Temporal Associations between Actigraphy-Measured Daytime Movement Behaviors and Nap Sleep in Early Childhood
Abstract
:1. Introduction
2. Materials and Methods
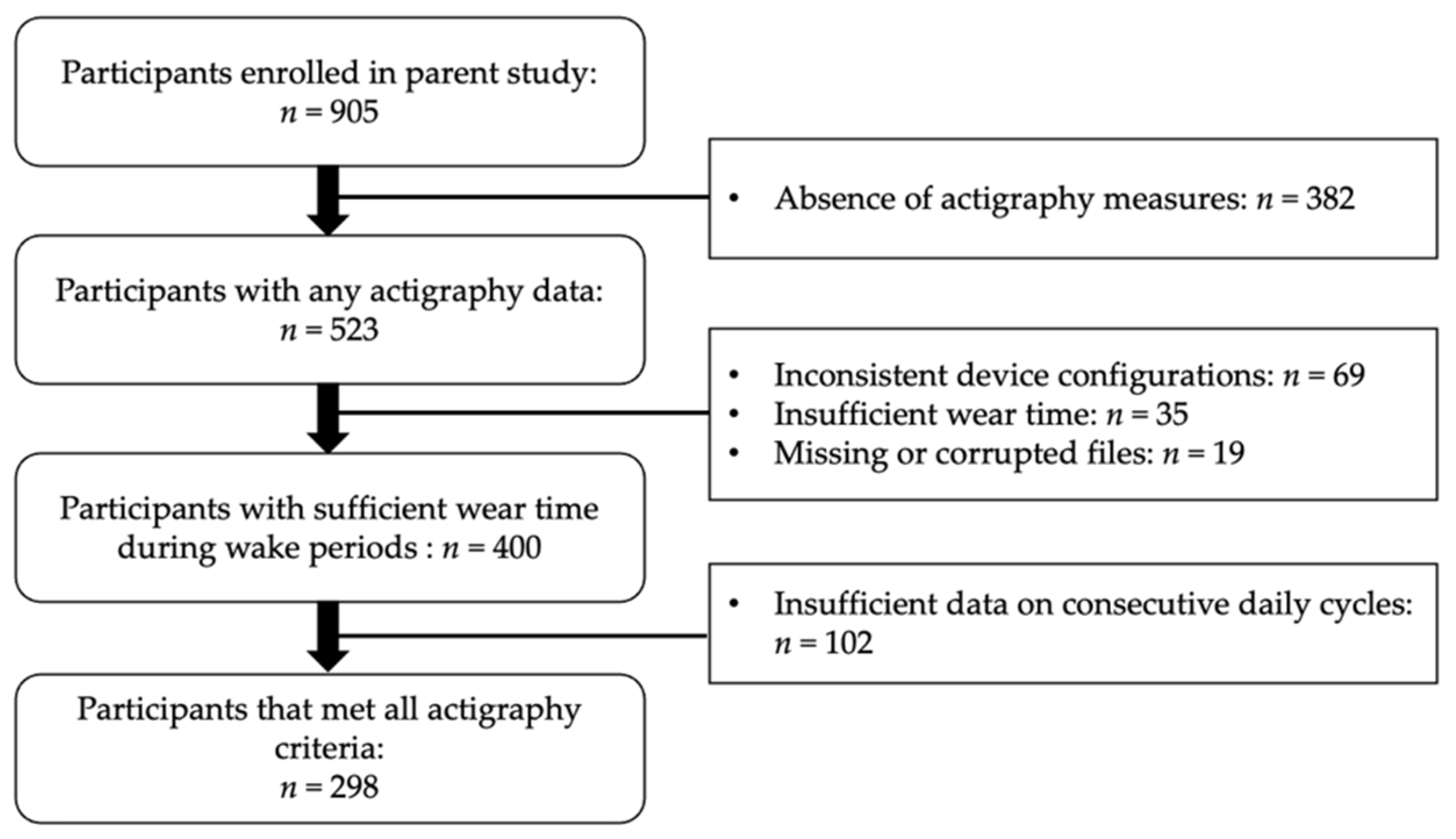
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Analysis
3. Results
3.1. Participant Characteristics
3.2. Likelihood of Napping
3.3. Nap Duration and Sleep Efficiency
3.4. Next Day Movement Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Galland, B.C.; Taylor, B.J.; Elder, D.E.; Herbison, P. Normal sleep patterns in infants and children: A systematic review of observational studies. Sleep Med. Rev. 2012, 16, 213–222. [Google Scholar] [CrossRef]
- Iglowstein, I.; Jenni, O.G.; Molinari, L.; Largo, R.H. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 2003, 111, 302–307. [Google Scholar] [CrossRef]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2016, 12, 785–786. [Google Scholar] [CrossRef]
- Smith, S.S.; Edmed, S.L.; Staton, S.L.; Pattinson, C.L.; Thorpe, K.J. Correlates of naptime behaviors in preschool aged children. Nat. Sci. Sleep 2019, 11, 27–34. [Google Scholar] [CrossRef] [Green Version]
- Spencer, R.M.C.; Riggins, T. Contributions of memory and brain development to the bioregulation of naps and nap transitions in early childhood. Proc. Natl. Acad. Sci. USA 2022, 119, e2123415119. [Google Scholar] [CrossRef]
- Hinkley, T.; Salmon, J.; Okely, A.D.; Hesketh, K.; Crawford, D. Correlates of preschool children’s physical activity. Am. J. Prev. Med. 2012, 43, 159–167. [Google Scholar] [CrossRef]
- Tonge, K.L.; Jones, R.A.; Okely, A.D. Correlates of children’s objectively measured physical activity and sedentary behavior in early childhood education and care services: A systematic review. Prev. Med. 2016, 89, 129–139. [Google Scholar] [CrossRef] [Green Version]
- Thorpe, K.; Staton, S.; Sawyer, E.; Pattinson, C.; Haden, C.; Smith, S. Napping, development and health from 0 to 5 years: A systematic review. Arch. Dis. Child 2015, 100, 615–622. [Google Scholar] [CrossRef]
- Liu, J.; Feng, R.; Ji, X.; Cui, N.; Raine, A.; Mednick, S.C. Midday napping in children: Associations between nap frequency and duration across cognitive, positive psychological well-being, behavioral, and metabolic health outcomes. Sleep 2019, 42, zsz126. [Google Scholar] [CrossRef]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and exercise: A reciprocal issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Dolezal, B.A.; Neufeld, E.V.; Boland, D.M.; Martin, J.L.; Cooper, C.B. Interrelationship between sleep and exercise: A systematic review. Adv. Prev. Med. 2017, 2017, 1364387. [Google Scholar] [PubMed] [Green Version]
- St. Laurent, C.W.; Spencer, R.M.C. A systematic review of the relationships between physical activity and sleep in youth. Ann. Behav. Med. 2020, 54 (Suppl. S1), C312. [Google Scholar]
- Antczak, D.; Lonsdale, C.; Lee, J.; Hilland, T.; Duncan, M.J.; del Pozo Cruz, B.; Hulteen, R.M.; Parker, P.D.; Sanders, T. Physical activity and sleep are inconsistently related in healthy children: A systematic review and meta-analysis. Sleep Med. Rev. 2020, 51, 101278. [Google Scholar] [CrossRef]
- Souabni, M.; Hammouda, O.; Romdhani, M.; Trabelsi, K.; Ammar, A.; Driss, T. Benefits of daytime napping opportunity on physical and cognitive performances in physically active participants: A systematic review. Sport. Med. 2021, 51, 2115–2146. [Google Scholar] [CrossRef] [PubMed]
- Parsons, A.A.; Ollberding, N.J.; Smith, L.; Copeland, K.A. Sleep matters: The association of race, bedtime, outdoor time, and physical activity with preschoolers’ sleep. Prev. Med. Rep. 2018, 12, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Kohyama, J. Early rising children are more active than late risers. Neuropsychiatr. Dis. Treat. 2007, 3, 959–963. [Google Scholar] [CrossRef] [Green Version]
- Yu, M.L.; Ziviani, J.M.; Haynes, M. Sleep, structured and social time use and young Australian children’s physical activity. Health Promot. J. Aust. 2011, 22, 203–209. [Google Scholar] [CrossRef] [PubMed]
- St. Laurent, C.W.; Burkart, S.; Rodheim, K.; Marcotte, R.; Spencer, R.M.C. Cross-sectional associations of 24-hour sedentary time, physical activity, and sleep duration compositions with sleep quality and habits in preschoolers. Int. J. Environ. Res. Public Health 2020, 17, 7148. [Google Scholar] [CrossRef] [PubMed]
- Bolger, N.; Laurenceau, J.P. Intensive Longitudinal Methods: An Introduction to Diary and Experience Sampling Research; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Irish, L.A.; Kline, C.; Rothenberger, S.D.; Krafty, R.; Buysse, D.J.; Kravitz, H.M.; Bromberger, J.; Zheng, H.; Hall, M.H. A 24-hour approach to the study of health behaviors: Temporal relationships between waking health behaviors and sleep. Ann. Behav. Med. 2014, 47, 189–197. [Google Scholar] [CrossRef] [Green Version]
- Atoui, S.; Chevance, G.; Romain, A.J.; Kingsbury, C.; Lachance, J.P.; Bernard, P. Daily associations between sleep and physical activity: A systematic review and meta-analysis. Sleep Med. Rev. 2021, 57, 101426. [Google Scholar] [CrossRef] [PubMed]
- Ekstedt, M.; Nyberg, G.; Ingre, M.; Ekblom, O.; Marcus, C. Sleep, physical activity and BMI in six to ten-year-old children measured by accelerometry: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 82. [Google Scholar] [CrossRef] [PubMed]
- Krietsch, K.N.; Armstrong, B.; McCrae, C.S.; Janicke, D.M. Temporal associations between sleep and physical activity among overweight/obese youth. J. Pediatr. Psychol. 2016, 41, 680–691. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Tremblay, M.S.; Katzmarzyk, P.T.; Fogelholm, M.; Hu, G.; Lambert, E.V.; Maher, C.; Maia, J.; Olds, T.; Sarmiento, O.L.; et al. Temporal and bi-directional associations between sleep duration and physical activity/sedentary time in children: An international comparison. Prev. Med. 2018, 111, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Pesonen, A.K.; Sjöstén, N.M.; Matthews, K.A.; Heinonen, K.; Martikainen, S.; Kajantie, E.; Tammelin, T.; Eriksson, J.G.; Strandberg, T.; Räikkönen, K. Temporal associations between daytime physical activity and sleep in children. PLoS ONE 2011, 6, e22958. [Google Scholar] [CrossRef]
- Sorić, M.; Starc, G.; Borer, K.T.; Jurak, G.; Kovač, M.; Strel, J.; Mišigoj-Duraković. Associations of objectively assessed sleep and physical activity in 11-year old children. Ann. Hum. Biol. 2015, 42, 31–37. [Google Scholar] [CrossRef]
- Vincent, G.E.; Barnett, L.M.; Lubans, D.R.; Salmon, J.; Timperio, A.; Ridgers, N.D. Temporal and bidirectional associations between physical activity and sleep in primary school-aged children. Appl. Physiol. Nutr. Metab. 2017, 42, 238–242. [Google Scholar] [CrossRef] [Green Version]
- Armstrong, B.; Beets, M.W.; Starrett, A.; Brazendale, K.; Turner-McGrievy, G.; E Saelens, B.; Pate, R.R.; Youngstedt, S.D.; Maydeu-Olivares, A.; Weaver, R.G. Dynamics of sleep, sedentary behavior, and moderate-to-vigorous physical activity on school versus nonschool days. Sleep 2020, 44, zsaa174. [Google Scholar] [CrossRef]
- St. Laurent, C.W.; Andre, C.; Holmes, J.F.; Fields, N.D.; Spencer, R.M.C. Temporal relationships between device-derived sedentary behavior, physical activity, and sleep in early childhood. Sleep 2022, 45, zsac008. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Meltzer, L.J.; Walsh, C.M.; Peightal, A.A. Comparison of actigraphy immobility rules with polysomnographic sleep onset latency in children and adolescents. Sleep Breath. 2015, 19, 1415–1423. [Google Scholar] [CrossRef] [Green Version]
- Hyde, M.; O’Driscoll, D.M.; Binette, S.; Galang, C.; Tan, S.K.; Verginis, N.; Davey, M.J.; Horne, R.S.C. Validation of actigraphy for determining sleep and wake in children with sleep disordered breathing. J. Sleep Res. 2007, 16, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, M.È.; Bernier, A.; Paquet, J.; Simard, V.; Carrier, J. Validating Actigraphy as a Measure of Sleep for Preschool Children. J. Clin. Sleep Med. 2013, 9, 701–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oakley, N. Validation with Polysomnography of the Sleepwach Sleep/Wake Scoring Algorithm Used by The Actiwatch activity Monitoring System; Philips Respironics: Bend, OR, USA, 1997. [Google Scholar]
- Sitnick, S.L.; Goodlin-Jones, B.L.; Anders, T.F. The use of actigraphy to study sleep disorders in preschoolers: Some concerns about detection of nighttime awakenings. Sleep 2008, 31, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Ekblom, O.; Nyberg, G.; Bak, E.E.; Ekelund, U.; Marcus, C. Validity and comparability of a wrist-worn accelerometer in children. J. Phys. Act. Health 2012, 9, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Alhassan, S.; Sirard, J.R.; Kurdziel, L.B.F.; Merrigan, S.; Greever, C.; Spencer, R.M.C. Cross-validation of two accelerometers for assessment of physical activity and sedentary time in preschool children. Pediatr. Exerc. Sci. 2017, 29, 268–277. [Google Scholar] [CrossRef]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Delisle Nyström, C.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: A systematic review and practical considerations. Sport. Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef]
- Berzofsky, M.; Smiley-McDonald, H.; Moore, A.; Krebs, C. Measuring Socioeconomic Status (SES) in the NCVS: Background, Options, and Recommendations; Bureau of Justice Statistics, U.S. Department of Justice: Washington, DC, USA, 2014. [Google Scholar]
- Wood, A.P.; Imai, S.; McMillan, A.G.; Swift, D.; DuBose, K.D. Physical activity types and motor skills in 3-5-year old children: National Youth Fitness Survey. J. Sci. Med. Sport 2020, 23, 390–395. [Google Scholar] [CrossRef]
- Sigmund, E.; de Ste Croix, M.; Miklánková, L.; Frömel, K. Physical activity patterns of kindergarten children in comparison to teenagers and young adults. Eur. J. Public Health 2007, 17, 646–651. [Google Scholar] [CrossRef] [Green Version]
- Best, J.R. Effects of physical activity on children’s executive function. Dev. Rev. 2010, 30, 331–551. [Google Scholar] [CrossRef]
- Reilly, J.J. When does it all go wrong? Longitudinal studies of changes in moderate-to-vigorous-intensity physical activity across childhood and adolescence. J. Exerc. Sci. Fit. 2016, 14, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Kurdziel, L.; Duclos, K.; Spencer, R.M.C. Sleep spindles in midday naps enhance learning in preschool children. Proc. Natl. Acad. Sci. USA 2013, 110, 17267–17272. [Google Scholar] [CrossRef] [PubMed]
- Spencer, R.M.C. Neurophysiological basis of sleep’s function on memory and cognition. ISRN Physiol. 2013, 71, 233–236. [Google Scholar] [CrossRef] [PubMed]
| Variables | Mean (SD) or n (%) | Range | |
|---|---|---|---|
| General characteristics | |||
| Age (months) | 51.0 (9.6) | 33 to 70 | |
| Sex (female) | 130 (43.6) | - | |
| Socioeconomic status (score: 0 to 7) | 4.5 (2.0) | 2 to 7 | |
| Race | |||
| White | 183 (61.3) | - | |
| Black/African American | 26 (8.7) | - | |
| Asian | 13 (4.4) | - | |
| Native Hawaiian/Pacific Islander | 2 (0.7) | - | |
| Two or more racial groups | 34 (11.4) | - | |
| Other | 21 (7.1) | - | |
| Missing | 19 (6.4) | - | |
| Hispanic | |||
| Yes | 79 (69.5) | - | |
| No | 207 (26.5) | - | |
| Missing | 12 (4.0) | - | |
| Nap sleep | |||
| Duration (min) * | 91.7 (25.9) | 24.6 to 221 | |
| Efficiency (%) | 85.2 (10.6) | 37.5 to 98 | |
| Frequency (#/week) | 3.7 (2.0) | 0 to 7 | |
| Daytime movement behaviors | |||
| Sedentary time (%) | 41.8 (7.6) | 18.3 to 65.4 | |
| Total physical activity (counts/min) | 565.73 (104.24) | 278.69 to 1025.68 | |
| Morning movement behaviors ** | |||
| Sedentary time (%) | 39.6 (8.6) | 14.3 to 70.0 | |
| Total physical activity (counts/min) | 579.59 (115.26) | 247.29 to 1049.63 | |
| Overnight sleep | |||
| Duration (min) | 570.31 (40.1) | 4660.15 to 690.97 | |
| Efficiency (%) | 88.3 (3.4) | 78.5 to 95.5 | |
| Next Day Nap | Same Day Nap | |||
|---|---|---|---|---|
| OR (SE) | 95% CI | OR (SE) | 95% CI | |
| Models with sedentary time | ||||
| Sedentary time | 1.00 (0.009) | 0.98 to 1.0 | 0.96 (0.009) | 0.94 to 0.98 |
| Night sleep | 0.99 (0.001) | 0.99 to 1.0 | 0.99 (0.002) | 0.99 to 1.0 |
| Day | 0.94 (0.02) | 0.91 to 0.98 | 0.93 (0.02) | 0.90 to 0.97 |
| Age | 0.94 (0.01) | 0.92 to 0.97 | 0.94 (0.01) | 0.92 to 0.97 |
| SES | 0.93 (0.05) | 0.84 to 1.0 | 0.89 (0.05) | 0.79 to 0.99 |
| Sex | 0.90 (0.19) | 0.59 to 1.4 | 0.92 (0.22) | 0.58 to 1.5 |
| Intercept | 1.47 (0.22) | - | 1.67 | - |
| Models with physical activity | ||||
| Physical activity | 0.99 (0.0008) | 0.99 to 1.00 | 10.01 (0.0007) | 1.001 to 1.004 |
| Night sleep | 0.99 (0.001) | 0.99 to 1.0 | 0.99 (0.001) | 0.99 to 1.00 |
| Day | 0.94 (0.02) | 0.91 to 0.98 | 0.93 (0.02) | 0.90 to 0.97 |
| Age | 0.95 (0.01) | 0.93 to 0.97 | 0.95 (0.01) | 0.92 to 0.97 |
| SES | 0.93 (0.05) | 0.84 to 1.1 | 0.89 (0.05) | 0.79 to 1.0 |
| Sex | 0.90 (0.19) | 0.60 to 1.4 | 0.98 (0.22) | 0.63 to 1.52 |
| Intercept | 1.49 (0.23) | - | 1.6 (0.27) | - |
| Nap Duration | Nap Sleep Efficiency | |||
|---|---|---|---|---|
| Coef. (SE) | 95% CI | Coef. (SE) | 95% CI | |
| Models with sedentary time | ||||
| Model 1 | ||||
| Previous day’s sedentary time | 0.29 (0.22) | −0.12 to 0.72 | 0.02 (0.08) | −0.13 to 0.19 |
| Previous night’s sleep | 0.01 (0.03) | −0.04 to 0.07 | −0.002 (0.01) | −0.03 to 0.02 |
| Day | 0.17 (0.37) | −0.55 to 0.89 | 0.02 (0.15) | −0.28 to 0.32 |
| Age | −0.42 (0.19) | −0.70 to −0.05 | −0.21 (0.09) | −0.38 to −0.04 |
| SES | −1.7 (0.93) | −3.4 to 0.15 | −0.48 (0.43) | −1.3 to 0.36 |
| Sex | −1.8 (3.6) | −8.9 to 5.2 | −0.10 (1.7) | −3.4 to 3.2 |
| Intercept | 93.4 (2.6) | - | 85.5 (1.2) | - |
| Model 2 | ||||
| Morning sedentary time | 0.17 (0.19) | −0.20 to 0.53 | 0.03 (0.07) | −0.11 to 0.17 |
| Previous night’s sleep | 0.0007 (0.03) | −0.05 to 0.06 | −0.002 (0.012) | −0.03 to 0.02 |
| Day | 0.42 (0.34) | −0.24 to 1.1 | 0.07 (0.14) | −0.21 to 0.35 |
| Age | −0.46 (0.18) | −0.81 to −0.12 | −0.19 (0.09) | −0.36 to −0.01 |
| SES | −1.6 (.86) | −3.3 to 0.07 | 0.54 (0.44) | −1.4 to 0.31 |
| Sex | −1.3 (3.3) | −7.9 to 5.2 | −0.26 (1.7) | −3.6 to 3.1 |
| Intercept | 92.6 (2.4) | - | 85.7 (1.2) | - |
| Models with physical activity | ||||
| Model 1 | ||||
| Previous day’s physical activity | −0.02 (0.16) | −0.05 to 0.007 | −0.003 (0.007) | −0.02 to 0.01 |
| Previous night’s sleep | 0.02 (0.03) | −0.04 to 0.07 | −0.004 (0.01) | −0.03 to 0.02 |
| Day | 0.19 (0.37) | −0.53 to 0.91 | 0.04 (0.15) | −0.26 to 0.02 |
| Age | −0.42 (0.19) | −0.79 to −0.05 | −0.21 (0.09) | −0.38 to −0.04 |
| SES | −1.7 (0.93) | −3.5 to 0.11 | −0.46 (.43) | −1.3 to 0.38 |
| Sex | −1.5 (3.6) | −8.6 to 5.6 | −0.13 (1.7) | −3.4 to 3.2 |
| Intercept | 93.1 (2.6) | - | 85.5 (1.2) | - |
| Model 2 | ||||
| Morning physical activity | −0.02 (0.01) | −0.05 to 0.007 | −0.006 (0.006) | −0.02 to 0.006 |
| Previous night’s sleep | 0.004 (0.03) | −0.05 to 0.06 | −0.002 (0.01) | −0.03 to 0.02 |
| Day | 0.36 (0.34) | −0.31 to 1.0 | 0.08 (0.14) | −0.19 to 0.36 |
| Age | −0.48 (0.18) | −0.82 to −0.13 | −0.18 (0.09) | −0.36 to −0.01 |
| SES | −1.7 (0.87) | −3.4 to −0.01 | −0.49 (0.44) | −0.13 to 0.37 |
| Sex | −1.9 (3.4) | −8.6 to 4.7 | −0.68 (1.7) | −4.1 to 2.7 |
| Intercept | 93.2 (2.5) | - | 85.9 (1.3) | - |
| Sedentary Time | Physical Activity | |||
|---|---|---|---|---|
| Coef (SE) | 95% CI | Coef (SE) | 95% CI | |
| Previous day nap occurrence | −2.09 (0.57) | −3.2 to −0.99 | 25.8 (6.9) | 12.3 to 39.3 |
| Previous night’s sleep | −0.006 (0.005) | −0.02 to 0.003 | 0.10 (0.06) | −0.006 to 0.22 |
| Day | 0.08 (0.06) | −0.04 to 0.21 | −0.37 (0.76) | −1.9 to 1.1 |
| Age | −0.12 (0.06) | −0.23 to −0.02 | 2.5 (0.72) | 1.1 to 3.9 |
| SES | −0.46 (0.27) | −0.98 to 0.07 | 1.1 (3.5) | −5.7 to 7.9 |
| Sex | −0.96 (1.1) | −3.0 to 1.1 | 45.9 (13.8) | 18.8 to 73.0 |
| Intercept | 42.7 (0.76) | - | 539.76 (9.86) | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
St. Laurent, C.W.; Holmes, J.F.; Spencer, R.M.C. Temporal Associations between Actigraphy-Measured Daytime Movement Behaviors and Nap Sleep in Early Childhood. Int. J. Environ. Res. Public Health 2022, 19, 15308. https://doi.org/10.3390/ijerph192215308
St. Laurent CW, Holmes JF, Spencer RMC. Temporal Associations between Actigraphy-Measured Daytime Movement Behaviors and Nap Sleep in Early Childhood. International Journal of Environmental Research and Public Health. 2022; 19(22):15308. https://doi.org/10.3390/ijerph192215308
Chicago/Turabian StyleSt. Laurent, Christine W., Jennifer F. Holmes, and Rebecca M. C. Spencer. 2022. "Temporal Associations between Actigraphy-Measured Daytime Movement Behaviors and Nap Sleep in Early Childhood" International Journal of Environmental Research and Public Health 19, no. 22: 15308. https://doi.org/10.3390/ijerph192215308
APA StyleSt. Laurent, C. W., Holmes, J. F., & Spencer, R. M. C. (2022). Temporal Associations between Actigraphy-Measured Daytime Movement Behaviors and Nap Sleep in Early Childhood. International Journal of Environmental Research and Public Health, 19(22), 15308. https://doi.org/10.3390/ijerph192215308







