; Vignolles, C.; Palany, P.; Tourre, Y.M.; Guerecheau, M.; Lacaux, J.P. Mapping Entomological Dengue Risk Levels in Martinique Using High-Resolution Remote-Sensing Environmental Data. ISPRS Int. J. Geo-Inf. 2014, 3, 1352–1371. [Google Scholar] [CrossRef]
- Ong, J.; Liu, X.; Rajarethinam, J.; Kok, S.Y.; Liang, S.; Tang, C.S.; Cook, A.R.; Ng, L.C.; Yap, G. Mapping dengue risk in Singapore using Random Forest. PLoS Negl. Trop. Dis. 2018, 12, e0006587. [Google Scholar] [CrossRef] [PubMed]
- Wen, T.-H.; Lin, M.-H.; Teng, H.-J.; Chang, N.-T. Incorporating the human-Aedes mosquito interactions into measuring the spatial risk of urban dengue fever. Appl. Geogr. 2015, 62, 256–266. [Google Scholar] [CrossRef]
- Martinez-Bello, D.; Lopez-Quilez, A.; Prieto, A.T. Spatiotemporal modeling of relative risk of dengue disease in Colombia. Stoch. Environ. Res. Risk Assess. 2018, 32, 1587–1601. [Google Scholar] [CrossRef]
- Espinosa, M.; Weinberg, D.; Rotela, C.H.; Polop, F.; Abril, M.; Scavuzzo, C.M. Temporal Dynamics and Spatial Patterns of Aedes aegypti Breeding Sites, in the Context of a Dengue Control Program in Tartagal (Salta Province, Argentina). PLoS Negl. Trop. Dis. 2016, 10, e0004621. [Google Scholar] [CrossRef]
- Mao, L.; Yin, L.; Song, X.; Mei, S. Mapping intra-urban transmission risk of dengue fever with big hourly cellphone data. Acta Trop. 2016, 162, 188–195. [Google Scholar] [CrossRef]
- Ghosh, S.; Dinda, S.; Das Chatterjee, N.; Das, K.; Mahata, R. The spatial clustering of dengue disease and risk susceptibility mapping: An approach towards sustainable health management in Kharagpur city, India. Spat. Inf. Res. 2019, 27, 187–204. [Google Scholar] [CrossRef]
- Fatima, S.H.; Atif, S.; Rasheed, S.B.; Zaidi, F.; Hussain, E. Species Distribution Modelling of Aedes aegypti in two dengue-endemic regions of Pakistan. Trop. Med. Int. Health 2016, 21, 427–436. [Google Scholar] [CrossRef]
- Yu, H.-L.; Lee, C.-H.; Chien, L.-C. A spatiotemporal dengue fever early warning model accounting for nonlinear associations with hydrological factors: A Bayesian maximum entropy approach. Stoch. Environ. Res. Risk Assess. 2016, 30, 2127–2141. [Google Scholar] [CrossRef]
- Desjardins, M.R.; Eastin, M.D.; Paul, R.; Casas, I.; Delmelle, E.M. Space-Time conditional autoregressive modeling to estimate neighborhood-level risks for dengue fever in Cali, Colombia. Am. J. Trop. Med. Hyg. 2020, 103, 2040–2053. [Google Scholar] [CrossRef] [PubMed]
- Little, E.; Bajwa, W.; Shaman, J. Local environmental and meteorological conditions influencing the invasive mosquito Ae. albopictus and arbovirus transmission risk in New York City. PLoS Negl. Trop. Dis. 2017, 11, e0005828. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.; Teng, Y.C.; Lin, B.C.; Fan, I.C.; Chan, T.C. Online platform for applying space-time scan statistics for prospectively detecting emerging hot spots of dengue fever. Int. J. Health Geogr. 2016, 15, 43. [Google Scholar] [CrossRef]
- Ordonez-Sierra, R.; Mastachi-Loza, C.A.; Diaz-Delgado, C.; Cuervo-Robayo, A.P.; Ortiz, C.R.F.; Gomez-Albores, M.A.; Torres, I.M. Spatial Risk Distribution of Dengue Based on the Ecological Niche Model of Aedes aegypti (Diptera: Culicidae) in the Central Mexican Highlands. J. Med. Entomol. 2020, 57, 728–737. [Google Scholar] [CrossRef] [PubMed]
- Estallo, E.L.; Sangermano, F.; Grech, M.; Luduena-Almeida, F.; Frias-Cespedes, M.; Ainete, M.; Almiron, W.; Livdahl, T. Modelling the distribution of the vector Aedes aegypti in a central Argentine city. Med. Vet. Entomol. 2018, 32, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Wijayanti, S.P.; Porphyre, T.; Chase-Topping, M.; Rainey, S.M.; McFarlane, M.; Schnettler, E.; Biek, R.; Kohl, A. The Importance of Socio-Economic Versus Environmental Risk Factors for Reported Dengue Cases in Java, Indonesia. PLoS Negl. Trop. Dis. 2016, 10, e0004964. [Google Scholar] [CrossRef]
- Pham, N.T.T.; Nguyen, C.T.; Vu, H.H. Assessing and modelling vulnerability to dengue in the Mekong Delta of Vietnam by geospatial and time-series approaches. Environ. Res. 2020, 186, 10. [Google Scholar] [CrossRef]
- Wiese, D.; Escalante, A.A.; Murphy, H.; Henry, K.A.; Gutierrez-Velez, V.H. Integrating environmental and neighborhood factors in MaxEnt modeling to predict species distributions: A case study of Aedes albopictus in southeastern Pennsylvania. PLoS ONE 2019, 14, 23. [Google Scholar] [CrossRef]
- Li, Q.; Ren, H.; Zheng, L.; Cao, W.; Zhang, A.; Zhuang, D.; Lu, L.; Jiang, H. Ecological niche modeling identifies fine-scale areas at high risk of dengue fever in the pearl river delta, China. Int. J. Environ. Res. Public Health 2017, 14, 619. [Google Scholar] [CrossRef]
- Naqvi, S.A.A.; Sajjad, M.; Waseem, L.A.; Khalid, S.; Shaikh, S.; Kazmi, S.J.H. Integrating Spatial Modelling and Space-Time Pattern Mining Analytics for Vector Disease-Related Health Perspectives: A Case of Dengue Fever in Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 12018. [Google Scholar] [CrossRef]
- Ha, T.V.; Kim, W.; Nguyen-Tien, T.; Lindahl, J.; Nguyen-Viet, H.; Thi, N.Q.; Nguyen, H.V.; Unger, F.; Lee, H.S. Spatial distribution of Culex mosquito abundance and associated risk factors in Hanoi, Vietnam. PLoS Negl. Trop. Dis. 2021, 15, e0009497. [Google Scholar] [CrossRef] [PubMed]
- Ren, H.; Zheng, L.; Li, Q.; Yuan, W.; Lu, L. Exploring Determinants of Spatial Variations in the Dengue Fever Epidemic Using Geographically Weighted Regression Model: A Case Study in the Joint Guangzhou-Foshan Area, China, 2014. Int. J. Environ. Res. Public Health 2017, 14, 1518. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Ren, H.; Lu, L. Increasingly expanded future risk of dengue fever in the Pearl River Delta, China. PLoS Negl. Trop. Dis. 2021, 15, e0009745. [Google Scholar] [CrossRef] [PubMed]
- Trewin, B.J.; Parry, H.R.; Pagendam, D.E.; Devine, G.J.; Zalucki, M.P.; Darbro, J.M.; Jansen, C.C.; Schellhorn, N.A. Simulating an invasion: Unsealed water storage (rainwater tanks) and urban block design facilitate the spread of the dengue fever mosquito, Aedes aegypti, in Brisbane, Australia. Biol. Invasions 2021, 23, 3891–3906. [Google Scholar] [CrossRef]
- Acharya, B.K.; Cao, C.; Lakes, T.; Chen, W.; Naeem, S.; Pandit, S. Modeling the spatially varying risk factors of dengue fever in Jhapa district, Nepal, using the semi-parametric geographically weighted regression model. Int. J. Biometeorol. 2018, 62, 1973–1986. [Google Scholar] [CrossRef]
- Yin, M.S.; Bicout, D.; Haddawy, P.; Schoning, J.; Laosiritaworn, Y.; Sa-Angchai, P. Added-value of mosquito vector breeding sites from street view images in the risk mapping of dengue incidence in Thailand. PLoS Negl. Trop. Dis. 2021, 15, 26. [Google Scholar]
- Ajim Ali, S.; Ahmad, A. Using analytic hierarchy process with GIS for Dengue risk mapping in Kolkata Municipal Corporation, West Bengal, India. Spat. Inf. Res. 2018, 26, 449–469. [Google Scholar] [CrossRef]
- Jaya, I.; Folmer, H. Spatiotemporal high-resolution prediction and mapping: Methodology and application to dengue disease. J. Geogr. Syst. 2022, 24, 527–581. [Google Scholar] [CrossRef]
- CDC Dengue Around the World. Available online: https://www.cdc.gov/dengue/areaswithrisk/around-the-world.html (accessed on 27 August 2022).
- Attaway, D.F.; Jacobsen, K.H.; Falconer, A.; Manca, G.; Waters, N.M. Risk analysis for dengue suitability in Africa using the ArcGIS predictive analysis tools (PA tools). Acta Trop. 2016, 158, 248–257. [Google Scholar] [CrossRef]
- Hu, W.; Clements, A.C.A.; Williams, G.M.; Tong, S.; Mengersen, K.L. Spatial Patterns and Socioecological Drivers of Dengue Fever Transmission in Queensland, Australia. Environ. Health Perspect. 2012, 120, 260–266. [Google Scholar] [CrossRef]
- de Melo, D.P.; Scherrer, L.R.; Eiras, A.E. Dengue fever occurrence and vector detection by larval survey, ovitrap and MosquiTRAP: A space-time clusters analysis. PLoS ONE 2012, 7, e42125. [Google Scholar] [CrossRef] [PubMed]
- WHO. Manual on Environmental Management for Mosquito Control, with Special Emphasis on Malaria Vectors; World Health Organization: Geneva, Switzerland, 1982. [Google Scholar]
- Qi, X.; Wang, Y.; Li, Y.; Meng, Y.; Chen, Q.; Ma, J.; Gao, G.F. The Effects of Socioeconomic and Environmental Factors on the Incidence of Dengue Fever in the Pearl River Delta, China, 2013. PLoS Negl. Trop. Dis. 2015, 9, e0004159. [Google Scholar] [CrossRef] [PubMed]
- Kala, A.K.; Tiwari, C.; Mikler, A.R.; Atkinson, S.F. A comparison of least squares regression and geographically weighted regression modeling of West Nile virus risk based on environmental parameters. PeerJ 2017, 5, e3070. [Google Scholar] [CrossRef]
- Ma, S.; Ooi, E.E.; Goh, K.T. Socioeconomic Determinants of Dengue Incidence in Singapore. Dengue Bull. 2008, 32, 17–28. [Google Scholar]
- Whiteman, A.; Delmelle, E.; Rapp, T.; Chen, S.; Chen, G.; Dulin, M. A Novel Sampling Method to Measure Socioeconomic Drivers of Aedes Albopictus Distribution in Mecklenburg County, North Carolina. Int. J. Environ. Res. Public Health 2018, 15, 2179. [Google Scholar] [CrossRef] [PubMed]
- Jordan, M.I.; Mitchell, T.M. Machine learning: Trends, perspectives, and prospects. Science 2015, 349, 255–260. [Google Scholar] [CrossRef]
- Charlton, M.; Fotheringham, S.; Brunsdon, C. Geographically Weighted Regression; White Paper; National Centre for Geocomputation, National University of Ireland Maynooth: Maynooth, Ireland, 2009; p. 2. [Google Scholar]
- Marshall, R.J. Mapping Disease and Mortality Rates Using Empirical Bayes Estimators. Appl. Stat. 1991, 40, 283–294. [Google Scholar] [CrossRef]
- Hussain-Alkhateeb, L.; Rivera Ramirez, T.; Kroeger, A.; Gozzer, E.; Runge-Ranzinger, S. Early warning systems (EWSs) for chikungunya, dengue, malaria, yellow fever, and Zika outbreaks: What is the evidence? A scoping review. PLoS Negl. Trop. Dis. 2021, 15, e0009686. [Google Scholar] [CrossRef]
- Lobo, J.M.; Jiménez-Valverde, A.; Real, R. AUC: A misleading measure of the performance of predictive distribution models. Glob. Ecol. Biogeogr. 2008, 17, 145–151. [Google Scholar] [CrossRef]
- Li, Y.; Li, M.; Li, C.; Liu, Z. Optimized Maxent Model Predictions of Climate Change Impacts on the Suitable Distribution of Cunninghamia lanceolata in China. Forests 2020, 11, 302. [Google Scholar] [CrossRef]
- Cromwell, E.A.; Stoddard, S.T.; Barker, C.M.; Van Rie, A.; Messer, W.B.; Meshnick, S.R.; Morrison, A.C.; Scott, T.W. The relationship between entomological indicators of Aedes aegypti abundance and dengue virus infection. PLoS Negl. Trop. Dis. 2017, 11, e0005429. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, W.P.; Suzuki, M.; Thiem, V.D.; White, R.G.; Tsuzuki, A.; Yoshida, L.M.; Yanai, H.; Haque, U.; Thole, H.; Anh, D.D.; et al. Population density, water supply, and the risk of dengue fever in Vietnam: Cohort study and spatial analysis. PLoS Med. 2011, 8, e1001082. [Google Scholar] [CrossRef] [PubMed]
- Chiaravalloti-Neto, F.; da Silva, R.A.; Zini, N.; da Silva, G.C.D.; da Silva, N.S.; Parra, M.C.P.; Dibo, M.R.; Estofolete, C.F.; Favaro, E.A.; Dutra, K.R.; et al. Seroprevalence for dengue virus in a hyperendemic area and associated socioeconomic and demographic factors using a cross-sectional design and a geostatistical approach, state of Sao Paulo, Brazil. BMC Infect. Dis. 2019, 19, 441. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Kao, S.-C.; Shih, C.-H.; Kan, M.-H. Open data mining for Taiwan’s dengue epidemic. Acta Trop. 2018, 183, 1–7. [Google Scholar] [CrossRef]
- Kraemer, M.U.; Bisanzio, D.; Reiner, R.; Zakar, R.; Hawkins, J.B.; Freifeld, C.C.; Smith, D.L.; Hay, S.I.; Brownstein, J.S.; Perkins, T.A. Inferences about spatiotemporal variation in dengue virus transmission are sensitive to assumptions about human mobility: A case study using geolocated tweets from Lahore, Pakistan. EPJ Data Sci. 2018, 7, 16. [Google Scholar] [CrossRef]
- Bomfim, R.; Pei, S.; Shaman, J.; Yamana, T.; Makse, H.A.; Andrade, J.S., Jr.; Lima Neto, A.S.; Furtado, V. Predicting dengue outbreaks at neighbourhood level using human mobility in urban areas. J. R Soc. Interface 2020, 17, 20200691. [Google Scholar] [CrossRef]
| Levels | Key Words for Querying |
|---|---|
| 1 | ‘dengue’ OR ‘dengue fever’ |
| 2 | ‘risk’ OR ‘vulnerability’ OR ‘hot spot’ |
| 3 | ‘map*’ OR ‘model*’ |
| 4 | ‘spatial’ OR ‘spatiotemporal’ OR ‘distribution’ |
| No. | References | No. | References | No. | References |
|---|---|---|---|---|---|
| D1 | Dickin and Schuster-Wallace [24] | D11 | Ong et al. [26] | A1 | Machault et al. [25] |
| D2 | Wen et al. [27] | D12 | Martinez-Bello et al. [28] | A2 | Espinosa et al. [29] |
| D3 | Mao et al. [30] | D13 | Ghosh et al. [31] | A3 | Fatima et al. [32] |
| D4 | Yu et al. [33] | D14 | Desjardins et al. [34] | A4 | Little et al. [35] |
| D5 | Chen et al. [36] | D15 | Ordonez-Sierra et al. [37] | A5 | Estallo et al. [38] |
| D6 | Wijayanti et al. [39] | D16 | Pham et al. [40] | A6 | Wiese et al. [41] |
| D7 | Li et al. [42] | D17 | Naqvi et al. [43] | A7 | Ha et al. [44] |
| D8 | Ren et al. [45] | D18 | Wu et al. [46] | A8 | Trewin et al. [47] |
| D9 | Acharya et al. [48] | D19 | Yin et al. [49] | ||
| D10 | Ajim Ali and Ahmad [50] | D20 | Jaya and Folmer [51] | ||
| Variables | Positive | Negative | Nonlinear | Unknown |
|---|---|---|---|---|
| Air temperature | D20 (monthly); A3 (monthly), A4(monthly), | D14 * (weekly), | D7 (warmest month); D18 (seasonally), A6(seasonally) | D3, D15 |
| Daily temperature range | D14 * (weekly) | A3 (monthly), | ||
| Cool days (<18 °C) | D14 * (weekly) | |||
| Warm days (>32 °C) | D14 * (weekly) | |||
| LST | D8, D9, D10 (>25 °C) | D12, D13, D17, D19 | ||
| nLST | D6 (<20 °C) | |||
| Relative humidity | D8 (yearly); A1 (daily), A4 (monthly) | |||
| Water vapor pressure | D20 (monthly); | |||
| Precipitation | D8 (yearly), D19 (seasonally), D20 (monthly); A1 (daily), A4 (monthly), A6 (seasonally), A8 (monthly) | D18 (monthly), D14 * (weekly) | D7 (warmest month); A3 (monthly), | D3, D15 |
| Solar radiation | D20 (monthly) |
| Types | Variables | Positive | Negative | Nonlinear | Unknown |
|---|---|---|---|---|---|
| Land Cover | Built-up/ impervious area | D7, D8 *, D17, D18 *; | |||
| A2, A5, A6 | A1 (asphalt) | A6 * | |||
| NDVI (EVI) | D17; A5, A7 | D8 *, D9, D11, D13 | D7 (warm season); A6 * | D15 | |
| Trees density/canopy | D14 | A6 * | |||
| NDWI | A2 | A4 * | A6 * | ||
| Land Use | Residential use | D11, D13; A4 * | |||
| Open space use | A4 * | ||||
| Greenings | A3, A4 | A1, A6 * | |||
| Vacant use | A2 | ||||
| Unplanned area | D13; A4 | ||||
| Morphology | Property size | A8 | |||
| Landscape | Proximity to parks/managed vegetation | D3 * | |||
| Proximity to water bodies/rivers | D13; A5 | D14; | D3 * | ||
| Road | Road density | D8 *, D11, D7, D18 | D3 * | ||
| Road length | A8 | ||||
| Establishment | Proximity to specific establishment | D14 (tires and plant nurseries); A5 (cemeteries, tires) | D6 (hospital) | D2 (species), D3 * (workplaces) | |
| Infrastructure | Container density | D19 (types) | |||
| Water tanks | A8 | ||||
| Drain network | D13 | ||||
| Topography | Flow accumulation | A6 * | |||
| Elevation | D13 | D3; A3 | A6 * | ||
| Slope | A6 * |
| Types | Variables | Positive | Negative | Nonlinear | Unknown |
|---|---|---|---|---|---|
| Population | Population density | D8 *, D19, D18 *; A7, A8 | D14 | D7; A6 * | A3 |
| Household density (households/100/km2) | D11; A5, A6 * | ||||
| Development | GDP | D8 *, D18 * | |||
| Demography | Age > 65/60 | D14 | |||
| Age < 14/15/school | D14 | ||||
| Low education | D6, D14 | A6 * | |||
| Low income | D14 | A6 * | |||
| Rate of unemployment | D14 | D6 | |||
| Living conditions | Infection history | D11 | |||
| Vacant housing | A6 * | ||||
| Neighborhood quality | A5 | A6 * | |||
| Without piped water | A5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yin, S.; Ren, C.; Shi, Y.; Hua, J.; Yuan, H.-Y.; Tian, L.-W. A Systematic Review on Modeling Methods and Influential Factors for Mapping Dengue-Related Risk in Urban Settings. Int. J. Environ. Res. Public Health 2022, 19, 15265. https://doi.org/10.3390/ijerph192215265
Yin S, Ren C, Shi Y, Hua J, Yuan H-Y, Tian L-W. A Systematic Review on Modeling Methods and Influential Factors for Mapping Dengue-Related Risk in Urban Settings. International Journal of Environmental Research and Public Health. 2022; 19(22):15265. https://doi.org/10.3390/ijerph192215265
Chicago/Turabian StyleYin, Shi, Chao Ren, Yuan Shi, Junyi Hua, Hsiang-Yu Yuan, and Lin-Wei Tian. 2022. "A Systematic Review on Modeling Methods and Influential Factors for Mapping Dengue-Related Risk in Urban Settings" International Journal of Environmental Research and Public Health 19, no. 22: 15265. https://doi.org/10.3390/ijerph192215265
APA StyleYin, S., Ren, C., Shi, Y., Hua, J., Yuan, H.-Y., & Tian, L.-W. (2022). A Systematic Review on Modeling Methods and Influential Factors for Mapping Dengue-Related Risk in Urban Settings. International Journal of Environmental Research and Public Health, 19(22), 15265. https://doi.org/10.3390/ijerph192215265







